Abstract
Background and Purpose
There have been few reports on recent trends in the occurrence of epilepsy. The aim of this study was to estimate the incidence and prevalence of epilepsy and analyze their annual trends in Korea over the period 2009–2017.
Methods
This nationwide population-based study was carried out using the National Health Insurance Service of Korea database. A prevalent case was defined as one of a patient receiving a prescription of anticonvulsants under the diagnostic codes for epilepsy or seizure. An incident case was ascertained by confirming the absence of any epilepsy-related diagnostic codes and anticonvulsant prescription for 2 years or more before the operational definition for a prevalent case was met. Alternative operational definitions for epilepsy were tested. The temporal trends of the incidence and prevalence of epilepsy were analyzed using a Poisson regression model, and are expressed as average annual percentage changes (AAPCs).
Results
The incidence of epilepsy increased from 28.7/100,000 persons in 2009 to 35.4/100,000 persons in 2017. The prevalence increased gradually from 3.4/1,000 persons in 2009 to 4.8/1,000 persons in 2017. These increasing trends were more evident among elderly subjects aged ≥75 years and in those who had codes for epilepsy or seizure as an additional diagnosis. Age standardization revealed a less prominent but still increasing trend in both incidence (AAPC=0.48%) and prevalence (AAPC=3.11%).
Conclusions
There have been increasing trends in both the prevalence and incidence of epilepsy in Korea between 2009 and 2017. This finding appears to be related to societal aging and the high incidence of symptomatic epilepsy in the elderly population.
Keywords: epilepsy, epidemiology, incidence, prevalence, trend
INTRODUCTION
Epilepsy is the third most common neurological disorder after stroke and dementia,1 affecting approximately 70 million patients worldwide.2 A recent meta-analysis of 222 studies reported a point prevalence of epilepsy of 6.38/1,000 persons and a lifetime prevalence of 7.6/1,000 persons. The incidence was 61.44/100,000 person-years.3 The prevalence has been reported to lie in the range 10.2–23.3/1,000 persons in developing countries,4,5,6 and 2.7–6.2/1,000 persons in developed countries.7,8,9 The incidence of epilepsy is also higher in developing countries than in developed countries.3 In short, around 90% of the global burden of epilepsy is carried by developing countries.10
With regard to age-specific occurrence, previous studies have demonstrated a high incidence of epilepsy in the first year of life and early childhood in both developing and developed countries,11 while an increase in the incidence of epilepsy among older people was noted in developed countries.12,13,14
How the occurrence of epilepsy changes as a society develops has not been fully addressed, since few studies have focused on time trends in the incidence and prevalence of epilepsy. The aim of this study was to estimate the annual incidence and prevalence of treated epilepsy in Korea and to identify time trends in these data between 2009 and 2017.
METHODS
Data sources and study population
Data from the National Health Insurance Service (NHIS) database of Korea between 2007 and 2017 were searched. The NHIS database encompasses the entire population and all medical facilities in Korea and includes a comprehensive database of diagnostic codes that were assigned according to the tenth revision of the International Classification of Diseases (ICD-10), laboratory examinations, medications, surgery, hospitalization, and socioeconomic profiles. The study population was the entire unselected Korean population registered in the NHIS database between 2009 and 2017.
Identification of prevalent and incident cases
Epilepsy was identified using the diagnostic codes for epilepsy and seizure, and anticonvulsant prescription data. The diagnostic codes for epilepsy included G40 (epilepsy), G41 (status epilepticus), F803 (Landau-Kleffner syndrome), and R56 (convulsion) according to the ICD-10, while R56.0 (febrile convulsion) was excluded. Anticonvulsants included carbamazepine, clobazam, ethosuximide, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, phenobarbital, phenytoin, pregabalin, primidone, topiramate, vigabatrin, valproate, zonisamide, lacosamide, and rufinamide. Clonazepam was excluded because it is usually administered for nonepileptic conditions such as tremors, insomnia, or anxiety, and is rarely used as an anticonvulsant monotherapy for epilepsy.
Four different operational definitions were used to identify epilepsy cases in the NHIS database, which are designated as criteria A–D. Criteria A comprised 1) at least two visits with one or more diagnostic codes for epilepsy extracted from among the five diagnostic codes, including primary, secondary, and additional diagnoses; and 2) the prescription of anticonvulsants for at least 180 days. Criteria B comprised 1) at least two visits with one or more diagnostic codes for epilepsy extracted from among the five diagnostic codes, including primary, secondary, and additional diagnoses; and 2) the prescription of anticonvulsants for any length of time. Criteria C comprised 1) at least one visit with one or more diagnostic codes for epilepsy extracted from the codes for primary or secondary diagnosis, and 2) the prescription of anticonvulsants for any length of time. Criteria D comprised 1) at least one visit with a diagnostic code for epilepsy extracted from the code for only primary diagnosis, and 2) the prescription of anticonvulsants for any length of time.
A prevalent case was defined as one in which a person satisfied criteria A, B, C, or D within each calendar year. An incident case was one in which a person had neither epilepsyrelated codes nor a prescription of anticonvulsants for at least 2 years before the operational definition for a prevalent case was met.
Age-standardized incidence and prevalence rates along with age- and sex-specific incidence and prevalence rates were estimated using criteria A.
Statistical analyses
The prevalence was calculated by dividing the number of prevalent cases by the total population for each calendar year. The cumulative incidence was calculated by dividing the number of incident cases by the total relevant standard population that excluded patients already diagnosed with epilepsy. The age-standardized incidence and prevalence rates were estimated by directly adjusting to the 2009 Korean population.
The annual trends in prevalence and incidence over time were assessed using a Poisson regression model and expressed as the average annual percent change (AAPC), which was calculated by exponentiating the coefficient of the regression. All reported p values are two-tailed, and p<0.05 was considered statistically significant. All statistical analyses were performed using SAS Enterprise Guide 7.1 for Windows (SAS Institute, Cary, NC, USA).
This study was approved by the Institutional Review Board of Sungkyunkwan University (approval number: 2018-06-006) and NHIS for Bioethics Policy (NHIS-2018-1-342).
RESULTS
Incidence according to diagnostic criteria, age, and sex
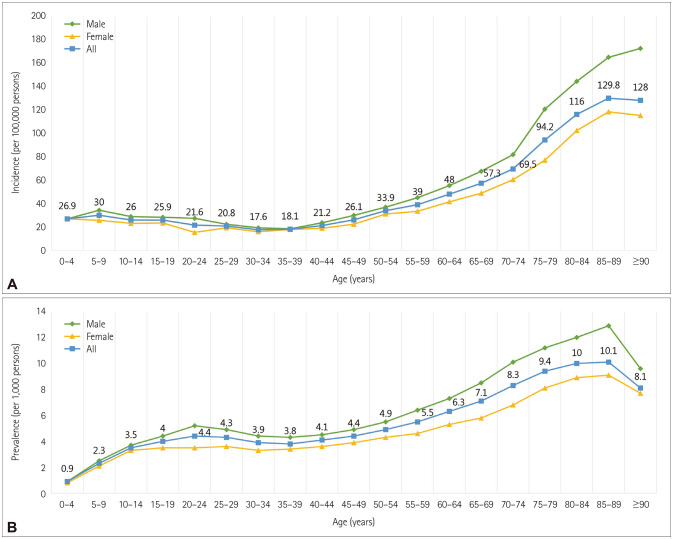
In 2017, the estimated annual cumulative incidence rates of epilepsy were 35.4/100,000 person-years according to criteria A, 132.9/100,000, 58.1/100,000, and 24.4/100,000 person-years according to criteria B–D, respectively (Table 1). The age-specific incidence estimated using criteria A exhibited a J-shaped curve, being lowest in the fourth decade of life (30s) and increasing thereafter, with an explosive increasing trend between the ages of 60 and 94 years. The incidence in 2017 was higher than 100/100,000 persons in males older than 75 years and in females older than 80 years. Among a total of 18,228 incident patients, 6,063 (33.2%) were 65 years or older in 2017. The incidence was higher in males than in females in most age groups [Supplementary Table 1 (in the online-only Data Supplement), Fig. 1A].
Table 1. Annual incidence of epilepsy for different operational definitions.
| Year | Incidence | Age-standardized incidence | AAPC, % | p | |||
|---|---|---|---|---|---|---|---|
| Criteria A | Criteria B | Criteria C | Criteria D | Criteria A | |||
| 2009 | 28.7 (14,258) | 86.8 (43,015) | 49.4 (24,498) | 24.6 (12,213) | 28.7 | 0.48 | <0.001* |
| 2010 | 30.7 (15,464) | 119.4 (59,997) | 64.8 (32,580) | 29.3 (14,783) | 30.3 | ||
| 2011 | 28.2 (14,261) | 116.0 (58,554) | 60.8 (30,716) | 27.5 (13,926) | 27.5 | ||
| 2012 | 29.3 (14,882) | 119.1 (60,313) | 60.7 (30,807) | 27.0 (13,715) | 28.2 | ||
| 2013 | 29.8 (15,155) | 122.1 (62,082) | 59.7 (60,427) | 25.1 (12,810) | 28.2 | ||
| 2014 | 31.1 (15,916) | 122.6 (62,560) | 57.1 (29,181) | 23.1 (11,845) | 29.1 | ||
| 2015 | 30.5 (15,634) | 118.6 (60,735) | 53.8 (27,593) | 22.0 (11,322) | 28.1 | ||
| 2016 | 31.2 (16,080) | 121.5 (62,398) | 54.5 (28,053) | 22.2 (11,461) | 28.5 | ||
| 2017 | 35.4 (18,228) | 132.9 (68,358) | 58.1 (29,959) | 24.4 (12,585) | 31.7 | ||
Annual incidence of epilepsy per 100,000 persons (numbers of incident cases) as estimated by applying criteria A–D (see main text).
*Statistical significance (p<0.05).
AAPC: average annual percentage change.
Fig. 1. Age-specific incidence (A) and prevalence (B) of epilepsy in 2017. A: Age-specific incidence was lowest in the thirties, explosive increasing trend from 60 years. B: The prevalence of epilepsy was found to be 10 per 1,000 persons or more in male aged 70 to 89. Both incidence and prevalence were higher in male than female in most age groups.
Annual trend of incidence
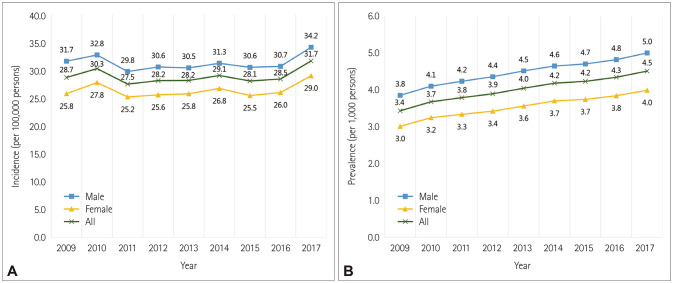
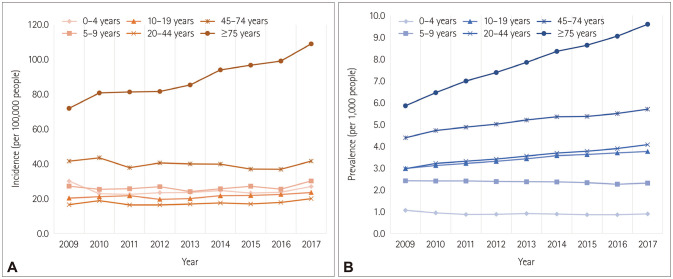
The incidence of epilepsy according to criteria A increased from 28.7/100,000 persons in 2009 to 35.4/100,000 persons in 2017 (Table 1). The incidence estimated using criteria B also increased, but was relatively stable when estimated using criteria C or D. The age-standardized incidence according to criteria A increased (AAPC=0.48%, p<0.001) (Fig. 2A, Table 1). Increasing trends were observed for both sexes [Fig. 2A, Supplementary Table 1 (in the online-only Data Supplement)]. The age-specific incidence exhibited a remarkable tendency to increase (AAPC increased by up to 15.49%) in the elderly population (age 75 years or older), but increased only slightly (AAPC=1.63–2.87%) in patients aged 10–34 years, and decreased slightly (AAPC=−1.6% to −0.84%) in patients aged 45–69 years [Fig. 3A, Supplementary Table 1 (in the online-only Data Supplement)].
Fig. 2. Annual trend of age-standardized incidence (A) and age-standardized prevalence (B) of epilepsy. Increasing trends of age-standardized incidence and prevalence were observed in both sexes.
Fig. 3. Annual trend of incidence (A) and prevalence (B) of epilepsy according to age. A: Age-specific incidence was a remarkable increasing tendency in 75 years or older. B: The prevalence tended to increase from the age of 9, the rate of increase has increased significantly since the age of 75.
Prevalence according to diagnostic criteria, age, and sex
In 2017, the prevalence rates of epilepsy were 4.8/1,000 persons according to criteria A, 6.7/1,000, 4.3/1,000, and 2.8/1,000 persons according to criteria B–D, respectively (Table 2). The age-specific prevalence increased until the ninth decade of life (80s), with a plateau from the third to fourth decades. In 2017, the prevalence of epilepsy was 10/1,000 persons or more in males aged 70–94 years. The total number of prevalent patients in that year was 249,878 according to criteria A, among whom 62,514 (25.0%) were older than 65 years. Sex-specific prevalence was higher in males than in females in all age groups [Fig. 1B, Supplementary Table 2 (in the online-only Data Supplement)].
Table 2. Annual prevalence of epilepsy for different operational definitions.
| Year | Prevalence | Age-standardized prevalence | AAPC, % | p | |||
|---|---|---|---|---|---|---|---|
| Criteria A | Criteria B | Criteria C | Criteria D | Criteria A | |||
| 2009 | 3.4 (170,730) | 4.5 (225,556) | 3.5 (174,583) | 2.4 (119,674) | 3.4 | 3.11 | <0.001* |
| 2010 | 3.7 (187,056) | 5.3 (269,076) | 4.0 (199,285) | 2.6 (131,602) | 3.7 | ||
| 2011 | 3.9 (195,125) | 5.5 (277,104) | 4.0 (202,479) | 2.6 (132,128) | 3.8 | ||
| 2012 | 4.0 (203,075) | 5.7 (289,541) | 4.1 (208,262) | 2.7 (133,953) | 3.9 | ||
| 2013 | 4.2 (213,484) | 5.9 (302,879) | 4.2 (213,042) | 2.7 (135,820) | 4.0 | ||
| 2014 | 4.4 (223,357) | 6.1 (311,874) | 4.2 (215,057) | 2.7 (135,832) | 4.2 | ||
| 2015 | 4.4 (228,614) | 6.1 (315,236) | 4.1 (213,016) | 2.7 (137,190) | 4.2 | ||
| 2016 | 4.6 (237,514) | 6.4 (328,541) | 4.2 (217,280) | 2.7 (138,767) | 4.3 | ||
| 2017 | 4.8 (249,878) | 6.7 (347,411) | 4.3 (225,459) | 2.8 (145,462) | 4.5 | ||
Prevalence of epilepsy per 1,000 persons (number of prevalent cases) as estimated by applying criteria A–D (see main text).
*Statistical significance (p<0.05).
Annual trend of prevalence
The prevalence increased every year from 2009 to 2017, regardless of the operational criteria used to identify epilepsy. The age-standardized prevalence according to criteria A also increased during that period (AAPC=3.11%, p<0.001) (Table 2). An increasing prevalence was observed for both sexes [Fig. 2B, Supplementary Table 2 (in the online-only Data Supplement)]. Annual trends showed that the prevalence was slightly decreased with each year in patients aged 0–9 years, whereas the prevalence tended to increase over the studied time period from the age of 10 years, showing a strong increase after an age of 75 years [Fig. 3B, Supplementary Table 2 (in the online-only Data Supplement)].
DISCUSSION
This study found increasing trends in both the incidence and prevalence of treated epilepsy over a 9-year period from 2009, reaching 35.4/100,000 person and 4.8/1,000 persons, respectively, in 2017, as estimated from data in the NHIS data. The incidence of epilepsy increased year on year, although this tendency was less prominent after age standardization. The increasing tendency of incidence in the elderly was prominent, while it was relatively static in the other age groups.
Cause of the increase in epilepsy
The increases in the incidence and prevalence of epilepsy in Korea reported here appear to be related to various factors. Ageing of the population is the primary reason. According to resident registration population by census, the proportion of people older than 65 years relative to the total population of Korea has gradually increased, to exceed 14% in 2017, indicating that Korea is now an aged society.15 In addition, there has been an improvement in the survival rate for people with epilepsy, which would contribute to the increasing prevalence of the disease, together with the improved survival of those with stroke and dementia. The Cardiovascular Health Study found that the prevalence of epilepsy increased from 3.7% to 5.4% during a 14-year follow-up period, and confirmed that a history of stroke was associated with a higher risk of developing epilepsy.16 Moreover, the reported prevalence of seizures in patients with dementia is high (10–22%).17 Therefore, an increase in the elderly population and an increase in those with chronic central nervous system illness could have contributed to the increases observed in both the incidence and prevalence of epilepsy in Korea.
A reduction in the treatment gap may also have contributed to the increased incidence and prevalence of treated epilepsy, as well as the actual increase in the occurrence of epilepsy.18 The treatment gap reportedly exceeds 75% in low-income countries while it is less than 10% in high-income countries, with lower rates being observed in urban areas. The treatment gap was reported to decrease over time in many countries irrespective of educational intervention, although there are currently no data on the treatment gap for epilepsy in Korea.18
Identification of epilepsy in administrative data
Several operational definitions have been used to identify individuals with epilepsy in the NHIS database. Criteria that include an anticonvulsant prescription for 180 days or more can increase specificity by excluding cases of acute symptomatic seizure and unconfirmed epilepsy under therapeutic trial conditions, but can also increase the false-negative rate by missing patients with nonadherent epilepsy and patients who died within 180 days. If the criteria include additional diagnostic codes for detecting epilepsy patients, the sensitivity increases as a result of the inclusion of more symptomatic epilepsy; however, the false-positive rate could be increased by including those who were treated for pain but who were coded as epilepsy or seizure for reimbursement. Meanwhile, if only the primary diagnosis is included (criteria D), many people with symptomatic epilepsy would be excluded. Previous reports used criteria C for 200919 and criteria D for 200720 to estimate the prevalence of epilepsy in Korea. The results of the present study demonstrate that the tendency toward increasing incidence and prevalence of epilepsy seen when applying criteria A and B, but not when applying criteria C and D suggests that the incidence and prevalence of symptomatic epilepsy are increasing, while those for primary epilepsy are stable.
Comparison with studies in other countries
The overall incidence of epilepsy in Korea (28.7–35.4/100,000 person-years) was comparable to that in other developed countries, including the United States and Europe (16–57/100,000 person-years), and Asia (24–97/100,000 person-years).21,22,23 The incidence and prevalence of epilepsy vary depending upon the study population, the method used to identify cases, and the diagnostic accuracy.11 The present study has demonstrated that the number of patients with epilepsy varies with the operational definition used to identify cases, even when using the same data source.
In this study, the incidence of epilepsy was lower in children than in the elderly. The few epidemiological studies of epilepsy in children found that the incidence was higher in developing countries than in developed countries. In addition, a community-based study in the United Kingdom found that the incidence of epilepsy appears to increase with increasing socioeconomic deprivation.24,25 The present study found a J-shaped curve for incidence according to age in 2017. A similar pattern was shown in a study conducted in the United States,14 which found that both the incidence and prevalence of epilepsy were higher in males than in females in most age groups. This is consistent with a meta-analysis finding that the epilepsy was more common in males than in females.26
Strengths and limitations of the study
This study is one of the very few to analyze the time trends of certain the epidemiological parameters of epilepsy. Moreover, this is the first to report on the incidence of epilepsy in Korea. It was an unbiased, population-based study carried out using nationwide data.
One of the limitations of this study is that it was based on administrative data. The estimations of incidence and prevalence did not include people with untreated epilepsy. The validity of the operational definitions is another potential limitation. According to a recent systematic review,27 administrative data can accurately identify people with epilepsy using operational definitions that combine disease codes with antiepileptic drugs (AEDs). In a previous Korean study using NHIS data, the positive predictive value for epilepsy identified using the criterion of one or more AED prescription with a diagnostic code representing epilepsy or seizure was 0.81 in 2009.19 Stricter criteria were used in the present study in order to increase the specificity, and several alternative criteria were tested to overcome this limitation.
Conclusions
The incidence and prevalence of epilepsy increased in Korea between 2009 and 2017. These increasing trends appear to be attributable to the increasing number of elderly and symptomatic patients with epilepsy. Accurate diagnosis and proper treatment of epilepsy in the elderly will become a more important issue in the future.
Acknowledgements
This work was supported by the Soonchunhyang University Research Fund and a grant from the Korean Neurological Association (KNA-18-MI-11).
Footnotes
- Conceptualization: Hye-Jin Moon, Seo-Young Lee.
- Data curation: Hye-Jin Moon, Ji-Ye Jeon.
- Formal analysis: Ji-Ye Jeon, Hyesung Lee, Ju-Young Shin.
- Funding acquisition: Hye-Jin Moon, Seo-Young Lee.
- Investigation: Hye-Jin Moon, Seo-Young Lee.
- Methodology: Hye-Jin Moon, Seo-Young Lee.
- Project administration: Hye-Jin Moon.
- Resources: Hye-Jin Moon, Seo-Young Lee.
- Software: Hyesung Lee, Ju-Young Shin.
- Supervision: Jae-Moon Kim.
- Validation: Hye-Jin Moon, Hyesung Lee.
- Visualization: Ji-Ye Jeon.
- Writing—original draft: Ji-Ye Jeon.
- Writing—review & editing: Hye-Jin Moon, Seo-Young Lee, Hyesung Lee.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.3988/jcn.2021.17.3.393.
Annual incidence of epilepsy according to age and sex
Annual prevalence of epilepsy according to age and sex
References
- 1.Hirtz D, Thurman DJ, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R. How common are the “common” neurologic disorders? Neurology. 2007;68:326–337. doi: 10.1212/01.wnl.0000252807.38124.a3. [DOI] [PubMed] [Google Scholar]
- 2.Ngugi AK, Bottomley C, Kleinschmidt I, Sander JW, Newton CR. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51:883–890. doi: 10.1111/j.1528-1167.2009.02481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon CS, Dykeman J, et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88:296–303. doi: 10.1212/WNL.0000000000003509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dent W, Helbok R, Matuja WB, Scheunemann S, Schmutzhard E. Prevalence of active epilepsy in a rural area in South Tanzania: a doorto-door survey. Epilepsia. 2005;46:1963–1969. doi: 10.1111/j.1528-1167.2005.00338.x. [DOI] [PubMed] [Google Scholar]
- 5.Karaagaç N, Yeni SN, Senocak M, Bozluolçay M, Savrun FK, Ozdemir H, et al. Prevalence of epilepsy in Silivri, a rural area of Turkey. Epilepsia. 1999;40:637–642. doi: 10.1111/j.1528-1157.1999.tb05567.x. [DOI] [PubMed] [Google Scholar]
- 6.Medina MT, Durón RM, Martínez L, Osorio JR, Estrada AL, Zúniga C, et al. Prevalence, incidence, and etiology of epilepsies in rural Honduras: the Salamá Study. Epilepsia. 2005;46:124–131. doi: 10.1111/j.0013-9580.2005.11704.x. [DOI] [PubMed] [Google Scholar]
- 7.Granieri E, Rosati G, Tola R, Pavoni M, Paolino E, Pinna L, et al. A descriptive study of epilepsy in the district of Copparo, Italy, 1964-1978. Epilepsia. 1983;24:502–514. doi: 10.1111/j.1528-1157.1983.tb04921.x. [DOI] [PubMed] [Google Scholar]
- 8.Kelvin EA, Hesdorffer DC, Bagiella E, Andrews H, Pedley TA, Shih TT, et al. Prevalence of self-reported epilepsy in a multiracial and multiethnic community in New York City. Epilepsy Res. 2007;77:141–150. doi: 10.1016/j.eplepsyres.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Reggio A, Failla G, Patti F, Nicoletti A, Grigoletto F, Meneghini F, et al. Prevalence of epilepsy. A door-to-door survey in the Sicilian community of Riposto. Ital J Neurol Sci. 1996;17:147–151. doi: 10.1007/BF02000846. [DOI] [PubMed] [Google Scholar]
- 10.de Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsy Behav. 2008;12:540–546. doi: 10.1016/j.yebeh.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 11.Banerjee PN, Filippi D, Allen Hauser W. The descriptive epidemiology of epilepsy-a review. Epilepsy Res. 2009;85:31–45. doi: 10.1016/j.eplepsyres.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavados J, Germain L, Morales A, Campero M, Lavados P. A descriptive study of epilepsy in the district of El Salvador, Chile, 1984–1988. Acta Neurol Scand. 1992;85:249–256. doi: 10.1111/j.1600-0404.1992.tb04040.x. [DOI] [PubMed] [Google Scholar]
- 13.Olafsson E, Hauser WA, Ludvigsson P, Gudmundsson G. Incidence of epilepsy in rural Iceland: a population-based study. Epilepsia. 1996;37:951–955. doi: 10.1111/j.1528-1157.1996.tb00532.x. [DOI] [PubMed] [Google Scholar]
- 14.Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935-1984. Epilepsia. 1993;34:453–468. doi: 10.1111/j.1528-1157.1993.tb02586.x. [DOI] [PubMed] [Google Scholar]
- 15.Korean Statistical Information Service. Entire population table of census. 2019. [accessed 2019 May 1]. Available from: http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01#SelectStatsBoxDiv.
- 16.Choi H, Pack A, Elkind MSV, Longstreth WT, Jr, Ton TGN, Onchiri F. Predictors of incident epilepsy in older adults: the Cardiovascular Health Study. Neurology. 2017;88:870–877. doi: 10.1212/WNL.0000000000003662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mendez M, Lim G. Seizures in elderly patients with dementia: epidemiology and management. Drugs Aging. 2003;20:791–803. doi: 10.2165/00002512-200320110-00001. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Epilepsy: a public health imperative. Geneva: WHO; 2019. [Google Scholar]
- 19.Lee SY, Chung SE, Kim DW, Eun SH, Kang HC, Cho YW, et al. Estimating the prevalence of treated epilepsy using administrative health data and its validity: ESSENCE study. J Clin Neurol. 2016;12:434–440. doi: 10.3988/jcn.2016.12.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee SY, Jung KY, Lee IK, Yi SD, Cho YW, Kim DW, et al. Prevalence of treated epilepsy in Korea based on National Health Insurance data. J Korean Med Sci. 2012;27:285–290. doi: 10.3346/jkms.2012.27.3.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benn EK, Hauser WA, Shih T, Leary L, Bagiella E, Dayan P, et al. Estimating the incidence of first unprovoked seizure and newly diagnosed epilepsy in the low-income urban community of Northern Manhattan, New York City. Epilepsia. 2008;49:1431–1439. doi: 10.1111/j.1528-1167.2008.01564.x. [DOI] [PubMed] [Google Scholar]
- 22.Olafsson E, Ludvigsson P, Gudmundsson G, Hesdorffer D, Kjartansson O, Hauser WA. Incidence of unprovoked seizures and epilepsy in Iceland and assessment of the epilepsy syndrome classification: a prospective study. Lancet Neurol. 2005;4:627–634. doi: 10.1016/S1474-4422(05)70172-1. [DOI] [PubMed] [Google Scholar]
- 23.Okamoto K, Fukuda M, Saito I, Horiuchi I, Okazawa T, Ishii E. Incidence of childhood epilepsy: a population-based study in rural Japan. Brain Dev. 2018;40:904–908. doi: 10.1016/j.braindev.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Cowan LD. The epidemiology of the epilepsies in children. Ment Retard Dev Disabil Res Rev. 2002;8:171–181. doi: 10.1002/mrdd.10035. [DOI] [PubMed] [Google Scholar]
- 25.Heaney DC, MacDonald BK, Everitt A, Stevenson S, Leonardi GS, Wilkinson P, et al. Socioeconomic variation in incidence of epilepsy: prospective community based study in south east England. BMJ. 2002;325:1013–1016. doi: 10.1136/bmj.325.7371.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kotsopoulos IA, van Merode T, Kessels FGH, de Krom MCTFM, Knottnerus JA. Systematic review and meta-analysis of incidence studies of epilepsy and unprovoked seizures. Epilepsia. 2002;43:1402–1409. doi: 10.1046/j.1528-1157.2002.t01-1-26901.x. [DOI] [PubMed] [Google Scholar]
- 27.Mbizvo GK, Bennett KH, Schnier C, Simpson CR, Duncan SE, Chin RFM. The accuracy of using administrative healthcare data to identify epilepsy cases: a systematic review of validation studies. Epilepsia. 2020;61:1319–1335. doi: 10.1111/epi.16547. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Annual incidence of epilepsy according to age and sex
Annual prevalence of epilepsy according to age and sex