1. BACKGROUND AND RATIONALE
Bronchiolitis is a frequent cause of hospital admission and significant mortality in developing countries. In Italy, bronchiolitis season usually begins in late October peaking in January–February.1, 2 During the SARS‐COV‐2 pandemic, containment measures and lockdowns considerably impacted respiratory infections, 3 but no data are available about the impact on bronchiolitis seasonality. Moreover, containment measures and seem to impact differently on each virus. 3 Therefore, we decided to explore this year's bronchiolitis trend, assess bronchiolitis severity and viruses involved as secondary outcomes.
2. MATERIALS AND METHODS
The study was performed at Bambino Gesù Children's Hospital, Rome; a third level pediatric hospital. We retrospectively collected clinical data of all infants (≤1 year), hospitalized between 1st September and 31th March in 2018–2019, 2019–2020, and 2020–2021 with a diagnosis of bronchiolitis confirmed by polymerase chain reaction (PCR) at nasopharyngeal aspirate. All patients up to one year of age, routinely undergo PCR aspirate at hospital admission, using Multiplex test able to detect the most commons respiratory viruses (adenovirus, influenza, parainfluenza 1–4, RSV A and B, metapneumovirus, three coronavirus, rhinovirus A/B/C, bocaparvovirus 1‐4, enterovirus). During the 2020–2021 period patients were tested for SARS‐CoV‐2 as well. By reviewing clinical records, we retrospectively collected personal and clinical data together with virological results. We assessed severity by length‐of‐stay, intensive care unit (ICU) admission; the need of ≥24 h of oxygen or other respiratory support (high flow nasal cannula, continuous positive airway pressure [CPAP], noninvasive ventilation [NIV], mechanical ventilation [MV]). We collected data on medications and administration days.
3. STATISTICAL ANALYSIS
We reported categorical variables as numbers and percentage; and continuous variables as mean and standard deviation. We compared the hospitalization timing in the current season to the same period of the two previous years with the Log‐rank test. We performed a Fisher test for continuous variables between this year RSV Season (RSV‐S) and each of the other RSV seasons considered. We performed Log‐rank‐test to compare the in‐hospital and ICU length‐of‐stay, and days of each treatment. We used a confidence interval of 95% and considered statistically significant a p ≤ .05.
4. RESULTS
Bronchiolitis hospitalizations did not occur significantly later this year compared to the previous 2 years (p = .11). Hospitalizations for bronchiolitis were considerably less (Figure 1) in 2020–2021 RSV‐S (seven patients compared to 131 in 2019–2020 and 130 in 2018–2019). All patients were infected by Rhinovirus in 2020–2021 RSV‐S but one, whereas Rhinovirus was responsible for bronchiolitis in 28 patients (21%) in 2019–2020 and 29 patients (22%) in 2018–2019. In the 2020–2021, RSV‐S up to March 31st, 2021, only one patient was infected by RSV. On the contrary, RSV accounted for 97 cases (74%) and 85 cases (65%), in the 2019–2020 and 2018–2019 RSV‐S, respectively (p = .002 and p = .01 respectively). No patients presented coinfection in 2020–2021 RSV‐S; 28 patients in 2019–2020 (18 presenting RSV plus another virus; three cases presented RSV and other two or more viruses), and 18 patients in 2018–2019 (12 presenting RSV plus another virus, three cases presented RSV, and other two or more viruses). No patients needed oxygen for ≥24 h in the 2020–2021 RSV‐S, 72 patients (55%) in the 2019–2020 RSV‐S and 51 (39%) in 2018–2019; days on oxygen were 2.5 ± 3.4 in 2019–2020 and 1.4 ± 2.4 in 2018–2019 RSV‐S. The length‐of‐stay in 2020–2021 RSV‐S (mean days 3.4 ± 1.6) was less compared to the previous two years (5.9 ± 4.2 for 2019–2020 and 4.9 ± 3.2 for 2018–2019). In 2020‐2021 RSV‐S, no bronchiolitis was admitted to ICU; 17 patients (13%) in 2019–2020 and 11 (8%) in 2018–2019. This difference was not statistically significant as well as the number of days spent in ICU. The need for respiratory supports other than oxygen (i.e., CPAP, NIV, and MV) did not statistically differ. All of the other variables considered did not statistically differ.
Figure 1.
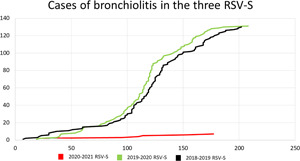
Cases of bronchiolitis admitted in the three different season's onset periods considered in the study (2020–2021 dark gray; 2019–2020 black line, and 2018–2019 light gray) [Color figure can be viewed at wileyonlinelibrary.com]
5. DISCUSSION
In 2020–2021, RSV‐S there was no delay in hospitalizations due to bronchiolitis compared to the two previous years. However, admissions due to bronchiolitis were markedly reduced (95% less). This year incidence of bronchiolitis was low and steady, whereas, in the past 2 years, peaked in the months of December‐January (Figure 1). This year only one hospitalization for RSV bronchiolitis occurred; whereas in the last year most cases were sustained by this virus, the first case of RSV was recorded on the 25th October according to the literature.1, 2 These three aspects (drastic reduction of cases, the absence of a peak of infections, and the absence of RSV bronchiolitis) suggest that bronchiolitis epidemic season was not started in 2020–2021 RSV‐S. Although the possible causes remain speculative, it seems reasonable a major role of COVID‐19 measures in reducing viral transmission. To our best concern, no data are available in the literature on COVID‐19 impact on bronchiolitis, except for a single Brazilian article based on nationwide surveillance without swab confirmed diagnosis 4 and outside the regional RSV season.1, 2
The length‐of‐stay in 2020–2021 RSV‐S was reduced as well as days on oxygen and oxygen need, suggesting a less severe disease. Such a difference in bronchiolitis severity could be, the lack of RSV infections. The presence of nearly exclusively rhinovirus infections on 2020–2021 RSV‐S, fits greatly with recent evidence reporting that rhinovirus incidence was not affected by COVID‐19 measures in school children and was reduced by physical distancing during lockdown periods. 3
The study is intended as an early communication on interesting findings that hopefully could pave the way for further studies. Our preliminary results need to be confirmed by the whole epidemic season data. It is a retrospective and monocentric study, identifying a low number of patients that might have affected study potency. Lastly, the study was conducted in Italy, the first European nation hit by the pandemic.
6. CONCLUSIONS
We registered an absence of a bronchiolitis season onset up to 31st March and a huge reduction in hospitalizations for bronchiolitis, suggesting a heavy influence of COVID‐19 containment measures on bronchiolitis epidemiology. We observed a reduction in bronchiolitis severity and an atypical virus etiology with the almost complete absence of RSV induced bronchiolitis. Finally, we confirmed that Rhinovirus seems to be less affected as already reported for older patients.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Sergio Ghirardo: conceptualization (supporting); data curation (lead); formal analysis (lead); investigation (equal); writing original draft (lead); writing review & editing (supporting). Nicola Ullmann: conceptualization (lead); supervision (equal); writing review & editing (equal). Marta Ciofi degli Atti: project administration (supporting); resources (supporting); supervision (supporting); writing review & editing (supporting). Massimiliano Raponi: project administration (supporting); supervision (supporting); writing review & editing (supporting). Renato Cutrera: conceptualization (supporting); project administration (lead); supervision (supporting); writing review & editing (supporting).
Ghirardo S, Ullmann N, Ciofi degli Atti ML, Raponi M, Cutrera R. Delayed season's onset and reduction of incidence of bronchiolitis during COVID‐19 pandemic. Pediatric Pulmonology. 2021;56:2780‐2781. 10.1002/ppul.25461
REFERENCES
- 1. Obando‐Pacheco P, Justicia‐Grande AJ, Rivero‐Calle I, et al. Respiratory syncytial virus seasonality: a global overview. J Infect Dis. 2018;217:1356‐1364. [DOI] [PubMed] [Google Scholar]
- 2. Friedrich F, Ongaratto R, Scotta MC, et al. Early impact of social distancing in response to coronavirus disease 2019 on hospitalizations for acute bronchiolitis in infants in Brazil. Clin Infect Dis. 2020:1‐5. 10.1093/cid/ciaa1458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Poole S, Brendish NJ, Tanner AR, Clark TW Physical distancing in schools for SARS‐CoV‐2 and the resurgence of rhinovirus. Lancet Respir. Med. 2020;8:e92‐e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu D, Lu J, Liu Y, Zhang Z, Luo L Positive effects of COVID‐19 control measures on influenza prevention. Int J Infect Dis. 2020;95:345‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]


