Abstract
Purpose
This study explored how patients with schizophrenia were provided with social support and treatment compliance during the pandemic.
Design and Methods
A total of 396 patients with schizophrenia and their relatives were interviewed by telephone calls.
Findings
Multiple antipsychotic use and depot antipsychotics were not superior in preventing relapse. A total of 70.2% of the patients wanted to meet with their psychiatrist online but only 7.1% of them were reached online. A total of 59% of patients were able to take their medication thanks to the extension of their drug prescriptions.
Practice Implications
Active inclusion of telepsychiatry applications in clinical practice is necessary for patients with schizophrenia. Government policies developed for treatment compliance seem important.
Keywords: antipsychotics, COVID‐19, schizophrenia, social compliance, treatment compliance
1. INTRODUCTION
A new Coronavirus type (2019‐nCoV) was identified as an etiological agent in pneumonia cases with unknown causes in Wuhan, China, on December 31, 2019. 1 The virus then spread rapidly around the world, causing the pandemic known as the Corona Virus Disease 2019 (COVID‐19).
The World Health Organization reported that 57,274,018 cases were affected in the world and 1,368,000 people have died due to the virus as of November 20, 2020. 2 The first case in Turkey was reported on March 11, 2020. Especially in the first 3 months of the pandemic, a stringent range of measures was implemented with a curfew; including not accepting patients without appointments, widening appointment intervals, symptom inquiries and fever control at hospital admissions, and testing COVID‐19 disease symptoms before interventional procedures are some of the measures in the health system.
In the pandemic, which is an unusual situation, besides being affected by the disease, problems may arise in terms of accommodation, food, and basic needs. It is expected that the mental health of people will be affected in addition to their physical health.3, 4 It has been reported that both healthcare professionals and other members of society have increased anxiety and hopelessness in the COVID‐19 pandemic. 5 The exact course of the disease is unknown, its severity and duration cannot be predicted, the lack of a definitive treatment method and the lack of vaccine create anxiety and hopelessness about the future.5, 6
In schizophrenia and other psychotic disorders (referred as schizophrenia in the rest of this manuscript), the risk of COVID‐19 is thought to increase and the disease is thought to progress more severely. Low socioeconomic level and social support, increased physical illnesses, and difficulty in accessing treatment were shown as the reasons for this increase. 7 Patients may not be able to reach their treatment centers and doctors due to restrictions, may not be able to provide their medicines and basic needs, and the risk of relapse may increase.7, 8 Moreover, it is known that stressful life events and increased anxiety level negatively affect the course of the disease and cause relapse in patients with schizophrenia. 9
So how did the COVID‐19 pandemic, which caused anxiety worldwide, affect patients with schizophrenia? Were any difficulties foreseen in the studies experienced and if so, how was the problem overcome? Although estimates have been made about how schizophrenic patients will be affected in the pandemic, we could not find a study in which patient interviews were conducted to examine how they were affected during the pandemic period, how they continued their treatment, and what the COVID‐19 prevalence was.7, 8, 10 In our study, it was aimed to determine what changes occurred in the course of their disease during the pandemic period, how they were provided with social support, treatment compliance, and which treatment increased compliance more. It is thought that the data of our study obtained through one‐to‐one interviews with patients and their relatives would be an important guide in both psychosocial and pharmacological interventions in the treatment of patients with schizophrenia in pandemics and other extraordinary situations.
2. MATERIALS AND METHOD
2.1. Ethical considerations
The study was approved by the University of Health Sciences, Ankara City Hospital Ethics Committee (numbered E1‐20‐690 and dated June 11, 2020) and was conducted according to the criteria set by the declaration of Helsinki. When the participants were called, the name of the researcher and the institution where he/she was working were given at first. It was stated right after that they were sought for a study. Knowledge of the study, all possible benefits and risks of the study were explained. The participants were included when they understood the study and verbally confirmed that they agreed to participate in the study. In addition, we could not obtain written consent because face‐to‐face interviews could not be made due to the pandemic. The forms were completed only with those who declared that they gave their consent to participate in the study.
2.2. Study design and participants
This research is a cross‐sectional study in which the scales are applied by phone calls. Patients who were followed up who had any of the diagnoses of schizophrenia (ICD10‐F20), schizoaffective disorder (ICD10‐F25), other psychotic disorder not due to a substance or known physiological condition (ICD10‐F28), and unspecified psychosis not due to a substance or known physiological condition (ICD10‐F29) in Ankara City Hospital were included in the study. The diagnoses made by the psychiatrist who monitored the patient through the clinical consultation and entered into the national health system were considered valid. According to the notes held during examinations, patients in remission within 6 months before the start of the pandemic were included in the study. Patients with a score of 3 or less according to the Clinical Global Impression (CGI)—Severity Scale, who were recorded in remission in the follow‐up notes of the patients, were accepted in remission. Noncompliance to treatment was defined as the notification of the patient's complete discontinuation of their medication for 10 consecutive days or taking less than 75% of the prescribed dose in the previous 30 days. 11
At the end of the third month of the pandemic, phone calls started on June 22, 2020 and were completed on September 22, 2020. The phone numbers of the patients were obtained from the hospital information registry system. A 20‐min phone call was made by two experienced psychiatrists, and a sociodemographic data form questions prepared previously was asked. Patients who were not in remission in the 6 months before the pandemic started, who were hospitalized in a psychiatry clinic, patients with comorbid organic mental disorders, or intellectual disability were excluded from the study. In the telephone interviews, relapse was defined as 1 week with recurrence of at least one positive symptom according to the Positive and Negative Syndrome Scale and a CGI of 4 or more.
A total of 941 patients were followed up in our outpatient unit with the specified diagnoses within 6 months and 396 people who agreed to participate in the study were interviewed. The flow chart of the patients included in the study is shown in Figure 1.
Figure 1.
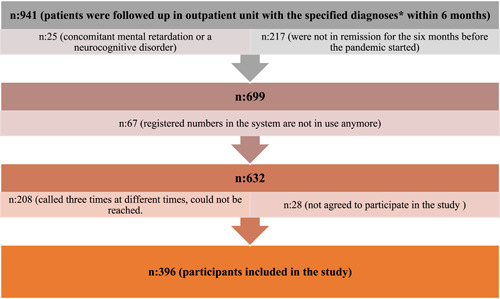
Flow chart of participants included in the study. n: number of persons [Color figure can be viewed at wileyonlinelibrary.com]
2.3. Measurement tools
During the telephone interviews, sociodemographic data were collected from the participants, including the following information: the patient's age, marital status, education level, the place where he or she is living before the pandemic and currently, the treatment s/he used, how s/he continued his/her treatment during the pandemic, whether s/he was infected by COVID‐19, how s/he accessed his/her doctor, and whether s/he wanted to meet with their doctor through telepsychiatry applications.
2.4. Statistical evaluation of data
The Kolmogorov–Smirnov test was used to check the compliance of variables to normal distribution. For the variables showing normal distribution, the Student t test was used in two independent group comparisons. The relationship between categorical variables was tested using χ 2 analysis. Binary logistic regression analysis was used to evaluate the factors affecting psychotic exacerbation. Average ± SD deviation values were given as introductory statistics. The SPSS for Windows version 22.0 package program was used for statistical analysis and p < 0.05 was considered statistically significant.
3. RESULTS
A total of the 396 patients participating in the study, 247 (62.4%) were men and 149 (37.6%) were women. The mean age was 41.7 ± 10.9, and the mean education duration were 10.1 ± 4.3 years.
With the pandemic curfew, 383 (96.7%) patients could continue to meet their basic needs, while 13 (3.3%) patients could not. A total of 162 of them (42.5%) continued to meet their needs themselves, 191 (50.1%) were provided by their families, 23 (6.0%) were provided by their families and themselves. Only a few had (n: 5, 1.3%) their basic needs provided by their friends or neighbors.
A total of 63 (15.9%) of the patients were in relapse. A total of 52 (13.7%) of the patients in relapse and 326 (86.3%) in remission were compliant to treatment, and this relationship between treatment compliance and relapse was statistically significant (p < 0.001; χ 2: 20.121). A total of 16 (15.1%) of 106 patients who continued their outpatient controls after the pandemic started and 47 (16.3%) of 289 patients who did not go to their outpatient visits were in relapse. There was no statistically significant difference between going to outpatient visits and relapse (p: 0.779; χ 2: 0.79). The comparison of the patients with schizophrenia in relapse and remission in terms of sociodemographic variables and psychotropics use is given in Table 1.
Table 1.
Comparison of patients with schizophrenia in relapse and remission in terms of sociodemographic variables and psychotropic use
| Patients in relapse (n: 63) | Patients in remission (n: 333) | Total (n: 396) | Statistical analysisa | |
|---|---|---|---|---|
| Gender | ||||
| Female | 20 (13.4%) | 129 (86.6%) | 149 | p: 0.286 |
| Male | 43 (17.4%) | 204 (82.6%) | 247 | χ 2: 1.139 |
| Marital status | ||||
| Single | 37 (16.5%) | 187 (83.5%) | 224 | |
| Married | 18 (14.9%) | 103 (85.1%) | 121 | p: 0.232 |
| Widow/divorced | 8 (15.7%) | 43 (84.3%) | 51 | χ 2: 5.586 |
| Age (mean ± SD) | 41.3±10.3 | 41.8±11.0 | 41.7 ±10.9 | p: 0754 |
| t: −0.313 | ||||
| Education years (mean ± SD) | 10.1±3.9 | 10.1±4.4 | 10.1±4.3 | p: 0.904 |
| t: −0.120 | ||||
| Working status | ||||
| Employment | 17 (16.8%) | 84 (83.2%) | 101 | p: 0.399 |
| Unemployment | 46 (15.6%) | 249 (84.4%) | 295 | χ 2: 1.835 |
| Living place | ||||
| Alone | 2 (6.5%) | 29 (93.5%) | 31 | p: 0.237 |
| Spouse/children | 22 (16.1%) | 115 (83.9%) | 137 | χ 2: 4.239 |
| Mother/father/siblings | 35 (16.3%) | 180 (83.7) | 215 | |
| Other | 4 (30.8%) | 9 (69.2%) | 13 | |
| Change in living order | ||||
| Yes | 1 (8.3%) | 11 (91.7%) | 12 | p: 0.694 |
| No | 62 (16.1%) | 322 (83.9%) | 384 | χ 2: 0.731 |
| Access to basic needs | ||||
| Yes | 59 (15.3%) | 324 (84.7%) | 383 | p: 0.138 |
| No | 4 (%30.8) | 9 (69.2%) | 13 | χ 2: 2.202 |
| How to reach basic needs? | ||||
| Himself | 23 (14.2%) | 139 (85.8%) | 162 | |
| Family | 29 (15.3%) | 161 (84.7%) | 190 | p: 0.520 |
| Himself and his family | 6 (26.1%) | 17 (73.9%) | 23 | χ 2: 2.260 |
| Neighbor/relative | 1 (20.0%) | 4 (80.0%) | 5 | |
| Depot antipsychotic use | ||||
| Yes | 21 (16.3%) | 108 (83.7%) | 129 | p: 0.864 |
| No | 42 (15.7%) | 225 (84.3%) | 267 | χ 2: 0.029 |
| Multiple antipsychotic use | ||||
| Yes | 20 (13.1%) | 133 (86.9%) | 153 | p: 0.214 |
| No | 43 (17.7%) | 200 (82.3%) | 243 | χ 2: 1.542 |
| Use of clozapine | ||||
| Yes | 11 (16.4%) | 56 (83.6%) | 67 | p: 0.908 |
| No | 52 (15.8%) | 277 (84.2%) | 329 | χ 2: 0.013 |
| Treatment compliance | ||||
| Yes | 52 (13.7%) | 326 (86.3%) | 378 | p < 0.001 |
| No | 11 (61.1%) | 7 (38.9%) | 18 | χ 2: 20.121 |
| Outpatient control | ||||
| Yes | 16 (15.1%) | 91 (84.9%) | 107 | p: 0.779 |
| No | 47 (16.3%) | 242 (83.7%) | 289 | χ 2: 0.079 |
| Phone call by the institution | ||||
| Yes | 5 (17.9%) | 23 (82.1%) | 28 | p: 0.874 |
| No | 58 (15.8%) | 310 (84.2%) | 368 | χ 2:0.269 |
Note: n: Number of persons; %: percent.
The χ 2 test was used for categorical variables, if the assumptions are not met, Fisher's Exact test was used, the Student t test was used for continuous variables.
When the treatments used by the patients were evaluated, the average number of patient psychotropic use was 1.59 ± 0.71 (min: 1, max: 4). It was found that 129 (32.6%) patients used depot antipsychotic treatment, and 125 (96.9%) of them could continue depot medication in the pandemic. It was found that 244 (61.6%) of the patients used a single psychotropic, 152 (38.4%) of them used two or more psychotropics together. A total of 86 (21.7%) patients had at least two antipsychotics together, 35 (8.8%) patients had antipsychotic and antidepressants together, 29 (7.3%) patients had antipsychotic and a mood stabilizers together, and 2 (0.5%) patients had both antipsychotic, antidepressant and mood stabilizer together. The oral and depot antipsychotics used by the patients and the most commonly used antipsychotic combination types are shown in Table 2.
Table 2.
Oral and depot antipsychotics and the most commonly used antipsychotic combinations in patients with schizophrenia
| Oral antipsychotic drugs | n: 396 |
|---|---|
| Olanzapine | 96 |
| Quetiapine | 74 |
| Clozapine | 67 |
| Aripiprazole | 62 |
| Risperidone | 58 |
| Amisulpride | 26 |
| Paliperidone | 18 |
| Haloperidol | 15 |
| Depot antipsychotic drugs | n: 129 |
| Paliperidone palmitate | 52 (40.3%) |
| Long‐acting injectable risperidone | 46 (35.6%) |
| Depot aripiprazole | 16 (12.4%) |
| Zuclopentixol decanoate | 11 (8.6%) |
| Flupenthixol Decanoate | 3 (2.3%) |
| Haloperidol decanoate | 1 (0.8%) |
| The most commonly used antipsychotic drug combinations | n: 86 |
| Risperidone‐quetiapine | 8 (9.3%) |
| Olanzapine‐aripiprazole | 8 (9.3%) |
| Olanzapine‐long acting injectable risperidone | 6 (7.0%) |
| Clozapine‐long acting injectable risperidone | 5 (5.9%) |
| Quetiapine‐amisulpride | 4 (4.7%) |
| Amisulpride‐Clozapine | 4 (4.7%) |
| Olanzapine‐paliperidone palmitate | 4 (4.7%) |
| Quetiapine‐paliperidone palmitate | 4 (4.7%) |
| Risperidone‐olanzapine | 3 (3.4%) |
| Quetiapine‐aripiprazole | 3 (3.4%) |
| Quetiapine‐long acting injectable risperidone | 3 (3.4%) |
| Others | 34 (39.5%) |
Note: n: Number of persons; %: percent.
It was found that 21 patients (16.3%) who used an antipsychotic depot treatment had a relapse in their disease, 42 patients (15.7%) who did not use depot therapy had a relapse, and there was no statistically significant difference between the two groups (p: 0.899; χ 2: 0.020).
It was found that 107 (23.0%) of the patients were able to go to outpatient visits during the pandemic, 289 (73.0%) could not, and the most common reason for not going to controls was the anxiety of contracting COVID‐19 (n: 215, 74.5%). It was determined that 27 (9.4%) patients wanted to go to controls but could not find an available appointment, 26 (9.0%) patients did not need to go to controls, and 10 (3.5%) patients could not go to controls due to the curfew. It was found that only 15 (22.4%) of the 67 patients using clozapine could go to hospital for a complete blood count, 52 (77.6%) could not, and 25 (75.8%) of 33 patients using valproic acid could not go to hospital for drug level monitoring.
A total of 378 (95.5%) of the patients were treatment compliant and 18 patients were noncompliant. It was found that 225 (59.5%) of the 378 treatment compliant patients were able to take their medicines directly from the pharmacy without the need for a prescription. The way for patients obtained their medicines during the pandemic period is shown in Figure 2.
Figure 2.
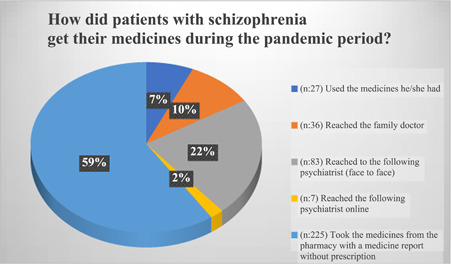
How did patients with schizophrenia get their medicines during the pandemic period? n: number of persons; %: percent [Color figure can be viewed at wileyonlinelibrary.com]
It was found that 13 (15.1%) of the 86 people with multiple antipsychotic use and 7 (10.6%) of the 66 people using other psychotropic combinations were in relapse, and there was no statistically significant difference between the two groups in terms of the type of combination and relapse (p: 0.415; χ 2: 0.665). There was no significant difference in terms of relapse between the use of a single and combined usage of antipsychotics (p: 0.214; χ 2: 1.542).
In separate comparisons of clozapine (p: 0.908; χ 2: 0.013), olanzapine (p: 0.420; χ 2: 1.002), quetiapine (p: 0.820; χ2: 0.052), aripiprazole (p: 0.406; χ 2: 0.692), paliperidone (p: 0.892; χ 2: 0.019) and risperidone (p: 0.120; χ 2: 2.412), no relationship was found between the type of antipsychotic used and relapse.
In the binary logistic regression model, in which relapse is a dependent variable, a meaningful model could not be created with variables such as meeting basic needs, marital status, years of education, age, gender, use of depot medication, single or multiple antipsychotic use, number of psychotropics used, and whether or not it patients attended outpatient controls (p: 0.924; χ 2: 3.804 in the omnibus test).
It was found that only 2 (0.5%) of the 396 people participating in the study were diagnosed with COVID‐19, one person was monitored at home, and one person was hospitalized. It was found that both people could continue their medication regularly during the period when they were being monitored with COVID‐19.
It was determined that 28 (7.1%) of the participants were called for controls during the pandemic period by the hospital where they were monitored. Most patients (n: 278, 70.2%) reported that they would want to see their psychiatrist if they had an online session.
4. DISCUSSION
Our study is a cross‐sectional study in which the system records were retrospectively examined, and the current conditions of the patients were evaluated by phone calls.
In follow‐up studies with patients with schizophrenia, 1‐year relapse rates were reported to be 37.0%. 12 In a comprehensive review including 4365 patients evaluated in 66 studies, the relapse rate was found to be 16% in patients who continued antipsychotic medication during the 9.7‐month follow‐up period, while the mean cumulative relapse rate in patients who stopped using the medicines was 53%. 13 In the same study, younger age, higher antipsychotic dose and shorter length of hospitalization were found to be associated with relapse. In our study, the relapse rate was 13.7% in treatment compliant patients, while it was 61.1% in noncompliant patients. Consistent with other studies in the literature, relapse was found to be low in patients with high treatment compliance. However, the fact that a large group of patients in our study was treatment compliant reduces the strength of this statistical significance.
It was determined that variables such as antipsychotic‐related characteristics, age, gender, marital status, and employment status were not predictors of relapse. In a study examining the relationship between relapse and antipsychotics in patients with schizophrenia and evaluating 11 oral antipsychotics, olanzapine was reported to be the most effective antipsychotic in preventing relapse. 14 In our study, no superiority of olanzapine in preventing relapse compared to other atypical antipsychotics was found. In a comprehensive meta‐analysis involving 6493 patients, the use of first‐generation or second‐generation antipsychotics was not associated with relapse, and depot antipsychotics, especially typical antipsychotic depot options, were more advantageous than oral antipsychotics in preventing relapse. 15 It was stated that characteristics such as disease duration, duration of remission before relapse, and number of episodes, which are among the variables associated with the disease, did not predict relapse. In another meta‐analysis, typical depot antipsychotics were reported to be superior in preventing relapse compared to oral antipsychotics. 16 In our study, depot antipsychotics were not found to prevent relapse compared to using oral antipsychotics. In our study, the use of typical depot antipsychotics is rare and most of the patients continued oral treatment. This may be the cause of no difference being found in terms of relapse. On the other hand, as in the previous discussions in the literature, antipsychotics may not have an advantage over each other in preventing relapse. 17 In our study, atypical antipsychotics were used in most of the patients and no antipsychotic, including clozapine, was found superior to the others in terms of relapse. The limited number of samples in our study and the short follow‐up period may be the reason for this similarity between antipsychotics. In the future, conducting studies with longer monitoring in this period when the effects of the pandemic gradually increase and with a wider patient population may be useful in detecting these differences.
A study found that 52.5% of the patients with schizophrenia were fully treatment compliant, 39.3% (n: 24) were partially compliant, and only 8.2% (n: 5) were noncompliant. 18 It was emphasized that patients' subjective attitudes and concerns about their illnesses and medications are important in treatment compliance. To increase treatment compliance in patients with schizophrenia, it has been recommended that patients and their relatives be included in the treatment decision‐making process. The fact that the majority of the patients with schizophrenia included in our study did not live alone, met their needs during the pandemic and that half of them had the support of their families over the telephone made us think that their social support was good, and this was interpreted to have possibly increased treatment compliance.
In the COVID‐19 pandemic, it is not difficult to think that patients with schizophrenia will have difficulty in accessing their doctors. In such a period, the use of depot antipsychotics that do not require frequent medicine prescriptions can be considered as an advantage. However, our data found that depot antipsychotic use is not superior in preventing relapse; this is an important piece of information in the transition from predictions to evidence‐based clinical practices. The importance of factors such as inclusion of patients in the treatment, providing social support and being contacted by the center where they are monitored, are increasing in the pandemic period and help in maintaining treatment compliance for patients.
In a meta‐analysis conducted by Matsui et al., 19 it was reported that there was no difference in terms of relapse between patients who continued to use multiple antipsychotics and patients who switched from multiple antipsychotics to a single antipsychotic. In a cohort study, antipsychotic combinations, other than a combination of clozapine and aripiprazole, was not found to have any advantage over monotherapy in preventing rehospitalization. 20 In another study, the combination of antipsychotics was not found to be superior to monotherapy in ensuring treatment compliance and preventing rehospitalization. 21 In our study, the use of single or multiple antipsychotics, and the combined use of antipsychotics and other psychotropics were not associated with relapse. Other disease‐related characteristics of the patients, such as disease severity, duration, and number of hospitalizations, could not be examined in our study. The reason for the similarity between the groups may be the absence of these variables. On the other hand, it was found that 37 different antipsychotic combinations were used in patients with schizophrenia. This situation reflects the wide spectrum of schizophrenia and the difficulties experienced by clinicians in its treatment.
The reporting periods of medicines used by those with chronic diseases were extended with a decision taken by the Ministry of Health during the COVID‐19 pandemic period. In our study, it was found that more than half of the patients with schizophrenia were able to obtain their medications without the need for a prescription. This is thought to be important in increasing treatment compliance. This situation shows us that pandemic management requires a multidisciplinary approach of the health system and state policies. The importance of making arrangements regarding the health system has also been seen in another place. It was observed that most of the patients (77.6%) using clozapine could not have a blood count during the pandemic period. Patients stated that they could not come to the hospital because they could not find an appointment and therefore they could not have a routine complete blood count. Here, the importance of the family medicine system becomes more evident. It seems important that patients who use regular medication and need to be monitored for drug‐related blood parameters should be monitored and searched by physicians and nurses in places where primary healthcare services are provided. In this way, these patients will continue to be followed up in cases where their important medical conditions cannot reach psychiatrists.
In the COVID‐19 period, online consultations with people with chronic psychiatric diseases are recommended in the literature. 22 It may be possible to evaluate mental state, to arrange medication, and to refer patients to hospital when necessary by online interviews with patients. Despite these suggestions, it was determined that a very small portion of the patients (7.1%) were reached online in our study. An important question here is how much patients with schizophrenia will want this? Or would the online conversation be a source of stress for them? For a psychosis patient, being called may be uncomfortable or may not want to continue the phone call. And even though we had ethical approval, we had thought to terminate the study in accordance with the principle of patient benefit, if they had a situation where they would feel uncomfortable. However, many patients were very pleased to be “remembered” and “wondered how they were,” instead of being uncomfortable. This is also seen in the results of the study. It was found that 70.2% of the patients stated that they would want to continue their follow‐up with the psychiatrist if they had the opportunity to meet online. The fact that a therapeutic relationship has been established with the institution before may have provided the trust of the patients. If it was the first time that they were called from a hospital or clinic they did not know, it might bother them. For this reason, it may be more advantageous to follow‐up online with patients with whom a therapeutic relationship has been established face‐to‐face.
It would be appropriate to start clinical practice for online interviews with patients with schizophrenia. In future studies, treatment compliance and relapse rates of patients who are followed up online and patients who are not monitored can be evaluated, and the effectiveness of these interviews can be investigated.
In our study, only two patients were treated for COVID‐19. The fact that the study was conducted within the first 3 months of the COVID‐19 pandemic may be a reason for this situation. The number of COVID‐19 cases are increasing in our country, Ankara is especially reported to be one of the most affected provinces. 23 The fact that patients were sought during the period when strict measures were applied may have led us to find that so few people were infected. Since no study could be found evaluating the prevalence of COVID‐19 in patients with schizophrenia, no comparison could be made with the literature. Determining the prevalence of schizophrenia in the population sample seems important to reach scientific data from estimates. Therefore, studies in this area are needed.
In conclusion, it was observed that the majority of patients with schizophrenia continued their pharmacological treatment in the pandemic, could meet their basic needs, and there was no major change in their family lifestyle. The majority of patients requested telemedicine applications, and it seems important to start clinical practices in this area. It was found that relapse was not associated with antipsychotic type, oral or depot antipsychotic use, and single or multiple antipsychotic use. Government policies planned for medicine supply seem to be quite important. It is thought that the data of our study will be a guide in reaching scientific data from estimates with longer follow‐up studies on how patients with schizophrenia are affected in the coming days when the second wave of the pandemic is expected.
5. IMPLICATIONS FOR PSYCHIATRIC NURSING PRACTICE
Schizophrenia is a chronic disease that still requires great progress in its treatment. There is an important body of literature regarding the provision of social adaptation and rehabilitation as well as the drug treatment to be chosen in the treatment of schizophrenia. With this study, it was seen that patients wanted to continue to communicate with the center they were being monitored with online applications under these extraordinary conditions. In addition, many of them received medication thanks to extended medication reports. Nurses, social workers, psychologists and psychiatrists, who work in community mental health centers to increase treatment compliance and social adaptation, should work together and follow‐up patients under pandemic conditions. It is clear that nurses, with whom patients establish and maintain an important relationship, have a great role in this follow‐up. In developing mental health‐based government policies, it is important that professionals working in the field of mental health take a role in determining the needs and developing policies in increasing the qualities of mental health services.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Kahve AC, Kaya H, Darben Y, Gul Cakil A, Goka E. From predictions to evidence: treatment compliance, disease progression and social compliance of patients with schizophrenia in the COVID‐19 pandemic. Perspect Psychiatr Care. 2021;57:1991‐1998. 10.1111/ppc.12824
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions.
REFERENCES
- 1. Zhu N, Zhang D, Wang W, et al. China novel coronavirus research: a novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO . Coronavirus disease (COVID‐19) Situation Report Available at: https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19-20-november-2020 Accessed November 24, 2020.
- 3. Rajkumar RP. COVID‐19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gao, J , Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID‐19 outbreak. PLoS One. 2020;15(4) e0231924. 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hacimusalar Y, Kahve AC, Yasar AB, Aydin MS. Effects of coronavirus disease 2019 (COVID‐19) pandemic on anxiety and hopelessness levels: a cross‐sectional study in healthcare workers and community sample in Turkey. J Psychiatr Res. 2020;129:181‐188. 10.1016/j.jpsychires.2020.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fiorillo A, Gorwood P. The consequences of the COVID‐19 pandemic on mental health and implications for clinical practice. European Psychiary. 2020;63(1):32. 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kozloff N, Mulsant B, Stergiopoulos V, Voineskos A. The COVID‐19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr Bull. 2020;46(4):752‐757. 10.1093/schbul/sbaa051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fonseca L, Diniz E, Mendonca G, Malinowski F, Mari J, Gadelha A. Schizophrenia and COVID‐19: risks and recommendations. Brazilian J Psychiatr. 2020;42(3):236‐238. 10.1590/1516-4446-2020-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mayo D, Corey S, Kelly LH, et al. The role of trauma and stressful life events among individuals at clinical high risk for psychosis: a review. Front Psychiatry. 2017;8:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ifteni P, Dima L, Teodorescu A. Long‐acting injectable antipsychotics treatment during COVID‐19 pandemic–a new challenge. Schizophrenia Res. 2020;220(220):265‐266. 10.1016/j.schres.2020.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ucok A, Çıkrıkçılı U, Ergül C, et al. Correlates of clozapine use after a first episode of schizophrenia: results from a long‐term prospective study. CNS Drugs. 2016;30(10):997‐1006. 10.1007/s40263-016-0358-z [DOI] [PubMed] [Google Scholar]
- 12. Godin O, Leboyer M, Schürhoff F, et al. Metabolic syndrome and illness severity predict relapse at 1‐year follow‐up in schizophrenia. J Clin Psychiatry. 2018;79(6):17m12007. 10.4088/JCP.17m12007 [DOI] [PubMed] [Google Scholar]
- 13. Gilbert PL, Harris MJ, McAdams LA, Jeste DV. Neuroleptic withdrawal in schizophrenic patients: a review of the literature. Archieves of General Psychiatry. 1995;52(3):173‐188. 10.1001/archpsyc.1995.03950150005001 [DOI] [PubMed] [Google Scholar]
- 14. Lin, L , Zhao YJ, Zhou HJ, et al. Comparative cost‐effectiveness of 11 oral antipsychotics for relapse prevention in schizophrenia within Singapore using effectiveness estimates from a network meta‐analysis. Int Clin Psychopharmacol. 2016;31(2):84‐92. 10.1097/YIC.0000000000000111 [DOI] [PubMed] [Google Scholar]
- 15. Leucht S, Tardy M, Komossa K, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta‐analysis. The Lancet. 2012;379(9831):2063‐2071. 10.1016/S0140-6736(12)60239-6 [DOI] [PubMed] [Google Scholar]
- 16. Kishimoto T, Robenzadeh A, Leucht C, et al. Long‐acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta‐analysis of randomized trials. Schizophr Bull. 2014;40(1):192‐213. 10.1093/schbul/sbs150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kishimoto T, Hagi K, Nitta M, Kane JM, Correll CU Long‐term effectiveness of oral second‐generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta‐analysis of direct head‐to‐head comparisons. World Psychiatry. 2019;18(2):208‐224. 10.1002/wps.20632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rettenbacher M, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patients' attitudes toward the illness and medication. J Clin Psychiatry. 2004;65(9):1211‐1218. 10.4088/JCP.v65n0908 [DOI] [PubMed] [Google Scholar]
- 19. Matsui K, Tokumasu T, Takekita Y, et al. Switching to antipsychotic monotherapy vs. staying on antipsychotic polypharmacy in schizophrenia: a systematic review and meta‐analysis. Schizophrenia Res. 2019;209:50‐57. [DOI] [PubMed] [Google Scholar]
- 20. Tiihonen J, Taipale H, Mehtälä J, Vattulainen P, Correll CU, Tanskanen A. Association of antipsychotic polypharmacy vs monotherapy with psychiatric rehospitalization among adults with schizophrenia. JAMA Psychiatry. 2019;76(5):499‐507. 10.1001/jamapsychiatry.2018.4320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kahve AC, Kaya H, Çakıl AG, et al. Multiple antipsychotics use in patients with schizophrenia: Why do we use it, what are the results from patient follow‐ups? Asian J Psychiatr. 2020;52:102063. 10.1016/j.ajp.2020.102063 [DOI] [PubMed] [Google Scholar]
- 22. Ramalho R, Adiukwu F, Gashi Bytyçi D, et al. Telepsychiatry and healthcare access inequities during the COVID‐19 pandemic. Asian J Psychiatr. 2020;53:102234. 10.1016/j.ajp.2020.102234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Republic of Turkey, Ministry of Health . Available at: https://covid19.saglik.gov.tr/TR-68443/covid-19-durum-raporu.html. Accessed September 27, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy/ethical restrictions.


