Abstract
Aim
To assess the impact of the coronavirus disease 2019 (COVID‐19) outbreak on pediatric emergency department (ED) visits for acute bronchiolitis during the epidemic season.
Methods
A retrospective analytical cross‐sectional study was performed in our hospital, analyzing medical charts of all children under 2 years of age with a diagnosis of acute bronchiolitis admitted to our ED in the last years. Demographics and clinical data of patients affected with acute bronchiolitis during the 2020–2021 season—COVID‐19 outbreak—were compared to those of the 5 previous years.
Results
We observed an average drop of 84% of the rate of acute bronchiolitis managed by pediatricians in ED in 2020–2021 compared with bronchiolitis seasons of 5 previous years. We also reported, during the COVID‐19 outbreak, a higher number of children affected by acute bronchiolitis referred to ED as Emergency Consultations who required hospitalization. Regarding etiological agents, no differences in respiratory virus circulation, especially RSV, were observed in the two groups.
The multivariate analysis showed no correlation between the diagnosis of RSV bronchiolitis and COVID‐19 period or prematurity; lower age was associated with an increased likelihood of exhibiting RSV bronchiolitis (odds ratio 0.9; 95% confidence interval 0.86–0.95 p < .01).
Conclusion
Our data emphasize the reduction in the rate of admission to pediatric ED for acute bronchiolitis during the COVID‐19 outbreak, regardless of changes in circulating respiratory viruses. Therefore we want to highlight the importance of nonpharmacological preventive hygiene measures that should be maintained even at the end of the COVID‐19 outbreak.
Keywords: bronchiolitis, children, COVID‐19, Emergency Department, outbreak
1. INTRODUCTION
Bronchiolitis is the most common acute infection of the lower respiratory tract in children under 2 years of age. 1 It affects around 1%–3% of all healthy children 2 and is a major cause of hospitalization during the epidemic season. Respiratory syncytial virus (RSV) is the most frequent pathogen involved, followed by other viruses such as rhinovirus, metapneumovirus, seasonal coronavirus, human bocavirus, (para) influenza, and adenovirus. 3
Every year, between September and March, pediatric hospitals in Italy note a large number of children affected by acute bronchiolitis. As with other infections, viruses that can cause bronchiolitis are transmitted through air droplets and aerosols and by direct or indirect contact with contaminated objects or surfaces. 2
As of December 2019, a new virus severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has spread worldwide, quickly resulting in a pandemic 4 and different personal protective equipment have been adopted in all hospitals to prevent its circulation. 5 SARS‐CoV‐2 causes severe bilateral pneumonia in adult patients, which often require hospitalization in the intensive care setting and can rapidly lead to death. Otherwise, children have a lower incidence of this infection and milder clinical manifestations than adults; this could be due to specific phenotypic and functional characteristics of their immune system. 6 However, recently, cases of severe multisystem inflammatory syndrome (MIS‐C) 7 and long‐term coronavirus disease (COVID) effects were described in children. 8
Since the beginning of the COVID‐19 outbreak, numerous socio‐sanitary measures have been adopted to reduce the spread of the virus: stay‐at‐home orders, social distancing, and nonpharmaceutical interventions, such as the use of face masks and hands hygiene. 9 These measures helped to contain the outbreak of SARS‐CoV‐2 but have also influenced the transmission of other respiratory viruses. 9
The aim of this study was to describe the rate of acute bronchiolitis in children admitted to the pediatric emergency department (ED) since the beginning of the pandemic, comparing these data with those of 5 previous years.
2. PATIENTS AND METHODS
We conducted a retrospective analytical cross‐sectional study in a University Third‐Level Hospital in Rome (Italy) with annual attendance at the pediatric Emergency Department (ED) of about 15,000 patients from 1 month to 18 years of age.
In our country, parents can bring their children to ED freely, without a referral from their pediatrician.
Patients were identified from the electronic hospital's information system used in the ED (Gipse®) by searching for the keywords “bronchiolitis” and “acute respiratory failure” for all patients under 2 years admitted to the ED.
We excluded children with mild upper airway infections (rhinitis and pharyngitis), children over 2 years of age with other respiratory infections such as bronchitis or pneumonia, and those with other infectious diseases (gastroenteritis, encephalitis, meningitis, otitis, mononucleosis, etc.).
Data were collected by pediatric specialists and included some information from the enrolled patients, such as age, sex, triage color code, pediatric clinical history (prematurity and other comorbidities), and outcome.
The triage color codes, assigned to the patients by the triage nurse basing on the child's general conditions, symptoms, and vital signs, were: “red code” for emergency care, “yellow code” for high priority care, and “green code” for low priority care.
We analyzed data of all children with a diagnosis of bronchiolitis admitted to our Pediatric ED from the start of the COVID‐19 outbreak, February 2020–February 2021. These data were subsequently compared with that observed in the same period in the previous 5 years.
In the group of hospitalized patients, we also analyzed microbiological data, especially the polymerase chain reaction for the identification of SARS‐CoV‐2 or other viruses on nasopharyngeal swabs.
This study protocol was approved by the Institutional Review Board and Medical Ethics Committee of our institution.
2.1. Statistical analysis
Categorical variables are reported as counts and percentages. Not normally distributed continuous variables are reported as median and interquartile ranges (IQR). Statistical comparisons between groups were obtained by χ 2 tests for categorical variables and Mann–Whitney U test for continuous variables. The incidence rate was obtained by dividing the number of cases of bronchiolitis by the number of visits to the ED during the COVID‐19 outbreak and other years. A multivariate logistic regression model was used to evaluate which determinants were independently associated with the diagnosis of RSV Bronchiolitis. Logistic regression results are reported as odds ratio (OR) (95% confidence intervals). A two‐sided p values less than .05 was considered statistically significant. All data analyses were performed using the Statistical Package for the Social Sciences (version 25.0).
3. RESULTS
The number of admissions to the pediatric ED of our hospital in 2020, during the COVID‐19 outbreak, was 7.873 children, compared with a median of 13,488 per year in the previous 5 years. This corresponds to a reduction of 42% of the number of total visits to our pediatric ED.
Analyzing specifically the cases of acute bronchiolitis managed by pediatricians in ED, we observed 33 cases in the COVID‐19 period compared to 1045 in the previous 5 years, which corresponds to a reduction of 84% in the rate of bronchiolitis admitted to ED (Figure 1). This is a very important observation, given that bronchiolitis is one of the main viral infectious diseases in childhood during the epidemic season.
Figure 1.
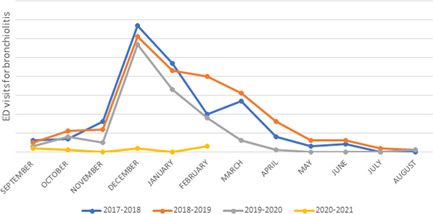
Monthly distribution visits for acute bronchiolitis in children admitted to our emergency department; season 2017–2021 [Color figure can be viewed at wileyonlinelibrary.com]
Afterward, we compared the demographic and clinical data of patients affected by acute bronchiolitis referred to our ED in 2020–2021 season versus 5 previous years.
Among the 33 children with bronchiolitis admitted to ED during the COVID‐19 outbreak, 24 (72.7%) were male and the median age was 4 months (IQR 2.5–7). When comparing the 2020–2021 season to 5 previous years no major differences were found with regard to gender, prematurity, other comorbidities, and age of admission (Table 1).
Table 1.
Demographics and clinical features, triage codes, and outcome of children admitted to ED during the COVID‐19 outbreak compared to the previous 5 years
| 2015–2019 years no. (%) | Median (IQR) | COVID‐19 outbreak no. (%) | Median (IQR) | p value | |
|---|---|---|---|---|---|
| Total number of patients to ED | 67,440 | 7873 | / | ||
| Total number of bronchiolitis | 1045 (1.5) | 33 (0.41) | <.01 | ||
| Gender (M) | 619 (59.2) | 24 (72.7) | .12 | ||
| Age in months (median‐IQR) | 4 (2‐8) | 4 (2.5–7) | .75 | ||
| Prematurity | 106 (10.3) | 5 (15.6) | .32 | ||
| Other comorbidity | 39 (3.8) | 3 (9.4) | .11 | ||
| Urgency (Triage code) | <.01 | ||||
| Emergency consultations (red code) | 50 (4.9) | 6 (18.2) | |||
| High priority consultations (yellow code) | 398 (38.8) | 16 (48.5) | |||
| Low priority consultations (green code) | 577 (56.3) | 11 (33.3) | |||
| Hospitalization | 347 (33.2) | 13 (39.4) | .45 | ||
| PICU | 80 (23.3) | 0 (0) | <.05 | ||
| Ward | 263 (76.7) | 13 (100) | |||
| RSV Bronchiolitis | 171 (49.7) | 6 (46.2) | .8 |
Abbreviations: COVID‐19, coronavirus disease 2019; ED, emergency department; IQR, interquartile range; PICU, pediatric intensive care units; RSV, respiratory syncytial virus.
As regards the triage color code assigned to the patient on admission to the ED, important differences emerged. During the 2020–2021 season—COVID‐19 outbreak—we recorded a higher number of children with acute bronchiolitis admitted as Emergency and High Priority Consultations compared to the 5 previous years (18.2% vs. 4.9% for Emergency Consultations, 48.5% vs. 38.8% for High Priority Consultations, p value < .05). In the same time, we observed a reduction of the number of bronchiolitis admitted to ED as Low Priority Consultations (33.3% vs. 56.3%).
Concerning the rate of hospitalization for acute bronchiolitis in the 2020–2021 season vs 5 previous years, no significant differences were observed: 39.4% of children in the 2020–2021 season required hospitalization compared to 33.2% of 5 previous years (p = .45). Instead, significant differences were observed in the rate of admission to pediatric intensive care units (PICU): during the COVID‐19 outbreak no patient required hospitalization to PICU compared with 4.7% of the 5 previous years (p < .05). This could be related to the total reduction in the number of acute bronchiolitis admitted to ED.
Regarding microbiological data, since the start of the outbreak, we have not detected any positive nasopharyngeal swabs for SARS‐CoV‐2 in children with acute bronchiolitis. Among 1078 patients with bronchiolitis included in this study, a nasal swab for other respiratory viruses was performed in 357 (33.1%) of them and one pathogen was detected in 220 (20.4%) children. The most common pathogen detected was RSV (49.6%) and other viruses, as Rhinovirus, Adenovirus, Metapneumovirus, and Influenza virus, were identified in 43 (12%) cases. The comparison of available microbiological data in the two groups—2020–2021 season versus 5 previous years—did not reveal statistically significant differences (p = .8) (Table 1).
A multivariate logistic regression was performed to ascertain the effects of the COVID‐19 period (and thus face mask use during this period), prematurity and age on the likelihood that participants have RSV bronchiolitis. The logistic regression model was statistically significant, χ 2(3) = 17, p < .01. The analysis showed no correlation with the COVID‐19 period or prematurity; instead lower age was associated with an increased likelihood of exhibiting RSV bronchiolitis (OR 0.9; 95% CI 0.86–0.95 p < .01) (Table 2).
Table 2.
Multivariate logistic regression analysis of risk factors for RSV Bronchiolitis in children admitted to our ED
| Risk factors | B | Wald | p value (χ 2 Test) | Odds ratio (95% CI) |
|---|---|---|---|---|
| COVID‐19 period | 0.31 | 0.258 | .61 | 1.36 (0.41–4‐49) |
| Age (months) | −0.10 | 13.56 | <.01 | 0.9 (0.85–0.95) |
| Prematurity | −0.27 | 0.84 | .36 | 1.31 (0.73–2.37) |
Abbreviations: COVID‐19, coronavirus disease 2019; ED, emergency department; RSV, respiratory syncytial virus.
4. DISCUSSION
During the COVID‐19 outbreak, our data showed a significant reduction in the total number of ED consultations, according to the literature.10, 11, 12, 13 This was due primarily to the recommendations imposed at the beginning of the pandemic to avoid access to ED, except in cases of real need, but also to the fear of being infected with SARS‐CoV‐2.
In the months following the national lockdown, the rate of visits to the ED remained consistently low, but the most interesting fact concerned infectious diseases. Different reports, from Italy and abroad, drawn attention to the reduction of acquired respiratory infections such as upper respiratory tract infections, streptococcal pharyngitis, otitis, bronchitis, and pneumonia.14, 15, 16, 17
Lin et al. 18 reported a reduction of respiratory tract infections in Taiwan from February to April 2020, simultaneously to a higher proportion of urinary tract infections and asthma.
According to our data, during the second COVID‐19 wave in France, visits for bronchiolitis were 82.1% lower than predicted by the time series analysis. 19
After the initial “total lockdown” in Italy, the whole country witnessed a recovery of works, business, and schools, while the physical distancing and nonpharmaceutical interventions, such as the use of face masks and hands hygiene, have remained effective.
Throughout it is important to note that during the autumn–winter 2020 season nurseries and schools remained mostly open and the impact on children's after‐school activities was limited. Therefore, we can assume that the decline in the incidence of bronchiolitis could be attributed to the nonpharmaceutical measures that adults and older children continue to maintain to prevent COVID‐19. Usually, having an older sibling attending school is considered a risk factor for an infant to develop acute bronchiolitis in the first two years of life. This year, the use of face masks and hand hygiene by parents and older siblings helped protect young children from respiratory viral infections. These findings suggest the importance of the diffusion of measures to prevent infectious diseases.
In addition, a very interesting finding from our analysis was the considerable increase in the rate of acute bronchiolitis admitted to the emergency department as Emergency and High Priority Consultations. This could be due to parents' fear of being infected by SARS‐CoV‐2 in hospital and therefore being more cautious before taking their child to the ED. If on one side this may reduce healthcare costs, on the other may increase the risk of having to treat patients with more serious conditions, that instead could be prevented by early and timely intervention.
Although in literature there are reported rare cases of acute bronchiolitis caused by SARS‐CoV‐2,20, 21 we have found no cases among children admitted to our hospital. This could be due to the reduced spread of the virus in the pediatric population and the use of nonpharmaceutical preventive measures. However, the nonavailability of SARS‐CoV‐2 detection kits in the early stage of the pandemic in our hospital may have distorted the collected data and caused the lost of some COVID‐19 positive bronchiolitis. This represents a clear limitation for our study.
Our microbiological data have not shown statistical differences between the rate of VRS bronchiolitis during the COVID‐19 outbreak and the previous 5 years. This shows that differences in the rate of bronchiolitis between analyzed periods are not due to changes in respiratory virus circulation.
Other important limitations are: the 2020–2021 season was observed until February 2021, not including the whole bronchiolitis season; this is a single‐center study and only a small sample of children was analyzed; we do not know whether, during the COVID‐19 outbreak, there was an increase in the number of bronchiolitis managed by their pediatricians, nor how telehealth was developed.
In conclusion, we want to highlight the importance of nonpharmacological preventive hygiene measures that should be maintained even at the end of the COVID‐19 outbreak, especially to protect the youngest and most defenseless patients. In addition, parents should be informed by pediatricians to recognize clinical conditions requiring immediate transport to the emergency care department.
AUTHOR CONTRIBUTIONS
Antonietta Curatola: conceptualization (equal); data curation (equal); formal analysis (equal); writing original draft (equal). Ilaria Lazzareschi: conceptualization (equal); writing review & editing (equal). Giulia Bersani: data curation (equal). Marcello Covino: data curation (equal); validation (equal). Antonio Gatto: writing review & editing (equal). Antonio Chiaretti: writing review & editing (equal).
Curatola A, Lazzareschi I, Bersani G, Covino M, Gatto A, Chiaretti A. Impact of COVID‐19 outbreak in acute bronchiolitis: Lesson from a tertiary Italian Emergency Department. Pediatric Pulmonology. 2021;56:2484‐2488. 10.1002/ppul.25442
DATA AVAILABILITY STATEMENT
Research data are not shared.
REFERENCES
- 1. Ralston SL, Lieberthal AS, Meissner HC, et al, American Academy of Pediatrics . Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. Pediatrics. 2014;134:e1474‐e1502. [DOI] [PubMed] [Google Scholar]
- 2. Kp K, Lee S. Complementary and alternative medicine for the treatment of bronchiolitis in infants: a systematic review. PLoS One. 2017;12:e0172289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Florin TA, Plint AC, Zorc JJ. Viral bronchiolitis. Lancet. 2017;389:211‐224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. WHO . Novel coronavirus (2019. ‐nCoV) situation report 5. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200125-sitrep-5-2019-ncov.pdf?sfvrsn=429b143d_8
- 5. Curatola A, Ferretti S, Gatto A, Chiaretti A. Use of handheld transceiver for hospital healthcare workers‐caregiver communication during the coronavirus disease 2019 (COVID‐19) outbreak in Pediatric Emergency Department. Pediatr Infect Dis J. 2020;39:e80‐e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ruggiero A, Attinà G, Chiaretti A. Additional hypotheses about why COVID‐19 is milder in children than adults. Acta Paediatr. 2020;109:1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cattalini M, Taddio A, Bracaglia C, et al. Childhood multisystem inflammatory syndrome associated with COVID‐19 (MIS‐C): a diagnostic and treatment guidance from the Rheumatology Study Group of the Italian Society of Pediatrics. Ital J Pediatr. 2021;47:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ludvigsson JF. Case report and systematic review suggest that children may experience similar long‐term effects to adults after clinical COVID‐19. Acta Paediatr. 2021;110:914‐921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fricke LM, Glöckner S, Dreier M, Lange B. Impact of non‐pharmaceutical interventions targeted at COVID‐19 pandemic on influenza burden: a systematic review. J Infect. 2021;82:1‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID‐19 pandemic of 2020. Arch Dis Child. 2020;105:704. [DOI] [PubMed] [Google Scholar]
- 11. Valitutti F, Zenzeri L, Mauro A, et al. Effect of population lockdown on pediatric emergency room demands in the era of COVID‐19. Front Pediatr. 2020;8:521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Clavenna A, Nardelli S, Sala D, Fontana M, Biondi A, Bonati M. Impact of COVID‐19 on the pattern of access to a pediatric emergency department in the Lombardy Region, Italy. Pediatr Emerg Care. 2020;36:e597‐e598. [DOI] [PubMed] [Google Scholar]
- 13. Cheek JA, Craig SS, West A, Lewena S, Hiscock H. Emergency department utilisation by vulnerable paediatric populations during the COVID‐19 pandemic. Emerg Med Australas. 2020;32:870‐871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goldman RD, Grafstein E, Barclay N, Irvine MA, Portales‐Casamar E. Paediatric patients seen in 18 emergency departments during the COVID‐19 pandemic. Emerg Med J. 2020;37:773‐777. [DOI] [PubMed] [Google Scholar]
- 15. Soo RJJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID‐ 19 control measures, Singapore. Emerg Infect Dis. 2020;26:1933‐1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hartnett KP, Kite‐Powell A, DeVies J, et al, National Syndromic Surveillance Program Community of Practice . Impact of the COVID‐19 pandemic on emergency department visits ‐ United States, January 1, 2019‐May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dopfer C, Wetzke M, Zychlinsky Scharff A, et al. COVID‐19 related reduction in pediatric emergency healthcare utilization: a concerning trend. BMC Pediatr. 2020;20:427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lin CF, Huang YH, Cheng CY, Wu KH, Tang KS, Chiu IM. Public health interventions for the COVID‐19 pandemic reduce respiratory tract infection‐related visits at pediatric emergency departments in Taiwan. Front Public Health. 2020;8:604089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guedj R, Lorrot M, Lecarpentier T, Leger PL, Corvol H, Carbajal R. Infant bronchiolitis dramatically reduced during the second French COVID‐19 outbreak. Acta Paediatr. 2021;110:1297‐1299. 10.1111/apa.15780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. André MC, Pätzug K, Bielicki J, Gualco G, Busi I, Hammer J. Can SARS‐CoV‐2 cause life‐threatening bronchiolitis in infants? Pediatr Pulmonol. 2020;55:2842‐2843. [DOI] [PubMed] [Google Scholar]
- 21. Grimaud E, Challiol M, Guilbaud C, et al. Delayed acute bronchiolitis in infants hospitalized for COVID‐19. Pediatr Pulmonol. 2020;55:2211‐2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.


