Conflict of interest
The authors have no financial obligations or conflict of interest to declare.
Funding source
None.
Dear Editor,
Vaccination against SARS‐CoV‐2 has spread around the world since December 2020. Herein, we describe three patients, with no history of SARS‐CoV‐2 infection, who developed skin reactions after receiving Pfizer‐BioNTech (New York, NY, USA) COVID‐19 vaccine. The first patient was a 44‐year‐old woman who presented with purpuric lesions on the right and left eyelid, respectively, 21 and 25 days after the second dose of the BNT162b2 mRNA vaccine (Fig. 1c,d). The lesions were circumscribed on the upper eyelid, totally asymptomatic and resolved spontaneously after ten days. The second patient was a 63‐year‐old man who presented similar lesions on the upper eyelid three weeks after the second dose of the vaccine (Fig. 1a,b). The lesions were asymptomatic as well and resolved spontaneously after 15 days. Both patients had complete laboratory evaluation for coagulation disorders that resulted unremarkable.
Figure 1.
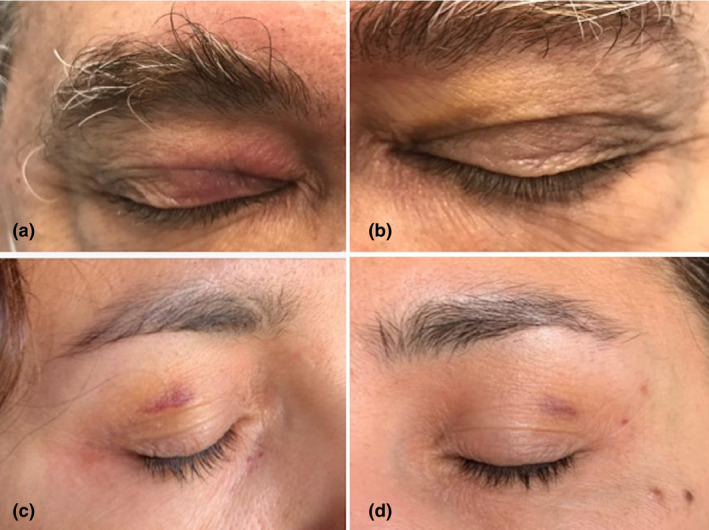
Purpuric lesions on the upper eyelids in patient 2 (a, b) and patient 1 (c, d).
The third was a 67‐year‐old woman who also developed ecchymotic lesions on upper eyelids 10 days after the first dose of the vaccine. The lesions were moderately itchy and resolved spontaneously after 12 days.
Several skin manifestations have been reported in association with coronavirus infection while cutaneous reactions to SARS‐CoV‐2 vaccines have not yet been well documented in literature. 1 Reported reactions included pain and swelling at injection site and erythematous or urticarial rash, usually associated with itch. The lesions were mostly transient with or without systemic symptoms, except for few cases of angioedema and laryngospasm (usually in patients with a well‐known allergic background). 2 However, these adverse events are unspecific and similar to those reported for other vaccines probably related to immune reaction at injection site or allergic reaction to vaccine components.
Herein, we report three cases of eyelid localized purpuric and ecchymotic reaction after BNT162b2 mRNA COVID‐19 vaccine, characterized by appearance after a median of 14 days after injection, absence of symptoms and spontaneous clearing after 10–15 days.
After the launch of vaccination campaign, several new potential adverse events have been reported both with BNT162b2 mRNA and ChAdOx1 adenovirus vaccine. In particular, BNT162b2 mRNA vaccine has been associated both with symptomatic and asymptomatic thrombocytopenia, 3 while ChAdOx1 with several cases of a new, life‐threatening, thrombotic thrombocytopenic disease resembling the heparin‐induced thrombocytopenia, for which the new term vaccine‐induced thrombocytopenic thrombosis (VITT) has been proposed. 4 Besides, in severe cases of COVID‐19 microthrombotic phenomenon is considered at the basis of the multiorgan microangiopathy associated with the SARS‐CoV‐2 infection, so that heparin is now one of the cornerstones of severe COVID‐19 treatment.
Finally, during the first and second wave of SARS‐CoV‐2 pandemic several papers reported purpuric and ecchymotic skin eruption on feet and hands, mostly in otherwise healthy adolescents, currently referred as ‘chilblain‐like lesions’. 5 , 6 , 7 , 8
Hence, in general SARS‐CoV‐2 infection and immune response to the virus may cause, with different pathogenetic mechanisms, endothelial damage and/or uncontrolled activation of coagulation system.
In this context, the observation of purpuric and ecchymotic lesions on eyelids shortly after receiving BNT162b2 mRNA vaccine could represent a form of very mild and localized form of vaccine‐induced microangiopathy. Less likely, these lesions may share similar pathogenetic mechanisms with CLL, which are now considered as a virus‐induced interferonopathy associated with a strong activation of innate immune system and fast clearance of antibodies. 9 , 10
We are aware that our three cases are not enough to establish a cause–effect relationship between these lesions and the BNT162b2 mRNA vaccine; however, we have described this condition firstly because it is important to report any new postmarketing reaction to vaccine and then to reassure patients of the transience of this clinical manifestation after the first or second dose of BNT162b2 mRNA vaccine. Further larger studies are desirable to confirm our data and possibly to enlighten the pathogenesis of this phenomenon.
Acknowledgements
The patients in this manuscript have given written informed consent to the publication of their case details
References
- 1. Corbeddu M, Diociaiuti A, Vinci MR et al. Transient cutaneous manifestations after administration of Pfizer‐BioNTech COVID‐19 Vaccine: an Italian single centre case series. J Eur Acad Dermatol Venereol 2021; 35: e483–e485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ring J, Worm M, Wollenberg A et al. Risk of severe allergic reactions to COVID‐19 vaccines among patients with allergic skin diseases – practical recommendations. A position statement of ETFAD with external experts. J Eur Acad Dermatol Venereol 2021: 35: e362–e365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee EJ, Cines DB, Gernsheimer T et al. Thrombocytopenia following Pfizer and Moderna SARS‐CoV‐2 vaccination. Am J Hematol 2021; 96: 534–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov‐19 vaccination. N Engl J Med 2021; 384: 2092–2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Piccolo V, Neri I, Manunza F, Mazzatenta C, Bassi A. Chilblain‐like lesions during the COVID‐19 pandemic: should we really worry? Int J Dermatol 2020; 59: 1026–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Piccolo V, Bassi A, Argenziano G et al. Dermoscopy of chilblain‐like lesions during the COVID‐19 outbreak: a multicenter study on 10 patients. J Am Acad Dermatol 2020; 83: 1749–1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Piccolo V, Bassi A. Acral findings during the COVID‐19 outbreak: Chilblain‐like lesions should be preferred to acroischemic lesions. J Am Acad Dermatol 2020; 83: e231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Piccolo V, Bassi A, Russo T et al. Chilblain‐like lesions and COVID‐19: second wave, second outbreak. J Eur Acad Dermatol Venereol 2021; 35: e316–e318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hubiche T, Cardot‐Leccia N, Le Duff F et al. Clinical, laboratory, and interferon‐alpha response characteristics of patients with chilblain‐like lesions during the COVID‐19 pandemic. JAMA Dermatol 2020; 157: e204324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sekine T, Perez‐Potti A, Rivera‐Ballesteros O et al. Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID‐19. Cell 2020; 183: 158–168.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]


