Abstract
Objectives
Investigation of potential erroneous behavior in the general public's use of face masks during the COVID‐19 pandemic.
Design
We conducted a naturalistic observational study in the period from April to June 2020.
Sample
In two western Austrian provinces, a total of 2080 persons were observed in front of 24 grocery stores.
Measurement
The frequencies and types of erroneous behavior in the use of face masks were collected using a standardized observation form.
Results
A total of 2080 persons were observed. Almost one‐third of all observations (n = 648; 31.2%) showed erroneous behavior before positioning the face masks. Another 935 (45.0%) persons touched the face mask front during the adjustment via mouth and nose, 501 (24.1%) persons touched the face mask front in the period after the adjustment. A total of 116 (5.6%) persons showed erroneous behavior in each sequence of the observation unit. Overall, almost half of all people observed showed at least one erroneous behavior within the observation period.
Conclusions
The behavior of the general public in handling face masks is highly error‐prone. Decision makers must increasingly provide accompanying information and educational measures in order to encourage the population at risk to use face masks correctly.
Keywords: COVID‐19, face mask, nursing research, observational study, usage behavior
1. BACKGROUND
With a current global infection rate of 126,697,603 cases and 2,776,175 deaths to date, COVID‐19 pandemic is a worldwide challenge at systemic and individual level (World Health Organization, 2021a). In Austria, approximately 530,844 people have been tested positive for COVID 19 and 8,995 deaths with COVID‐19 diagnosis have been recorded (World Health Organization, 2021b). Following the WHO guidance for the containment of the virus, Austria and several other countries have introduced the obligation to wear face masks in public places in addition to the measure of physical distancing (Federal Ministry of Social Affairs, Health, Care, & Consumer Protection, 2020b; Pharmacists' Defence Association, 2020).
The main transmissions of SARS‐CoV‐2 are contact and droplet spread (Santarpia et al., 2020). When breathing, speaking, or coughing, viruses are transmitted via respiratory droplets (Jayaweera et al., 2020). Therefore, this transmission path should be interrupted by covering mouth and nose (Jefferson et al., 2011). Several studies have shown the effectiveness of wearing face masks in public as a means of preventing transmission (Chu et al., 2020; Chughtai et al., 2016; Eikenberry et al., 2020; Li et al., 2020; Liang et al., 2020; Macintyre & Chughtai, 2020). However, the effectiveness of the use of masks depends on the general public's behavior in handling face masks. Throughout this study, the term behavior is strictly referred to the general public's behavior in handling face masks. According to international hygienic guidance (World Health Organization, 2020a), the spread of microorganisms is probable if (a) the front of the mask is touched with the fingers during transport, positioning, or subsequent wearing, (b) the mask does not completely cover the mouth and nose after positioning, and (c) the surface of the mask over the mouth and nose is not tightened (for surgical masks the stiff edge must also be adjusted). If these behavioral aspects are not respected, there is a risk of virus transmission via the air as well as the risk of virus transfer from contaminated palms to surfaces in the environment (Chu et al., 2020). This risk is particularly high in grocery stores, where many people are moving around in a limited space at the same time and are constantly in contact with potentially contaminated surfaces (Ong et al., 2020).
Based on the assessment of this risk, the mandatory wearing of face masks as an accompanying intervention to physical distancing in this setting was introduced in Austria on April 6, 2020 for all persons over the age of 6 years (Federal Ministry of Social Affairs, Health, Care, & Consumer Protection, 2020c). However, as the general population is not familiar with wearing a face mask, incorrect use is inevitable. Systemic measures to change the health‐related behavior of individuals can only be effective, if people are informed about the meaning, purpose, and intended objectives of the measure (Howard et al., 2020) in a target‐group‐specific manner and under sufficient time conditions (Marasinghe, 2020). However, due to the urgent need for action in the context of COVID‐19 pandemic, suggested public health measures (World Health Organization, 2020b) could not be sufficiently addressed to all persons concerned by policymakers. As a consequence, there could be a lack of acceptance for the mandatory use of face masks (Chughtai et al., 2016). Furthermore, the inadequate explanation of the proper use of face masks could lead to potential erroneous behavior in the population using a hygiene and protection measure that is basically meant for healthcare professionals.
In the past, nurses have rarely been seen as an important resource for taking on responsibilities in the public health context in Austria (Schaeffer & Pelikan, 2017), although providing population‐related information as part of health promotion measures is a core competence of nursing in Austria (Federal Ministry of Social Affairs, Health, Care, & Consumer Protection, 2020a). Generally, the evaluation of the status quo is a prerequisite for the development of target group‐oriented health promotion (World Health Organization, 2020b). Therefore, the aim of the study was to investigate the general public's behavior in handling face masks in a public space. Based on the data collected, the frequency of erroneous behavior according to the international hygienic guidance (World Health Organization, 2020a) should be identified and quantified. The results should provide a basis for the development of information and education measures.
2. METHODS
2.1. Research questions
a. Which behaviors, non‐compliant with the WHO guidance on the use of masks, can be observed in the general population?
b. How often can behaviors, non‐compliant with the WHO guidance on the use of masks, be found in the general population?
2.2. Study design
We conducted a naturalistic observational study.
2.3. Objects and sample
A non‐probabilistic convenience sample was observed. We defined to include any adolescent and adult person who would enter the observation corridor after any one‐minute time interval to ensure the exclusion of arbitrary selection.
2.4. Observation sites
The observations were conducted in front of 24 grocery stores of different companies in two provinces of Western Austria. We defined an observation corridor of approximately 20‐by‐20 meters around the entrance areas.
2.5. Observation times
The observations were conducted over a period of 6 weeks from April to June 2020. For each observation unit, a duration of 25 to 40 s was pre‐estimated based on the findings from the pre‐test.
2.6. Observation procedure
2.6.1. Observers
The standardized observations were carried out by a total of 13 persons. All observers were nursing science students. The students were instructed face to face as well as via specially designed videos regarding the specific observational conditions. Figure 1 provides information about the structure of the standardized observation process.
FIGURE 1.
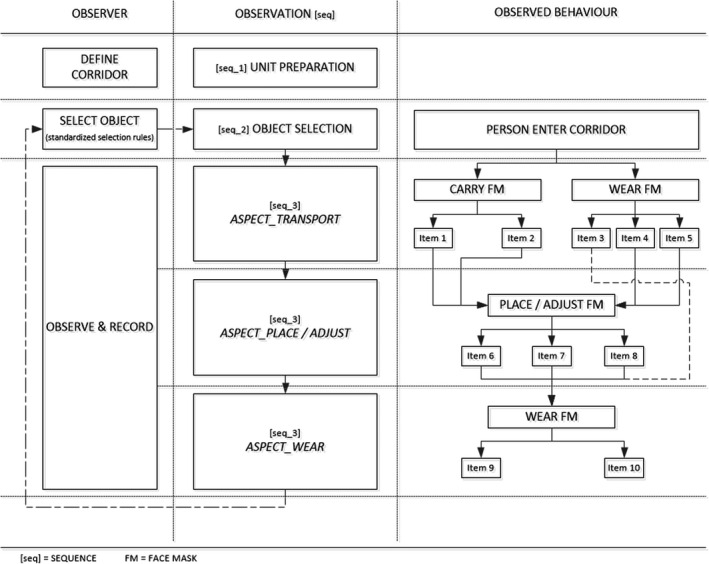
Structure of the standardized observation process
2.6.2. Observation units and standardized assessment
Based on a thematically specific literature research conducted by two independent researchers, various criteria were identified which seemed to be scientifically valid in the correct usage of face masks (Coia et al., 2013; Ho, 2012; World Health Organization, 2020a). This pool of identified criteria was topically structured, assessed for relevance and synthesized in a consensus procedure by two researchers. Subsequently, 12 items were formulated that relate to three main behavioral aspects Transport, Place/Adjust, and Wear. The resulting observation form was tested by the students in a pre‐test observation. Based on written and verbal feedbacks of the students on practicability and comprehensibility of the observation form following the pre‐test, the observation form was reduced by two items. Another three items were revised and reformulated due to a reported lack of comprehensibility and clarity.
The final version of the observation form enables a standardized recording of a complete observation unit. It consists of a total of 10 items, which are assigned to three observable main behavioral aspects and are responded by marking the observed behavior corresponding to a dichotomous rating (Figure 2).
FIGURE 2.

Standardized observation form to observe the behavior in the use of face masks
2.7. Data analysis
Descriptive data analysis was performed using SPSS Statistics for Windows, version 24.0 (SPSS Inc., Chicago, Ill., USA). Data visualization was performed using SankeyMATIC open source software (www.sankeymatic.com).
2.8. Ethical considerations
The study protocol was submitted for consideration to the university's competent ethics committee. This ethical committee confirmed in a written statement that there was no need for an ethical committee approval nor an institutional submission requirement.
3. RESULTS
3.1. Observation characteristics
Table 1 provides information on the observation time per site and the number of persons observed both per site and in total in the respective federal provinces.
TABLE 1.
Observation characteristics
|
Observation Site Store number # |
Observation Objects n |
Observation Time min/site; mean (range) |
|---|---|---|
| Store #01 a | 52 | 60 |
| Store #02 a | 48 | 60 |
| Store #03 a | 156 | 190 |
| Store #04 a | 84 | 95 |
| Store #05 a | 125 | 160 |
| Store #06 a | 154 | 190 |
| Store #07 a | 102 | 110 |
| Store #08 a | 124 | 140 |
| Store #09 a | 42 | 60 |
| Store #10 a | 37 | 60 |
| Store #11 a | 79 | 120 |
| Store #12 a | 32 | 60 |
| Total a | 1.035 | 1.305; 108.75 (130) |
| Store #13 b | 48 | 65 |
| Store #14 b | 62 | 80 |
| Store #15 b | 27 | 60 |
| Store #16 b | 31 | 60 |
| Store #17 b | 38 | 60 |
| Store #18 b | 271 | 600 |
| Store #19 b | 156 | 450 |
| Store #20 b | 48 | 60 |
| Store #21 b | 137 | 270 |
| Store #22 b | 102 | 115 |
| Store #23 b | 81 | 115 |
| Store #24 b | 44 | 60 |
| Total b | 1.045 | 1.995; 166.25 (540) |
| Total a , b | 2.080 | 3.300; 137.5 (540) |
Abbreviation: min, minutes.
Federal Province Tyrol.
Federal Province Vorarlberg.
3.2. Observation results
In total, the carrying, adjusting and wearing behavior of 2,080 persons was observed. In observation sequence 1 (carrying/wearing behavior when entering the observation corridor), 1,352 persons (65.0%) wore the face masks either already completely (n = 1,078; 51.8%) or only partially (n = 274; 13.2%) adjusted, 728 persons (35.0%) carried the face masks either directly at the face mask front (n = 374; 51.4%) or at the straps (n = 354; 48.6%).
Nearly half of all persons that had either carried the face masks by hand or had only partially adjusted the face mask when entering the observation corridor (n = 935; 45.0%; missing: n = 67) touched the face mask front (n = 394; 42.1%) when positioning the face mask (observation sequence 2), 541 persons (57.9%) touched the straps. The stiff edge of the face masks was also adjusted by about every third person (n = 301; 30.6%), two thirds (n = 683; 69.4%) of all observed persons skipped this step completely.
In the third observation sequence, it one could see that nearly a quarter of all observed persons (n = 501; 24.1%) touched the face mask front in the period after adjusting the face masks and before leaving the observation corridor. The facial area covered by the face mask was touched by a total of 46 persons (2.2%) in this observation sequence. Figure 3 gives information about the number of observed errors in face mask usage per sequence in relation to the defined subgroups. In total, 1,083 persons (52.1%) did not show any obvious behavioral error within the observation unit, while 116 persons (5.6%) showed one error in each observation sequence. In total, the face mask front was touched at least once during each observation unit by 928 persons (44.6%; missing: n = 69).
FIGURE 3.

Sankey diagram of error frequencies in relation to the observed carrying and wearing [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
This study aimed to observe behaviors that do not comply with the WHO guidance for the use of face masks in the general population and to record frequencies in erroneous behavior regarding transport, positioning, and wearing of the mask. Considering the results, erroneous behavior in the use of face masks is highly prevalent in the general population.
At least one erroneous behavior could be observed in almost half of all observed persons. With regard to the erroneous carriage of masks, there are potential risks of virus transmission in the sense of self and external hazard. Primarily hands are potentially contaminated with pathogens. This could mean that any contact of the hands with the inside of the mask contributes to the transmission of viruses into the respiratory tract (Chowell et al., 2015). Conversely, especially in the case of multiple use of disposable masks as well as uncleaned cloth masks by infected persons, it can be expected that viruses will be further spread by the contaminated mask as a result of further contact with surfaces (van Doremalen et al., 2020). It could also be observed that a part of all persons wore the mask only under the nose or mouth. In addition to the inadequate protection of the immediate environment caused by this behavior, there is also the possibility that viruses are exhaled directly onto the outside of the mask. As the observation showed, a large proportion of the people who wore the mask below the nose or mouth touched the potentially contaminated mask surface when the mask was completely positioned or before entering the grocery store. Based on the premise that the described cascade of infections can be triggered by touching the mask and that almost half of all persons observed made this mistake in their wearing behavior at least once, the intended effectiveness of the measure may be limited. Taking into account the average observation time (<1 min), this result is concerning inasmuch as these behavioral errors could occur repeatedly with increasing wearing time. Furthermore, people who had already worn face masks prior to entering the observation corridor may have gone through adjustments with errors. The time until mouth and nose was completely covered by the mask varied within the time of entering the observation corridor and entering the store. In combination with not reaching the minimum distance, this could have significantly increased transmission risk (Jefferson et al., 2011).
The WHO guidance on the use of masks in the context of COVID‐19 points out the importance of accompanying information and education measures when the governmental health authority introduces the obligation of wearing masks (World Health Organization, 2020b). Generally speaking, established theories on behavioral change in health‐related contexts unanimously point out that the success of systemic public health interventions not only depends on the provision of measure‐related information, but that the factors time and the possibility of motivational adaptation are decisive for implementation (Bandura, 2005), (Prochaska & Velicer, 1997), (Rogers, 1975). Due to the acute need for action, however, the implementation of the mask obligation could not be carried out under the mentioned strategically essential aspects. In combination with the negative effects of limited health literacy in the context of COVID‐19 (Paakkari & Okan, 2020), this could provide an explanation for the insufficient handling of face masks in the sample observed.
4.1. Strengths and limitations
The study design was appropriate for an explorative baseline assessment of the behavior in handling face masks, as no data were available for Austria so far. A strength of the study was the high standardization of the observations by using a structured observation form and professionally trained observers. Nevertheless, it must be critically noted that possible bias cannot be ruled out due to the lack of testing of the observation form for inter‐rater reliability. In addition to the standardized observation corridor, observation sites were strictly determined, which minimized bias caused by different conditions within the observations. In order to prevent selection bias, we tried to include people from all income and consumer groups by including grocery stores of different companies (from low budget to exclusive stores). Furthermore, the observed persons were selected by following a strictly regulated procedure with constant time criteria. However, due to the chosen sampling method (convenience sample), selection bias is possible. Due to pandemic‐related travel restrictions at the time of the study, only two of a total of nine provinces in Austria could be included in the data collection. The results of this observational study can therefore not be generalized to the Austrian population.
We did not choose observation dates according to any defined pattern. This is due to the fact that no theory could be found in the literature which associates preferred shopping times with characteristics of a certain kind of population. Furthermore, at the time of the study, social life and daily routines in Austria were highly influenced by the restrictions and effects of the lockdown. Moreover, the obligation to wear masks in Austria applies without exception to all persons from the age of 6 years onwards and irrespective of individual personal characteristics. Therefore, all observations were carried out on different days of the week at different times of the day in order to reduce bias in this context as far as possible.
The sample size (n = 2,080) would be suitable to generalize the results to the whole Austrian population. Based on a sample calculation assuming an estimated total population of 970,000 persons in the Austrian provinces of Tyrol and Vorarlberg, the minimum sample size would be 384 persons (95% CI) (Qualtrics, 2020). However, the representativeness of the sample cannot be assumed due to the lack of sociodemographic characteristics. Nevertheless, it should be considered that the wearing of face masks is a measure that is equally relevant for all persons in the general population (excluding children <6 years) and can therefore provide trend information about the wearing behavior in the general public. The short observation time per observed person and the selection of observation sites cannot give any information about the long‐term wearing behavior. We decided to conduct the study under the described conditions, as this was the only way to ensure the safety of the observers. A further strength is the comprehensible visualization of the structured observation process and the presentation of the results using a Sankey diagram, which clearly illustrates the error frequencies in relation to the observed carrying and wearing behavior in an innovative form.
5. CONCLUSIONS
The usage of face masks in the general public is highly error‐prone concerning the behavioral aspects of transporting, adjusting, and wearing. Even if the study is not able to respond to the question of the reasons for the erroneous usage, there is an obvious need for action for the decision makers. Especially because of the potential risk of increase of COVID‐19 infections and the associated maintenance of the mask obligation, further research should explore potential associations between erroneous behaviors in the use of masks and various population groups.
CONFLICT OF INTEREST
None.
Kellerer JD, Rohringer M, Deufert D. Behavior in the use of face masks in the context of COVID‐19. Public Health Nurs. 2021;38:862–868. 10.1111/phn.12918
Jan Daniel Kellerer & Matthias Rohringer: ex aequo authorship.
Funding information
No external funding.
REFERENCES
- Bandura, A. (2005). The growing centrality of self‐regulation in health promotion and disease prevention. The European Health, Psychologist, 1, 11–12. [Google Scholar]
- Chowell, G. , Abdirizak, F. , Lee, S. , Lee, J. , Jung, E. , Nishiura, H. , & Viboud, C. (2015). Transmission characteristics of MERS and SARS in the healthcare setting: A comparative study. BMC Medicine, 13(1), 210. 10.1186/s12916-015-0450-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu, D. K. , Akl, E. A. , Duda, S. , Solo, K. , Yaacoub, S. , Schünemann, H. J. , Chu, D. K. , Akl, E. A. , El‐harakeh, A. , Bognanni, A. , Lotfi, T. , Loeb, M. , Hajizadeh, A. , Bak, A. , Izcovich, A. , Cuello‐Garcia, C. A. , Chen, C. , Harris, D. J. , Borowiack, E. , … Schünemann, H. J. (2020). Physical distancing, face masks, and eye protection to prevent person‐to‐person transmission of SARS‐CoV‐2 and COVID‐19: A systematic review and meta‐analysis. The Lancet, 395(10242), 1973–1987. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chughtai, A. A. , Seale, H. , Dung, T. C. , Hayen, A. , Rahman, B. , & Raina MacIntyre, C. (2016). Compliance with the use of medical and cloth masks among healthcare workers in vietnam. The Annals of Occupational Hygiene, 60(5), 619–630. 10.1093/annhyg/mew008 [DOI] [PubMed] [Google Scholar]
- Coia, J. E. , Ritchie, L. , Adisesh, A. , Makison Booth, C. , Bradley, C. , Bunyan, D. , Carson, G. , Fry, C. , Hoffman, P. , Jenkins, D. , Phin, N. , Taylor, B. , Nguyen‐Van‐Tam, J. S. , & Zuckerman, M. (2013). Guidance on the use of respiratory and facial protection equipment. The Journal of Hospital Infection, 85(3), 170–182. 10.1016/j.jhin.2013.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eikenberry, S. E. , Mancuso, M. , Iboi, E. , Phan, T. , Eikenberry, K. , Kuang, Y. , Kostelich, E. , & Gumel, A. B. (2020). To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID‐19 pandemic. Infectious Disease Modelling, 5, 293–308. 10.1016/j.idm.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Ministry of Social Affairs, Health, Care and Consumer Protection . (2020a). Austrian Health and Nursing Act. Retrieved from https://www.ris.bka.gv.at/GeltendeFassung.wxe?Abfrage=Bundesnormen&Gesetzesnummer=10011026 [Google Scholar]
- Federal Ministry of Social Affairs, Health, Care and Consumer Protection (2020b). Coronavirus ‐ Information available for download. Retrieved from https://www.sozialministerium.at/en/Coronavirus/Coronavirus‐‐‐Information‐available‐for‐download.html [Google Scholar]
- Federal Ministry of Social Affairs, Health, Care and Consumer Protection . (2020c). Coronavirus ‐ Rechtliches. Retrieved from https://www.sozialministerium.at/Informationen‐zum‐Coronavirus/Coronavirus‐‐‐Rechtliches.html [Google Scholar]
- Ho, H. S. W. (2012). Use of face masks in a primary care outpatient setting in Hong Kong: Knowledge, attitudes and practices. Public Health, 126(12), 1001–1006. 10.1016/j.puhe.2012.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard, J. , Huang, A. , Li, Z. , Tufekci, Z. , Zdimal, V. , van der Westhuizen, H.‐M. , von Delft, A. , Price, A. , Fridman, L. , Tang, L.‐H. , Tang, V. , Watson, G. L. , Bax, C. E. , Shaikh, R. , Questier, F. , Hernandez, D. , Chu, L. F. , Ramirez, C. M. , & Rimoin, A. W. (2020). Face Masks Against COVID‐19: An Evidence Review. 10.20944/preprints202004.0203.v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayaweera, M. , Perera, H. , Gunawardana, B. , & Manatunge, J. (2020). Transmission of COVID‐19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environmental Research, 188, 109819. 10.1016/j.envres.2020.109819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson, T. , Del Mar, C. B. , Dooley, L. , Ferroni, E. , Al‐Ansary, L. A. , Bawazeer, G. A. , van Driel, M. L. , Nair, S. , Jones, M. A. , Thorning, S. , & Conly, J. M. (2011). Physical interventions to interrupt or reduce the spread of respiratory viruses. The Cochrane Database of Systematic Reviews, 7, CD006207. 10.1002/14651858.CD006207.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, T. , Liu, Y. , Li, M. , Qian, X. , & Dai, S. Y. (2020). Mask or no mask for COVID‐19: A public health and market study. PLoS One, 15(8), e0237691. 10.1371/journal.pone.0237691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, M. , Gao, L. , Cheng, C. , Zhou, Q. , Uy, J. P. , Heiner, K. , & Sun, C. (2020). Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta‐analysis. Travel Medicine and Infectious Disease, 36, 101751. 10.1016/j.tmaid.2020.101751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre, C. R. , & Chughtai, A. A. (2020). A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. International Journal of Nursing Studies, 108, 103629. 10.1016/j.ijnurstu.2020.103629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marasinghe, K. M. (2020). Concerns around public health recommendations on face mask use among individuals who are not medically diagnosed with COVID‐19 supported by a systematic review search for evidence. Advance Online Publication. 10.21203/rs.3.rs-16701/v3 [DOI]
- Ong, S. W. X. , Tan, Y. K. , Chia, P. Y. , Lee, T. H. , Ng, O. T. , Wong, M. S. Y. , & Marimuthu, K. (2020). Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) from a symptomatic patient. JAMA, 323(16), 1610– 10.1001/jama.2020.3227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paakkari, L. , & Okan, O. (2020). COVID‐19: Health literacy is an underestimated problem. The Lancet Public Health, 5(5), e249–e250. 10.1016/S2468-2667(20)30086-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pharmacists' Defence Association (2020). Wearing face masks in Public: Approach of different countries across the world. Retrieved from https://www.the‐pda.org/wp‐content/uploads/001‐Facemask‐in‐public‐EU‐Iman‐V2.pdf [Google Scholar]
- Prochaska, J. O. , & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38–48. 10.4278/0890-1171-12.1.38 [DOI] [PubMed] [Google Scholar]
- Qualtrics . (2020). Stichprobenrechner. Retrieved from https://www.qualtrics.com/de/erlebnismanagement/marktforschung/stichprobenrechner/ [Google Scholar]
- Rogers, R. W. (1975). A protection motivation theory of fear appeals and attitude change1. The Journal of Psychology, 91(1), 93–114. 10.1080/00223980.1975.9915803 [DOI] [PubMed] [Google Scholar]
- Santarpia, J. L. , Rivera, D. N. , Herrera, V. , Morwitzer, M. J. , Creager, H. , Santarpia, G. W. , Crown, K. K. , Brett‐Major, D. , Schnaubelt, E. , Broadhurst, M. J. , Lawler, J. V. , Reid, S. P. , & Lowe, J. J. (2020). Aerosol and Surface Transmission Potential of SARS‐CoV‐2. 10.1101/2020.03.23.20039446 [DOI] [Google Scholar]
- Schaeffer, D. , Pelikan, J. M. , Eds (2017). Health literacy: Forschungsstand und Perspektiven (1. Auflage). Hogrefe. [Google Scholar]
- van Doremalen, N. , Bushmaker, T. , Morris, D. H. , Holbrook, M. G. , Gamble, A. , Williamson, B. N. , Tamin, A. , Harcourt, J. L. , Thornburg, N. J. , Gerber, S. I. , Lloyd‐Smith, J. O. , de Wit, E. , & Munster, V. J. (2020). Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. The New England Journal of Medicine, 382(16), 1564–1567. 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020a). Advice on the use of masks in the context of COVID‐19: Interim guidance, 6 April 2020. World Health Organization. https://apps.who.int/iris/handle/10665/331693 [Google Scholar]
- World Health Organization (2020b). Strengthening and adjusting public health measures throughout the COVID‐19 transition phases. Retrieved from https://www.euro.who.int/__data/assets/pdf_file/0018/440037/Strength‐AdjustingMeasuresCOVID19‐transition‐phases.pdf?ua=1 [Google Scholar]
- World Health Organization (2021a). WHO Coronavirus Disease (COVID‐19) Dashboard | WHO Coronavirus Disease (COVID‐19) Dashboard. Retrieved from https://covid19.who.int/ [Google Scholar]
- World Health Organization (2021b). WHO Coronavirus Disease (COVID‐19) Dashboard‐Austria. Retrieved from https://covid19.who.int/region/euro/country/at [Google Scholar]


