Abstract
Aim
To describe the epidemiology of respiratory viruses in children before and during the 2020 SARS‐CoV‐2 pandemic and the relationship to public health measures instituted by the Victorian government.
Methods
Retrospective audit of respiratory viruses at a tertiary paediatric hospital in Melbourne from January 2015 up to week 47, 2020 in children under 18 years of age. The proportion of positive cases in weeks 1–47 in 2015–2019 (period 1) were compared to weeks 1–47, 2020 (period 2), and reviewed in the context of public health restrictions in Victoria.
Results
An annual average of 4636 tests were performed in period 1 compared to 3659 tests in period 2. Proportions of positive influenza A virus, influenza B virus, respiratory syncytial virus (RSV) and human parainfluenza virus were significantly reduced in period 2 compared to period 1: 77.3, 89.4, 68.6 and 66.9% reductions, respectively (all P < 0.001). From week 12–47, 2020, 28 893 SARS‐CoV‐2 tests were performed with a 0.64% positivity rate. Influenza viruses were not detected after week 17, RSV was not detected after week 35.
Conclusions
Strict public health measures and border closures were successful in eliminating community transmission of SARS‐CoV‐2 in Melbourne. This was associated with a significant reduction in other respiratory virus infections in children. Identifying sustainable and effective ongoing public health interventions to reduce transmission of RSV and influenza could result in reduced morbidity and mortality in children and requires further research.
Keywords: children, COVID‐19, influenza, respiratory syncytial virus, respiratory virus
What is already known on this topic
Public health interventions including lockdown, border closures, enhanced hygiene and physical distancing have been effective in controlling transmission of SARS‐CoV‐2 and other respiratory viruses in children in Australian states with low SARS‐CoV‐2 community transmission.
This has largely been attributed to strict border closures, but numbers of respiratory syncytial virus have increased in Western Australia and New South Wales since easing of public health restrictions.
What this paper adds
Metropolitan Melbourne experienced the highest rates of SARS‐CoV‐2 community transmission in Australia despite border closures, with resultant strict public health interventions of varying degrees during 2020.
We describe the effect of these measures on circulating respiratory viruses in children in Melbourne during the pandemic compared to previous years.
Mandatory masks did not show additional benefit as respiratory virus detections had already diminished prior to their introduction. Identifying sustainable and effective ongoing public health interventions to reduce transmission of respiratory syncytial virus and influenza could result in reduced morbidity and mortality in children and requires further research.
Respiratory viruses, particularly respiratory syncytial virus (RSV) are associated with high morbidity and mortality in children. RSV has seasonal peaks between April and June in the Southern hemisphere and is a common cause of bronchiolitis; national data suggests an RSV‐related hospitalisation rate of 418 per 100 000 among children less than 5 years of age and 224/100 000 in infants less than 6 months of age. 1 Influenza epidemic months occur between May and October in the Southern hemisphere; however, it is known that international travellers may import the virus leading to local transmission outside these months. 2 Children are more likely to have mild or asymptomatic severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection and may have a limited role in transmission of this virus, as opposed to other seasonal respiratory viruses. 3 , 4 , 5 In Australia, public health interventions, including strict lockdowns, have been very effective in controlling transmission of SARS‐CoV‐2. Melbourne, Victoria, Australia, has experienced the highest number of COVID‐19 cases (20 345 as of 11 December 2020) in the country and had the highest rates of community transmission. The state government of Victoria implemented varying degrees of public health interventions for metropolitan Melbourne since 29/3/20, such as stay‐at‐home‐orders, school and business closures, travel restrictions, border closures and mandatory face coverings (see Appendix I for detailed timeline). These measures achieved elimination of community transmission of COVID‐19 from 31 October 2020.
Other states in Australia (Western Australia, New South Wales) have reported a significant reduction in frequency of seasonal respiratory infections such as influenza and RSV in children during periods of lockdown, compared with previous years. 6 , 7 This is consistent with national influenza surveillance data showing substantial decreases in laboratory confirmed influenza from mid‐March. 8 Western Australia and New South Wales have not experienced such prolonged stay‐at‐home orders. While multifactorial, Yeoh et al. emphasise the role of strict border closures on reduction in virus transmission . 7 Both of these states have seen re‐emergence of RSV with easing of local restrictions. 9 , 10
Here, we report on trends in respiratory viruses in children presenting to a large tertiary centre in Melbourne during 2020 compared to previous years, and review the temporal associations between various public health interventions to control the COVID‐19 pandemic and respiratory virus detection in children.
Methods
The Royal Children's Hospital (RCH) Melbourne is a tertiary paediatric referral centre with approximately 136 000 admissions and emergency department presentations per year. Children may be tested for respiratory viruses (using a multiplex respiratory polymerase chain reaction (PCR) panel) when they have a significant respiratory illness requiring admission. Respiratory samples (nasopharyngeal swabs, deep nasal/oral swabs, nasopharyngeal aspirates, sputum, broncho‐alveolar lavage) were tested for respiratory viruses on clinician request through the RCH diagnostic laboratory. Swabs were eluted into 500 μL of phosphate buffered saline. Nucleic acid (NA) from 200 μL of each sample was extracted on the Roche MagNA Pure 96 extraction system (Roche, Basel, Switzerland) using the MagNA Pure DNA and Viral NA Small Volume Kit (Roche). Until November 2019, the laboratory tested DNA extracts using an in‐house respiratory virus assay (influenza A and B viruses, human parainfluenza viruses (HPIV) 1, 2 and 3, RSVs A and B) on the Roche LightCycler 480 platform. From November 2019, extracts were tested with the AusDiagnostics Respiratory Pathogens 16‐well assay (AusDiagnostics, Mascot, Australia) on the AusDiagnostics High‐Plex 24 system. De‐identified data on the following respiratory viruses were obtained from the microbiology laboratory information system from January 2015: influenza A and B viruses, HPIV 1, 2 and 3, RSV. Data on SARS‐CoV‐2 positive cases were also collected from week 12 (commencement of SARS‐CoV‐2 PCR testing at RCH) to week 47 of 2020. All children including inpatients and outpatients from birth to 18 years were included. Period 1: average cases per week 1–47, 2015–2019, were compared with period 2: week 1–47, 2020. The proportion of positive tests for these periods were compared and p‐values were calculated with χ2 tests on Graphpad Prism 9.0 ©.
Organisational ethics approval was not required as this was deemed a quality activity in line with the Australia Health Records Act and no individual‐level data were used.
Timeline of public health measures
We reviewed respiratory virus testing in the context of public health restrictions in Victoria. Appendix I provides a detailed timeline of public health measures. The international border was closed to non‐Australian citizens on 20 March 2020, and returning citizens were required to undertake mandatory 14‐day quarantine on arrival. Further staged public health measures were instituted by the Victorian government as outlined in Table A1. Periods of strict lockdown were from 23 March 2020 to 11 May 2020 (‘Lockdown 1.0’) with a short period of easing, prior to further interventions from 20 June 2020 to 13 September 2020 (‘Lockdown 2.0’) with stage IV restrictions from week 32 to 38. Stage IV restrictions included: 8 pm curfew, 4 reasons to leave home within 5 km, no visitors and no gatherings. Universities moved to remote learning and schools predominantly utilised remote learning for 4 months. Childcare centres remained open (for children of permitted workers only during stage IV restrictions). Mandatory wearing of face coverings outside home for people >12 years old was enforced from 22 July 2020 (week 30) until 7 December 2020 (week 50) (fitted face masks from 27 September 2020). From 2 July 2020 to 7 December 2020 Victoria was closed to all international arrivals.
Results
The average total number of respiratory tests done in period 1 (week 1–47, 2015–2019) was 4636 (range 3758–5348), compared to 3659 tests in period 2 (week 1–47, 2020), representing a 21% reduction in testing numbers during the pandemic period.
In the period 2015–2019, the annual number of influenza A and B virus detections ranged from 178 to 762 (average = 396 detections), with the average peak detections occurring in week 37. The average proportion of total tests that were positive for influenza A virus in period 1 was 5.6% and for influenza B virus, 3.3%. For the first 13 weeks of 2020, prior to local COVID‐19 restrictions, there were 49 total influenza A or B virus detections (proportion positive 4%) compared to average 63 total detections over weeks 1–13 for 2015–2019 (proportion positive 8%). There was a 77.3% reduction in the proportion of positive influenza A virus detections and a 89.4% reduction in proportion of positive influenza B virus detections from period 1 to period 2 (Table 1). There have been no positive influenza A virus detections from week 14, 2020 and no positive influenza B virus detections from week 17, 2020, 2 weeks after initial lockdown (Fig. 1).
Table 1.
Comparison of respiratory viruses period 1 versus period 2
| Period 1 week 1–47, 2015–2019 | Period 2 week 1–47, 2020 | |||||||
|---|---|---|---|---|---|---|---|---|
| Virus | Weekly number of tests, average (range) | Weekly number of detections, average (range) | Proportion positive for period 1, % | Weekly number of tests, average (range) | Weekly number of detections, average (range) | Proportion positive for period 2, % | Reduction in proportion positive, % | P value |
| Influenza A | 92.2 (33.6–134.6) | 4.79 (0–12.75)† | 5.58 | 65.4 (35–138) | 0.83 (0–7)‡ | 1.27 | 77.3 | <0.001 |
| Influenza B | 92.2 (33.6–134.6) | 3.08 (0–7.5)§ | 3.33 | 65.4 (35–138) | 0.23 (0–4)¶ | 0.36 | 89.4 | <0.001 |
| RSV | 92.2 (33.6–134.6) | 13.9 (8.4–21.2)†† | 15.4 | 65.4 (35–138) | 3.17‡‡ | 4.85 | 68.6 | <0.001 |
| Human parainfluenza viruses 1, 2 and 3 | 92.2 (33.6–134.6) | 5.94 (1–12.2)§§ | 6.34 | 65.4 (35–138) | 1.81¶¶ | 2.1 | 66.9 | <0.001 |
| SARS‐CoV‐2††† | NA | NA | 797.9 (86–1974) | 4.8 (0–26) | NA | |||
Statistical analysis of comparison of proportions using χ2 tests on Graphpad Prism 9.0©.
Peak week 37 (average 14.4 detections/week).
Peak week 4 = 7 detections.
Peak week 37 (average 11.6 detections/week).
Peak week 5 = 4 detections.
Peak week 26 (average 41 detections/week).
Peak week 12 = 13 detections.
Peak week 38 (average 12.2/week).
Peak week 11 = 16 detections.
SARS‐CoV‐2 testing commenced week 12, 2020.
Fig 1.
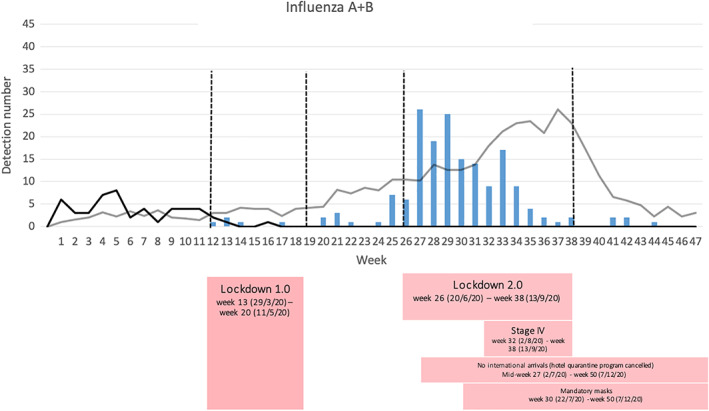
Influenza A and B detections period 1 versus period 2. SARS‐CoV‐2 testing commenced week 12, 2020. No positive influenza A detections from week 14, 2020 and no positive influenza B detections from week 17. ( ), SARS‐CoV‐2; (
), SARS‐CoV‐2; ( ), flu A+B 2015–2019; (
), flu A+B 2015–2019; ( ), flu A+B 2020.
), flu A+B 2020.
In the period 2015–2019, the annual number of RSV detections ranged from 526 to 964 (average = 693), with the average peak detections occurring in week 26. For RSV, there were 94 detections in weeks 1–13 in 2020 (proportion positive 7.8%) compared to average 50.4 detections for the same weeks in period 1 (proportion positive 6.6%). For the RSV epidemic months April to June, there were on average 107.8 detections/month in 2015–2019 (range 34–206, proportion positive 23%) compared to an average of 12 detections/month (range 11–14, proportion positive 5.4%) for this period in 2020. This represents a 76.7% reduction in proportion of RSV detections per month in April to June 2020. Overall, there was a 68.6% reduction in the proportion of positive detections from period 1 to period 2 (Table 1). There have been no RSV detections from week 36, 2020. The trend in relation to different lockdown measures is demonstrated in Figure 2.
Fig 2.
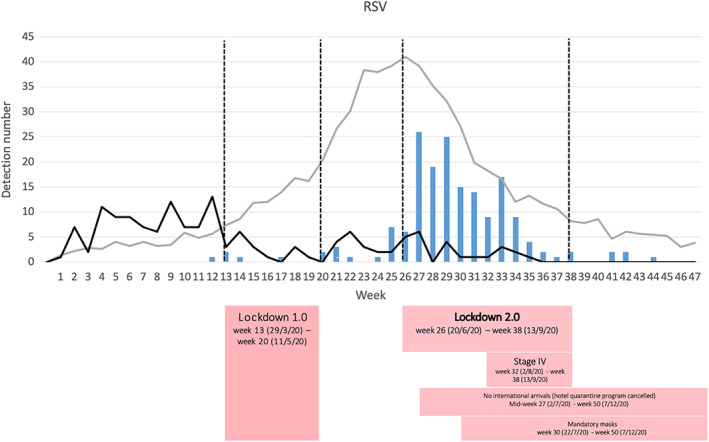
RSV detections period 1 versus period 2. SARS‐CoV‐2 testing commenced week 12, 2020. ( ), SARS‐CoV‐2; (
), SARS‐CoV‐2; ( ), RSV 2015–2019; (
), RSV 2015–2019; ( ), RSV 2020.
), RSV 2020.
In the period 2015–2019, the annual number of HPIV 1, 2 and 3 detections ranged from 254–404 (average = 307.6), with the average peak detections occurring in week 38. There were 75 detections in weeks 1–13 in 2020 (proportion positive 6.4%) compared to average 41.4 detections for the same weeks in period 1 (proportion positive 5.3%). There was a 66.9% reduction in proportion of positive HPIV detections from period 1 to period 2 (Table 1). There have been no positive HPIV detections from week 28, 2020, 2 weeks after lockdown 2.0 (Fig. 3). Predominant human parainfluenza type in the baseline period was HPIV 3 (63–81% of HPIV detections in weeks 1–47 per year) compared to HPIV 1 in 2020 (56%).
Fig 3.
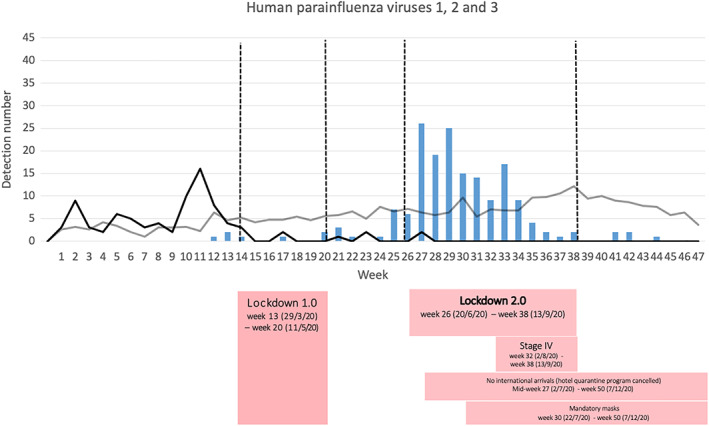
Human parainfluenza viruses 1, 2 and 3 detections period 1 versus period 2. SARS‐CoV‐2 testing commenced week 12, 2020. ( ), SARS‐CoV‐2 2020; (
), SARS‐CoV‐2 2020; ( ), Parainfluenza 1–3 2015–2019; (
), Parainfluenza 1–3 2015–2019; ( ), Parainfluenza 1–3 2020.
), Parainfluenza 1–3 2020.
From week 12–47, 2020, we performed 28 893 SARS‐CoV‐2 tests in children <18 years, with detection of 186 detections. This represents a positivity rate of 0.64% in this age group. Peak detections occurred in week 27 to 29, immediately after lockdown 2.0 measures were introduced in week 26. There were 0–3 detections/week from week 36 and there have been no further positive COVID‐19 detections from week 45 until time of writing.
Discussion
After initial control of SARS‐CoV‐2 transmission facilitated by public health measures in Melbourne in the first half of 2020, a second wave occurred in July–August 2020, with high rates of community transmission.
Victoria saw the largest number of children infected with SARS‐CoV‐2 (as it had the largest outbreak nationally), however overall children represented only a small proportion of those infected with COVID‐19 across the state, consistent with national and international data. 4 The second wave of COVID‐19 infections led to further and stricter public health measures from week 26, mandatory mask‐wearing outside the home from week 30, with eventual down‐trending in rates of transmission after peak detections in week 32.
In our cohort of children presenting to a tertiary children's hospital in metropolitan Melbourne we found a > 65% reduction, compared to previous years, in RSV, influenza and HPIV associated with COVID‐19 public health measures. There were no detections of influenza from implementation of first lockdown measures in week 13 and no re‐emergence despite evidence of other respiratory virus (i.e. SARS‐CoV‐2) community transmission. RSV detections continued in low numbers during the first lockdown (albeit at far lower numbers than in previous years), with no detections of RSV seen since week 35, coinciding with the strictest lockdown measures occurring between week 32–38.
Whilst this sample does not represent all children tested for respiratory viruses in Melbourne, and it is possible that observed reductions in respiratory viruses could have represented changes in health‐seeking behaviour early in the pandemic in our institution, 11 our findings are consistent with published state‐wide surveillance data for influenza captured by the FluCAN surveillance programme to October 31. 12 State‐wide, there has been a 90 and 93% reduction in influenza virus detections in 2020 compared with 2017–2019 year to date average in 0–4 and 5–14 year olds, respectively. Our data therefore likely represents a true reduction in these viruses rather than under‐detection. This is also consistent with Victorian paediatric data showing that there have only been three hospitalisations for influenza in 2020 and no intensive care unit admissions compared to 796 hospitalisations and 91 ICU admissions in 2019. 12 A further potential limitation of this study is the change in testing assays between baseline and observation periods; however, both assays have similar sensitivity and specificity for the reported targets, as confirmed by a laboratory verification study [unpublished data], thus it should not have significantly affected the findings. There was a temporary reduction in respiratory multiplex PCR testing numbers in early 2020 due to an international shortage of molecular laboratory consumables for testing and priority was given to SARS‐CoV‐2 testing. Overall testing was reduced by about 30% compared with previous years. As our analysis compares proportion positive between the two periods (rather than absolute numbers), this is unlikely to have significantly impacted our findings.
The public health response consisted of multiple measures. It is not possible to determine which measure had the largest impact in reducing transmission of respiratory viruses, however it is interesting that influenza viruses disappeared (and did not re‐appear) after the initial lockdown period, whereas RSV persisted at low levels until the most severe measures under stage IV restrictions which included childcare closure except for permitted workers. It is also possible that the decline in RSV infections seen from week 35 reflect the seasonal nature of the virus. New South Wales public health have identified higher than average RSV detections since early October, in conjunction with easing of local restrictions, 9 similar to Western Australia. 10 These states maintained mandatory quarantine for international travellers whilst Victoria was closed to international arrivals from July 2 (mid‐week 27)–December 7 and Melburnians were not able to travel beyond a 25 km radius until week 46. The number of RSV detections in Melbourne has since been reported to have surged in late January 2021 (week 4). 13
It is clear that strict public health restrictions can significantly reduce respiratory virus transmission, with a resultant reduction in childhood morbidity (including hospital and ICU admissions). The lockdown measures in Victoria, which eventually resulted in COVID‐19 elimination, were very restrictive on personal liberties and, in the absence of a pandemic threatening lives and hospital systems, would not be seen as reasonable restrictions by the general community. It is important to observe that other Australian states with less stringent public health interventions also saw a large reduction in respiratory virus transmission. 5 , 6 In most states, border restrictions (significant reduction in interstate and international travel, together with mandatory quarantine for returned travellers) were the major public health intervention after the initial lockdowns were eased, combined with (non‐mandatory) recommendations around personal hygiene measures and physical distancing. Similarly, internationally there have been reductions in influenza without lockdown measures and with border restrictions, school closures, physical distancing and mask wearing. 14
In our analysis there was no evidence of an additional benefit of adult mask wearing to the reduction in respiratory virus detections in children in Melbourne, compared to other public health measures. Mandatory masks were introduced 2 weeks prior to stage IV restrictions, however masks were not mandatory for children <12 years and were not used in childcare or primary school settings. Influenza infections had already disappeared prior to introduction of mandatory mask wearing in July 2020. Consistent reduction in RSV detections (<5 per week) and disappearance of the usual seasonal peak was also seen prior to mask introduction. There was ongoing reduction in RSV infections after introduction of masks; however, this also coincided with stage IV restrictions and closure of most child care centres. It is likely that physical distancing in addition to international border closures resulted in near absence of influenza early in the pandemic.
Conclusions
Strict public health measures and border closures were successful in eliminating community transmission of SARS‐CoV‐2 in Melbourne. These measures resulted in a significant reduction in other respiratory virus infection in children, likely representing a significant reduction in childhood morbidity. This reduction in respiratory virus transmission is similar to that seen in children in other states of Australia, where lockdown measures were less prolonged and severe. It will be important to identify specific elements of the public health response that were most successful in reducing respiratory virus transmission, so that the least restrictive, and most effective, measures can be considered for periods of high respiratory virus transmission in the future. It was not possible to determine the contribution of mandatory mask wearing to our findings as this was introduced after reductions in respiratory detections were already noted.
Acknowledgements
The authors wish to acknowledge the work of the RCH molecular microbiology laboratory team.
Table A1.
Outline of varying degrees of public health restrictions in metropolitan Melbourne
| Dates | Summary of public health restrictions |
|---|---|
| Lockdown 1.0: March 23 (week 13)–May 11 (week 20) |
Stay‐at‐home orders (four reasons to leave home only: going to work or school, care or care giving, daily exercise, buying food and other essentials), school and university closures (remote learning), two person gatherings March 19: Borders closed to non‐residents – March 28: Returning residents mandatory hotel (as opposed to home) quarantine School holidays March 25 to April 14 (week 13–week 15) |
| Lockdown easing 1.0: May 11 (week 20)–June 20 (week 26) |
|
| Lockdown 2.0: June 20 (week 26)–Sep 13 (week 38) |
Schools and university remote learning unless exemption School holidays June 27 to July 12 (week 27–week 28) |
| Lockdown easing 2.0: Sep 13 (week 38)–Nov 23 (week 47) (10 weeks) |
Sep 13: First step (week 38): curfew extended to 9 pm and gatherings increased to 2 people or a household that can meet outdoors for 2 h max Sep 28: Second step (week 40): no curfew, 25 km travel restriction, up to 10 people can meet outdoors, 1 visitor and any children visitors Sep 28: Childcare open Oct 27: All retail reopens Nov 9: Third step (week 46): no restrictions on reasons to leave home or distance, up to 2 people can visit a household once per day. Non‐essential businesses open. Hospitality venues 40 guests inside and 70 guests outside. Up to 20 people can attend a funeral indoors, and 50 outdoors. Indoor gyms will reopen with a capacity of up to 20 people. Indoor pools reopen with a capacity of up to 20 people. Cinemas reopen with 20 guests per space Schools staged return to onsite learning: 12 October 2020 primary school, year 7 and year 12; 26 October 2020, years 8–10 Adult education learn from home if you can Victoria opened to international arrivals from 7 December 2020 with enforced 14‐day hotel quarantine School holidays September 19 to October 4 (week 30–40) |
Conflict of interest: None declared.
References
- 1. Saravanos GL, Sheel M, Homaira N et al. Respiratory syncytial virus‐associated hospitalisations in Australia, 2006–2015. Med. J. Aust. 2019; 210: 447–53. [DOI] [PubMed] [Google Scholar]
- 2. Deng L, Mazzocato P, Saravanos G, Leder K, Britton PN. A high proportion of interseasonal childhood influenza detections in 2019 were travel related. Public Health Res. Pract. 2020; 30: e3022012. [DOI] [PubMed] [Google Scholar]
- 3. COVID‐19 in Children and the Role of School Settings in COVID‐19 Transmission, 2020. Stockholm: European Centre for Disease Prevention and Control; 2020. [Google Scholar]
- 4. Viner RM, Mytton OT, Bonell C et al. Susceptibility to SARS‐CoV‐2 infection among children and adolescents compared with adults: A systematic review and meta‐analysis. JAMA Pediatr. 2021; 175: 143–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Macartney K, Quinn HE, Pillsbury AJ et al. Transmission of SARS‐CoV‐2 in Australian educational settings: A prospective cohort study. Lancet Child Adolesc. Health 2020; 4: 807–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Britton PN, Hu N, Saravanos G et al. COVID‐19 public health measures and respiratory syncytial virus. Lancet Child Adolesc. Health 2020; 4: e42–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yeoh DK, Foley DA, Minney‐Smith CA et al. Impact of COVID‐19 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin. Infect. Dis. 2020: ciaa1475. 10.1093/cid/ciaa1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Australian Influenza Surveillance Report . Reporting Fortnight: 16 to 29 November 2020. Canberra, Australia: Department of Health; 2020. [Google Scholar]
- 9. Virus Watch Week Ending 13th December 2020. Perth, Australia: Government of Western Australia Department of Health; 2020. [Google Scholar]
- 10. COVID‐19 Weekly Surveillance in NSW. Epidemiological Week 49, Ending 5 December 2020. Sydney, Australia: NSW Government Health Department; 2020. Available from: https://www.health.nsw.gov.au/Infectious/covid-19/Pages/weekly-reports.aspx. [accessed 1 December 2020]. [Google Scholar]
- 11. Kadambari S, Abo YN, Phuong LK, Osowicki J, Bryant PA. Decrease in infection‐related hospital admissions during COVID‐19: Why are parents avoiding the doctor? Pediatr. Infect. Dis. J. 2020; 39: e385–6. [DOI] [PubMed] [Google Scholar]
- 12. Victorian Weekly Influenza Report . Victoria State Government Health and Human Services. Melbourne, Australia: Victoria State Government Health and Human Services; 2020. Available from: https://www2.health.vic.gov.au/about/publications/researchandreports/seasonal‐influenza‐reports‐2020 [accessed 1 December 2020].
- 13. McNab S, Ha Do LA, Clifford V et al. Changing epidemiology of respiratory syncytial virus in Australia – Delayed re‐emergence in Victoria compared to WA/NSW after prolonged lock‐down for COVID‐19. Clin. Infect. Dis. 2021. 10.1093/cid/ciab240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cowling BJ, Ali ST, Ng TWY et al. Impact assessment of non‐pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020; 5: e279–88. [DOI] [PMC free article] [PubMed] [Google Scholar]


