ABSTRACT
Background
American Indian and Alaska Native (AI/AN) women have a higher risk of gestational diabetes mellitus (GDM) and subsequent diagnosis of diabetes than do non-Hispanic White women. Healthy eating is key to weight management both prior to pregnancy and between pregnancies and can reduce the risk of developing GDM. Our research team developed an innovative preconception counseling and diabetes risk-reduction program, which includes nutrition and weight-management principles and is culturally tailored for adolescent AI/AN women. The program is entitled Stopping Gestational Diabetes Mellitus (SGDM).
Objective
The purpose of this article is to examine nutrition-related information collected as a part of the formative qualitative research conducted for the development of a preconception counseling and gestational diabetes risk-reduction program, SGDM.
Methods
This in-depth secondary analysis explored the original qualitative data from the needs assessment for SGDM program development. Participants included AI/AN women with a history of GDM (n = 5); AI/AN girls at risk of GDM (n = 14), and their mothers (n = 11), health care providers, and health administrators who care for AI/AN girls (n = 16); AI/AN elected leaders; and Indian health system administrators (n = 12). All focus groups and interviews were reanalyzed utilizing the following research question: “How do key stakeholders discuss food and/or nutrition in terms of gestational diabetes risk reduction for AI/AN adolescent girls?”
Results
Three primary nutrition themes emerged: 1) AI/AN women were aware of healthy nutrition, healthy weight gain
during pregnancy, and healthy nutrition for people with type 2 diabetes, but these principles were not linked to reducing the risk of GDM; 2) participants expressed the need for education on the role of nutrition and weight management in GDM risk reduction; 3) participants shared challenges of healthful eating during and before pregnancy for AI/AN women.
Conclusions
These stakeholders’ comments informed the development of the nutrition components of SGDM.
Keywords: American Indian and Alaska Native, gestational diabetes, diabetes prevention, qualitative, diabetes nutrition education
We examined qualitative data to understand perspectives of key stakeholders regarding the role of nutrition in gestational diabetes mellitus (GDM) risk reduction for at-risk American Indian and Alaska Native women.
Introduction
Gestational diabetes mellitus (GDM) is one of the most common medical complications of pregnancy, affecting 2–10% of all United States (US) pregnancies (1). There has been a dramatic increase in the reported rates of GDM in the US, paralleled by the worldwide epidemic of obesity (2). Defined as glucose intolerance with onset during pregnancy, GDM and obesity can cause severe complications for both the mother and infant, and GDM is a significant risk factor for both of them to develop type 2 diabetes (T2D) later in life (3). GDM and obesity complications during pregnancy include maternal high blood pressure, preeclampsia, and high maternal risks of developing T2D in the future (3). GDM and obesity increase the risk of fetal macrosomia, birth trauma, hypoglycemia, hyperbilirubinemia, and hypocalcemia (3, 4) and increase the risk of obesity and T2D in the offspring (5). Women are more likely to develop GDM if they have high prepregnancy weight, elevated BMI, weight gain in young adulthood, a history of GDM or hypertension, and a family history of diabetes (6). American Indian and Alaska Native (AI/AN) women are twice as likely to have GDM and subsequent diagnosis of T2D than non-Hispanic white females (7). Thus, GDM and T2D as caused by obesity related to poor nutrition and physical inactivity create an intergenerational cycle of adverse health outcomes and highlight the importance of preconception health (8, 9).
Modifiable risk factors for developing GDM, such as elevated body weight and physical inactivity, can be addressed through education and support (10). Key modifiable environmental factors that impact individual behavior include increasing access to healthful food (11, 12) and safe places for physical activity (13). Research suggests that GDM risk-reduction and GDM-prevention programs that include diet education, physical activity, and lifestyle support can significantly improve the likelihood a woman will not be diagnosed with GDM (14–16). The American Diabetes Association Standards of Care designate nutrition as a cornerstone to diabetes self-management education and support for people with type 1 or 2 diabetes (17) as well as for women who have GDM (18). Furthermore, research suggests that when health education is culturally tailored for a specific audience, acceptance and engagement of the program is higher (19). This is true with diabetes nutrition education programs for AI/ANs as well (20, 21).
Given the increased risk of GDM for AI/AN women, and the lack of culturally tailored GDM risk-reduction resources for this audience (22), our team developed and evaluated a preconception counseling program to fill this gap called Stopping GDM in Daughters and Mothers (SGDM). SGDM was modified from a theory- and evidence-based preconception counseling and pregnancy-planning program for girls with existing diabetes, entitled READY-Girls (Reproductive-health Education and Awareness of Diabetes in Youth for Girls) (23). READY-Girls is theoretically supported by the Expanded Health Belief Model (EHBM) (24) and targeted girls who had existing diabetes. READY-Girls has also been shown to have positive long-term effects in reproductive health knowledge, beliefs, and intentions (25). The intent of the main study was to culturally adapt READY-Girls for AI/AN girls who are at risk of GDM and test the newly developed program (SGDM) in a randomized controlled trial in 5 AI/AN settings. The first year of this 5-y project involved a comprehensive qualitative needs assessment with key stakeholders to understand GDM risk-reduction and preconception counseling education needs from the perspective of the priority audience and health care providers who serve AI/AN women in health care capacities to inform the cultural adaptation of the program (20, 21). Details of the study team's cultural adaptation process will be reported elsewhere. Briefly, key adaptations include: the use of images, colors, and motifs that reflect the multigenerational diversity found among AI/AN families; the avoidance of directive language and the use of third person instead of, for example, “you should...”, the use of “real stories” of AI/AN women who have experienced GDM; and the use of messages of empowerment for AI/AN girls to make safer reproductive health choices. The purpose of this article is to examine nutrition-related information collected as a part of the formative qualitative research conducted for the development of a preconception counseling and gestational diabetes risk-reduction program entitled SGDM. (26).
Methods
Study design
During phase 1 of the 5-y main study, we conducted focus groups and individual interviews with key stakeholders to understand diverse perspectives on AI/AN adolescent GDM risk-reduction needs, and recommendations for a culturally and developmentally tailored program. We also sought to understand preferred methods of program delivery (i.e., paper booklet vs. eBook) and recommendations regarding specific content desired in such a program (27, 28). This input was used to inform the development of a GDM risk-reduction and preconception counseling program for AI/AN adolescent girls and young-adult women at risk of GDM.
We have now conducted a more in-depth analysis of themes from all focus groups and individual interviews in phase 1 of the main SGDM study (26) to understand the specific role of food and nutrition in GDM risk reduction among AI/AN communities from the perspective of our key stakeholders.
Recruitment and participants
Data for this secondary analysis included the initial stakeholder focus group participants: AI/AN girls (n = 13), their AI/AN mother or other adult female caregiver (n = 9), and AI/AN women with a history of GDM (n = 5). Of note, some of the mothers of the AI/AN girls also had a history of GDM. Two additional focus groups included one with tribal leaders (n = 12) and health care professionals/experts in AI/AN health, diabetes, reproductive health, GDM, and mother–daughter communication (n = 10). An additional 6 nationally known health care professionals/experts were interviewed one-on-one because they were not able to attend the focus group session. Six of these 16 health care providers/experts were also AI/AN. Tribal leaders were recruited from attendees at a national AI/AN health conference. A detailed description/methodology of the qualitative focus groups has been previously described (27, 28).
Data collection
As described in detail elsewhere (27, 28) we used a moderator guide of open-ended questions, with additional follow-up questions and probes, which varied depending on the response of the interviewee(s) (29) to facilitate semi-structured focus group and individual interviews. In addition, video snippets and booklet excerpts were used to elicit conversation and impressions of the original READY-Girls program. We chose to use focus group methods of qualitative data collection with AI/AN girls, their mothers, and women with a history of GDM to intentionally offset power dynamics between researcher and participant (29). Approval was received from the Colorado Multiple Institutional Review Board (COMIRB) and the approved protocol was followed. Per COMIRB guidelines, since this was a qualitative study and no identifying information was collected, we were granted a waiver of informed consent and instead participants received an information sheet explaining the purpose of the project.
Analysis
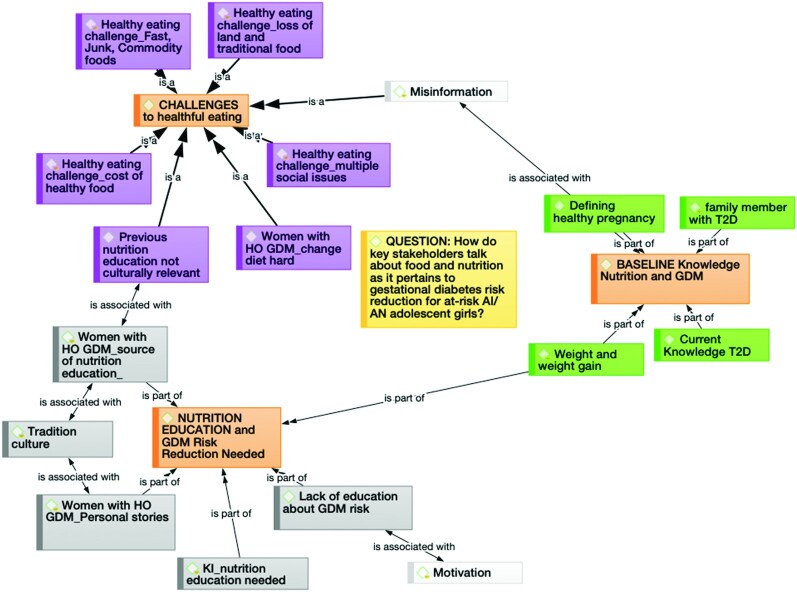
We conducted a more in-depth analysis of themes from the main SGDM study. This analysis specifically focused on food and nutrition as discussed by the participants, and the analysis was conducted by a trained qualitative researcher who is also a registered dietitian nutritionist. This secondary analysis of existing qualitative data used the constant comparison method (30). The constant comparison analytical approach included coding data, categorizing the codes, and reorganization of the categories into thematic representation through a series of assertions and interpretations (29, 31). Using this method, data were compared across transcriptions to find similarities and differences (31). This analytical technique allowed the researcher to collapse redundant codes, merge like codes, and begin to see relationships between codes for preliminary category development. We used both an inductive and deductive (a priori) coding approach (32). The deductive coding approach was informed by the moderator guide, and these deductive codes served as a basis for the first version of the codebook. For example, 1 deductive code was “healthy_pregnancy_defined” in response to the moderator guide question “Tell me what it means to be healthy for pregnancy,” in the case where participants responded with a food- or nutrition-focused answer. Additionally, inductive coding was used to code findings that emerged from the transcripts—for example, the code “healthy_eating challenge_cost” was generated this way. Transcripts were coded by 1 researcher and codes, categories, and themes were discussed within the research team. All transcripts were analyzed in their entirety, however, not every focus group discussion included relevant dialogue related to this specific research question. We used Atlas.ti (Mac version 8.1.1, ATLAS.ti Scientific Software Development GmbH) to organize transcripts and code data to digitalize the analytic process. A graphic representation of how codes were constructed into categories and overarching themes using Atlas.ti (Mac version 8.1.1) can be found in Figure 1.
FIGURE 1.
A graphic representation of how codes were constructed into categories and overarching themes using Atlas.ti (Mac version 8.1.1; ATLAS.ti Scientific Software Development GmbH). AI/AN, American Indian and Alaska Native; GDM, gestational diabetes mellitus; HO, history of; KI, Key informant; T2D, type 2 diabetes.
Results
Three key nutrition-related themes were constructed across all qualitative data-collection methods. These include the following: 1) AI/AN women were aware of healthy nutrition, healthy weight gain during pregnancy, and healthy nutrition for people with T2D, but these principles were not linked to reducing the risk of GDM; 2) participants expressed the need for education on the role of nutrition and weight management in GDM risk reduction; 3) participants shared challenges of healthful eating during and before pregnancy for AI/AN women.
Theme 1: AI/AN women were aware of healthy nutrition, healthy weight gain during pregnancy, and healthy nutrition for people with T2D, but these principles were not linked to reducing the risk for GDM
AI/AN girls, their mothers, and women with a history of GDM understood and verbalized the importance of nutrition in terms of how to be healthy for pregnancy. When questioned to elaborate on her comment about what “healthy eating” means to her, one AI/AN girl shared the following:
‘It means just having balanced meals and incorporating proteins and fruits and vegetables into your diet. Probably staying away from carbs so you don't put on extra weight, and not eating a lot of sugar.’
In response to the question “how can women stay healthy during a pregnancy” another AI/AN girl shared the following:
‘By eating lots of fruits and vegetables, and cutting out bad things from your diet, like junk food and coffee, and not smoking, using drugs, alcohol, and lots of exercise, and sleep. And junk food like lots of chips and stuff like that. I know you're not supposed to have cold deli meats, certain cheeses that don't melt down. Hot dogs … stuff like chips, candy, and stuff like that. Lots of sugar that's not from fruits, unnatural. It's pretty bad for you.’
Participants also understood the importance of managing weight gain during pregnancy in order to not gain “too much weight.” One AI/AN woman with a history of GDM shared her thoughts on having a healthy pregnancy:
‘Not overeating. Not saying just because you're pregnant that you have to eat for two. Staying physically active, mostly after your meals, to digest your food better, to lower your blood sugar levels.’
Participants also shared what they knew about weight gain for a healthy pregnancy, as shared by this AI/AN mother:
‘I think you're supposed to gain—I think it varies on the size that you are already, depending on how much food you intake, and nutrition and stuff like that. But depending on the person, I think, you're, on average, supposed to gain 30 pounds or something during a pregnancy.’
Although participants shared knowledge about healthy eating for pregnancy and healthy weight gain for pregnancy, none mentioned these are principles to reduce one's risk for GDM. Specifically, when asked about GDM, 1 woman with a history of GDM shared her diagnosis story:
‘I remember doing that [blood sugar testing]. I just thought—the way my doctor said, “Oh, this is just the regular routine diabetes test we do with all pregnant women.” But he didn't use the term “gestational.” My original doctor didn't explain anything to me. So I was just totally oblivious to it. Didn't really pay no mind or worry about it, or think that I had to worry about it, or prepare for it, or anything. I was just thinking, “No, I'm not diabetic. I know this.” I know it runs in my family, and on both sides, and almost the majority of all my family members have it on my mom's side. And both my parents are Natives. I just didn't know anything—and no one ever told me I could have prevented it or done something to prevent it.’
Together, these quotes exemplify the baseline knowledge about healthy nutrition and weight management prior to and during pregnancy. Yet, they also suggest there is a disconnect between nutrition/weight management and GDM risk reduction.
Theme 2: Participants expressed the need for education on the role of nutrition and weight management in GDM risk reduction
AI/AN women with a history of GDM shared what they wished they had known prior to their own diagnosis, and what they would want their daughters or other AI/AN women to know. One AI/AN mother who had a history of GDM shared:
‘I don't know, I think for Native women, it'd be nice to know that we're at a way higher risk of developing diabetes, no matter what body type you have. Especially for me, it was like, oh my gosh, now I have a higher chance of developing diabetes after I have him, or later on in life, that increases my chances. And then for my kids, too. So it's a scary thing. I know now it's preventable, but it's still something you don't want to have, or have to live with the rest of your life.’
Another AI/AN woman with a history of GDM shared how her experience with GDM has impacted the nutrition practices of her whole family:
‘Even now, as a mom and that I had gestational diabetes, it really changed the way that my whole household eats. Like we don't eat so much pasta. We don't eat food like that, because of the carbs, because it's a white food. And I'm just—we don't have that many sweets. I'm just so—not worried, but I'm just so—I want to give her that knowledge to eat right, right now. And all my kids—even my husband, I really try to get him to eat good.’
In response to what kind of GDM risk-reduction education we need to include in the SGDM program, 1 health care provider who was also AI/AN shared the following:
‘I just wanted to say… the focus is to help prevent gestational diabetes—so preconception health, to prevent GDM, to strengthen Native families. Like the food issue, okay, so how do we eat healthier? … we can put more frozen fruits in our freezers so that we have them. … Our girls are our future mothers, so it's to say... I think, in a way to empower them, to say nobody's alone in this. We're trying to make things better so that you can be strong mothers when you're ready.’
An AI/AN woman with a history of GDM shared the pain and stigma of having GDM, suggesting that education for the entire AI/AN community (not just women at risk of GDM) would be beneficial:
‘I think for me, I just shared that it was embarrassing for me to tell people that I had gestational diabetes, because I felt that they were already blaming me, like, “How did you do [that]—what did you eat? What were you doing? How were you taking care of yourself, how did you get that?” And then my family members, of course, were like, “You don't look like you have it,” or, “You don't look unhealthy, you don't look overweight.” And it's just like, but it's not that. It's deeper. Yeah, there is a stigma to it, just like everything else. Like everything else with being Native American. But I would say, put in here that it's not your fault, you didn't do anything wrong, it's something that happens, it's out of your control—because that was the one thing I… that was the issue I had where it was, I couldn't control that. It was something that I could not control, but I could keep it under control. So I would say to reiterate that, especially to a young mom.’
Finally, women shared concerns that nutrition education they received was not culturally relevant nor did it provide the support they needed to make healthful changes. One AI/AN woman with a history of GDM shared the following:
‘Well, when I went to the doctor, the dietitian and my doctor just said, “If you don't watch what you eat, or if you're not maintaining a good, healthy diet—especially because you have gestational diabetes—you could have an overweight baby, and then they will be more at risk for developing diabetes later on.” And it goes against me, too, because we're Native American. And it runs in our family already. So it's already in our genes. I think that makes it harder for us, but they didn't talk about that.’
Theme 3: Participants shared many challenges of healthful eating during and before pregnancy for AI/AN women
These challenges to healthful eating include food insecurity, loss of traditional food-acquisition habits, and easy access to fast and processed food. When asked about challenges to healthy eating, one mother who had a history of GDM shared the following:
‘Yeah, and it's easier just to go pick up a 99-cent burger … or even going to the grocery store is hard because everything is so filled with preservatives, or expensive, period… A lot of Native families are pretty big, so it's hard to feed all your kids and … healthy, on a tight income.’
When asked to elaborate on what she meant by “eat healthy” 1 AI/AN girl shared,
‘Like more fruits or vegetables, or organic stuff. I know it's hard to eat more healthy because it's a little more expensive, but really trying to stay away from the fast food stuff, a lot of things with high fat, or overeating.’
In addition to sharing the financial challenges of eating healthy, this same AI/AN girl went on to share,
‘I know a lot of people—with Natives, when you're visiting relatives and stuff, you tend to, “Let's eat,” gotta feed them. So sometimes—especially when you're visiting family—you can go to three or four different houses in a few days and you just tend to eat a lot. And when you're pregnant, that's probably not very healthy and stuff.’
When reviewing the existing READY-Girls booklet, 1 AI/AN tribal leader referenced a page in the booklet that mentioned the benefit of eating “healthy foods” and shared the following:
‘I mean, what are healthy foods? It says “eat fruits and vegetables”—but, first of all, you can tell in a lot of our communities—do they even know how to access healthy foods like that? So, it probably needs more information there.’
After conversation about challenges to healthy eating, 1 AI/AN mother shared her experience with taking her sister, who had been diagnosed with GDM, to receive medical care for her GDM:
‘I think that would be good to have this information brought to the nutritionist [this information meaning financial limitations in purchasing healthy food]. Because … she [sister] was diagnosed with being obese, so we went to see a nutritionist…I know we went a few times, but then she got tired of hearing the same thing from her [nutritionist], because it was more of the nagging, “Are you doing this? Are you doing that?” And there's just a lot of things to play into that role and it all goes back to eating healthy. And a lot of Natives can't because it's expensive to try and eat healthy. She [nutritionist] offered us food banks and things like that, which is fine, but when you go to the food banks, they don't offer you healthy food and stuff like that.’
Finally, participants shared concerns about loss of traditional food and food-acquisition practices and how that impacts rates of diabetes in AI/AN communities. In response to the moderator probing a statement about loss of traditional foods, one AI/AN mother shared the following:
‘Or just … our food being colonized. People are really obsessed with fry bread; that's not a traditional food. It's really awful, and people are obsessed with eating it and having it. I wonder [about] the pathway of fry bread leading to diabetes. I think so. I think that has a lot to do with it, just because on the reservation, any time they have a dinner for anything, there's always fry bread for it. That was like a survival food. Yeah, that was like a survival food, just because of the flour and all of the ingredients. All of the commodities, yeah. So I think it was just what they had, they had to make do with it.’
Discussion
Collectively, these findings confirmed the importance of a culturally tailored nutrition component of a gestational diabetes risk-reduction and preconception counseling education program for AI/AN girls. Specifically, findings suggest participants were knowledgeable about healthy nutrition for pregnancy but not as it relates to GDM risk reduction; they wanted more education about GDM risk reduction specific to nutrition and weight management, and they were vocal about challenges of healthy eating before and during pregnancy. Together, these findings suggest further education for both health care providers who care for AI/AN women and the women themselves on healthy weight management and specific nutrition education that addresses barriers to healthful eating. This education might focus on food resource management such as healthy eating on a budget, and for health care providers—education on food aid services offered in their communities, to assist families with financial barriers to accessing healthful food. The Policy, Systems, Environment (33) approach to nutrition education also supports addressing social determinants of health including the built food environment. This could be addressed by educating health care administrators on systems approaches to improving healthy food access such as fruit and vegetable prescription programs (34–36) This in-depth secondary data analysis confirmed the nutrition themes that informed the development of SGDM, as nutrition-specific focused analysis was not possible due to limitations in time and resources during the initial data analysis period (26).
In general, GDM risk reduction focuses on healthy weight management both prior to conception and during pregnancy through healthful diet and physical activity (33–35). GDM-prevention education typically focuses on women postpartum after having GDM, with weight-management principles to prevent T2D later in life (7, 8). SGDM is innovative in that it is a preconception counseling program that targets AI/AN adolescent girls at risk of GDM prior to developing GDM. The goal is to initiate preconception counseling prior to sexual debut so that each pregnancy is planned and a healthy weight attained prior to all pregnancies. When asked “how to be healthy for pregnancy?” participants in this study almost always mentioned healthy nutrition first. When probed further to talk about what “healthy nutrition” means to them, they correctly shared basic weight-management and nutrition principles such as eating more fruits and vegetables, eating less processed food, eating less “junk” food. Further, these participants mentioned the importance of appropriate weight gain for pregnancy and cautioned about gaining “too much weight.” However, when asked about gestational diabetes risks and prevention strategies, participants admitted they had not learned these concepts and, for women with a history of GDM, they did not learn about “healthy GDM nutrition” management principles until after they were diagnosed with GDM.
There is a paucity in the literature about GDM risk reduction and prevention and most “prevention” emphasis for GDM is actually on the prevention of T2D postpartum, after having GDM. Reputable gestational diabetes education resources rarely include information on GDM risk reduction, such as the March of Dimes webpage on Gestational Diabetes (36), which focuses on how to manage GDM after it is diagnosed. To support participants’ understanding of healthy eating and weight management as key factors in maintaining a healthy pregnancy weight and reducing risk of GDM, the SGDM program developers drew on education theories that specify effective pedagogical approaches to health care that include building on existing knowledge and tying existing knowledge to new concepts (37). For example, the section in the SGDM book that focuses on healthy eating includes language about the congruencies between healthy eating for pregnancy and healthy eating for GDM risk reduction.
In addition to increasing GDM risk-reduction education and resources for AI/AN women who may be at risk of GDM, participants suggested the importance of educating the broader AI/AN community. This may help decrease stigma and “blame” associated with GDM and, as several participants shared, GDM healthy-eating principles are of benefit to the whole family. As supported by the literature (38), SGDM provides a family-based approach to the program, with a special focus on including adult female caregivers as role models and support persons for AI/AN girls. Both the SGDM video and eBook include scenes and images on family-based food preparation and sharing meals to promote healthful eating. Additionally, SGDM focuses on empowering young women to make healthy food and beverage choices and the educational video includes a variety of AI/AN women sharing their stories and experience with GDM as a means to connect with younger viewers and help de-stigmatize the diagnosis.
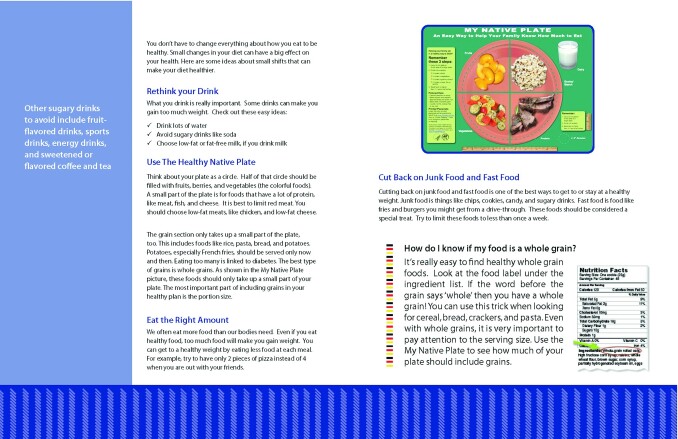
The SGDM program is based on the preconception counseling program READY-Girls, which is theoretically grounded in the EHBM (24). Specific constructs from the EHBM include perceived risk and susceptibility and are depicted in the SGDM book and video with a reference to prepregnancy body weight as a risk factor and a recommendation for weight management and nutrition as primary ways to reduce GDM risk. The EHBM construct of self-efficacy also supports the inclusion of small changes as management tips and recommendations to improve healthy eating. The SGDM booklet reinforces that small changes can make a big effect and highlights the Native Plate as a tool for healthy meal planning as shown in Figure 2.
FIGURE 2.
Example of pages from SGDM book reproduced from reference (55) with permission.
Participants in this study also shared challenges to healthful eating. Many of these challenges are related to limited access to healthy food and the cost of healthy food. The United States Department of Agriculture defines food insecurity as lack of consistent access to enough food for an active, healthy life (39). The literature suggests that AI/ANs are disproportionately impacted by food insecurity (40–43) and are more likely to live in food deserts than any other racial group, which can also contribute to food insecurity (44–46). Map the Meal Gap data from 2014 indicates counties with American Indian reservations have significantly higher rates of food insecurity than neighboring counties (47). Furthermore, a growing body of research indicates that food insecurity can contribute to unwanted weight gain in both adults and children (41, 48, 49). Additionally complicating access to healthy foods for AI/AN people includes the lasting impacts of the Indian Relocation Act of 1956 (50), which encouraged AI/ANs to leave their traditional lands and to assimilate into urban areas—leading to loss of access to traditional food-acquisition practices such as hunting, fishing, and gathering (51). This loss has greatly contributed to lack of access to healthful foods, as traditional cultural foods are less processed, contain less refined flour and sugar, less saturated fat, and more fiber than modern Western foods (52, 53). Participants also shared that excessive access to processed and “fast food” can make healthy eating a challenge. Some research suggests that over-access to processed foods can more negatively impact body weight than living in a food desert (54).
Strengths of this study include the multiple vantage points from key stakeholders, use of focus groups to intentionally offset power dynamics between participant and researcher, locations of focus groups and interviews in places familiar and comfortable to the participants, and expertise in qualitative data collection and analysis. Limitations include the small sample size and convenience sampling of AI/AN girls, their mothers, and AI/AN women with a history of GDM. Furthermore, as is the nature of qualitative research, these findings are not generalizable beyond the experiences of these particular participants.
In conclusion, this focused secondary analysis will inform revisions and additions to the original SGDM program. For example, additional information may be added to the program specifically addressing barriers to healthy nutrition habits as discussed by these participants. The SGDM program is a paradigm shift in counseling and educating women about GDM, because it targets adolescent girls prior to any pregnancy, decreasing their risk of any incidence of GDM, to break the cycle of diabetes in families. We have developed the SGDM program so it is free and available in its entirety at www.stoppinggdm.com. As a strategic component of the broader SGDM study, we are disseminating the program broadly throughout Indian Country in collaboration with AI/AN community partners through a series of webinars, national academic presentations, and local community-based presentations. SGDM would be appropriate for use in health classes in schools, as a “prescription” from a health care provider, or as part of the Special Supplemental Nutrition Assistance Program for Women, Infants, and Children (WIC).
ACKNOWLEDGEMENTS
The SGDM Study Group includes the following: Aletha Akers, Sandra Beirne, Angela G Brega, Laura Chalmers, Denise Charron-Prochownik, Andrea Fischl, Heather Garrow, Kelly Gonzales, Jean Howe, Gale Marshall, Kristie McNealy, Kelly Moore, Kristen Nadeau, Nancy O'Banion, Jeff Powell, Ellen Seely, Susan Serika, Howard Stein, Sarah A Stotz, Martha A Terry, Shelly Thorkelson, and Xochil Uribe-Rios.
The authors’ responsibilities were as follows—SAS: collected data, analyzed qualitative data, drafted the manuscript, and revised all versions of the manuscript; DC-P: designed the research, oversaw all data collection and analysis, and provided substantial revisions and critical feedback on all drafts of the manuscript; MAT: collected qualitative data and analyzed quantitative data; GM: collected qualitative data; ARF: provided substantial revisions and critical feedback to the first draft of this manuscript; KRM: designed the research, oversaw all data collection and analysis, provided substantial revisions and critical feedback on all drafts of the manuscript, and has primary responsibility for final content; and all authors: read and approved the final manuscript.
Notes
Supported by the NIH–National Institute of Nursing Research (1R01NR014831-01A1).
Author disclosures: The authors report no conflicts of interest. KRM received funding (registration fee and lodging) to attend the 2019 Seeds of Native Health conference as she was a member of the 2019 conference planning committee. All other travel expenses were paid from her own grant funding.
This article appears as part of the supplement “Proceedings of the Fourth Annual Conference on Native American Nutrition,” sponsored by the Shakopee Mdewakanton Sioux Community's Seeds of Native Health campaign through a gift to the University of Minnesota. The guest editor of the supplement is Mindy S Kurzer. MSK is supported by the Shakopee Mdewakanton Sioux Community for her role as chair of the conference planning committee and editing the proceedings. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Current Developments in Nutrition.
Abbreviations used: AI, American Indian; AN, Alaska Native; COMIRB, Colorado Multiple Institutional Review Board; EHBM, Expanded Health Belief Model; GDM, gestational diabetes mellitus; SGDM, Stopping Gestational Diabetes Mellitus; READY-Girls, Reproductive-health Education and Awareness of Diabetes in Youth for Girls; T2D, type 2 diabetes.
Contributor Information
Sarah A Stotz, Email: sarah.stotz@cuanschutz.edu, University of Colorado Anschutz Medical Campus; Colorado School of Public Health, Centers for American Indian and Alaska Native Health, Aurora, CO, USA.
Denise Charron-Prochownik, University of Pittsburgh, Nursing and Graduate School of Public Health, Department of Health Promotion and Development, Pittsburgh, PA, USA.
Martha A Terry, University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA, USA.
Gale Marshall, Two Feathers Media, LLC, Canton, NC, USA.
Andrea R Fischl, University of Pittsburgh, Nursing and Graduate School of Public Health, Department of Health Promotion and Development, Pittsburgh, PA, USA.
Kelly R Moore, University of Colorado Anschutz Medical Campus; Colorado School of Public Health, Centers for American Indian and Alaska Native Health, Aurora, CO, USA.
SGDM Study Team:
Aletha Akers, Sandra Beirne, Angela G Brega, Laura Chalmers, Denise Charron-Prochownik, Andrea Fischl, Heather Garrow, Kelly Gonzales, Jean Howe, Gale Marshall, Kristie McNealy, Kelly Moore, Kristen Nadeau, Nancy O'Banion, Jeff Powell, Ellen Seely, Susan Serika, Howard Stein, Sarah A Stotz, Martha A Terry, Shelly Thorkelson, and Xochil Uribe-Rios
References
- 1. Centers for Disease Control and Prevention . Gestational diabetes. Atlanta (GA): Centers for Disease Control and Prevention, Atlanta, GA; 2019, Available from: https://www.cdc.gov/diabetes/basics/gestational.html. [Google Scholar]
- 2. American Diabetes Association . Standards of medical care in diabetes. Diabetes Care. [Internet]2020;43(Suppl 1):S183. Available from: http://care.diabetesjournals.org/content/43/Supplement_1/S1.abstract. 10.2337/dc20-S014. [DOI] [PubMed] [Google Scholar]
- 3. American Diabetes Association . American Diabetes Association, Proceeding of the Fifth International Workshop—Conference on Gestational Diabetes Mellitus. Diabetes Care. 2007;30(Supp 2, 10.2337/dc07-s225). [DOI] [Google Scholar]
- 4. Wong T, Ross G, Jalaudin B, Flack J. The clinical significance of overt diabetes in pregnancy. Diabetes Metab Syndr Clin Res Rev. 2013;30(4):468–74. [DOI] [PubMed] [Google Scholar]
- 5. Pettitt D, Jovanovic L. The vicious cycle of diabetes and pregnancy. Curr Diab Rep. 2007;7:295–7. [DOI] [PubMed] [Google Scholar]
- 6. Beckles G, Thompson-Reid P. Diabetes and women's health across the life stages: a public health perspective. Atlanta (GA): US Department of Health and Human Services; Centers for Disease Control and Prevention; 2001. [Google Scholar]
- 7. Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(Suppl 2):S141–6. [DOI] [PubMed] [Google Scholar]
- 8. Barker J, Su F, Alwan NA. Risk factors for type 2 diabetes after gestational diabetes: a population-based cohort study. Lancet [Internet]. 2017;390:S21, 10.1016/S0140-6736(17)32956-2. [DOI] [Google Scholar]
- 9. Stephenson J, Heslehurst N, Hall J, Schoenaker D, Hutchinson J, Cade JE, Poston L, Barrett G, Cozier SR, Barker Met al. Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet [Internet]. 2018;391(10132):1830–41., 10.1016/S0140-6736(18)30311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Evert AB, Vande Hei K. Gestational diabetes education and diabetes prevention strategies. Diabetes Spectr. 2006;19(3):135–9. [Google Scholar]
- 11. Breland JY, McAndrew LM, Gross RL, Leventhal H, Horowitz CR. Challenges to healthy eating for people with diabetes in a low-income, minority neighborhood. Diabetes Care. 2013;36(10):2895–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blue Bird Jernigan V, D'Amico EJ, Duran B, Buchwald D. Multilevel and community-level interventions with native americans: challenges and opportunities. Prev Sci. 2018;(Trickett 2009):1–9., 21, doi: 10.1007/s11121-018-0916-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Madhuvrata P, Govinden G, Bustani R, Song S, Farrell TA. Prevention of gestational diabetes in pregnant women with risk factors for gestational diabetes: a systematic review and meta-analysis of randomised trials. Obstet Med. 2015;8(2):68–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Koivusalo SB, Rönö K, Klemetti MM, Roine RP, Lindström J, Erkkola M, Kaaja RJ, Poyhonen-Alho M, Titinen A, Huvinen Eet al. Gestational diabetes mellitus can be prevented by lifestyle intervention: the Finnish Gestational Diabetes Prevention Study (RADIEL): a randomized controlled trial. Diabetes Care. 2016;39(1):24–30. [DOI] [PubMed] [Google Scholar]
- 16. Rönö K, Stach-Lempinen B, Eriksson JG, Pöyhönen-Alho M, Klemetti MM, Roine RP, Huvinen E, Andersson S, Laivori H, Valkama Aet al. Prevention of gestational diabetes with a prepregnancy lifestyle intervention—findings from a randomized controlled trial. Int J Womens Health. . [Internet].2018;10:493–501. Available from: https://www.dovepress.com/prevention-of-gestational-diabetes-with-a-prepregnancy-lifestyle-inter-peer-reviewed-article-IJWH, doi: 10.2147/IJWH.S162061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. American Diabetes Association . Improving care and promoting health in populations: standards of medical care in diabetes. Diabetes Care. 2018;41(Suppl 1):S7–12. [DOI] [PubMed] [Google Scholar]
- 18. American Diabetes Association . Management of diabetes in pregnancy: standards of medical care in diabetes. Diabetes Care. 2018;41(Suppl 1):S137–43., S126–36. [DOI] [PubMed] [Google Scholar]
- 19. Kreuter MW, Lukwago SN, Bucholtz R, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–46. [DOI] [PubMed] [Google Scholar]
- 20. Kattelmann KK, Conti K, Ren C. The Medicine Wheel Nutrition Intervention: a diabetes education study with the Cheyenne River Sioux Tribe. J Am Diet Assoc [Internet]. 2009;109(9):1532–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Conti KM. Diabetes prevention in Indian Country: developing nutrition models to tell the story of food-system change. J Transcult Nurs. 2006;17(3):234–45. [DOI] [PubMed] [Google Scholar]
- 22. Moore K, Stotz S, Fischl A, Beirne S, McNealy K, Abujaradeh H, Charron-Prochownik D. Pregnancy and gestational diabetes mellitus (GDM) in North American Indian adolescents and young adults (AYA): implications for girls and stopping GDM. Curr Diab Rep [Internet]. 2019;19:(11):113. [Accessed 2020 May 28]. Available from: 10.1007/s11892-019-1241-3. [DOI] [PubMed] [Google Scholar]
- 23. Charron-Prochownik D, Downs J. READY-Girls. Pittsburgh (PA): University of Pittsburgh; 2009. [Google Scholar]
- 24. Burns A. The Expanded Health Belief Model as a basis for enlightened preventive health care practice and research. J Health Care Mark. 1992;12(3):32–45. [PubMed] [Google Scholar]
- 25. Charron-Prochownik D, Sereika S, Becker D, White N, Schmitt P, Powell A, Diaz MA, Jones J, Herman W, Rogers Fischl AFet al. Long-term effects of the booster enhanced READY-Girls preconception counseling program on intentions and behaviors for family planning in teens with diabetes. Diabetes Care. 2013;36(12):3870–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ruggiano N, Perry TE. Conducting secondary analysis of qualitative data: should we, can we, and how?. Qual Soc Work. 2019;18(1):81–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Stotz SA, Charron-Prochownik D, Terry MA, Gonzales K, Moore KR. Reducing risk for gestational diabetes mellitus (GDM) through a preconception counseling program for American Indian/Alaska Native girls: perceptions from women with type 2 diabetes or a history of GDM. Diabetes Educ. 2019;45(2):137–45. [DOI] [PubMed] [Google Scholar]
- 28. Moore K, Stotz S, Nadeau KJ, Terry MA, Garcia-Reyes Y, Gonzales K, Charron-Prochownik D. Recommendations from American Indian and Alaska Native adolescent girls for a community-based gestational diabetes risk reduction and reproductive health education program. Res J Women's Heal. 2019;6(1):1. [Google Scholar]
- 29. Roulston K. Reflective interviewing. Los Angeles (CA): Sage Publications; 2010. [Google Scholar]
- 30. Anafara VA, Brown KM, Magione TL. Qualitative analysis on stage: making the research process more public. Educ Res. 2002;31(7):28–38. [Google Scholar]
- 31. Charmaz K. Constructing grounded theory. 2nd ed. Los Angeles (CA): Sage Publications; 2014. [Google Scholar]
- 32. Saldaña J. The coding manual for qualitative researchers. 2nd ed. Thousand Oaks (CA): Sage Publications; 2012. [Google Scholar]
- 33. Contento I, Balch GI, Bronner YL, et al. The effectiveness of nutrition education and implications for nutrition education policy, programs, and research: a review of research. J Nutr Educ. 1995;27:279–418., 3. [Google Scholar]
- 34. Ridberg RA, Bell JF, Merritt KE, et al. , Effect of a fruit and vegetable prescription program on children’s fruit and vegetable consumption. Prev Chronic Dis. 2019;16(6):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tier J, Sheppard E, Middleton P, Crowther C. Diet or exercise, or both, for preventing excessive weight gain in pregnancy [review]. Cochrane Database Syst Rev. 2015;1:1465–858.. doi: 10.1002/14651858.CD010443.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Swartz H, Produce RX programs for diet-based chronic disease prevention. AMA J Ethics. 2018; 20(10): 960–973..doi: 10.1001/amajethics.2018.960. [DOI] [PubMed] [Google Scholar]
- 37. Knowles M. Andragogy in action. San Francisco (CA): Jossey-Bass; 1984. [Google Scholar]
- 38. McLaughlin S. Traditions and diabetes prevention: a healthy path for Native Americans. Diabetes Spectr. 2010;23(4):272–7. [Google Scholar]
- 39. USDA . Definitions of food security. Washington (DC): Economic Research Service; 2019. [Google Scholar]
- 40. Jernigan VBB, Huyser KR, Valdes J, Simonds VW. Food insecurity among American Indians and Alaska Natives: a national profile using the current Population Survey–Food Security Supplement. J Hunger Environ Nutr. 2017;12(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bauer KW, Widome R, Himes JH, Smyth M, Rock BH, Hannan PJ, Story M. High food insecurity and its correlates among families living on a rural American Indian reservation. Am J Public Health. 2012;102(7):1346–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pardilla M, Prasad D, Suratkar S, Gittelsohn J. High levels of household food insecurity on the Navajo Nation. Public Health Nutr. 2014;17(1):58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gundersen C. Measuring the extent, depth, and severity of food insecurity: an application to American Indians in the USA. J Popul Econ. 2008;21(1):191–215. [Google Scholar]
- 44. Jernigan VBB, Garroutte E, Krantz EM, Buchwald D. Food insecurity and obesity among American Indians and Alaska Natives and whites in California. J Hunger Environ Nutr. 2013;8(4):458–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. O'Connell M, Buchwald DS, Duncan GE. Food access and cost in American Indian communities in Washington State. J Am Diet Assoc. 2011;111(9):1375–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kaufman P, Dicken C, Williams R. Measuring access to healthful, affordable food in American Indian and Alaska Native Tribal areas. 2014;(131):29.[Internet].[Cited 2020 May 20]. Available from: https://permanent.access.gpo.gov/gpo55515/eib131.pdf. [Google Scholar]
- 47. Gundersen G, Dewey A, Crumbaugh A. et al. Map the Meal Gap 2016: food insecurity and child food insecurity estimates at the county level. 2016, Feeding America, Chicago, IL. [Google Scholar]
- 48. Adams AK, Tomayko E, Cronin K, Prince RJ, Kyungmann K, Carmichael L, Parker T. Predictors of overweight and obesity in American Indian families with young children. J Nutr Educ Behav. 2018;51(2):190–8. [Internet]. [Cited 2020 May 28]. doi: 10.1016/j.jneb.2018.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tomayko EJ, Mosso KL, Cronin KA, Carmichael L, Kim K, Parker T, Yaroch A, Adams A. Household food insecurity and dietary patterns in rural and urban American Indian families with young children. BMC Public Health. 2017;17(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Indian Relocation Act of 1956 . In: An Act relative to employment for certain adult Indians on or near Indian reservations. Indian Relocation Act of 1956; Enacted by the 84th United States Congress. World; Heritage Encyclopedia. [Google Scholar]
- 51. Gurney RM, Caniglia BS, Mix TL, Baum KA. Native American food security and traditional foods: a review of the literature, Sociology Compass. 2015;8:681–93. [Google Scholar]
- 52. Centers for Disease Control and Prevention . Traditional Foods Project 2008–2014. [Internet]. Native Diabetes Wellness Program. [cited 2019 Nov 17]. Available from: https://www.cdc.gov/diabetes/ndwp/traditional-foods/index.html. [Google Scholar]
- 53. Coté C. “Indigenizing” food sovereignty. Revitalizing indigenous food practices and ecological knowledges in Canada and the United States. Humanities. [Internet].2016;5(3):57. Available from: http://www.mdpi.com/2076-0787/5/3/57, doi: https://doi.org/10.3390/h5030057. [Google Scholar]
- 54. Cooksey-Stowers K, Schwartz MB, Brownell KD. Food swamps predict obesity rates better than food deserts in the United States. Int J Environ Res Public Health. 2017;14(11):1–20., doi 10.3390/ijerph14111366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Charron-Prochownik D, Moore K, Stotz S. Daughters and Mothers Stopping Gestational Diabetes Mellitus: Balancing Body, Mind and Spirit. 2017. Pittsburgh: University of Pittsburgh. [Google Scholar]