Abstract
Background
Rehabilitation outcomes of patients with coronavirus disease 2019 (COVID‐19) are unknown.
Objective
To describe patients with COVID‐19 who are undergoing inpatient rehabilitation and their rehabilitation outcomes.
Design
Retrospective observational cohort study of all inpatients from a rehabilitation hospital between March 1 and September 30, 2020.
Setting
Inpatient rehabilitation hospital.
Patients
Among all inpatients, inclusion criteria are: ≥18 years of age and admission and discharge within the study time frame. The initial search yielded 920 patients; 896 met the inclusion criteria. Subjects were stratified by COVID‐19 status and rehabilitation impairment.
Main Outcome Measures
Data included age, gender, body mass index (BMI), length of stay (LOS), discharge location, and functional ability in self‐care and mobility (FA‐SC, FA‐Mob). One‐sample t‐tests were used to assess the difference of age, BMI, LOS, FA‐SC, FA‐Mob, and FA efficiency between COVID‐19+ and COVID‐19− patients.
Results
COVID‐19+ patients were younger (59.4 years vs 62.9 years; t[894] = −2.05, p = .04) with a higher mean BMI (32 vs 28; t[894] = 3.51, p < .01) than COVID‐19− patients. COVID‐19+ patients had equivalent or superior improvements in FA‐SC and FA‐Mob, functional change efficiency, and LOS relative to COVID‐19− patients. When medically complex patients were compared, those with COVID‐19 had greater FA‐SC and FA‐Mob efficiencies than COVID‐19− patients. COVID‐19+ patients had similar rates of return to the community.
Conclusions
Patients with COVID‐19 who meet the admission criteria for inpatient rehabilitation can benefit from inpatient rehabilitation similarly to their non‐COVID‐19 counterparts with similar rehabilitation‐specific diagnoses.
INTRODUCTION
The first case of coronavirus disease 2019 (COVID‐19) traces back to China on November 17, 2019 and appeared in the United States on January 20, 2020; thereafter, the World Health Organization officially announced a global pandemic (on March 11, 2020). All sectors of medicine have been severely affected, including rehabilitation medicine.
Rehabilitation clinicians and programs have had to undertake the new challenge of delivering safe, effective, and efficient rehabilitation for patients who are recovering from COVID‐19 and other traditional rehabilitation diagnoses within the frequently changing environment(s) and restrictions imposed by this unprecedented pandemic. Early programmatic changes during the pandemic included increased inpatient acute care and rehabilitation bed capacity (up to 50%), development of COVID‐19 specific recovery/precaution units, prohibition of visitors, limiting/elimination of in‐person family and caregiver training, and transition of multidisciplinary team rounds to a virtual setting. 1 , 2 Patient rehabilitation plans of care were shortened, and patients were discharged from inpatient settings more quickly in order to maintain bed availability for incoming COVID‐19 patients and to reduce the risk of patients contracting COVID‐19 while in the hospital. As such, a significant amount of rehabilitation was transitioned to virtual outpatient therapies. 3 , 4 , 5
As the pandemic continues throughout the world and in the United States, the evidence base on post‐acute rehabilitative care of COVID‐19 patients is just beginning to emerge. Much of the literature to date has focused on early effects of COVID‐19 on rehabilitation systems and proposed protocols for rehabilitation during COVID‐19 recovery. 6 , 7 , 8 At the patient level, links to comorbidities observed in COVID‐19 patients requiring intensive care include muscle weakness, nerve damage, delirium, and others, which have the potential to significantly impact their physical and cognitive function. 9 , 10 , 11 , 12 Furthermore, existing respiratory rehabilitation approaches have been modified and applied to those with COVID‐19 and respiratory involvement; however, the effectiveness of these methods has not yet been assessed. 6 , 13 , 14 , 15
The purpose of this study is to describe the characteristics and post‐acute rehabilitation outcomes of people with COVID‐19 undergoing inpatient rehabilitation to inform post‐acute rehabilitative care. Specifically, we compare patients with a positive COVID‐19 polymerase chain reaction (PCR) swab (COVID‐19+) to their counterparts with a negative COVID‐19 PCR swab (COVID‐19−) within related rehabilitation diagnostic groups (Stroke/Brain Injury, Spinal Cord, Orthopedic, and Medically Complex) and during the same period of time to determine whether COVID‐19+ patients benefit from inpatient rehabilitation to the same extent that COVID‐19− patients do. To do this, we prospectively followed all patients admitted to a free‐standing inpatient rehabilitation facility (IRF) from March 01, 2020 to September 30, 2020. Finally, in this context, we describe rehabilitation system changes that allowed for the delivery of inpatient post‐acute rehabilitation care during the pandemic.
METHODS
This study was reviewed and approved by the MedStar Health Institutional Review Board (Approval ID: 00003031). All study personnel are certified in, and the study protocol conformed to, the ethical guidelines of the 1975 Declaration of Helsinki. The authors followed the strengthening the reporting of observational studies in epidemiology (STROBE) checklist for cohort, case‐control, and cross‐sectional studies in the preparation of this article. 16 This study had no study sponsors. All authors had full access to all the data in the study and accept responsibility for validity of the data presented.
Design
This study is a retrospective observational cohort study of all inpatients admitted to a free‐standing, 128‐bed rehabilitation hospital located in Washington, DC. Early in the pandemic, an entire floor of our rehabilitation hospital (which included a pediatric unit and locked brain injury/neuro unit) was reconfigured such that all patients were relocated (pediatric to our partner Children's Hospital and brain injury patients to another floor of the hospital) and the locked brain injury/neuro unit was converted to an isolated COVID‐19 rehabilitation unit. Admission procedures and criteria changed during the period of study as needed due to the pandemic. Initially, all patients considered for inpatient rehabilitation and not known to have COVID‐19 within the prior 3 months were required to have a negative confirmatory nasopharyngeal screen 72 hours before admission. During the initial COVID‐19 peak, any potential patients who had tested positive for COVID‐19 during their acute admission (and only within‐system COVID‐19+ patients) were considered for admission to our COVID‐19 rehabilitation unit. Later in the pandemic as bed capacity increased, outside system COVID‐19+ patients were considered for admission. Once admitted, COVID‐19+ patients were assigned rooms by sub‐cohorts based on time since diagnosis. Those who were actively recovering from COVID‐19 remained on isolation precautions for 20 days since the first positive PCR swab. All admitted patients were still required to meet the regular qualifications for acute rehabilitation including confirmable etiologic diagnosis requiring rehabilitation management, medical stability, ability to withstand 3 hours of therapy a day, and potential to progress toward achievable goals.
Patients
Patients included in this study were admitted and discharged between March 1, 2020 and September 30, 2020. Inclusion criteria are: 18 years of age or older and admitted and discharged during the study time frame. The initial search (by data) yielded 920 patients, of which 896 met the inclusion criteria.
Data collection
Data were derived from the eRehabData database, which is an online system used by inpatient rehabilitation facilities (IRF) to document patient assessments required by the Centers for Medicare & Medicaid Services (CMS) under the IRF PPS (prospective payment system). 17 Data collected include: demographics, height (self‐report), weight (measured), body mass index (BMI, calculated), comorbidities, length of stay in acute rehabilitation (LOS), pre/post hospital living setting, and functional ability measures in self‐care (FA‐SC) and mobility (FA‐Mob). Patients who were missing FA data at either admission or discharge were not included in the FA analyses (Figure 1).
FIGURE 1.
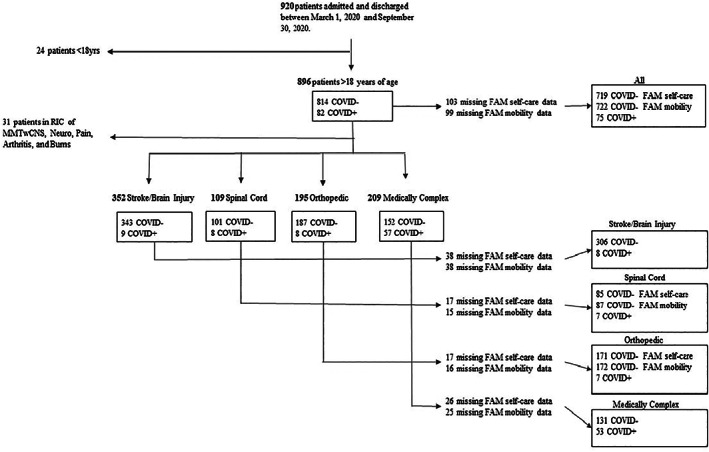
Overview of patients screened, excluded, and included in the study. CNS, central nervous system; FAM, Functional Assessment Measure; MMT, multiple major trauma; RIC, rehabilitation impairment category
Patients were initially stratified by rehabilitation impairment category (RIC), according to primary etiologic diagnosis for admission to the IRF. Due to relatively small numbers in selected RICs, the RICs were combined into the following etiologic‐related groups to facilitate analyses: (1) Stroke and Brain Injury, including individuals with stroke, traumatic brain injury, and non‐traumatic brain injury; (2) Spinal Cord, including traumatic and nontraumatic spinal cord injury and disease, and Guillain‐Barre syndrome; (3) Orthopedic, including fractures, joint replacements, amputation, orthopedics, and multiple major trauma; and (4) Medically Complex, including cardiac, pulmonary, and medically complex patients (inclusive of a primary diagnosis of COVID‐19 determined by ICD‐10 code U0.71). The RICs of major multiple trauma with central nervous system (CNS) involvement, neurologic, pain, arthritis, and burns were not included in the analysis due to either having no patients meeting the inclusion criteria and/or no patients in those RICs with a co‐existing COVID‐19+ diagnosis (Figure 1).
Patients were further stratified by COVID‐19 status and were considered to be COVID‐19+ if they were diagnosed with COVID‐19 within the 3 months prior to admission to inpatient rehabilitation. Furthermore, to meet the criteria for inpatient rehabilitation admission, all patients (regardless of COVID‐19 status) must have: (1) required ≤ 2 L O2; (2) be afebrile for 24 hours without use of antipyretics; and (3) demonstrated clinical improvement in respiratory symptoms.
Outcomes
Descriptive statistics were generated for the following variables: (1) length of stay (LOS); (2) discharge location; (3) functional ability measure for self‐care (FA‐SC) admission and discharge scores; (4) functional ability measure for mobility (FA‐Mob) admission and discharge scores; and (5) FA‐SC and FA‐Mob efficiencies. Self‐care and mobility FA items are scored from 1 to 6, where 1 signifies dependence with the activity (maximum burden of care) and 6 signifies independence with the activity (no assistance from another person or assistive device needed). A score of zero was given if the task was refused, not applicable, or not attempted due to medical condition or safety concerns. Total FA‐SC score range is 0 to 42, inclusive of eating, oral hygiene, toileting hygiene, showering/bathing, upper body dressing, lower body dressing, and donning/doffing footwear. Total FA‐Mob range is 0 to 60, inclusive of rolling left and right, sit to lying, lying to sitting on side of bed, sit to stand, chair/bed to chair transfer, toilet transfer, car transfer, walking 10 ft, ascending/descending 1 step (curb), and picking up objects. Change in FA was calculated by subtracting the total FA score at admission from that at discharge. The FA efficiency was calculated by dividing the change in FA by LOS. The following FA‐Mob items were excluded from the analysis due to missing data (% missing): walking 50 ft with 2 turns (38.9%), walking 150 ft (38.9%), walking 10 ft on uneven terrain (38.9%), ascending/descending 4 steps (70%), and ascending/descending 12 steps (74.5%).
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics 27. 18 We used qualitative (plots) and quantitative (one‐sample independent t‐tests against the test value 0.50) approaches to assess the difference in age, BMI, LOS, FA‐SC, FA‐Mob, and FA efficiency between COVID‐19+ and COVID‐19− patients. For all t‐tests, plots and the Levine's test of equality were used to determine the presence of unequal variances between groups (significant if <.05). Descriptive statistics were used to describe age, BMI, gender, LOS, and discharge location among COVID‐19+ and COVID‐19− patients. Furthermore, descriptive statistics were used to describe age, BMI, gender, LOS, FA‐SC, and FA‐Mob for each RIC group stratified by COVID‐19 status.
RESULTS
Of 920 patients who underwent inpatient rehabilitation in our IRF during this time, 896 patients met the inclusion criteria of which 82 were COVID‐19+ (9%). Demographics and descriptive statistics for the patient population by rehabilitation impairment group and COVID‐19 status are presented in Table 1. For the population as a whole, COVID‐19+ patients were younger (mean age 59.4 years vs. 62.9 years; t[894] = −2.05, p = .04) and had a higher mean BMI (32 vs 28; t[894] = 3.51, p < .01). These trends persisted for all rehabilitation impairment subgroups but were statistically significant for the Medically Complex subgroup only (t[207] = −2.12, p = .035).
TABLE 1.
Demographic information for all patients (n = 896)
| COVID‐19 status (+) or (−) | Age (y) mean ± SD (range) | BMI (kg/m2) mean ± SD (range) | Gender (percent female) | |
|---|---|---|---|---|
| All | COVID‐19+ n = 82 | 59.40 ± 15.70 a (21‐97) | 31.66 ± 8.31 c (16.3‐60) | 38 (46.3%) |
| COVID‐19− n = 814 | 62.95 ± 14.87 a (19‐104) | 28.45 ± 7.84 c (12.6‐73.9) | 370 (45.5%) | |
| Stroke/Brain Injury | COVID‐19+ n = 9 | 57.67 ± 14.04 (33‐74) | 28.76 ± 6.33 (16.3‐58.6) | 5 (55.6%) |
| COVID‐19− n = 343 | 63.87 ± 14.62 (19‐94) | 27.15 ± 6.76 (13.8‐54.8) | 150 (43.7%) | |
| Spinal Cord | COVID‐19+ n = 8 | 56.00 ± 14.88 (29‐74) | 37.23 ± 8.69 (17.8‐39.7) | 3 (37.5%) |
| COVID‐19− n = 101 | 59.21 ± 16.20 (20‐87) | 27.78 ± 6.33 (13.2‐46.8) | 37 (36.6%) | |
| Orthopedic | COVID‐19+ n = 8 | 59.63 ± 19.43 (21‐87) | 32.29 ± 12.13 (22.8‐49.6) | 3 (37.5%) |
| COVID‐19−n = 187 | 62.81 ± 14.17 (23‐104) | 29.74 ± 8.97 (15.5‐61.6) | 100 (53.5%) | |
| Medically Complex | COVID‐19+ n = 57 | 60.12 ± 15.82 b (24‐97) | 31.95 ± 8.04 d (20.7‐60) | 27 (47·4%) |
| COVID‐19− n = 152 | 64.96 ± 14.26 b (20‐95) | 29.27 ± 8.87 d (12.6‐73.9) | 65 (42.8%) |
t(894) = −2.05, p = .041.
t(207) = −2.12, p = .035.
t(894) = 3.51, p < .001.
t(207) = 1.99, p = .047.
BMI, body mass index.
Rehabilitation outcomes
Figure 2 shows the improvement from admission to discharge in self‐care and mobility functional abilities by impairment group and COVID‐19 status (no significant differences between any of the groups). Table 2 shows LOS and FA efficiencies by impairment group and COVID‐19 status. Overall, LOS and FA efficiencies were similar regardless of COVID‐19 status. In the Stroke/Brain Injury group, FA efficiencies were significantly higher for COVID‐19+ patients. In the medically complex group, only FA‐SC efficiency was significantly different despite a longer LOS (see Table 2).
FIGURE 2.
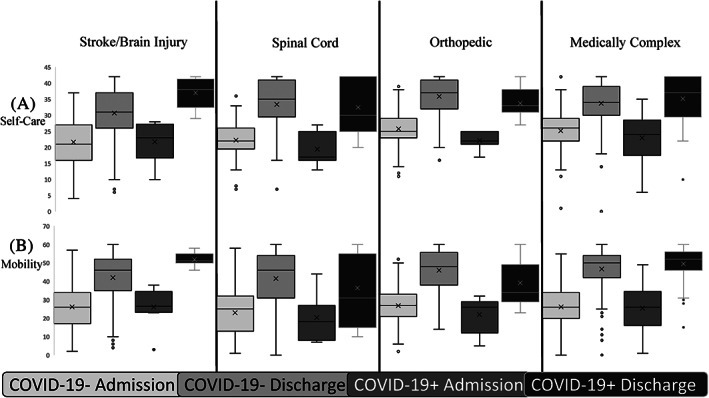
Functional Assessment Measure admission for Self‐Care (A) and Mobility (B) stratified by diagnostic group and coronavirus disease 2019 (COVID‐19) status
TABLE 2.
Length of stay (LOS) and Functional Assessment Measure (FAM) efficiency for each diagnosis group
| COVID‐19 status (+) or (−) | FA‐SC Efficiency mean ± SD (range) | FA‐Mob Efficiency mean ± SD (range) | LOS (days) mean ± SD (range) | |
|---|---|---|---|---|
| All | COVID‐19+ |
0.9 ± 0.62 (−0.04‐3.85) n = 75 |
1.6 ± 0.87 (0.13‐4.25) n = 75 |
16.4 ± 8.69 (2‐47) n = 82 |
| COVID‐19− |
0.8 ± 0.69 (−0.72‐5.5) n = 719 |
1.4 ± 2.12 (−48‐7.67) n = 722 |
16.7 ± 13.73 (1‐167) n = 814 |
|
| Stroke/Brain Injury | COVID‐19+ |
1.4 ± 1.09 a (−0.04‐2.38) n = 8 |
2.2 ± 0.96 b (0.17‐4.25) n = 8 |
15.2 ± 8.64 (22‐41) n = 9 |
| COVID‐19− |
0.8 ± 0.81 a (−0.36‐5.5) n = 306 |
1.2 ± 1.00 b (−0.71‐5.14) n = 306 |
17.8 ± 14.76 (1‐156) n = 343 |
|
| Spinal Cord | COVID‐19+ |
0.6 ± 0.31 (0.33‐3.86 ) n = 7 |
0.7 ± 0.48 (0.89‐4.14) n = 7 |
21.5 ± 4.34 (7‐30) n = 8 |
| COVID‐19− |
0.7 ± 0.54 (−0.09‐2.33) n = 85 |
1.2 ± 0.96 (−2.36‐3.57) n = 87 |
21.1 ± 20.05 (1‐167) n = 101 |
|
| Orthopedic | COVID‐19+ |
0.8 ± 0.52 (0.27‐1.17) n = 7 |
1.2 ± 0.97 (0.13‐1.48) n = 7 |
15.1 ± 4.09 (10‐23) n = 8 |
| COVID‐19− |
0.9 ± 0.63 (−0.07‐3.33) n = 171 |
1.7 ± 1.17 (0‐7.67) n = 172 |
14.3 ± 9.71 (2‐96) n = 187 |
|
| Medically Complex | COVID‐19+ |
0.9 ± 0.55 c (0.3‐1.6) n = 53 |
1.7 ± 0.80 (0.13‐3.09) n = 53 |
16.1 ± 9.48 (15‐20) n = 57 |
| COVID‐19− |
0.7 ± 0.53 c (−0.72‐2.33) n = 131 |
1.3 ± 4.45 (−.48‐4.8 ) n = 131 |
14.2 ± 8.86 (1‐65) n = 152 |
t(312) = 2.17, p = .031.
t(312) = 2.72, p = .007.
t(182) = 2.10, p = .037.
FA‐SC, functional ability measure for self‐care; FA‐Mob, functional ability measure for mobility; LOS, length of stay.
Discharge to the community is inclusive of home discharge and discharge with home health services. Overall, COVID‐19+ patients had higher rates of home discharges (84% vs. 75%) and lower rates of discharge to subacute nursing facilities (SNF; 9% vs. 13%). Among patients with Stroke/Brain Injury and Medically Complex, a greater proportion of COVID‐19+ patients were discharged to the community (89% vs. 73% and 89% vs. 76%) and fewer were discharged to skilled nursing facilities (0% vs. 16% and 5% vs. 9%) compared with their COVID‐19− counterparts. In contrast, among Spinal Cord and Orthopedic COVID‐19+ patients, the proportion of discharge to community was lower (50% vs. 69% and 75% vs. 81%) and discharge to SNF was higher (38% vs. 14% and 13% vs. 10%) (Figure 3).
FIGURE 3.
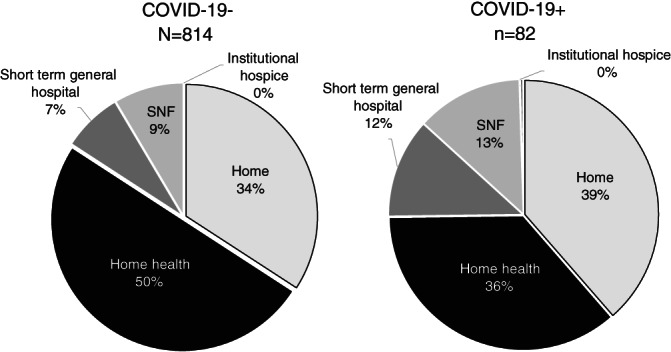
Discharge location for overall coronavirus disease 2019 (COVID‐19)± patients
DISCUSSION
In this retrospective observational cohort study, we demonstrated that patients with COVID‐19 who met the medical criteria to participate in rehabilitation in an IRF had outcomes and gains in functional abilities similar to their counterparts undergoing rehabilitation who were not affected by COVID‐19. Furthermore, our population of COVID‐19+ rehabilitation patients tended to be younger and have higher BMI than the general COVID‐19− rehabilitation population.
It is important to note that our designation of COVID‐19+ status included patients whose COVID‐19 was an incidental finding on screening and those with active COVID‐19. For example, among the Stroke/Brain Injury group, three had COVID‐19 symptoms prior to their admission to acute care and only one had further complications due to COVID‐19. The remainder (5) were incidental findings and asymptomatic. Of the Spinal Cord COVID‐19+ patients, five were incidental findings, three were asymptomatic, and only one had minimal symptoms secondary to COVID‐19. Four Orthopedic COVID‐19+ patients were incidental findings, and four were asymptomatic or with mild symptoms (mild cough, minimal O2 requirements). Among the Medically Complex patients, 50 had a primary diagnosis of COVID‐19 and 7 were listed as having COVID‐19 as a comorbidity. Of those seven, one was an incidental finding/asymptomatic, four required rehabilitation for COVID‐19 related debility, and two had mild symptoms (fever, cough, minimal O2 requirements).
When we examined specific impairment groups, several themes emerged. Our Medically Complex subgroup represents patients without traditional rehabilitation diagnoses (orthopedic, neurologic), but who have cardiac, pulmonary, or other medical conditions often resulting in “debility.” Not surprisingly, this was our largest group of COVID‐19+ patients (N = 57) and also represented most of the COVID‐19+ patients who had a primary diagnosis of COVID‐19, and thus likely were more severely affected (not incidentally identified on screening) but still met the criteria for inpatient rehabilitation admission. In this subgroup comparison, the COVID‐19+ patients were younger and had a higher BMI than their COVID‐19− counterparts but made similar (mobility) or greater (self‐care) improvements in functional abilities, over a similar period of rehabilitation.
Surprisingly, there is very little evidence available on rehabilitation outcomes among COVID‐19 patients with stroke, brain injury, and orthopedic diagnoses, despite these diagnoses being much more prevalent in rehabilitation. Among our Stroke/Brain Injury and Orthopedic groups, rehabilitation outcomes were comparable (Orthopedic) or even slightly improved (Stroke/Brain Injury) among patients with co‐existing COVID‐19. Our COVID‐19+ patients with Stroke or Brain Injury were younger than their COVID‐19− counterparts and were admitted to rehabilitation at a higher level functionally (for both self‐care and mobility). These baseline differences, although not significant, could have contributed to their ability to participate in rehabilitation and shorter LOS (non‐significant) and significantly greater gains in both self‐care and mobility functional gains.
Our Spinal Cord Injury/Disease (SCI/D) patients (n = 8) with COVID‐19 were either incidentally identified or had minimal or no symptoms during their time in acute rehabilitation. This is consistent with the few cases in the literature (most from Italy). 19 , 20 , 21 In fact, the North American Spinal Cord Injury Consortium (NASCIC) recently released (December 2020) a white paper summarizing the available evidence in which the authors conclude that “people with spinal cord injury are not at higher risk of getting infected with the COVID‐19‐19 virus” and that “the severity of symptoms and disease course of COVID‐19 in people with SCI, so far, is not as bad as initially expected.” 22 Our subpopulation with SCI/D and the NASCIC conclusions contrast with those from the one retrospective medical chart review of 17,452 Veterans with SCI/D in which 140 Veterans tested positive for COVID‐19 and 19% of these died. 23 However, this Veteran population was older (mean age 67 years) than ours and others, likely represented people with long‐standing SCI, likely had more health conditions putting them at risk for COVID‐19, and they did not identify COVID‐19+ individuals who were not experiencing symptoms (thereby potentially increasing their reported rate of infection and death). 23 Because our Spinal Cord/COVID‐19+ subpopulation was actively in inpatient rehabilitation, they were all newly injured, younger, and therefore not directly comparable.
In our study population, similar proportions of patients, regardless of COVID‐19 status, were discharged to the community (inclusive of home and home health care). These results may have been biased, although, by sub‐acute nursing facilities limiting acceptance of COVID‐19+ patients (~22% of rehabilitation patients are discharged to a SNF, depending on their rehabilitation diagnosis). Furthermore, it would be expected that the COVID‐19+ patients accepted for inpatient rehabilitation admission may have been more likely to have support for home discharge (due to their younger age and other factors), thereby increasing their likelihood for discharge to community.
It is important to interpret these results within the context of the range of post‐acute care options, including intensive inpatient, subacute, outpatient, and home health rehabilitation. This study only reports on patients with COVID‐19 admitted for inpatient rehabilitation care, and as such, does not represent the entire spectrum of rehabilitation patients. Furthermore, patients must meet certain criteria for inpatient rehabilitation admission, and this selectivity of patients impacts the results of this study. Effectively, patients must be medically stable for IRF level care and have sufficient functional impairments. Therefore, the results of this study are not necessarily representative of the entirety of the COVID‐19+ population; however, the subgroup analysis by rehabilitation diagnostic group is informative as to the effect of COVID‐19 on rehabilitation outcomes.
Although the advantages of this study include the large sample size (second only to the VA study mentioned above), analysis of comparator groups by rehabilitation diagnosis used, and comparison to other patients during the same period of care, there are several limitations. First, because this was a retrospective cohort study with data derived from a large database, certain variables of interest were not able to be collected (such as laboratory values, clinical symptoms, etc.). Missing data were handled by eliminating those patients from select analyses, and analyses of several functional mobility tasks were not possible due to missing data. As a single center study, the diversity of patients in each grouping may have been limited. Furthermore, the low numbers in subgroups (eg, COVID‐19+ rehabilitation diagnostic groups), and the limited number of patients within these subgroups represent a mixture of people with incidentally found COVID‐19 and those with variable (mild‐severe) active disease, ultimately limiting conclusions that can be drawn. In addition, although not limitations per se, it should be considered that during the period of study, factors related to the pandemic may have driven some of the outcomes. For example, during the period of this study, LOS was likely impacted in part by unique, period‐dependent external factors, such as an impetus to discharge patients as quickly as safe and feasible and return them to the community and reduce chances of hospital‐acquired infection, and to also to make available beds during periods of reduced acute care capacity. We do not think that this would have differentially affected the outcomes by group, but the possibility remains that these external factors could have differentially influenced our results. Furthermore, discharge disposition may have been impacted by SNFs not accepting patients who were COVID‐19+, which would have increased the discharge rate to home for this group.
In conclusion, our results are encouraging in that patients with COVID‐19 who meet the admission criteria for inpatient rehabilitation care are able to benefit from inpatient rehabilitation similarly to their non‐COVID‐19 counterparts with similar rehabilitation‐specific diagnoses. This is tempered by an acknowledgement that many COVID‐19 patients do not improve to the level to meet inpatient rehabilitation admission criteria; therefore, these conclusions likely reflect the experience of those not as severely affected. In addition, there is preliminary evidence to suggest that people with COVID‐19 undergoing inpatient rehabilitation are younger and have higher BMIs. Despite significant (and appropriate) focus and attention being paid to the acute effects and treatments of COVID‐19, this study emphasizes the importance of rehabilitation in returning people to the community and functioning after COVID‐19. The results argue for early involvement of physiatry as a part of the COVID‐19 treatment team to ensure optimal recovery, transitions between levels of care, and long‐term oversight of care.
ICMJE statement
We acknowledge Cynthia T. Pham, Amanda K. Rounds, and Suzanne L. Groah for project design conceptualization, investigation, methodology, project administration, data verification, writing, reviewing, and editing. Cynthia T. Pham and Amanda K. Rounds made substantial contributions to the literature search, data curation, formal analysis, and creation of figures. We also acknowledge Dr. Jennifer J. Semel for involvement in data verification, manuscript revision, and project supervision. All mentioned qualify for authorship under ICMJE recommendations.
DISCLOSURE
Cynthia T. Pham has nothing to disclose. Dr. Rounds has nothing to disclose. Suzanne Groah reports grants from National Institute on Disability, Independent Living and Rehabilitation Research (NIDILRR), grants from Congressionally Directed Medical Research Programs (CDMRP), and grants from Craig H Neilsen Foundation, all outside the submitted work. Dr. Semel has nothing to disclose.
DATA SHARING STATEMENT
Original individual patient data collected for this study will not be made available to others.
Groah SL, Pham CT, Rounds AK, Semel JJ. Outcomes of patients with COVID‐19 after inpatient rehabilitation. PM&R. 2022;14(2):202–209. 10.1002/pmrj.12645
Funding information This study did not utilize any funding source
REFERENCES
- 1. Stein J, Visco CJ, Barbuto S. Rehabilitation medicine response to the COVID‐19 pandemic. Am J Phys Med Rehabil. 2020;99(7):573‐579. Available from: /pmc/articles/PMC7268871/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McNeary L, Maltser S, Verduzco‐Gutierrez M. Navigating coronavirus disease 2019 (COVID‐19) in Physiatry: a CAN report for inpatient rehabilitation facilities. PM R. 2020;12(5):512‐515. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/pmrj.12369. [DOI] [PubMed] [Google Scholar]
- 3. Boldrini P, Bernetti A, Fiore P. Impact of COVID‐19 outbreak on rehabilitation services and physical and rehabilitation medicine physicians' activities in Italy an official document of the Italian PRM society (SIMFER). Eur J Phys Rehabil Med. 2020;56:315‐318. Available from: https://pubmed.ncbi.nlm.nih.gov/32175719/. [DOI] [PubMed] [Google Scholar]
- 4. Negrini S, Donzelli S, Negrini A, Negrini A, Romano M, Zaina F. Feasibility and acceptability of telemedicine to substitute outpatient rehabilitation services in the COVID‐19 emergency in Italy: an observational everyday clinical‐life study. Arch Phys Med Rehabil. 2020;101(11):2027‐2032. Available from: https://pubmed.ncbi.nlm.nih.gov/32800748/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Choon‐Huat Koh G, Hoenig H. How should the rehabilitation community prepare for 2019‐nCoV? Arch Phys Med Rehabil. 2020;101:1068‐1071. Available from: https://pubmed.ncbi.nlm.nih.gov/32194034/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Curci C, Pisano F, Bonacci E, et al. Early rehabilitation in post‐acute COVID‐19 patients: data from an Italian COVID‐19 rehabilitation unit and proposal of a treatment protocol. Eur J Phys Rehabil Med. 2020;56(5):633‐641. Available from: https://www.minervamedica.it/en/journals/europa-medicophysica/article.php?cod=R33Y2020N05A0633. [DOI] [PubMed] [Google Scholar]
- 7. Zeng B, Chen D, Qiu Z, et al. Expert consensus on protocol of rehabilitation for COVID‐19 patients using framework and approaches of WHO international family classifications. Aging Med. 2020;3(2):82‐94. Available from: /pmc/articles/PMC7338700/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID‐19. Am J Phys Med Rehabil. 2020;99:769‐774. Available from: /pmc/articles/PMC7315835/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. PAHO‐WHO . Rehabilitation considerations during the outbreak COVID‐19. Paho‐Who. 2020;1‐22. Available from: www.paho.org/coronavirus. [Google Scholar]
- 10. Vitacca M, Migliori GB, Spanevello A, Melazzini MG, Ambrosino N. Management and outcomes of post‐acute COVID‐19 patients in northern Italy. Eur J Intern Med. 2020;78:159‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS‐CoV‐2 pneumonia in Wuhan, China: a single‐centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475‐481. Available from: /pmc/articles/PMC7102538/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sheehy LM. Considerations for postacute rehabilitation for survivors of COVID‐19. J Med Internet Res. 2020;22: Available from: /pmc/articles/PMC7212817/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID‐19. Complementary Ther Clin Pract. 2020;39:101132 Available from: /pmc/articles/PMC7102525/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID‐19: a randomized controlled study. Complement Ther Clin Pract. 2020;39:101166 Available from: /pmc/articles/PMC7118596/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lazzeri M, Lanza A, Bellini R, et al. Respiratory physiotherapy in patients with COVID‐19 infection in acute setting: a position paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis. 2020;90:163‐168. Available from: https://pubmed.ncbi.nlm.nih.gov/32236089/. [DOI] [PubMed] [Google Scholar]
- 16. Bern I‐U of . STROBE statement‐checklist of items that should be included in reports of observational studies. 2009 [cited 2020 Dec 14]. Available from: http://www.epidem.com/ [DOI] [PubMed]
- 17. Association AMRP . eRehabData [Internet]. Silver Spring, MD: Fleming Advanced Outcomes Design Officers; 2001 [cited 2020 Dec 14]. Available from: https://web2.erehabdata.com/erehabdata/index.jsp
- 18. IBM Corp . IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp; 2020. [Google Scholar]
- 19. Righi G, del Popolo G. COVID‐19 tsunami: the first case of a spinal cord injury patient in Italy. Spinal Cord Ser Cases. 2020;6(1):22 Available from: 10.1038/s41394-020-0274-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rodriguez‐Morales AJ, Cardona‐Ospina JA, Gutiérrez‐Ocampo E, et al. Clinical, laboratory and imaging features of COVID‐19: a systematic review and meta‐analysis. Travel Med Infect Dis. 2020;34:101623 Available from: /pmc/articles/PMC7102608/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Korupolu R, Stampas A, Gibbons C, Hernandez Jimenez I, Skelton F, Verduzco‐Gutierrez M. COVID‐19: screening and triage challenges in people with disability due to spinal cord injury. Spinal Cord Ser Cases. 2020;6(1):35. 10.1038/s41394-020-0284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Consortium NASCI. Evidence Related to COVID‐19 in People Living with Spinal Injury. Niagara Falls, NY; North American SCI Consortium; 2020. https://nasciconsortium.org/wp‐content/uploads/2021/03/White‐Paper‐Known‐Evidence‐Related‐to‐COVID‐FINAL‐03‐27‐21.pdf. [Google Scholar]
- 23. Burns SP, Eberhart AC, Sippel JL, Wilson GM, Evans CT. Case‐fatality with coronavirus disease 2019 (COVID‐19) in United States veterans with spinal cord injuries and disorders. Spinal Cord. 2020;58(9):1040‐1041. 10.1038/s41393-020-0529-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


