A 24‐year old woman was hospitalized on June 13 2020 for fever (38 C°), right upper abdominal pain, pruritus, and a skin rash of one week's duration. Two months earlier she had had fever (38.5 C°), malaise and cough that resolved in one week without medical attention.
Physical examination showed a diffuse macular erythematous monomorphic rash on trunk and limbs and right upper quadrant abdominal tenderness. Analysis showed lymphopenia, alterations in liver function tests and a mild increase in C‐reactive protein and IL‐6 (Table 1). Urine sediment, blood cultures and chest X‐ray were normal. Nasopharyngeal exudate was positive for SARS‐CoV‐2 PCR and antibodies were positive for IgG and negative for IgM. Abdominal ultrasound and biliary MRI showed thickening of the gallbladder wall without lithiasis or bile duct dilatation (Figure 1a).
Table 1.
Evolution of analytical parameters.
| Bilirubin (μmol/L) | AST (U/L) | ALT (U/L) | ALP (U/L) | GGT (U/L) | Platelet count (x109/L) | CRP (mg/L) | IL‐6 (pg/mL) | |
|---|---|---|---|---|---|---|---|---|
| Jun 13 | 48 | 100 | 358 | 196 | 322 | 261 | 12.5 | ‐ |
| Jun 26 | 35 | 156 | 214 | 648 | 1166 | 425 | 56.7 | 34.2 |
| Jul 6 | 35 | 152 | 242 | 1175 | 1439 | 423 | 41.4 | 22.0 |
| Jul 27 | 21 | 125 | 162 | 615 | 645 | 296 | 4.1 | ‐ |
| Oct 20 | 11 | 35 | 48 | 151 | 226 | 272 | <1 | ‐ |
AST: aspartate aminotransferase; ALT: alanine aminotransferase; ALP: alkaline phosphatase; GGT: gamma‐glutamyl transferase, CRP: C‐reactive protein.
Figure 1.
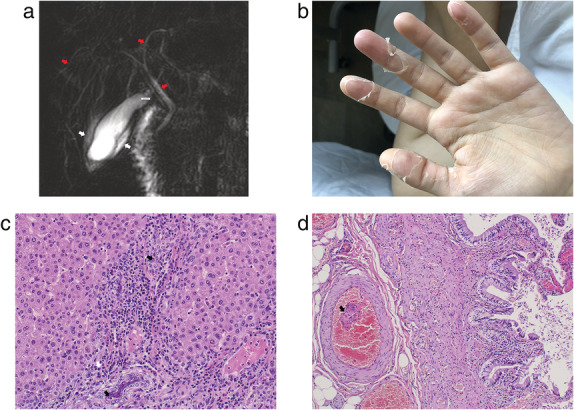
a) MRI showing normal biliary tree (red arrows) and wall edema of the gallbladder (white arrows); b) desquamation of palms and finger peeling; c) liver biopsy revealed cholangitis of the small bile ducts consisting of a mixed inflammatory infiltrate with lymphocytes, plasma cells and neutrophils (black arrows) accompanied by eosinophils (white arrow) localized around and within the bile ducts; d) cholecystectomy specimen showed subacute and chronic acalculous cholecystitis with eosinophils, vascular ectasia, and formation of occasional endoluminal thrombus (black arrow).
Intravenous antibiotic treatment with ceftriaxone and metronidazole was started but fever, abdominal pain and rash persisted. Cracked lips, desquamation of palms and soles and finger peeling appeared (Figure 1b). On June 23 a laparoscopic cholecystectomy and liver biopsy were performed. The pathology is shown in Figure 1c and Figure 1d.
After surgery, fever (<38C°), anorexia, abdominal pain and finger peeling persisted. Liver function tests were higher than before surgery and platelet count had increased (Table 1). Further analysis ruled out viral, parasitic, metabolic, and autoimmune etiology, including IgG4 levels. On this point, cholangitis in the context of a multi‐system inflammatory syndrome mimicking an incomplete adult Kawasaki disease was suspected and treatment with ursodeoxycholic acid and aspirin was initiated. A cardiac CT scan ruled out coronary aneurisms. Immunoglobulin treatment was not initiated due to the lack of a marked inflammatory state at diagnosis and the already increased thrombotic risk due to coronavirus disease‐19 (COVID‐19). Her subsequent evolution was satisfactory with progressive resolution of symptoms and improvement of liver function tests.
Alterations in liver tests in patients with COVID‐19 are usually mild and transient. They predominantly show an increase in transaminases, and are more often seen in patients with a severe clinical course. Such alterations are considered secondary to a direct viral effect, to the proinflammatory state, or to drugs used for treatment. However, severe intrahepatic cholangitis and cholecystitis has not been previously reported. The angiotensin‐converting enzyme 2 receptor and the transmembrane protease serine subtype 2 are responsible for SARS‐CoV‐2 cell tropism and are expressed in the liver, mainly in cholangiocytes. In the present case, a direct effect of the virus on cholangiocytes is unlikely considering the serological profile and the time lapse between possible SARS‐CoV‐2 infection and the clinical picture. In view of the patient's age, the concomitant presence of skin rash, cracked lips, finger peeling, thrombocytosis and the proinflammatory state we considered the patient could have had a multi‐system inflammatory syndrome mimicking an incomplete Kawasaki disease induced by SARS‐CoV‐2, a phenomenon mainly reported in children. In effect, intrahepatic cholangitis and hydrops of the gallbladder have been described in association with Kawasaki disease not related to SARS‐CoV‐2.
Fajardo, J. , Núñez, E. , Szafranska, J. , Poca, M. , Lobo, D. , Martín, B. , Hernández, D. , Roig, C. , Huerta, A. , Corominas, H. , Sánchez‐Cabús, S. , and Soriano, G. (2021) We report a patient who presented intrahepatic cholangitis and cholecystitis after SARS‐CoV‐2 infection. Journal of Gastroenterology and Hepatology, 36: 2037. 10.1111/jgh.15537.


