Abstract
The coronavirus pandemic has exposed healthcare professionals to suffering and stressful working conditions. The aim of this study was to analyze professional quality of life among healthcare professionals and its relationship with empathy, resilience, and self‐compassion during the COVID‐19 crisis in Spain. A cross‐sectional study was conducted with 506 healthcare professionals, who participated by completing an online questionnaire. A descriptive correlational analysis was performed. A multivariate regression analysis and a decision tree were used to identify the variables associated with professional quality of life. Empathy, resilience, and mindfulness were the main predictors of compassion fatigue, compassion satisfaction, and burnout, respectively.
Keywords: empathy, hospital/institutional environment, job related stress, nursing care/interventions, systems research/patterns of care, work/job satisfaction
1. INTRODUCTION
Spain has been one of the countries most affected by the coronavirus in the world, with very high daily mortality and infection rates (Ceylan, 2020). Healthcare professionals have faced a wide range of specific challenges arising from the pandemic (Shanafelt et al., 2020), including working without sufficient personal protective equipment, fear of contagion, acting as intermediaries between isolated patients and family members, witnessing a large number of deaths, assisting dying patients, facing rationing decisions, poor work environments with insufficient staff, hostile working relationships, and ineffective leadership (Halcomb et al., 2020; Shanafelt et al., 2020).
Compassion and self‐compassion are potential protective factors against the psychological consequences of these situations for healthcare professionals (Duarte et al., 2016). Compassion may be defined as sensitivity to others' suffering coupled with the motivation to alleviate and prevent this suffering (Sinclair et al., 2017). Compassion involves sensitivity, recognition, understanding, emotional resonance, empathic concern, and tolerance for the distress generated by the suffering of others, coupled with the relational actions to alleviate and prevent it (Faqihi et al., 2017; Lown et al., 2015; Mills et al., 2017; Sinclair et al., 2017). Self‐compassion, on the other hand, is understood as providing ourselves with the care, comfort, and reassurance that we provide to those we care for when they are suffering (Stuntzner, 2015). To be self‐compassionate, one must be kind to oneself rather than judging or criticizing oneself (self‐kindness), recognize that suffering is part of human nature (common humanity), and experience the present without over‐identifying oneself with one's emotions (over‐identification; Neff, 2003).
The continuous contact with patients' suffering to which healthcare professionals are exposed can have negative consequences for them, although there may be some positive consequences as well. Professional quality of life is a three‐dimensional concept that is understood as the degree to which the members of a group are able to fulfill their personal needs through their experiences in the organizational context in which they work (Roney & Acri, 2018; Stamm, 2005). The three dimensions of professional quality of life are compassion fatigue (CF), burnout (BO; negative consequences), and compassion satisfaction (CS; positive consequence of professional caregiving). Compassion fatigue is defined as the cost of caring for others or caring about their emotional pain (Figley, 2004). Compassion fatigue may cause a communication deficit with patients, family members, and other colleagues (Nolte et al., 2017), and is considered to be an avoidance mechanism adopted in response to the suffering of patients and their families (Babineau et al., 2019). In turn, BO is a syndrome characterized by emotional exhaustion, depersonalization (Lahana et al., 2017), and lack of personal fulfillment at work appearing as a consequence of continuous exposure to occupational stress (Cañadas‐De la Fuente et al., 2018; Maslach & Jackson, 1981). Among the risk factors for BO, factors related to the environment and working conditions have been described, such as work overload, multiple employment, or working shifts, especially at night (Molina‐Praena et al., 2018). In addition, some studies indicate that among the stressors that can influence the occurrence of BO in health professionals is the continuous contact with the suffering of the people they care for (Duarte & Pinto‐Gouveia, 2017). In contrast, CS, that is, the feeling of accomplishment derived from efforts made to help someone else (Mooney et al., 2017; Roney & Acri, 2018), is a positive aspect of a healthcare professional's work (Craigie et al., 2016).
There is evidence to suggest that internal resources such as empathy, self‐compassion, or resilience can help prevent CF or BO in healthcare professionals (Delgado et al., 2017; Duarte et al., 2016). Empathy may be defined as the affective and cognitive attunement that facilitates the understanding of the inner world of others (Hunt et al., 2019). Empathy has been described in terms of two dimensions: cognitive empathy, which refers to the ability to understand others, and affective empathy, which refers to the ability to share feelings in consonance with others' emotional states (Ge et al., 2016). In turn, resilience involves enduring stress, tolerating pressure in adverse situations, and reacting by deploying strategies to overcome negative or traumatic experiences (Cooper et al., 2020; Henshall et al., 2020; Terry et al., 2019). Self‐compassion training, meanwhile, has been shown to increase resilience and decrease CF and BO among healthcare professionals (Conversano et al., 2020; Delaney, 2018). However, studies exploring the relationship of these emotional variables with professional quality of life in health crisis situations are scarce. Therefore, the aim of this study was to analyze professional quality of life and its relationship with empathy, resilience, and self‐compassion in healthcare professionals in response to the COVID‐19 healthcare crisis in Spain.
2. METHODS
2.1. Study design and participants
A descriptive cross‐sectional study was conducted with a sample of 108 physicians and 398 nurses (n = 506) working in primary care, inpatient care, nursing homes, and specific COVID‐19 units in 16 regions of Spain. The inclusion criterion was to currently be working as a professional in care services involving direct contact with patients. Professionals working in management or in positions in which they did not have direct contact with patients were excluded.
2.2. Variables
Professional quality of life was assessed using the Spanish version of the Professional Quality of Life Scale (ProQoL; Morante‐Benadero et al., 2006; Stamm, 2005). It is a self‐report questionnaire consisting of 30 items rated on a 6‐point Likert scale, divided into three subscales: CF (10 items), CS (10 items), and BO (10 items). On all subscales, higher scores indicate higher levels of CF, CS, or BO respectively. In each case, scores can be categorized as low, moderate, or high: CF (<8 = low; 9–17 = moderate; >17 = high); CS (<33 = low; 34–41 = moderate; >42 = high), and BO (<18 = low; 19–26 = moderate; >27 = high). The Spanish version of ProQoL has a Cronbach's α of 0.782 for CF, 0.774 for CS, and 0.537 for BO, respectively (Galiana et al., 2017).
The Spanish version of the Basic Empathy Scale (BES; Jolliffe & Farrington, 2006; Oliva Delgado et al., 2011) was used to assess empathy. The scale consists of 9 items rated from 1 (strongly disagree) to 5 (strongly agree), and is divided into two dimensions: affective empathy (4 items), with scores ranging from 4 to 20 points, and cognitive empathy (5 items), with scores ranging from 5 to 25 points. Higher scores indicate higher levels of empathy. Τhe internal consistency of the total scale was 0.84, with 0.85 for the cognitive empathy subscale and 0.84 for the affective empathy subscale (Oliva Delgado et al., 2011).
Resilience, which is considered to be a positive personal characteristic allowing the individual to adapt to adverse situations, was measured using the Spanish version of the 14‐item Resilience Scale (RS‐14; Sánchez‐Teruel & Robles‐Bello, 2015; Wagnild, 2009). The scale consists of 14 items rated on a Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). The final score is between 14 and 98 points, and higher scores indicate higher levels of resilience. The scale has an adequate level of internal consistency in Spanish population (α = .79) (Sánchez‐Teruel & Robles‐Bello, 2015).
Self‐compassion, defined as how individuals behave toward themselves at the most difficult times, was measured using the Spanish version of the Self‐Compassion Scale (SCS; Garcia‐Campayo et al., 2014; Neff, 2003). This is a 12‐item questionnaire with responses rated on a 5‐point ordinal Likert scale from 1 (almost never) to 5 (almost always). The scale has six subdimensions, each containing two items: self‐kindness, common humanity, mindfulness, and their opposites: self‐judgment, isolation, and over‐identification, which are calculated by reversing the scores. To calculate the subscale scores and total values, it is first necessary to calculate the reverse scores for the items in the negative subscales (self‐judgment, isolation, and over‐identification). The psychometric properties were adequate, with a Cronbach's α of .89 for the total scale score and ranging between 0.79 and 0.91 for the six subscales (Garcia‐Campayo et al., 2014).
2.3. Data collection
An online questionnaire was designed for data collection due to the lockdown restrictions in place during the pandemic. Social media pages and the research group's website (http://cuidadoscompasion.es/) were used to distribute basic information on the study and link professionals to the questionnaire. Participation was voluntary, anonymous, and open to all professionals working in Spain who wanted to participate. Data collection took place between March 30, 2020, and April 16, 2020, a period in which the pressure and workload that healthcare professionals faced in Spain were particularly high due to the COVID‐19 pandemic.
2.4. Ethical considerations
Participation through the online questionnaire was voluntary. Before answering the questionnaire, participants had to read a pop‐up window with information on the study objectives and give their consent to participate and have their data processed. The confidentiality of the data and the anonymity of the participants were preserved at all times in compliance with Spanish regulations and the ethical principles enshrined in the Declaration of Helsinki. The study was approved by an institutional research ethics committee.
2.5. Data analysis
Means and standard deviations were calculated for quantitative variables (professional quality of life, empathy, resilience, and self‐compassion) and absolute values and percentages were calculated for qualitative variables (age, occupation, sex, marital status, work setting during the crisis, employment status, and work shift). Student's t test and ANOVA were used to determine whether there were differences in the mean scores of the ProQoL components according to sociodemographic and occupational variables. Pearson's correlation was used to analyze correlations between variables. Subsequently, a multiple linear regression analysis was performed for each of the ProQoL components (dependent variables), considering as independent variables those which were related to managing emotions (empathy, resilience, and self‐compassion). The sociodemographic and work‐related variables that were significant were also included in the model as independent variables. Finally, a classification and regression tree were made with the multiple linear regression variables using the CART model (Classification and Regression Trees), with a minimum number of cases of 100 for the parent node and 50 for the child nodes. This model allows subjects to be classified into homogeneous groups of subjects (nodes) which in turn are heterogeneous between them. It does this by using a binary division based on the dependent variable. A series of divisions takes place, producing primary and secondary nodes until a terminal node is reached. The model algorithm divides groups according to the predictor variable that it considers to be the most significant in the regression model. Therefore, this method made it possible to identify the most significant predictor variables and classify subjects in homogeneous groups based on the dependent variable of the regression model (Al Ghoson, 2010). SPSS Statistics v.25 (IBM Corp.) was used for data processing.
3. RESULTS
Table 1 shows sociodemographic and work‐related data from the sample. A total of 506 healthcare professionals participated in the study, with an average age of 46.7 (SD = 10.2), of whom the majority were nurses with a stable employment status, female, over 46 years old, and married. Mean CS scores were significantly higher in nurses than in physicians, whereas mean BO and CF scores were significantly higher in physicians than in nurses.
Table 1.
Sociodemographic and work‐related characteristics of the participants and differences in means based on the Professional Quality of Life questionnaire (n = 506)
| CS | BO | CF | ||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | n | % | M (SD) | p | M (SD) | p | M (SD) | p |
| Age (years) | ||||||||
| ≤35 | 79 | 15.6 | 40.06 (6.66) | .48a | 25.89 (5.91) | .13a | 19.84 (7.07) | .96a |
| 36–45 | 153 | 30.2 | 39.39 (5.92) | 24.75 (5.83) | 19.99 (7.97) | |||
| ≥46 | 274 | 54.2 | 39.08 (6.62) | 24.37 (5.83) | 19.79 /7.60) | |||
| Occupation | ||||||||
| Nurse | 398 | 78.7 | 39.94 (5.94) | <.001b,* | 24.32 (5.73) | .016b,* | 19.39 (7.27) | .003b,* |
| Physician | 108 | 21.3 | 37.06 (7.55) | 26.21 (6.55) | 21.58 (8.61) | |||
| Sex | ||||||||
| Female | 338 | 76.7 | 39.40 (6.23) | .13b | 24.97 (5.89) | .88b | 20.26 (7.65) | .75b |
| Male | 118 | 23.3 | 39.08 (7.01) | 23.92 (6.13) | 18.54 (7.41) | |||
| Marital status | ||||||||
| Married or in civil partnership | 374 | 73.9 | 39.39 (6.12) | .93a | 24.68 (5.78) | .46a | 20.03 (7.57) | .64a |
| Single | 79 | 15.6 | 39.13 (7.26) | 25.37 (6.52) | 19.16 (7.79) | |||
| Separated or widow/er | 53 | 10.5 | 39.19 (7.21) | 24.09 (6.31) | 19.68 (7.81) | |||
| Work setting during the crisis | ||||||||
| Primary care center | 186 | 36.8 | 38.74 (6.55) | .44a | 24.58 (6.12) | .71a | 20.01 (7.82) | .59a |
| Regular inpatient care | 140 | 27.7 | 40.42 (5.61) | 24.2 (5.69) | 19.43 (7.42) | |||
| ICU | 64 | 12.8 | 39.75 (5.66) | 25.15 (5.32) | 20.35 (7.45) | |||
| Emergency department | 76 | 15.0 | 39.94 (7.22) | 24.63 (7.22) | 18.92 (6.64) | |||
| Specific COVID‐19 unit | 30 | 5.9 | 37.7 (7.35) | 28.96 (7.32) | 24.35 (8.14) | |||
| Nursing homes | 10 | 1.8 | 41.52 (6.43) | 21.85 (5.36) | 15.32 (14.5) | |||
| Employment status | ||||||||
| Stable/permanent | 365 | 72.1 | 38.95 (6.70) | .66b | 24.24 (5.95) | .88b | 19.49 (7.59) | .85b |
| Temporary/replacement/unstable | 141 | 27.9 | 39.77 (6.05) | 25.31 (5.92) | 20.30 (7.65) | |||
| Work shift | ||||||||
| Fixed morning shift | 210 | 41.5 | 39.67 (6.50) | .71a | 24.58 (5.96) | .29a | 19.49 (7.39) | .38a |
| Rotating without night shifts (mornings/evenings) | 66 | 13.0 | 39.15 (6.42) | 24.58 (5.88) | 19.76 (7.98) | |||
| Rotating with night shifts | 224 | 44.3 | 38.17 (7.38) | 28.83 (7.19) | 21.67 (7.36) | |||
| Fixed night shift | 6 | 1.2 | 38.83 (6.12) | 25.29 (6.06) | 21.24 (7.32) | |||
Abbreviations: BO, burnout; CF, compassion fatigue; CS, compassion satisfaction; M, mean; p, level of statistical significance.
F = ANOVA.
t = Student's t test.
p < .05.
Table 2 shows the mean values for the different variables analyzed. With regard to professional quality of life, it can be observed that participants had moderate levels of CS (M = 39.33; SD = 6.42), moderate levels of BO (M = 24.72; SD = 5.95), and high levels of CF (M = 18.86; SD = 7.62). Regarding the Basic Empathy Scale (BES), the mean scores for affective empathy and cognitive empathy were high, with a higher mean score for cognitive empathy (M = 20.76; SD = 3.04) than for affective empathy (M = 14.31; SD = 3.45). The mean scores for resilience was high (M = 78.46; SD = 11.60), as per the instructions for the RS‐14 questionnaire. Finally, with respect to self‐compassion, high mean scores were observed for mindfulness (M = 3.61; SD = .83), self‐kindness (M = 3.25; SD = .88), and common humanity (M = 3.21; SD = .86) (Table 2).
Table 2.
Descriptive statistics for the total number of participants (n = 506)
| Variable | Subscales | Range | M | SD | Skewness | Kurtosis |
|---|---|---|---|---|---|---|
| Professional quality of life (ProQoL) | CS | 5–50 | 39.33 | 6.42 | −1.20 | 2.408 |
| BO | 11–42 | 24.72 | 5.95 | 0.291 | −0.304 | |
| CF | 3–46 | 19.86 | 7.62 | 0.268 | −0.273 | |
| Empathy (BES) | Affective | 4–20 | 14.31 | 3.45 | −0.491 | −0.080 |
| Cognitive | 5–25 | 20.76 | 3.04 | −0.675 | 1.037 | |
| Resilience (RS‐14) | Resilience | 35–98 | 78.46 | 11.60 | −0.796 | 0.681 |
| Self‐compassion (SCS) | Self‐kindness | 1–5 | 3.25 | 0.88 | −0.008 | −0.415 |
| Self‐judgment | 1–5 | 2.97 | 1.01 | 0.123 | −0.488 | |
| Common humanity | 1–5 | 3.21 | 0.86 | −0.137 | 0.044 | |
| Isolation | 1–5 | 3.22 | 1.05 | −0.081 | −0.766 | |
| Mindfulness | 1–5 | 3.61 | 0.83 | −0.310 | −0.041 | |
| Over‐identification | 1–5 | 2.87 | 1.02 | 0.143 | −0.655 |
Abbreviations: BO, burnout; CF, compassion fatigue; CS, compassion satisfaction; M, mean.
Table 3 shows the correlations between the different study variables. The correlations between CS and BO (r = −.57; p < .01), CS and CF (r = −.38; p < .01), and CS and affective empathy (r = −.14; p < .01) were significant and negative. In addition, CS was found to be significantly and positively correlated with cognitive empathy (r = .15; p < .01), resilience (r = .55; p < .01), and all the subdimensions of self‐compassion. Within the subdimensions of self‐compassion, significantly stronger correlations between CS and self‐kindness (r = .41; p < .01) and between CS and mindfulness (r = .38; p < .01) were observed. In turn, BO was shown to be significantly and positively correlated with CF (r = .69; p < .01) and affective empathy (r = .25; p < .01), and weakly correlated with cognitive empathy (r = .02; p < .01). Burnout was found to be significantly and negatively correlated with resilience (r = −.47; p < .01) and all subdimensions of self‐compassion, especially over‐identification (r = −.47; p < .01). Finally, CF was significantly and positively correlated with affective empathy (r = .44; p < .01), but less so with cognitive empathy (r = .18; p < .01). Compassion Fatigue was negatively correlated with resilience (r = −.40; p < .01) and all subdimensions of self‐compassion, especially over‐identification (r = −.49; p < .01) (Table 3).
Table 3.
Correlations between study variables (n = 506)
| ProQoL | BES | RS‐14 | SCS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | BO | CF | Affective | Cognitive | Resilience | Self‐kindness | Self‐judgment | Common humanity | Isolation | Mindfulness | Over‐identification | |
| Professional quality of life (ProQoL) | CS | −.57** | −.38** | −.14** | .15** | .55** | .41** | .24** | .27** | .32** | .38** | .36** |
| BO | .69** | .25** | .02** | −.45** | −.41** | −.32** | −.20** | −.44** | −.39** | −.47** | ||
| CF | .44** | .18** | −.40** | −.37** | −.35** | −.14** | −.46** | −.40** | −.49** | |||
| Empathy (BES) | Affective | .37** | −.23** | −.20** | −.24** | −.12 | −.26** | −.22** | −.34** | |||
| Cognitive | .20** | .08* | −.10* | .14** | .02 | .06 | −.07 | |||||
| Resilience (RS‐14) | Resilience | .58** | .33** | .36** | .47** | .56** | .51** | |||||
| Self‐compassion (SCS) | Self‐kindness | .39** | .39** | .53** | .62** | .52** | ||||||
| Self‐judgment | .32** | .49** | .29** | .52** | ||||||||
| Common humanity | .23** | .32** | .24** | |||||||||
| Isolation | .41** | .68** | ||||||||||
| Mindfulness | .45** | |||||||||||
Abbreviations: BO, burnout; CF, compassion fatigue; CS, compassion satisfaction.
p < .05.
p < .01.
Different multiple regression models were evaluated to determine the predictive capacity of the variables of empathy, resilience, and self‐compassion with respect to the three dimensions of professional quality of life. The results of the analyses are shown in Table 4. Resilience, self‐kindness, and occupation explained 36% of the variance of CS (F = 96.87; p < .001), with the best positive predictor being resilience. For every 1‐unit increased in resilience, CS increased 0.51 points. Resilience and the self‐compassion subdimensions of isolation, over‐identification, and mindfulness explained 29% of the variance of BO (F = 54.63; p < .001). Of all these variables, and according to the β coefficient, mindfulness was the best negative predictor. For every 1‐unit increased in mindfulness, BO decreased 0.11 points. Resilience, affective empathy, cognitive empathy, and the self‐compassion subdimensions of isolation, over‐identification, and mindfulness explained 39% of the variance of CF (F = 55.41; p < .001). Taking into account the value of β, affective empathy and cognitive empathy were the best positive predictors of CF (Table 4). For every 1‐unit increased in affective empathy and cognitive empathy, CF increased 5.96 and 3.01 points, respectively.
Table 4.
Multiple linear regression model for empathy, resilience, and self‐compassion predicting Professional Quality of Life (n = 506)
| Variables | Model | B | SE B | β | t | p | 95% CI | R 2 |
|---|---|---|---|---|---|---|---|---|
| CS | Constant | 16.36 | 1.81 | 8.84 | <.001 | 12.81, 19.92 | ||
| Resilience (RS‐14) | 0.27 | 0.024 | .50 | 11.94 | <.001 | −0.32, 0.23 | .36 | |
| Self‐kindness (SCS) | 0.44 | 0.15 | .12 | 2.81 | .005 | −0.75, 0.13 | ||
| Occupation | −1.52 | 0.56 | −.09 | −2.17 | .007 | −2.62, −0.42 | ||
| BO | Constant | 41.85 | 1.54 | 27.17 | <.001 | 38.82, 44.87 | ||
| Resilience (RS‐14) | −0.09 | 0.02 | −.19 | −3.96 | <.001 | −0.14, −0.05 | ||
| Isolation (SCS) | −0.41 | 0.14 | −.14 | −2.85 | .004 | −0.70, −0.13 | .29 | |
| Over‐identification (SCS) | −0.66 | 0.15 | −.22 | −4.22 | <.001 | −0.97, −0.35 | ||
| Mindfulness (SCS) | −0.39 | 0.16 | −.11 | −2.39 | .017 | −0.72, −0.07 | ||
| CF | Constant | 251.6 | 2.62 | 9.57 | <.001 | 20, 39.32 | ||
| Resilience (RS‐14) | −0.09 | 0.03 | −.13 | −2.91 | .004 | −0.14, −0.02 | ||
| Affective empathy (BES) | 0.51 | 0.09 | .23 | 5.69 | <.001 | 0.33, 0.69 | ||
| Cognitive empathy (BES) | 0.29 | 0.09 | .11 | 3.01 | .003 | 0.10, 0.48 | .39 | |
| Isolation (SCS) | −0.51 | 0.17 | −.14 | −2.95 | .003 | −0.85, −0.17 | ||
| Over‐identification (SCS) | −0.67 | 0.19 | −.18 | −3.54 | <.001 | −1.05, −0.30 | ||
| Mindfulness (SCS) | −0.63 | 0.19 | −.14 | −3.20 | .001 | −1.02, −0.24 |
Note: p is significant at the p < .05 level.
Abbreviations: B, unstandardized regression coefficients; BO, burnout; CF, compassion fatigue; CI, confidence interval; CS, compassion satisfaction; R 2, variance explained; SE B, standard error of B; t, Student's t; β, standardized regression coefficients.
Figure 1 shows the decision tree for the dimension of CS. Resilience was found to be the greatest predictor of CS, followed by mindfulness. Participants with higher resilience (>83.5) scores were those with higher mean scores for CS (M = 42.75). As per node 4, 37.4% (n = 189) of the participants were categorized within this node (Figure 1).
Figure 1.
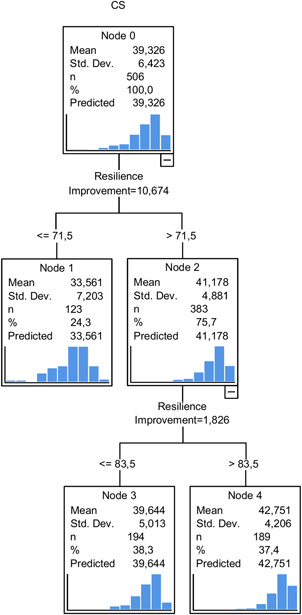
Decision tree for CS. CS, compassion satisfaction [Color figure can be viewed at wileyonlinelibrary.com]
In turn, over‐identification, resilience, isolation, and mindfulness were the main predictors of BO. The highest mean score for BO (M = 29.45) was observed in node 3, with low mean scores for over‐identification (≤6.5) and resilience (≤67.5). This node included 15.6% (n = 79) of the participants (Figure 2). Over‐identification, affective empathy, resilience, and isolation were the main predictors of CF. Node 4 shows the highest mean values for CF (M = 25.78), with 22.5% (n = 114) of healthcare professionals. Participants in this node had a lower over‐identification score (≤6.5) and a higher affective empathy score (>16.5). In addition, the mean score for CF was found to be the lowest in node 5 (M = 13.41), where over‐identification (> 6.5) and affective empathy were lower (≤13.5; Figure 3).
Figure 2.
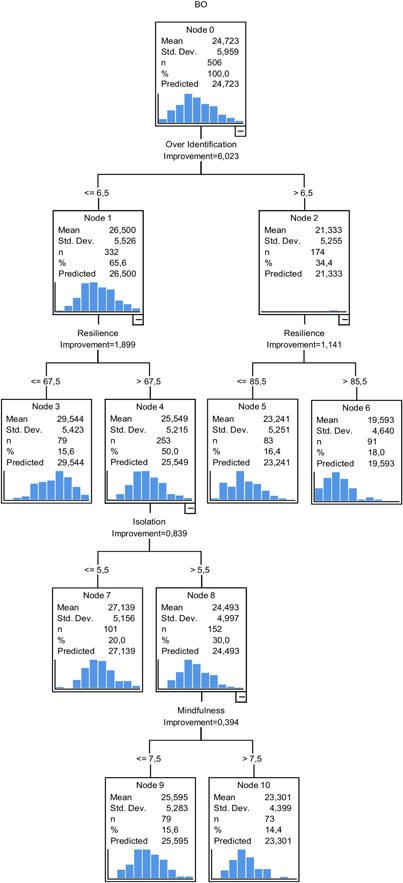
Decision tree for BO. BO, burnout [Color figure can be viewed at wileyonlinelibrary.com]
Figure 3.
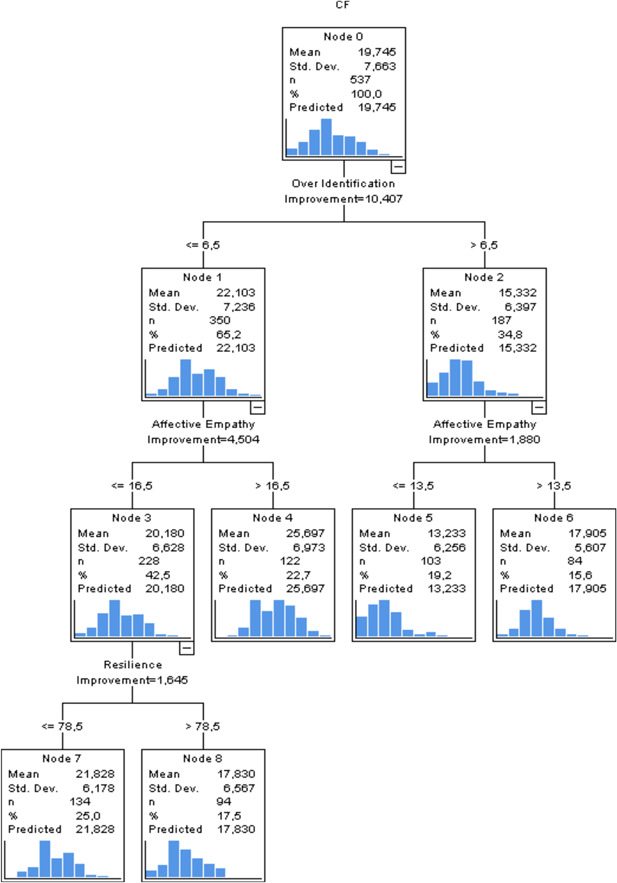
Decision tree for CF. CF, compassion fatigue [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
The aim of this study was to analyze professional quality of life among healthcare professionals and its relationship with empathy, resilience, and self‐compassion in an unusual situation for the Spanish health system that has been generated by the COVID‐19 pandemic. We found high levels of CF, BO, and CS in the midst of this health crisis. These data are consistent with those obtained in other countries with a serious COVID‐19 crisis situation, such as China (Lai et al., 2020; Li et al., 2020), and with studies conducted before the pandemic showing that continuous contact with patients' suffering can increase CF—as well as CS—among healthcare professionals (Craige et al., 2016; Ruiz‐Fernández et al., 2020). However, other authors state that, despite the emotional and psychological exhaustion experienced by professionals, the satisfaction they obtain from helping others is very pronounced and could act as a protector against CF and BO (Cummings et al., 2018).
Resilience has been shown to be the main predictor of CS in this study. The components of resilience include, on the one hand, the acceptance of impermanence and suffering, and on the other hand, equanimity and kindness toward one's own suffering (Southwick et al., 2014). Resilience appears to be related to compassion and a variety of studies suggest that having experienced adversity in the past may predispose individuals toward compassion (Lim & DeSteno, 2016), while other studies point out that cultivating acceptance of death and suffering not as a failure but as a natural part of human existence fosters personal growth (Edo‐Gual et al., 2015). Thus, if CS is understood as a sense of achievement or gratification felt by healthcare professionals as a result of their contributions to the wellbeing of patients and their families (Roney & Acri, 2018; Sacco & Copel, 2018) that is achieved through the provision of compassionate care (Coetzee & Laschinger, 2018), resilience is a personal resource necessary for achieving CS, as it enables healthcare professionals to adjust to the constantly stressful environments that care settings often are (Coetzee & Laschinger, 2018; Sacco & Copel, 2018).
Interestingly, our results show that occupation (being a nurse or a physician) appears among the variables influencing CS. Nurses have significantly higher CS scores, although they carry out their work under the same difficult conditions generated by the pandemic in terms of workload, uncertainty, and availability of resources and protective measures. Furthermore, the levels of CS obtained among the nurses in our study are also higher than those reported among Spanish nurses in recent studies conducted before the pandemic (Galiana et al., 2017; Ruiz‐Fernández et al., 2020). We believe that the special circumstances generated by the pandemic have given nurses the opportunity to rediscover their own intrinsic motivation to provide care, which had prompted them to choose the nursing profession, through their unconditional effort and commitment to alleviating the suffering of patients in a situation of extreme hardship and uncertainty. The pandemic has also increased the visibility of the work of nurses, showing society the need for highly qualified, specialized professionals, elements that have been considered necessary to improve the social image of the nursing profession (Hoeve et al., 2014). Thus, in line with Schwartz et al. (2003), nurses derive satisfaction from working hard and seeing others benefit from their own efforts. This, which could be applicable to physicians, may have been attenuated in their case for two reasons. First, the social image of physicians was already good before the pandemic, so they might have not perceived a significant change in this respect. Second, in the healthcare context in Spain, the final decision on the administration of treatment rests with physicians. During the data collection period of this study, many physicians had to treat critically ill patients with high mortality rates, had to deliver bad news to family members more frequently, or had to prioritize some cases over others due to a lack of resources such as ventilators or ICU beds. It is highly likely that physicians as a whole were not prepared for these situations, causing them to experience moral injury (Greenberg et al., 2020) and contributing to the development of CF and BO (Winner & Knight, 2019).
Regarding BO, our regression analysis shows that the mindfulness subdimension of self‐compassion is the main negative predictor of BO. Nonetheless, the decision tree shows that over‐identification also has a significant influence on BO, which is consistent with over‐identification being conceptualized as the opposite of mindfulness in the construction of the scale used to measure self‐compassion in our study (Neff, 2003). This negative relationship between mindfulness and BO is to be expected, as mindfulness is a state of balance in which individuals are aware of their thoughts and feelings without judging them and without running away from them (Neff, 2003), whereas BO is characterized by, among other things, a lack of professional fulfilment resulting in low self‐esteem and negative assessments of one's own work (Nabizadeh‐Gharghozar et al., 2020).
Empathy, especially affective empathy, is the greatest predictor of CF, as reported in other studies (Duarte et al., 2016; Hayuni et al., 2019). Compassion fatigue has been defined as a progressive, cumulative process of continuous, intense contact with patients' suffering, coupled with a use of self that leads to compassion stress (Coetzee & Klopper, 2010; Coetzee & Laschinger, 2018). However, several authors have raised questions about compassion having negative effects on compassionate individuals (Brito‐Pons & Librada‐Flores, 2018), thus challenging the idea that CF is a type of fatigue caused by an excess of compassion (Figley, 2004). Although empathy has been described as a necessary skill for the development of compassion, other skills such as friendliness, distress tolerance, sensitivity, courage, and generosity are also necessary (Gilbert, 2015). As a result, a number of authors propose that the negative consequences of exposure to the suffering of others could be termed empathic distress (Klimecki & Singer, 2012) or secondary traumatic stress (Cummings et al., 2018), instead of CF. Additionally, over‐identification, as a subdimension of self‐compassion, refers to becoming so immersed in one's own emotional reactions that it becomes difficult to connect with others. According to our results, over‐identification was associated with CF, which is consistent with the fact that a high use of self constitutes one of the main antecedents of CF (Coetzee & Klopper, 2010; Jenkins & Warren, 2012).
5. LIMITATIONS
First, this was a cross‐sectional descriptive study. As such, it did not determine the causality of the variables analyzed, which would require a longitudinal study with further active observation over time. Second, this study used an online questionnaire, which may have introduced some reporting bias. However, this method allowed us to reach different autonomous communities in Spain. Third, the BO subscale of the Spanish version of the ProQoL has shown a moderate Cronbach ɑ coefficient (0.537), so the results on this dimension should be interpreted with caution. Finally, the professionals who participated in the study worked in different health and social care settings. This factor may have influenced the participants' responses, since the care provided during the COVID‐19 health crisis differed according to the setting. The authors did not set out to analyze this factor and the wide range of settings has made it possible to gain a general overview of the emotional situation of healthcare professionals. Further research is needed to delve deeper into professional quality of life and emotion management across different health and social care settings.
6. CONCLUSION
The results of this study show that levels of CF, BO, and CS in health crisis situations caused by COVID‐19 are high. Individual factors such as resilience, empathy, or self‐compassion influence whether the care work will be positive (CS) or negative (CF and BO) for healthcare professionals. However, situational or environmental factors such as the workload, work organization, or social environment (the recognition of their professional work) may also be influential, although these variables have not been taken into account in this study.
In response to this situation, a series of intervention programs are needed to enhance certain emotion management resources and help prevent the onset of these syndromes. Resilience and the cultivation of compassion must be encouraged among healthcare professionals to prevent CF and BO and increase CS. Being equable and accepting of suffering will enable professionals to make sense of the experiences they face on a daily basis. In addition, cultivating compassion will foster resilience and self‐compassion, and ultimately enable professionals to cope with suffering and death without CF and with CS (Duarte et al., 2016). The presence of compassion will permit professionals to remain present in the face of suffering. For this reason, mindfulness should be included in intervention programs for cultivating compassion. Health institutions must take responsibility for the care that their healthcare workers require. The implementation of evidence‐based programs that foster compassion will have an impact on the wellbeing of professionals and on the quality of care received by patients. In addition to individual interventions, interventions are needed that involve healthcare institutions and organizations (Crawford et al., 2014) such as offering support services to their own healthcare workers, ethical counseling or psychological support, providing sufficient material and human resources for adequate patient care, and promoting a healthcare system that is safe for both patients and professionals, even in exceptional circumstances such as those generated by the COVID‐19 pandemic.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENTS
The authors would like to thank all of the nursing professionals who collaborated in this study, as well as the PiCuida (Plan Integral de Cuidados de Andalucía, Spanish for Comprehensive Care Plan of Andalusia) for making this study possible. This study has been funded by a grant from the Ministry of Health of the Regional Government of Andalusia, Spain (AP‐0100‐2016) and the Andalusian Association of Community Nurses (ASANEC), Spain. Funding for open access charge has been received by University of Huelva/CBUA.
Ruiz‐Fernández, M. D. , Ramos‐Pichardo, J. D. , Ibáñez‐Masero, O. , Carmona‐Rega, M. I. , Sánchez‐Ruiz, M. J. , & Ortega‐Galán, Á. M. (2021). Professional quality of life, self‐compassion, resilience, and empathy in healthcare professionals during COVID‐19 crisis in Spain. Research in Nursing & Health. 44, 620–632. 10.1002/nur.22158
REFERENCES
- Al Ghoson, A. M. (2010). Decision tree induction & clustering techniques in SAS Enterprise Miner, SPSS Clementine, And IBM Intelligent Miner—A comparative analysis. International Journal of Management & Information Systems, 14(3), 57–70. 10.19030/ijmis.v14i3.841 [DOI] [Google Scholar]
- Babineau, T. , Thomas, A. , & Wu, V. (2019). Physician burnout and compassion fatigue: Individual and institutional response to an emerging crisis. Current Treatment Options in Pediatrics, 5, 1–10. 10.1007/s40746-019-00146-7 [DOI] [Google Scholar]
- Brito‐Pons, G. , & Librada‐Flores, S. (2018). Compassion in palliative care: A review. Current Opinion in Supportive and Palliative Care, 12(4), 472–479. 10.1097/SPC.0000000000000393 [DOI] [PubMed] [Google Scholar]
- Cañadas‐De la Fuente, G. , Ortega, E. , Ramirez‐Baena, L. , De la Fuente‐Solana, E. , Vargas, C. , & Gómez‐Urquiza, J. (2018). Gender, marital status, and children as risk factors for burnout in nurses: A meta‐analytic study. International Journal of Environmental Research and Public Health, 15(10), 2102. 10.3390/ijerph15102102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceylan, Z. (2020). Estimation of COVID‐19 prevalence in Italy, Spain, and France. Science of the Total Environment, 729, 138817. 10.1016/j.scitotenv.2020.138817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coetzee, S. K. , & Klopper, H. C. (2010). Compassion fatigue within nursing practice: A concept analysis. Nursing & Health Sciences, 12(2), 235–243. 10.1111/j.1442-2018.2010.00526.x [DOI] [PubMed] [Google Scholar]
- Coetzee, S. K. , & Laschinger, H. K. (2018). Toward a comprehensive, theoretical model of compassion fatigue: An integrative literature review. Nursing & Health Sciences, 20(1), 4–15. 10.1111/nhs.12387 [DOI] [PubMed] [Google Scholar]
- Conversano, C. , Ciacchini, R. , Orrù, G. , Di Giuseppe, M. , Gemignani, A. , & Poli, A. (2020). Mindfulness, compassion, and self‐compassion among health care professionals: What's new? A systematic review. Frontiers in Psychology, 11, 1683. 10.3389/fpsyg.2020.01683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, A. L. , Brown, J. A. , Rees, C. S. , & Leslie, G. D. (2020). Nurse resilience: A concept analysis. International Journal of Mental Health Nursing, 29(4), 553–575. 10.1111/inm.12721 [DOI] [PubMed] [Google Scholar]
- Craigie, M. , Osseiran‐Moisson, R. , Hemsworth, D. , Aoun, S. , Francis, K. , Brown, J. , Hegney, D. , & Rees, C. (2016). The influence of trait‐negative affect and compassion satisfaction on compassion fatigue in australian nurses. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 88–97. 10.1037/tra0000050 [DOI] [PubMed] [Google Scholar]
- Crawford, P. , Brown, B. , Kvangarsnes, M. , & Gilbert, P. (2014). The design of compassionate care. Journal of Clinical Nursing, 23(23–24), 3589–3599. 10.1111/jocn.12632 [DOI] [PubMed] [Google Scholar]
- Cummings, C. , Singer, J. , Hisaka, R. , & Benuto, L. T. (2018). Compassion satisfaction to combat work‐related burnout, vicarious trauma, and secondary traumatic stress. Journal of Interpersonal Violence, 36, 5304. 10.1177/0886260518799502 [DOI] [PubMed] [Google Scholar]
- Delaney, M. C. (2018). Caring for the caregivers: Evaluation of the effect of an eight‐week pilot mindful self‐compassion (MSC) training program on nurses' compassion fatigue and resilience. PLOS One, 13(11), e0207261. 10.1371/journal.pone.0207261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado, C. , Upton, D. , Ranse, K. , Furness, T. , & Foster, K. (2017). Nurses' resilience and the emotional labour of nursing work: An integrative review of empirical literature. International Journal of Nursing Studies, 70, 71–88. 10.1016/j.ijnurstu.2017.02.008 [DOI] [PubMed] [Google Scholar]
- Duarte, J. , & Pinto‐Gouveia, J. (2017). The role of psychological factors in oncology nurses' burnout and compassion fatigue symptoms. European Journal of Oncology Nursing, 28, 114–121. 10.1016/j.ejon.2017.04.002 [DOI] [PubMed] [Google Scholar]
- Duarte, J. , Pinto‐Gouveia, J. , & Cruz, B. (2016). Relationships between nurses' empathy, self‐compassion and dimensions of professional quality of life: A cross‐sectional study. International Journal of Nursing Studies, 60, 1–11. 10.1016/j.ijnurstu.2016.02.015 [DOI] [PubMed] [Google Scholar]
- Edo‐Gual, M. , Monforte‐Royo, C. , Aradilla‐Herrero, A. , & Tomás‐Sábado, J. (2015). Death attitudes and positive coping in Spanish nursing undergraduates: A cross‐sectional and correlational study. Journal of Clinical Nursing, 24(17–18), 2429–2438. 10.1111/jocn.12813 [DOI] [PubMed] [Google Scholar]
- Faqihi, F. , Alharthy, A. , Alodat, M. , Asad, D. , Aletreby, W. , Kutsogiannis, D. J. , Brindley, P. G. , & Karakitsos, D. (2017). The development of compassionate engagement and action scales for self and others. Journal of Compassionate Health Care, 4(1), 1–24. 10.1186/s40639-017-0033-3 [DOI] [Google Scholar]
- Figley, C. R. (2004). Systemic traumatization: Secondary traumatic stress disorder in family therapists. In Mikesell R. H., Lusterman D.‐D., & McDaniel S. H. (Eds.), Integrating family therapy: Handbook of family psychology and systems theory (pp. 571–581). American Psychological Association. 10.1037/10172-033 [DOI] [Google Scholar]
- Galiana, L. , Arena, F. , Oliver, A. , Sansó, N. , & Benito, E. (2017). Compassion satisfaction, compassion fatigue, and burnout in Spain and Brazil: ProQOL validation and cross‐cultural diagnosis. Journal of Pain and Symptom Management, 53(3), 598–604. [DOI] [PubMed] [Google Scholar]
- Garcia‐Campayo, J. , Navarro‐Gil, M. , Andrés, E. , Montero‐Marin, J. , López‐Artal, L. , & Demarzo, M. M. P. (2014). Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self‐Compassion Scale (SCS). Health and Quality of Life Outcomes, 12(1), 4. 10.1186/1477-7525-12-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geoffrion S., Morselli, C. , & Guay, S. (2016). Rethinking compassion fatigue through the lens of professional identity: The case of child protection workers. Trauma, Violence and Abuse, 17(3), 270–283. 10.1177/1524838015584362 [DOI] [PubMed] [Google Scholar]
- Gilbert, P. (2015). The evolution and social dynamics of compassion. Social and personality psychology compass, 9(6), 239–254. 10.1111/spc3.12176 [DOI] [Google Scholar]
- Greenberg, N. , Docherty, M. , Gnanapragasam, S. , & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during COVID‐19 pandemic. BMJ, 368, m1211. 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- Halcomb, E. , McInnes, S. , Williams, A. , Ashley, C. , James, S. , Fernandez, R. , Stephen, C. , & Calma, K. (2020). The experiences of primary healthcare nurses during the COVID‐19 pandemic in Australia. Journal of Nursing Scholarship, 52, 553–563. 10.1111/jnu.12589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayuni, G. , Hasson‐Ohayon, I. , Goldzweig, G. , Bar Sela, G. , & Braun, M. (2019). Between empathy and grief: The mediating effect of compassion fatigue among oncologists. Psycho‐Oncology, 28(12), 2344–2350. 10.1002/pon.5227 [DOI] [PubMed] [Google Scholar]
- Henshall, C. , Davey, Z. , & Jackson, D. (2020). Nursing resilience interventions. A way forward in challenging healthcare territories. Journal of Clinical Nursing, 29(19–20), 3597–3599. 10.1111/jocn.15276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeve, Y. T. , Jansen, G. , & Roodbol, P. (2014). The nursing profession: Public image, self‐concept and professional identity. A discussion paper. Journal of Advanced Nursing, 70(2), 295–309. 10.1111/jan.12177 [DOI] [PubMed] [Google Scholar]
- Hunt, P. , Denieffe, S. , & Gooney, M. (2019). Running on empathy: Relationship of empathy to compassion satisfaction and compassion fatigue in cancer healthcare professionals. European Journal of Cancer Care, 28(5), e13124. 10.1111/ecc.13124 [DOI] [PubMed] [Google Scholar]
- Jenkins, B. , & Warren, N. A. (2012). Concept analysis: Compassion fatigue and effects upon critical care nurses. Critical Care Nursing Quarterly, 35(4), 388–395. 10.1097/CNQ.0b013e318268fe09 [DOI] [PubMed] [Google Scholar]
- Jolliffe, D. , & Farrington, D. P. (2006). Development and validation of the basic empathy scale. Journal of Adolescence, 29(4), 589–611. 10.1016/j.adolescence.2005.08.010 [DOI] [PubMed] [Google Scholar]
- Klimecki, O. , & Singer, T. (2012). Empathic distress fatigue rather than compassion fatigue? Integrating findings from empathy research in psychology and social neuroscience. In Oakley B., Knafo A., Madhavan G., & Wilson D. S. (Eds.), Pathological altruism (pp. 368–383). Oxford University Press. [Google Scholar]
- Lahana, E. , Papadopoulou, K. , Roumeliotou, O. , Tsounis, A. , Sarafis, P. , & Niakas, D. (2017). Burnout among nurses working in social welfare centers for the disabled. BMC Nursing, 16(1), 15. 10.1186/s12912-017-0209-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, C.‐C. , Wang, C.‐Y. , Wang, Y.‐H. , Hsueh, S.‐C. , Ko, W.‐C. , & Hsueh, P.‐R. (2020). Global epidemiology of coronavirus disease 2019 (COVID‐19): Disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. International Journal of Antimicrobial Agents, 55(4), 105946. 10.1016/j.ijantimicag.2020.105946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Z. , Ge, J. , Yang, M. , Feng, J. , Qiao, M. , Jiang, R. , Bi, J. , Zhan, G. , Xu, X. , Wang, L. , Zhou, Q. , Zhou, C. , Pan, Y. , Liu, S. , Zhang, H. , Yang, J. , Zhu, B. , Hu, Y. , Hashimoto, K. , … Yang, C. (2020). Vicarious traumatization in the general public, members, and non‐members of medical teams aiding in COVID‐19 control. Brain, Behavior, and Immunity, 88, 916–919. 10.1016/j.bbi.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim, D. , & DeSteno, D. (2016). Suffering and compassion: The links among adverse life experiences, empathy, compassion, and prosocial behavior. Emotion, 16(2), 175–182. 10.1037/emo0000144 [DOI] [PubMed] [Google Scholar]
- Lown, B. A. , Muncer, S. J. , & Chadwick, R. (2015). Can compassionate healthcare be measured? The Schwartz Center Compassionate Care ScaleTM . Patient Education and Counseling, 98(8), 1005–1010. 10.1016/j.pec.2015.03.019 [DOI] [PubMed] [Google Scholar]
- Maslach, C. , & Jackson, S. E. (1981). The measurement of experienced Burnout. Journal of Occupational Behavior, 2, 99–113. 10.1002/job.4030020205 [DOI] [Google Scholar]
- Mills, J. , Wand, T. , & Fraser, J. A. (2017). Palliative care professionals' care and compassion for self and others: A narrative review. International Journal of Palliative Nursing, 23(5), 219–229. 10.12968/ijpn.2017.23.5.219 [DOI] [PubMed] [Google Scholar]
- Molina‐Praena, J. , Ramirez‐Baena, L. , Gómez‐Urquiza, J. L. , Cañadas, G. R. , & De la Fuente, E. I. (2018). Levels of burnout and risk factors in medical area nurses: A meta‐analytic study. International Journal of Environmental Research and Public Health, 15(12), 2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney, C. , Fetter, K. , Gross, B. W. , Rinehart, C. , Lynch, C. , & Rogers, F. B. (2017). A preliminary analysis of compassion satisfaction and compassion fatigue with considerations for nursing unit specialization and demographic factors. Journal of Trauma Nursing, 24(3), 158–163. 10.1097/JTN.0000000000000284 [DOI] [PubMed] [Google Scholar]
- Morante‐Benadero, M. E. , Moreno‐Jiménez, B. , & Rodríguez‐Muñoz, A. (2006). Professional satisfaction and fatigue subscales—Version IV (ProQOL). Spanish translation of the instrument. http://www.proqol.org/uploads/ProQol_vIV_Spanish_Oct05.pdf
- Nabizadeh‐Gharghozar, Z. , Adib‐Hajbaghery, M. , & Bolandianbafghi, S. (2020). Nurses' job burnout: A hybrid concept analysis. Journal of Caring Sciences, 9(3), 154–161. 10.34172/jcs.2020.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff, K. D. (2003). The development and validation of a scale to measure self‐compassion. Self and Identity, 2(3), 223–250. 10.1080/15298860309027 [DOI] [Google Scholar]
- Nolte, A. G. , Downing, C. , Temane, A. , & Hastings‐Tolsma, M. (2017). Compassion fatigue in nurses: A metasynthesis. Journal of Clinical Nursing, 26(23–24), 4364–4378. 10.1111/jocn.13766 [DOI] [PubMed] [Google Scholar]
- Oliva Delgado, A. , Antolín Suárez, L. , Pertegal Vega, M. Á. , Ríos Bermúdez, M. , & Parra Jiménez, Á. (2011). Instruments for assessing mental health and positive adolescent development and the assets that promote it. Seville (Spain): Ministry of Health. Government of Andalusia.
- Roney, L. N. , & Acri, M. C. (2018). The cost of caring: An exploration of compassion fatigue, compassion satisfaction, and job satisfaction in pediatric nurses. Journal of Pediatric Nursing, 40, 74–80. 10.1016/j.pedn.2018.01.016 [DOI] [PubMed] [Google Scholar]
- Ruiz‐Fernández, M. D. , Pérez‐García, E. , & Ortega‐Galán, Á. M. (2020). Quality of life in nursing professionals: Burnout, fatigue, and compassion satisfaction. International Journal of Environmental Research and Public Health, 17(4), 1253. 10.3390/ijerph17041253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco, T. L. , & Copel, L. C. (2018). Compassion satisfaction: A concept analysis in nursing. Nursing Forum, 53(1), 76–83. 10.1111/nuf.12213 [DOI] [PubMed] [Google Scholar]
- Schwartz, C. , Meisenhelder, J. B. , Ma, Y. , & Reed, G. (2003). Altruistic social interest behaviors are associated with better mental health. Psychosomatic Medicine, 65(5), 778–785. 10.1097/01.psy.0000079378.39062.d4 [DOI] [PubMed] [Google Scholar]
- Shanafelt, T. , Ripp, J. , & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic. Journal of the American Medical Association, 323(21), 2133–2134. 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- Sinclair, S. , Beamer, K. , Hack, T. F. , McClement, S. , Raffin Bouchal, S. , Chochinov, H. M. , & Hagen, N. A. (2017). Sympathy, empathy, and compassion: A grounded theory study of palliative care patients' understandings, experiences, and preferences. Palliative Medicine, 31(5), 437–447. 10.1177/0269216316663499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick, S. M. , Bonanno, G. A. , Masten, A. S. , Panter‐Brick, C. , & Yehuda, R. (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5, 1. 10.3402/ejpt.v5.25338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamm, B. (2005). The professional quality of life scale: Compassion satisfaction, burnout & compassion fatigue/secondary trauma scales. Lutherville, MD.
- Stuntzner, S. (2015). Self‐compassion: Stop beating yourself up and leave insecurity behind By: Dr. Kristen Neff (review). Counseling faculty publications and presentations. https://scholarworks.utrgv.edu/coun_fac/9
- Sánchez‐Teruel, D. , & Robles‐Bello, M. A. (2015). 4‐item resilience scale (RS‐14): Psychometric properties of the spanish version. Revista Iberoamericana de Diagnóstico y Evaluación–e Avaliação Psicológica, 40(2), 103–113. [Google Scholar]
- Terry, V. R. , Graham, C. J. , Rogers, C. , Craigie, M. , Hegney, D. G. , Rees, C. S. , & Small, C. (2019). Building resilience among rural and remote nurses in Queensland, Australia. Collegian, 27(3), 265–270. 10.1016/j.colegn.2019.08.007 [DOI] [Google Scholar]
- Wagnild, G. (2009). The resilience scale user's guide: For the US English version of the Resilience Scale and the 14‐item Resilience Scale (RS‐14). Montana, USA: The Resilience Center.
- Winner, J. , & Knight, C. (2019). Beyond burnout: Addressing system‐induced distress. Family Practice Management, 26(5), 4–7. 10.1016/j.dib.2020.105619 [DOI] [PubMed] [Google Scholar]


