Abstract
Aims and Objectives
We aimed to determine the impact of COVID‐19 related home confinement on the paediatric population by focusing on anxiety, behavioural disturbances and somatic symptoms.
Background
To limit the spread of the COVID‐19 outbreak, governments have imposed nationwide lockdowns to prevent direct contact; this has affected everyday lives and activities such as attending school classes. Such isolation may have impacted children’s anxiety levels.
Design and Methods
We conducted a cross‐sectional observational study using a web‐based anonymous questionnaire from 22–26 April, 2020, among children (N = 2,292) in Spain. For children below 7 years of age, parents reported the children’s behavioural, emotional and somatic symptoms and family environment data on a questionnaire designed by the researchers. Children over 7 years answered the Revised Children’s Manifest Anxiety Scale either independently or with their parents’ assistance.
Results
Children over 7 years, boys in particular, scored high on the anxiety spectrum. Moreover, participants who knew someone who had suffered from COVID‐19 at home or whose parent was directly involved in the pandemic, obtained higher Total Anxiety scores. Significantly high values were found in all aspects of anxiety among those who feared infection or whose parents been unemployed. Of the children below 7 years, 56.3% had four or more anxiety‐related symptoms, the most frequent of which were tantrums, emotional changes, restlessness and fear of being alone. The number of symptoms reported was significant when someone in the family home had been infected with COVID‐19.
Conclusions
The COVID‐19 home confinement had a significant impact on children, causing anxiety, behavioural problems and somatic manifestations.
Relevance to clinical practice
Nurses play a key role in screening children who have experience confinement owing to the COVID‐19 pandemic in order to detect early anxiety symptoms using tele‐health. Suitable direct interventions can then be implemented or interdisciplinary manage could be started.
Keywords: anxiety, communicable diseases, confinement, COVID‐19, mental health, nursing
What does this paper contribute to the wider global community?
Vulnerable children should be closely monitored during confinement to identify anxiety situations that could trigger them.
Although new tools have been developed to help individuals survive this pandemic, social distancing, avoiding direct physical contact and self‐isolation continue to be valid measures; however, these are also risk factors that can increase anxiety levels, especially in children.
1. INTRODUCTION
In December 2019, a novel coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), emerged in Wuhan, China (Guan et al., 2020). Since then, it has caused a pandemic with vast health and economic repercussions, afflicting 119 million people and causing 2.6 million mortalities (World Health Organization, 2021). The disease, termed COVID‐19 by the WHO, has a wide range of clinical manifestations, ranging from a mild, self‐limiting form to multiple‐organ failure and death (Chen et al., 2020; Liu et al., 2020). However, paediatric manifestations appear to take a milder form of the disease (Cao et al., 2020; García‐Salido, 2020; Götzinger et al., 2020).
The global focus is to mitigate transmission and reduce the economic impact of COVID‐19. Social distancing measures are among the strategies to limit transmission, reduce in‐person contact and protect at‐risk populations. In the beginning of March 2020, Spain’s cases increased exponentially, with China as the origin and Italy as a reference to the disease’s impact in Europe. On 10 March, China had 80,944 confirmed cases and 3,157 deaths, while Italy had 10,969 confirmed cases and 560 mortalities (World Health Organization, 2020a).
Spain closed its schools on 10 March, 2020, after reaching 1,459 cases and 46 deaths. In the following week, on 14 March, the government imposed a nationwide lockdown when the daily infections and mortalities increased to 5,497 and 156, respectively (World Health Organization, 2020b). All residents were mandated to stay home, except in special cases, such as visiting shops for food or medicine or going to the hospital. On 21 April, 2020, after 44 days of home confinement, the government announced that from 27 April, 2020, children under the age of 14 would be allowed to go outside for short walks accompanied by their parents or other adults from the same household.
Owing to a second wave from mid‐October 2020, the Spanish government imposed a new lockdown with regional confinement and a national curfew from midnight to 6 a.m. from 25 October, 2020, until 9 May, 2021, with restrictions increasing in mid‐March, finishing third wave and expecting a fourth. At that time Spain in had exceeded 3.2 million reported cases and 72,793 mortalities, with an increase of 60,150 diagnosed cases within 14 days (Centro de Coordinación y Alerta de Emergencias Sanitarias and Ministerio de Sanidad, 2021).
Currently, Spain and the rest of Europe are facing a new COVID‐19 wave. In the first half of March 2021, Europe reported 20,809 new deaths and 1.2 million new cases in a week, which translates to 40% of the global cases (World Health Organization, 2021); this was similar to the numbers observed during mid‐October 2020. Subsequently, European governments have enforced partial lockdowns, restricting the number of people in meetings or events, and closing non‐essential businesses, restaurants and bars. Schools could remain open, and children’s routines have had to adapt to the different waves of the pandemic. However, if Europe continues to see a spike in case numbers, governments may have to reinstate school closures, which would pose a similar situation as that in April 2020.
2. BACKGROUND
SARS‐CoV‐2 virus and the situation around it is novel in many ways. Healthcare workers have been managing the impact of the pandemic for almost a year. They have found many ways to tackle the virus, despite various aspects of COVID‐19’s physiopathology still being unknown, and we value their efforts. Nevertheless, the general population has never had to suffer such stringent restrictions such as working online, isolating elders in residences, keeping children at home while attending school classes online, and restricting in‐person contact.
During the unprecedented March to April 2020 confinement period, Spain and Italy had one of the strictest lockdowns in Europe and even briefly halted non‐essential production altogether (University of Oxford, 2020). Children were exposed to vast amounts of information from socialising in their home environment and online, as well as the media, which was heavily dominated by grave issues surrounding the pandemic. Furthermore, they were subjected to substantial changes in their daily routines, such as online learning, suspension of playing outside and interruption of face‐to‐face relationships. With their social infrastructure removed, they were exposed to the high levels of stress and anxiety of the adults around them (Bradbury‐Jones & Isham, 2020; Guessoum et al., 2020; Murray et al., 2009; Wood et al., 2003). This new situation may have caused anxiety in children, as well as behavioural problems and somatic manifestations (Brooks et al., 2020; Dalton et al., 2020). Moreover, due to limited direct contact, school closures resulted in increased feelings of isolation and loneliness, possibly triggering mental health problems, both by internalising and externalising issues, the duration of loneliness having been a predictor of these problems (Bukowski & Adams, 2005; Laursen et al., 2007; Loades et al., 2020).
In addition, physical activity during home confinement was reduced, sports events suspended, especially social or contact sports, with the consequent risk of developing emotional or psychological problems. Not only would the largely increased screen time spent in virtual classes and interacting with peers have had a negative health impact (Carson et al., 2016), but limited physical activity or dropping out of sports may have also caused psychological difficulties in children. Sport is especially valuable for females in combatting mild depressive symptoms (Bailey et al., 2018). Notably, the reduction in physical activity may not have impacted adolescents as much (Van Dijk et al., 2016). Other implication with negative outcomes was the fact of the spent large time in front of screens (Carson et al., 2016), in pandemic, being in class or speaking with peers.
We investigated the impact of lockdown and assessed whether the COVID‐19 related confinement compounded paediatric stress, consequently presenting as anxiety, behavioural disturbances related to the anxiety spectrum, or somatic disorders.
3. METHOD
3.1. Design
This research used a cross‐sectional observational study design.
3.2. Setting
We conducted the study using a web‐based anonymous questionnaire from 00:00 on 22–23:59 on 26 April 2020 among children (N = 2,292) in Spain. The data were collected online. Parents received an informative message with a link to the questionnaire, distributed through social media in Madrid and Barcelona. After reading the informed consent document and agreeing to participate in the study, participants were asked to complete the questionnaire. For children younger than 7 years old, parents reported their children’s symptoms. Children older than 7 years answered their questionnaire either independently or with their parents’ assistance where needed. The participants were supported by EU and Spanish data and privacy laws. We only recorded the time track, and no other data, such as location or IP address, were collected. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist was followed for this study (see Supplementary File 1).
3.3. Participants
Children under 17 years of age were included in the study. The sample was collected using snowball‐sampling technique during the time window.
3.4. Measurement
The questionnaire consisted of two parts. First, the following information was collected: age and gender of the child, and information on the family environment related to COVID‐19. The second part of the questionnaire included age‐specific questions divided into two sections: for children below 7 years of age and for those over 7 years of age.
3.5. Children aged 7 years and older: Children's Manifest Anxiety Scale
We used the validated Spanish version (Gussinyé Canabal, 2005) of the revised Children’s Manifest Anxiety Scale’s (Reynolds & Richmond, 1997) for children older than 7 years. The 37‐item self‐report questionnaire assesses the anxiety symptoms (physiological, subjective and motoric symptoms) and spectrum manifested in children aged 6–19 years old by means of the following scores: total anxiety (TA), physiological anxiety (PA), restlessness or hypersensitivity (R/H), and social concerns and concentration (Sc/C). Scores range from 0–28, and the score obtained is transformed into a percentile. Results between the 40th and 74th percentiles are considered moderate expressions of anxiety that could generate psychological distress in children. Percentiles greater than 75th are considered clinically significant, in which case the child is likely to benefit from professional care. Reliability was established as Cronbach’s alphas were 0.83 for the original paper and 0.818 for our sample (Appendix S1, Assessment of Stress in Children and Adolescents Exposed to COVID‐19 Pandemic: Children aged 7 years and older questionnaire).
3.6. Children younger than 7 years: Research's Developed Anxiety Questionnaire
We designed a questionnaire based on the DSM‐V criteria, and our institution’s paediatric team’s experience and consultations during confinement since it reflected the actual problems and symptoms in children and families. We checked the paediatric HM Hospitales team’s recommendations against previous literature (Caballo & Simón, 2012; Costello et al., 2005). Moreover, we included the symptoms to explore the most common physical manifestations or somatisations related to anxiety and evaluate their frequency compared to that before confinement. The children’s parents answered the questionnaire item checklist according to the increased presence of behavioural, emotional and somatic symptoms in their child during the confinement compared to that during pre‐confinement (Appendix S2, Assessment of Stress in Children and Adolescents Exposed to COVID‐19 Pandemic: Children <7 years of age). As it was not our study aim to validate the research team’s survey, the scale has not been validated.
3.7. Ethical considerations
Ethics approval for this study was granted by the ethics committee of HM Hospitales (approval number 20.04.1603‐GHM). Participants give their consent to participate by accepting an Informed Consent prior to the survey. Participants were assured that their data would not be shared with anyone other than the research team and used for research purposes only.
3.8. Data analysis
We used spss version 24.0 for the analyses. The Kolmogorov–Smirnov test with Lilliefors correction was used to evaluate the normal distribution of the data within the collected variables. Data were expressed as means ± standard deviation (SD) for continuous variables and numbers and percentages for categorical variables, and analysed using chi‐squared and Fisher’s exact tests. Two types of tests were applied for continuous variables: a two‐tailed test when the normality and homogeneity of variance assumptions were met, and the nonparametric Mann–Whitney U test for non‐normally distributed variables. To compare more than two groups, data were analysed using analysis of variance (ANOVA) with Bonferroni post hoc test or the nonparametric Kruskal–Wallis test. For all statistical tests, we considered statistically significant differences with a confidence interval (CI) of 95% or higher (p ≤.05).
4. RESULTS
The data were obtained from eligible individuals, including 2,292 children (boys: N = 1,145; 49.9%; girls: N = 1,147; 50.1%) under 17 years of age (7 years or older: N = 989 [43.1%]; younger than 7 years old: N = 1,303 [56.8%]) who were subjected to a confinement period of 39−44 days. Our analyses showed there were no missing data (<5%). Among the boys, 51.4% (N = 670) and 48% (N = 475) were younger than 7 years and 7 years or older, respectively.
Figure 1 shows the ages of the surveyed individuals. Table 1 summarises the findings and characteristics of the older age group, with the anxiety percentiles obtained from the RCMAS. Table 2 lists the anxiety spectrum values according to the different factors surveyed.
FIGURE 1.
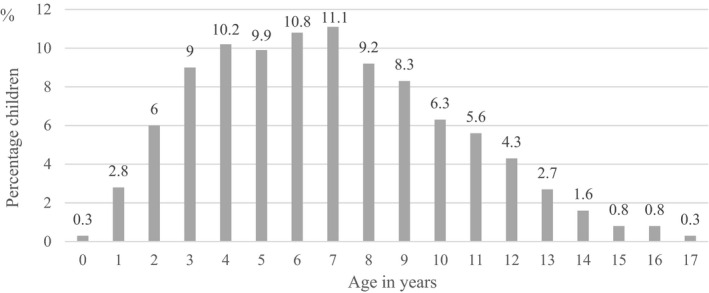
Participants’ age (in years) distribution as percentages (N = 2,292). Participants’ (those aged 0–17 years) data distribution as percentages
TABLE 1.
Anxiety percentile distribution for children aged 7 years or more
|
n = 989 No. (%) |
||||
|---|---|---|---|---|
| Percentile | TA | PA | R/H | Sc/C |
| p3 | 16 (1.6) | 34 (3.4) | 5 (0.5) | 0 |
| p25 | 278 (28.1) | 349 (35.3) | 113 (11.4) | 380 (38.4) |
| p50 | 262 (26.5) | 248 (25.1) | 267 (27) | 213 (21.5) |
| p75 | 202 (20.5) | 205 (20.8) | 263 (26.6) | 188 (19) |
| p97 | 195 (19.7) | 122 (12.3) | 290 (29.3) | 169 (17.1) |
| p99 | 36 (3.6) | 31 (3.1) | 51 (5.2) | 39 (4) |
Abbreviations: No, individuals surveyed; p, percentile; PA, physiological anxiety; R/H, restlessness or hypersensitivity; Sc/C, social concerns or concentration; TA, total anxiety.
TABLE 2.
Frequency and statistical significance for children aged 7 years or more
| n = 989 | Mean ± SD | p Value | ||
|---|---|---|---|---|
| Male | Female | |||
| Children gender | No. (%) | 475 (48) | 514 (52) | |
| TA | 53.2 ± 28.6 | 42.6 ± 28.7 | <.001 | |
| PA | 42.9 ± 28.4 | 37.8 ± 28.9 | .005 | |
| R/H | 65.6 ± 24.0 | 53.7 ± 25.6 | <.001 | |
| Sc/C | 47.5 ± 30.1 | 39.2 ± 30.2 | .001 | |
| Yes | No | p Value | ||
| Does the child have close relatives affected by COVID‐19? | No. (%) | 240 (24.3) | 749 (75.7) | |
| TA | 48.9 ± 29.8 | 47.3 ± 28.9 | .465 | |
| PA | 42.6 ± 30.0 | 39.6 ± 28.4 | .160 | |
| R/H | 59.7 ± 25.6 | 59.4 ± 25.5 | .857 | |
| Sc/C | 42.7 ± 30.2 | 43.3 ± 30.4 | .759 | |
| Has someone at home been affected or infected by COVID‐19? | No. (%) | 124 (12.5) | 865 (87.5) | |
| TA | 53.0 ± 30.2 | 47.0 ± 28.9 | .034 | |
| PA | 49.0 ± 31.7 | 39.1 ± 28.1 | <.001 | |
| R/H | 59.4 ± 27.2 | 59.5 ± 25.3 | .984 | |
| Sc/C | 46.7 ± 27.6 | 42.7 ± 30.7 | .138 | |
| Has any death occurred due to COVID‐19 close to the child’s environment? | No. (%) | 123 (12.4) | 866 (87.6) | |
| TA | 49.2 ± 28.8 | 47.5 ± 29.1 | .552 | |
| PA | 43.9 ± 29.4 | 39.8 ± 28.7 | .134 | |
| R/H | 62.2 ± 23.7 | 59.1 ± 25.8 | .209 | |
| Sc/C | 40.5 ± 30.5 | 43.6 ± 30.4 | .296 | |
| Has someone informed the child of this death? | No. (%) | 135 (13.7) | 854 (86.3) | |
| TA | 49.2 ± 29.3 | 47.5 ± 29.1 | .541 | |
| PA | 44.1 ± 29.3 | 39.7 ± 28.7 | .098 | |
| R/H | 61.2 ± 23.9 | 59.2 ± 25.8 | .397 | |
| Sc/C | 40.1 ± 30.6 | 43.7 ± 30.3 | .214 | |
| Has any of the parents been directly implied in the COVID‐19 pandemic? | No. (%) | 384 (38.8) | 605 (61.2) | |
| TA | 50.7 ± 30.2 | 45.8 ± 28.2 | .012 | |
| PA | 44.4 ± 30.2 | 37.7 ± 27.5 | <.001 | |
| R/H | 61.0 ± 25.9 | 58.5 ± 25.3 | .123 | |
| Sc/C | 44.8 ± 30.9 | 42.1 ± 30.0 | .186 | |
| Does someone regularly talk to the child about the situation he/she is experiencing? | No. (%) | 866 (87.6) | 123 (12.4) | |
| TA | 47.9 ± 29.2 | 46.4 ± 29.0 | .602 | |
| PA | 40.9 ± 28.9 | 36.1 ± 27.0 | .090 | |
| R/H | 59.5 ± 25.6 | 59.4 ± 25.2 | .963 | |
| Sc/C | 43.0 ± 30.3 | 44.4 ± 31.0 | .634 | |
| I worried about seeing my grandparents | No. (%) | 789 (79.8) | 200 (20.2) | |
| TA | 50.1 ± 29.3 | 38.7 ± 26.6 | <.001 | |
| PA | 42.2 ± 29.0 | 32.8 ± 26.8 | <.001 | |
| R/H | 61.8 ± 25.2 | 50.5 ± 24.7 | <.001 | |
| Sc/C | 44.7 ± 30.8 | 37.2 ± 27.7 | .001 | |
| I miss my friends | No. (%) | 917 (92.7) | 72 (7.3) | |
| TA | 48.0 ± 29.3 | 44.1 ± 27.4 | .280 | |
| PA | 40.6 ± 28.9 | 35.9 ± 27.2 | .183 | |
| R/H | 59.8 ± 25.6 | 56.2 ± 23.9 | .259 | |
| Sc/C | 43.3 ± 30.5 | 41.6 ± 28.8 | .657 | |
| I have trouble concentrating on my homework | No. (%) | 532 (53.8) | 457 (46.2) | |
| TA | 58.2 ± 28.3 | 35.8 ± 25.2 | <.001 | |
| PA | 49.2 ± 29.9 | 30.0 ± 23.6 | ||
| R/H | 65.8 ± 24.6 | 52.2 ± 24.6 | ||
| Sc/C | 55.8 ± 28.5 | 28.5 ± 25.5 | ||
| I am worried about getting COVID‐19 | No. (%) | 530 (53.6) | 459 (46.4) | |
| TA | 54.5 ± 28.5 | 40.0 ± 27.9 | <.001 | |
| PA | 45.3 ± 29.0 | 34.5 ± 27.4 | ||
| R/H | 66.3 ± 23.8 | 51.7 ± 25.3 | ||
| Sc/C | 48.3 ± 31.2 | 37.2 ± 28.2 | ||
| I am worried about my parents losing their jobs | No. (%) | 432 (43.7) | 557 (56.3) | |
| TA | 56.3 ± 28.9 | 41.2 ± 27.6 | <.001 | |
| PA | 48.6 ± 29.5 | 33.9 ± 26.5 | ||
| R/H | 66.8 ± 24.4 | 53.9 ± 25.0 | ||
| Sc/C | 48.5 ± 31.0 | 39.0 ± 29.2 |
Abbreviations: No, subjects surveyed; PA, physiological anxiety; R/H, restlessness or hypersensitivity; Sc/C, social concerns or concentration; TA, total anxiety.
In the younger age group, the most common paediatric symptoms included tantrums (56.4%), emotional changes (34.1%), restlessness (33.6%) and fear of being alone (33.2%) (Figure 2). Furthermore, 50.9%, 15%, 13.9%, 11% and 9.2% of the participants reported four or more, three, two, one and no symptoms, respectively. To assess the influence of those aspects of a child's environment that were included in the questionnaire, we further clustered the groups by number of symptoms experienced into the following categories: children with three or more (65.9%), one or two (24.9%), and no (9.2%) symptoms. Interestingly, a significant difference between groups (p = .027) was observed only when a family member had been affected or infected by COVID‐19 (Table 3).
FIGURE 2.
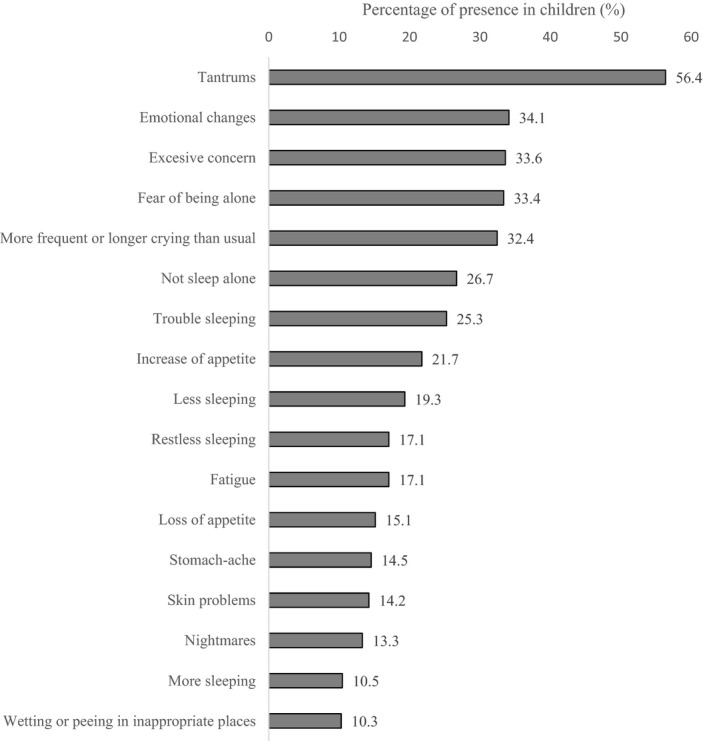
Most frequent symptoms in children younger than 7 years. Symptoms most frequently appearing in children younger than 7 years, expressed as a percentage of the total number of children with symptoms. Note. The complete name of ‘Trouble sleeping’ is ‘Trouble sleeping (the child wakes up more often than usual during the night)’
TABLE 3.
Children aged less than 7 years categorised by number of symptoms, frequency and statistical significance
| n = 1,303 | No. (%) | Chi‐square | p Value | ||
|---|---|---|---|---|---|
| YES | NO | ||||
| Does the child have close relatives affected by COVID‐19? | No. (%) | 260 (20) | 1,043 (80) | ||
| 0 S | 21 (17.5) | 99 (82.5) | 1.608 | .448 | |
| 1–2 S | 59 (18.2) | 265 (81.8) | |||
| ≥3 S | 180 (21) | 679 (79) | |||
| Has someone at home been affected or infected by COVID‐19? | No. (%) | 152 (11.7) | 1,151 (88.3) | ||
| 0 S | 10 (8.3) | 110 (91.7) | 7.257 | .027 | |
| 1–2 S | 27 (8.3) | 297 (91.7) | |||
| ≥3 S | 115 (13.4) | 744 (86.6) | |||
| Has any death occurred due to COVID‐19 close to the child’s environment? | No. (%) | 93 (7.1) | 1,210 (92.9) | ||
| 0 S. | 4 (3.3) | 116 (96.7) | 3.328 | .189 | |
| 1–2 S | 27 (8.3) | 297 (91.7) | |||
| ≥3 S | 62 (7.2) | 797 (92.8) | |||
| Has someone informed the child of this death? | No. (%) | 71 (5.4) | 1,232 (94.6) | ||
| 0 S | 6 (5) | 114 (95) | .450 | .798 | |
| 1–2 S | 20 (6.2) | 304 (93.8) | |||
| ≥3 S | 45 (5.2) | 814 (94.8) | |||
| Has any of the parents been directly implied in the COVID‐19 pandemic? | No. (%) | 505 (38.8) | 798 (61.2) | ||
| 0 S | 40 (33.3) | 80 (66.7) | 1.977 | .372 | |
| 1–2 S | 123 (38) | 201 (62) | |||
| ≥3 S | 342 (39.8) | 517 (60.2) | |||
| Does someone regularly talk to the child about the situation he/she is experiencing? | No. (%) | 957 (73.4) | 346 (26.6) | ||
| 0 S | 84 (70) | 36 (30) | 1.669 | .434 | |
| 1–2 S | 233 (71.9) | 91 (28.1) | |||
| ≥3 S | 640 (74.6) | 219 (25.4) |
Abbreviations: ≥3 S = three or more symptoms 0 = no symptoms; 1–2S = one or two symptoms; No, individuals surveyed.
5. DISCUSSION
At this point, the long‐term consequences of children’s home confinement have not yet been clarified. During the preparation of this manuscript, several recently published articles reached similar conclusions. In our study, 50.9% of the children aged below 7 reported four or more symptoms and 23.3% of those older than 7 years scored above the 75th percentile in the RCMAS. A comparable study conducted during confinement in Hubei, China, found similar results; among 2,330 students, 18.9% of the students reported anxiety symptoms (Xie et al., 2020). Another study conducted across 21 Chinese provinces surveying students aged 12–18 years showed that 36.2% of male and 38.4% of female students exhibited anxiety symptoms (Zhou et al., 2020). In southern Europe, a study conducted in adolescents during the early confinement period revealed that Spanish children reported more behavioural changes than Italian and Portuguese children (Francisco et al., 2020).
Our research was conducted at the very end of the confinement period in Spain, one of the countries with the most restrictive, but most complied with, confinement globally. Therefore, our results were compiled just before the children were allowed to leave the house, making our findings unique and adding differential value to our research. The findings showed that the confinement and stress caused by the pandemic have had a significant impact on the children.
During lockdown, children witnessed the pandemic’s vast health and socioeconomic effects and experienced its profound impact on normal daily routines, including loss of direct contact with peers, family members and nature. The implications ranged from disrupted sleep patterns, diet and household‐harmony, which occasionally caused familial conflict and even domestic violence (Mengin et al., 2020). In general, anxiety disorders are the most frequent psychiatric disorders in children, with an increased prevalence of up to 21% (Creswell et al., 2014; Ruiz Sancho & Lago Pita, 2005). Moreover, evidence suggests that stressful situations can trigger psychological distress (Giannakopoulos et al., 2011; Kolaitis et al., 2003). In this regard, confinement has a profound and potentially long‐lasting psychological impact; 30% of children isolated or quarantined due to pandemic disasters and subsequent disease‐containment responses have reported traumatic stress (Sprang & Silman, 2013).
Our results for children older than 7 years showed that only 0.4% of them scored 0 on the anxiety scale. The mean percentile of total anxiety in these children was 47.7 ± 27.9. Among them, 54% and 23.3% scored above the 40th and 75th percentiles, respectively. A high percentile on the RCMAS does not necessarily indicate the presence of an anxiety disorder. However, since those percentiles correlate with anxiety symptoms, it requires further examination and professional intervention according to the RCMAS (Ruiz Sancho & Lago Pita, 2005). Furthermore, for children over 7 years old, despite the slight gender imbalance (48% male vs. 52% female), both sexes had high anxiety scores in all aspects of anxiety covered by the RCMAS, but the male anxiety levels were significantly higher across the board (p < .01, Table 2). This finding, despite contravening the majority of published studies (Canals et al., 2019; Esbjorn et al., 2010; Mohammadi et al., 2020), is not an isolated fact (Costa et al., 2020).
Admittedly, this study was focused on children experiencing confinement in the general population, supposedly without previous mental disorders or grouped characteristics, and there is no specific consideration thereunder. Although personality patterns tend to make females more anxious, the particular circumstances and management of each child’s confinement must be considered. High to very high scores were obtained for anxiety‐provoking environmental factors in the child’s surroundings which may previously have been seen as not influencing the child’s anxiety. However, considering the factors impacting a child, significantly higher scores on the TA scale were obtained by participants who have a healthcare worker for a parent (p50.7 ± 30.2 vs. p45.8 ± 28.2, p = .012) or whose parent has suffered from COVID‐19 at home (p53 ± 30.2 vs. p47 ± 28.9, p = .034). Furthermore, very significant values were found in all assessed aspects of anxiety in those who feared COVID‐19 infection (p < .001) or whose parents lost their jobs (p < .001) (Table 2). The factor of exposure to COVID‐19 related death in the child’s environment did not show a difference in score. All participants were aware of this issue, according to their responses, but both groups showed high mean scores (TA: p49.2 ± 28.8 vs. p47.5 ± 29.1, p = .552), thus not significantly influencing participants’ anxiety levels (Table 2).
The anxiety scores were not significantly different between the group of children that were exposed to COVID‐19 conversations and those who were not; both groups showed high scores (TA: p47.9 ± 29.2 vs. p46.4 ± 29, p = .602). This may indicate that the children were aware and affected by the situation despite not being directly involved in those conversations.
Considering relationships with friends, most (92.9%) participants missed being in contact with their friends, but their anxiety scores were not significantly different from those who did not. This result may be misunderstood by the nurturing of relationships with friends through mobile devices, online games and virtual classrooms. In contrast, those who missed their grandparents (79.9%) showed significantly higher scores in all aspects of anxiety (p < .001). This may be due to identifying older people as being more vulnerable to COVID‐19 (Table 2).
In terms of age, 53.6% of the children older than 7 years reported problems concentrating on homework and showed significantly higher scores in all anxiety facets (p < .001) (Table 2). Younger children are less able to symbolise and express their subconscious states. Clinical manifestations of anxiety include neurovegetative symptoms (psychomotor restlessness, tachycardia, tachypnoea, sweating and increased perspiration) and somatic symptoms (insomnia, somniloquy, hyperactivity‐excitation, abdominal pain, hyperphagia/anorexia, nausea and headache). Long‐term cognitive symptoms, damage to self‐esteem, interpersonal functioning and social adaptation have also been reported (Orchando & Peris, 2017). Our results showed that 88.7% of the children younger than 7 years of age reported at least one symptom indicated in the questionnaire, compared to 56.3% of those experiencing four or more. This, combined with symptoms occurring more frequently than these did during pre‐confinement (tantrums [56.4%], emotional changes [34.1%], restlessness [33.6%], fear of being alone [33.2%]), reflects the impact of the confinement on this age group (Figure 2). However, the aspects assessed in the questionnaire did not influence the number of symptoms that these children reported, except if someone in their family home had been affected or infected by COVID‐19 (p = .027) (Table 3).
Survey research provides high reliability and standardisation in data collection, which is ideal for comparing responses across groups. However, it presents several challenges. Anxiety and symptoms were measured through parental reporting, but it was expected that the questionnaire would be answered by children with their parents’ assistance, except for very young children. Notably, in 19.8% of the cases, at least one parent was a frontline healthcare worker.
The COVID‐19 pandemic continues to create great concern, in addition to the specific psychological effects of quarantine, with children not being strangers to this situation (Reynolds & Richmond, 1997). Although children’s understanding evolves throughout childhood and adolescence, even 2‐year olds have been shown to be aware of changes around them, which potentially manifests in emotional problems (Blaney et al., 2015; Achenbach, 2000). In fact, tantrums, usually occurring when children are unable to adaptively express their emotions or control their frustrations, were the most prevalent symptom among children aged below seven.
Our results indicate that 87.6% and 73.4% of parents with children older than and younger than 7 years old, respectively, regularly conversed with them about the COVID‐19 crisis. However, adults often do not practice what they preach and do not share all their feelings. The absence of emotionally focused conversations may partly explain the anxiety in children who do not know their parents’ emotional state. Sensitive and effective communication about life‐threatening diseases hold important benefits for children and their families’ long‐term psychological well‐being. If this information is restricted, children respond with their own coping mechanisms (Christ & Christ, 2006; Dalton et al., 2019).
Concerning the practical and policy implications of this study, when health professionals and authorities consider the needs of children in exceptional times to detect risk and conduct interventions, the negative repercussions on children and their families can be limited (Palusci, 2013). Governments’ health policies should promote physical activities, a balanced diet and regular sleep patterns. In addition, schools should be advised to maintain regular and close communication with their pupils to identify potential psychological issues while teaching (Mengin et al., 2020; Wang et al., 2020).
5.1. Limitations
This study was conducted during an unprecedented period and was inspired by the repercussions that we observed in our patients through online hospital consultations. Owing to the study design, we could not conduct comparisons with the pre‐confinement situation, and thus do not know what the participants’ baseline anxiety levels were. Furthermore, our questions were aimed at COVID‐19 circumstances and government measures. We did not record the location of the surveyed individuals. Despite this, as the questionnaire was distributed in Madrid and Barcelona using social media, which were two of the worst COVID‐hit cities in Spain, we expected that most surveyed individuals would belong to these regions. Using this method, the responses could have been collected in clusters of schools, neighbourhoods and other typologies. Other information, such as metropolitan or countryside location, town dimension and community resources, was not collected because our survey was designed to allow participants’ anonymity.
Likewise, other factors (previous mental health situation, bullying in school, parents’ educational and financial status, number of relatives living in the home, size of home, presence of open areas such as balconies and smart devices available at home) that may have had conditioning effects or provide additional information were discarded so that the study could focus on the effects of anxiety, making the survey more accessible and easier to complete. We hoped that this would encourage participation. Undoubtedly, some of the above factors could condition prior anxiety. However, we considered that adding a new conditioning factor, such as confinement, would increase baseline anxiety levels. Furthermore, for children younger than 7 years of age, the reported symptoms indicate parents’ opinions about their children’s behaviour and changes observed during confinement. This may have induced information bias.
6. CONCLUSION
Our findings imply that the COVID‐19 pandemic has had a significant impact on children during confinement. It has caused anxiety, behavioural problems and somatic manifestations, which is evident from the high anxiety scores reported among the children. Notably, adults’ own concerns about the implications of COVID‐19 may have affected their ability to recognise and respond to these anxiety signals. It is essential to understand the factors that cause anxiety in children in these exceptional times. Moreover, parents, paediatricians, nurses, psychologists and health authorities should consider the needs of those children, not only to detect individuals at risk but also to develop effective intervention and preventative strategies.
7. RELEVANCE TO CLINICAL PRACTICE
Nursing has had a principal role in this pandemic, both on the front line and at home through monitoring by phone. The monitoring was performed through scheduled examinations as part of the ‘Healthy Child’ programme. These interviews present valuable opportunities to check children’s anxiety levels during home confinement, and depending on the results, initiate multiprofessional intervention, if necessary. School nurses in particular can provide tele‐health services and maintain close contact with students and families to identify needs or vulnerable situations and screening factors that may trigger anxiety responses (Rosário, 2020). In the global community, vulnerable children, in particular, should be watched carefully during confinement to identify risk‐related anxiety situations. Social distancing, limited direct contact and self‐isolation are valid measures for preventing transmission, but these also increase the risk of heightened anxiety levels, especially in children.
CONFLICT OF INTEREST
The authors report no biomedical financial interests or potential conflicts of interest.
AUTHOR CONTRIBUTIONS
JMCR, AJP, SIGA and ALE had full access to all of the data (acquisition, analysis and interpretation) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design, including the surveys, was developed by JMCR, AJP, SIGA and ALE. The statistical analysis was performed by JMCR, PSV and ALE. Administrative, technical or material support was supplied by JMCR and ALE. All authors actively participated in the critical revision and drafting the manuscript. In addition, ALE provided feedback on previous versions of the manuscript, and approved the final version.
ETHICAL APPROVAL STATEMENT
Ethics approval for this study was granted by human research ethics committees at HM Hospitals (approval number 20.04.1603‐GHM).
Supporting information
Supplementary Material
Supplementary Material
Supplementary Material
ACKNOWLEDGEMENTS
We are extremely grateful to all parents and children taking part in the study and especially we thank Isabel S. Ludeña, Charli Suchin and Dr. JM Castellano Vázquez for the careful revision of the manuscript.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request send to Dr. Lopez‐Escobar.
REFERENCES
- Achenbach, T. M. (2000). ASEBA preschool forms & profiles: An integrated system of multi‐informant assessment. ASEBA. [Google Scholar]
- Bailey, R. P. , Howells, K. , & Glibo, I. (2018). Physical activity and mental health of school‐aged children and adolescents: A rapid review. International Journal of Physical Education, 55(1), 2–15. [Google Scholar]
- Blaney, P. H. , Krueger, R. F. , & Millon, T. (2015). Oxford textbook of psychopathology (3rd ed.). Oxford University Press. [Google Scholar]
- Bradbury‐Jones, C. , & Isham, L. (2020). The pandemic paradox: The consequences of COVID‐19 on domestic violence. Journal of Clinical Nursing, 29(13‐14), 2047–2049. 10.1111/jocn.15296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukowski, W. M. , & Adams, R. (2005). Peer relationships and psychopathology: Markers, moderators, mediators, mechanisms, and meanings. Journal of Clinical Child and Adolescent Psychology, 34(1), 3–10. 10.1207/s15374424jccp3401_1 [DOI] [PubMed] [Google Scholar]
- Caballo, V. E. , & Simón, M. Á. (2012). Manual de psicología clínica infantil y del adolescente: Trastornos especificos. Pirámide. [Google Scholar]
- Canals, J. , Voltas, N. , Hernández‐Martínez, C. , Cosi, S. , & Arija, V. (2019). Prevalence of DSM‐5 anxiety disorders, comorbidity, and persistence of symptoms in Spanish early adolescents. European Child & Adolescent Psychiatry, 28(1), 131–143. 10.1007/s00787-018-1207-z. [DOI] [PubMed] [Google Scholar]
- Cao, Q. , Chen, Y.‐C. , Chen, C.‐L. , & Chiu, C.‐H. (2020). SARS‐CoV‐2 infection in children: Transmission dynamics and clinical characteristics. Journal of the Formosan Medical Association, 119(3), 670–673. 10.1016/j.jfma.2020.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson, V. , Hunter, S. , Kuzik, N. , Gray, C. E. , Poitras, V. J. , Chaput, J.‐P. , Saunders, T. J. , Katzmarzyk, P. T. , Okely, A. D. , Connor Gorber, S. , Kho, M. E. , Sampson, M. , Lee, H. , & Tremblay, M. S. (2016). Systematic review of sedentary behaviour and health indicators in school‐aged children and youth: An update. Applied Physiology Nutrition and Metabolism, 41(6), S240–S265. 10.1139/apnm-2015-0630 [DOI] [PubMed] [Google Scholar]
- Centro de Coordinación y Alerta de Emergencias Sanitarias and Ministerio de Sanidad (2021). ‘Actualización no 334. Enfermedad por el coronavirus (COVID‐19). 17.03.2021.’ Retrieved from: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_334_COVID‐19.pdf
- Chen, N. , Zhou, M. , Dong, X. , Qu, J. , Gong, F. , Han, Y. , Qiu, Y. , Wang, J. , Liu, Y. , Wei, Y. , Xia, J. , Yu, T. , Zhang, X. , & Zhang, L. I. (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet, 395(10223), 507–513. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christ, G. H. , & Christ, A. E. (2006). Current approaches to helping children cope with a parent’s terminal illness. CA: A Cancer Journal for Clinicians, 56(4), 197–212. 10.3322/canjclin.56.4.197 [DOI] [PubMed] [Google Scholar]
- Costa, D. , Cunha, M. , Ferreira, C. , Gama, A. , Machado‐Rodrigues, A. M. , Rosado‐Marques, V. , Nogueira, H. , Silva, M.‐R. , & Padez, C. (2020). Self‐reported symptoms of depression, anxiety and stress in Portuguese primary school‐aged children. BMC Psychiatry, 20(1), 87. 10.1186/s12888-020-02498-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello, E. J. , Egger, H. L. , & Angold, A. (2005). The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America, 14(4), 631–648. 10.1016/j.chc.2005.06.003 [DOI] [PubMed] [Google Scholar]
- Creswell, C. , Waite, P. , & Cooper, P. J. (2014). Assessment and management of anxiety disorders in children and adolescents. Archives of Disease in Childhood, 99(7), 674–678. 10.1136/archdischild-2013-303768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton, L. , Rapa, E. , & Stein, A. (2020). Protecting the psychological health of children through effective communication about COVID‐19. The Lancet Child & Adolescent Health, 4(5), 346–347. 10.1016/S2352-4642(20)30097-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton, L. , Rapa, E. , Ziebland, S. , Rochat, T. , Kelly, B. , Hanington, L. , Bland, R. , Yousafzai, A. , Stein, A. , Betancourt, T. , Bluebond‐Langner, M. , D'Souza, C. , Fazel, M. , Fredman‐Stein, K. , Harrop, E. , Hochhauser, D. , Kolucki, B. , Lowney, A. C. , Netsi, E. , & Richter, L. (2019). Communication with children and adolescents about the diagnosis of a life‐threatening condition in their parent. The Lancet, 393(10176), 1164–1176. 10.1016/S0140-6736(18)33202-1 [DOI] [PubMed] [Google Scholar]
- Esbjorn, B. H. , Hoeyer, M. , Dyrborg, J. , Leth, I. , & Kendall, P. (2010). Prevalence and co‐morbidity among anxiety disorders in a national cohort of psychiatrically referred children and adolescents. Journal of Anxiety Disorders, 24(8), 866–872. 10.1016/j.janxdis.2010.06.009 [DOI] [PubMed] [Google Scholar]
- Francisco, R. , Pedro, M. , Delvecchio, E. , Espada, J. P. , Morales, A. , Mazzeschi, C. , & Orgilés, M. (2020). Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID‐19 quarantine in three European countries. Frontiers in Psychiatry, 11, 570164. 10.3389/fpsyt.2020.570164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García‐Salido, A. (2020). Three hypotheses about children COVID19. Pediatric Infectious Disease Journal, 39(7), e157. 10.1097/INF.0000000000002701 [DOI] [PubMed] [Google Scholar]
- Giannakopoulos, G. , Ntre, V. , Moulla, V. , Tzavara, C. , Tomaras, V. , & Kolaitis, G. (2011). Posttraumatic stress, depression and anxiety in children and adolescents following a massive fire disaster: prevalence and related factors. European Child & Adolescent Psychiatry, 20(1), S74–S75. 10.9734/BJMMR/2011/505 [DOI] [Google Scholar]
- Götzinger, F. , Santiago‐García, B. , Noguera‐Julián, A. , Lanaspa, M. , Lancella, L. , Calò Carducci, F. I. , Gabrovska, N. , Velizarova, S. , Prunk, P. , Osterman, V. , Krivec, U. , Lo Vecchio, A. , Shingadia, D. , Soriano‐Arandes, A. , Melendo, S. , Lanari, M. , Pierantoni, L. , Wagner, N. , L'Huillier, A. G. , … Riordan, A. (2020). COVID‐19 in children and adolescents in Europe: A multinational, multicentre cohort study. The Lancet Child & Adolescent Health, 4(9), 653–661. 10.1016/S2352-4642(20)30177-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan, W.‐J. , Ni, Z.‐Y. , Hu, Y. U. , Liang, W.‐H. , Ou, C.‐Q. , He, J.‐X. , Liu, L. , Shan, H. , Lei, C.‐L. , Hui, D. S. C. , Du, B. , Li, L.‐J. , Zeng, G. , Yuen, K.‐Y. , Chen, R.‐C. , Tang, C.‐L. , Wang, T. , Chen, P.‐Y. , Xiang, J. , … Zhong, N.‐S. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine, 382(18), 1708–1720. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum, S. B. , Lachal, J. , Radjack, R. , Carretier, E. , Minassian, S. , Benoit, L. , & Moro, M. R. (2020). Adolescent psychiatric disorders during the COVID‐19 pandemic and lockdown. Psychiatry Research, 291, 113264. 10.1016/j.psychres.2020.113264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gussinyé Canabal, S. (2005). Aplicación del programa de tratamiento integral para la obesidad infantil" Niñ@ s en movimiento". Universitat Autònoma de Barcelona, Tesis Doctoral.
- Kolaitis, G. , Kostopoulos, J. , Tsiantis, J. , Harataki, S. , Rigizou, F. , Zacharaki, L. , Riga, E. , Augoustatou, A. , Bimbou, A. , Kanari, N. , Liakopoulou, M. , & Katerelos, P. (2003). Posttraumatic stress reactions among children following the Athens earthquake of September 1999. European Child & Adolescent Psychiatry, 12(6), 273–280. 10.1007/s00787-003-0339-x [DOI] [PubMed] [Google Scholar]
- Laursen, B. , Bukowski, W. M. , Aunola, K. , & Nurmi, J.‐E. (2007). Friendship moderates prospective associations between social isolation and adjustment problems in young children. Child Development, 78(4), 1395–1404. 10.1111/j.1467-8624.2007.01072.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, K. , Fang, Y.‐Y. , Deng, Y. , Liu, W. , Wang, M.‐F. , Ma, J.‐P. , & Liu, H.‐G. (2020). Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chinese Medical Journal, 133(9), 1025–1031. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades, M. E. , Chatburn, E. , Higson‐Sweeney, N. , Reynolds, S. , Shafran, R. , Brigden, A. , Linney, C. , McManus, M. N. , Borwick, C. , & Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. Journal of the American Academy of Child and Adolescent Psychiatry, 59(11), 1218. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mengin, A. , Alle, M. C. , Rolling, J. , Ligier, F. , Schroder, C. , Lalanne, L. , Berna, F. , & Giersch, A. (2020). Psychopathological consequences of confinement. Encephale‐Revue De Psychiatrie Clinique Biologique Et Therapeutique, 46(3), S43–S52. 10.1016/j.encep.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammadi, M. R. , Ahmadi, N. , Yazdi, F. R. , Khaleghi, A. , Mostafavi, S.‐A. , Hooshyari, Z. , Molavi, P. , Sarraf, N. , Hojjat, S. K. , Mohammadzadeh, S. , Amiri, S. , Arman, S. , Ghanizadeh, A. , Ahmadipour, A. , Ostovar, R. , Nazari, H. , Hosseini, S. H. , Golbon, A. , Derakhshanpour, F. , … Mehrparvar, A. H. (2020). Prevalence, comorbidity and predictors of anxiety disorders among children and adolescents. Asian Journal of Psychiatry, 53, 102059. [DOI] [PubMed] [Google Scholar]
- Murray, L. , Creswell, C. , & Cooper, P. J. (2009). The development of anxiety disorders in childhood: An integrative review. Psychological Medicine, 39(9), 1413–1423. 10.1017/S0033291709005157 [DOI] [PubMed] [Google Scholar]
- Orchando, G. , & Peris, S. P. (2017). Actualizacion de la ansiedad en la edad pediatrica. Pediatria Integral, XX(1), 39–46. [Google Scholar]
- Palusci, V. J. (2013). Adverse childhood experiences and lifelong health. JAMA Pediatrics, 167(1), 95–96. 10.1001/jamapediatrics.2013.427 [DOI] [PubMed] [Google Scholar]
- Reynolds, C. R. , & Richmond, B. O. (Eds.) (1997). Ed. El Manual Moderno. Escala de ansiedad manifiesta en niños (CMAS‐R). Mexico, DF.
- Rosário, R. (2020). COVID‐19 and schools closure: Implications for school nurses. The Journal of School Nursing, 36(4), 241–242. 10.1177/1059840520925533 [DOI] [PubMed] [Google Scholar]
- Ruiz Sancho, A. M. , & Lago Pita, B. (2005). ‘Transtornos de ansiedad en la infancia y en la adolescencia’, Curso de Actualización en Pediatria. Edited by Exlibris Ediciones, pp. 265–280.
- Sprang, G. , & Silman, M. (2013). Posttraumatic stress disorder in parents and youth after health‐related disasters. Disaster Medicine and Public Health Preparedness, 7(1), 105–110. 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- University of Oxford (2020). Coronavirus Government Response Tracker. Retrieved from https://www.bsg.ox.ac.uk/research/research‐projects/coronavirus‐government‐response‐tracker.
- Van Dijk, M. L. , Savelberg, H. H. C. M. , Verboon, P. , Kirschner, P. A. , & De Groot, R. H. M. (2016). Decline in physical activity during adolescence is not associated with changes in mental health. BMC Public Health, 16(1), 1–9. 10.1186/s12889-016-2983-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, G. , Zhang, Y. , Zhao, J. , Zhang, J. , & Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID‐19 outbreak. The Lancet, 395(10228), 945–947. 10.1016/S0140-6736(20)30547-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood, J. J. , McLeod, B. D. , Sigman, M. , Hwang, W. C. , & Chu, B. C. (2003). Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry, 44(1), 134–151. 10.1111/1469-7610.00106 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020a). Coronavirus disease 2019 (COVID‐19): Situation Report‐54. Retrieved from https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200314‐sitrep‐54‐covid‐19.pdf?sfvrsn=dcd46351_8. [Google Scholar]
- World Health Organization (2020b). Coronavirus disease 2019 (COVID‐19): Situation Report‐50. Retrieved from https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200310‐sitrep‐50‐covid‐19.pdf?sfvrsn=55e904fb_2. [Google Scholar]
- World Health Organization (2021). COVID‐19 Weekly Epidemiological Update – 16 March 2021. Retrieved from https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20210316_weekly_epi_update_31.pdf?sfvrsn=c94717c2_17&download=true. [Google Scholar]
- Xie, X. , Xue, Q. , Zhou, Y. , Zhu, K. , Liu, Q. , Zhang, J. , & Song, R. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics, 174(9), 898–900. 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, S.‐J. , Zhang, L.‐G. , Wang, L.‐L. , Guo, Z.‐C. , Wang, J.‐Q. , Chen, J.‐C. , Liu, M. , Chen, X. I. , & Chen, J.‐X. (2020). Prevalence and socio‐demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID‐19. European Child & Adolescent Psychiatry, 29(6), 749–758. 10.1007/s00787-020-01541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request send to Dr. Lopez‐Escobar.


