Abstract
Objectives
The coronavirus disease 2019 (COVID‐19) pandemic has severely affected nursing home residents. Given the continued high incidence of COVID‐19, and the likelihood that new variants and other infectious agents may cause future outbreaks, we sought to understand the relationship of nursing home quality ratings and measures of COVID‐19 outbreak severity and persistence.
Design
We analyzed nursing home facility‐level data on COVID‐19 cases and deaths, county‐level COVID‐19 rates, and nursing home data from the Centers for Medicare & Medicaid Services (CMS), including ratings from the CMS Nursing Home Five‐Star Quality Rating System. We used regression analysis to examine the association between star ratings and cumulative COVID‐19 incidence and mortality as well as persistent high resident incidence.
Setting
All nursing homes in the CMS COVID‐19 Nursing Home Dataset reporting data that passed quality assurance checks for at least 20 weeks and that were included in the January 2021 Nursing Home Care Compare update.
Participants
Residents of the included nursing homes.
Measurements
Cumulative resident COVID‐19 incidence and mortality through January 10, 2021; number of weeks with weekly resident incidence of COVID‐19 in the top decile nationally.
Results
As of January 10, 2021, nearly all nursing homes (93.6%) had reported at least one case of COVID‐19 among their residents, more than three‐quarters (76.9%) had reported at least one resident death, and most (83.5%) had experienced at least 1 week in the top decile of weekly incidence. In analyses adjusted for facility and county‐level characteristics, we found generally consistent relationships between higher nursing home quality ratings and lower COVID‐19 incidence and mortality, as well as with fewer high‐incidence weeks.
Conclusion
Nursing home quality ratings are associated with COVID‐19 incidence, mortality, and persistence. Nursing homes receiving five‐star ratings, for overall quality as well as for each domain, had lower COVID‐19 rates among their residents.
Keywords: COVID‐19, long‐term care, nursing homes, quality of care
Key Points
As of January 10, 2021, nearly all nursing homes (93.6%) had reported at least one case of COVID‐19 among their residents, more than three‐quarters (76.9%) had reported at least one resident death, and the majority (83.5%) had experienced at least 1 week in the top decile of weekly incidence.
Higher nursing home quality ratings are associated with lower COVID‐19 incidence and mortality, as well as with fewer high‐incidence weeks, after controlling for local community COVID‐19 spread and relevant facility‐level factors.
Why Does this Paper Matter?
The COVID‐19 pandemic has severely affected nursing home residents. This article demonstrates a consistent relationship between higher quality ratings and lower COVID‐19 incidence, mortality, and the number of high‐incidence weeks. These findings indicate that the data and methodology used in the star ratings capture important aspects of quality related to infection control. Policymakers can use star ratings, along with information on county infection rates and nursing home payor mix, to identify nursing homes more at risk of COVID‐19 or potentially other infectious outbreaks. Nursing homes can also use these indicators to identify areas to target improvement to reduce the risk of future infectious outbreaks.
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has profoundly affected the nursing home population. Nursing home residents are often frail, older individuals who cannot live independently due to their health status, functional limitations, cognitive and physical impairments, and other age‐related disabilities. 1 COVID‐19 has highlighted the vulnerability of nursing home residents, who have disproportionately suffered effects of the pandemic. They are at higher risk of severe disease and mortality from COVID‐19 due to their age 2 and comorbidities. 3 In addition, nursing homes' communal living environment increases the risk of the spread of COVID‐19, particularly for nursing homes that lack adequate infection prevention and control measures to prevent transmission. 4
As of February 18, 2021, nearly 625,000 confirmed COVID‐19 cases were reported among U.S. nursing home residents, representing about 23% of the total COVID‐19 cases in the United States. During this period, nursing home residents accounted for 26% of reported COVID‐19 related deaths. 5 , 6 More than 90% of nursing homes have had at least one confirmed COVID‐19 case among residents, and about 77% of nursing homes reported at least one COVID‐19 death among residents. In addition, COVID‐19 infection and death rates vary considerably across nursing homes.
Given the continued high incidence of COVID‐19, and the possibility of new variants or other infectious diseases that may cause future outbreaks, an understanding of the relationship between nursing home characteristics, in particular those that nursing homes can control, and COVID‐19 incidence is critical. Several studies have examined the relationship of COVID‐19 infections and/or mortality with nursing home quality 7 , 8 , 9 , 10 , 11 , 12 and nurse staffing levels. 12 , 13 , 14 However, the findings of these studies have been mixed partly because they either did not use national data and/or were conducted early in the pandemic, limiting their generalizability across states and across time periods with different COVID‐19 infection rates. Furthermore, much of the existing literature has focused on COVID‐19 incidence or mortality as the main outcomes of interest. Comparatively, little attention has been given to nursing homes with persistent COVID‐19 burden. The lack of consistent understanding of factors related to COVID‐19 outbreaks hampers the development of responses to mitigate COVID‐19 effects.
In this study, we used national and publicly reported data from the Centers for Medicare & Medicaid Services (CMS) to examine the association between nursing home quality of care and COVID‐19 incidence, mortality, and persistent burden. Understanding the extent to which nursing homes can mitigate outbreaks through better performance on health inspection surveys, improved quality of care, and higher nurse staffing can help target resources, which may help to mitigate the impacts of future outbreaks.
METHODS
Study sample and data sources
For this study, we obtained COVID‐19 data for nursing homes from the COVID‐19 Nursing Home Dataset, 5 which is derived from the Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network system. This dataset contains weekly resident and staff COVID‐19 case and death counts as well as total weekly resident counts for all federally certified nursing homes in the United States. Nursing homes began reporting weekly COVID‐19 data the week ending May 31, 2020, and we included data reported through January 10, 2021, in our analyses.
We used data on nursing home quality of care star ratings and other facility characteristics from Care Compare for Nursing Homes and the Certification and Survey Provider Enhanced Reports (CASPER), which are derived from the data publicly reported in January 2021. These analyses included nursing homes that reported COVID‐19 data that passed the CDC and CMS Quality Assurance Checks 15 for at least 20 of the 28 total weeks covered in this study and that were included in the January 2021 Care Compare update (N = 14,693).
We obtained measures of community burden of COVID‐19 from USAFacts.org. 16 These data are collected from state and local public health agencies and the CDC and provide daily county‐level data on confirmed COVID‐19 cases and deaths. For this study, we aggregated daily county‐level COVID‐19 cases through January 3, 2021, and expressed the rates as cumulative incidence per 1000 population. We used the area deprivation index (ADI) as a measure of socioeconomic status for nursing home locations. 17 , 18 , 19 , 20 Census‐block ADI rankings were weighted by population size and aggregated to the county‐level; higher scores indicate greater socioeconomic disadvantage.
Five‐star rating methodology
The rating system features an overall quality rating of one to five stars based on nursing home performance on three domains, each with its own rating of one to five stars: health inspections, nurse staffing, and resident quality measures (QMs). For each rating, more stars indicate higher quality, and each incorporates aspects of risk‐adjustment, to account for factors captured by the ratings that are not within the nursing home's control, such as resident case‐mix. We briefly describe each domain below. 21
The health inspection star rating is based on the scope and severity of regulatory deficiencies identified on the three most recent annual state health inspections as well as inspections arising from complaints and, during the pandemic, focused infection control surveys. The most recent survey findings are weighted more heavily than those from prior surveys. The focused infection control surveys are surveys CMS developed early in the pandemic to allow surveyors to quickly inspect nursing homes explicitly for compliance with federal expectations for preventing the transmission of COVID‐19, 22 , 23 and the results of these surveys were first incorporated into the health inspection ratings in January 2021. To account for variation among states in survey results, health inspection ratings are based on the relative performance of facilities within a state. 21
The staffing rating is based on two, quarterly, case‐mix adjusted staffing measures: (1) total nursing hours per resident per day, including registered nurses (RN), licensed practical/vocational nurses, and certified nurse aides 21 , 24 ; and (2) RN hours per resident per day. Staffing levels are based on Payroll Based Journal data that nursing homes report on a quarterly basis. 24 The case‐mix adjustment for staffing levels is based on resident daily census derived from the Minimum Data Set (MDS) and each nursing home's daily distribution of residents in each of 66 Resource Utilization Groups (RUG‐IV), with the data for grouping derived from resident MDS assessments.
The QM rating is based on a set of 16 measures derived from the MDS and Medicare claims data. The measures address a broad range of function and health status indicators. All the claims‐based measures and most of the MDS‐based measures are risk‐adjusted for a variety of factors such as residents' demographic characteristics and case‐mix variation. 25
The overall quality star rating is calculated by starting with the health inspection rating. Nursing homes receive an additional star on their overall rating for a 5‐star QM rating and/or a 4‐star or 5‐star staffing rating. Nursing homes lose a star on their overall rating for a 1‐star rating on QMs and/or staffing. These adjustments are made with the stipulation that the overall quality star rating must remain between 1 and 5 stars. The star ratings for special focus facilities are suppressed, and nursing homes cited for abuse and neglect (indicated with an icon on Care Compare) have their health inspection domain rating capped at 2 stars. In this study, we examined the association between COVID‐19 rates and overall quality rating as well as three domain‐specific ratings. 21
Outcomes
We examined three outcomes for nursing homes: (1) cumulative confirmed resident COVID‐19 incidence; (2) cumulative resident COVID‐19 mortality; and (3) number of weeks in the top decile of the national distribution of weekly confirmed resident COVID‐19 incidence (weekly confirmed cases/1000 residents). Although nursing homes were not required to submit COVID‐19 data to the CDC until May 2020, many nursing homes included retrospective confirmed cases and deaths since January 1, 2020, and additional data continued to be added weekly. We used these cumulative data to examine the first two outcomes, cumulative incidence, and mortality. In addition, we chose to examine the additional measure of high‐incidence weeks to capture nursing homes that may have had repeated or sustained outbreaks, which may have different characteristics compared with nursing homes with high COVID‐19 rates initially but that have since avoided additional outbreaks. Since many nursing homes included retrospective data in their first report for the week ending May 24, this first week of reporting includes COVID‐19 cases for multiple weeks. Therefore, we excluded data from this week in the analysis of nursing homes with high‐incidence weeks to focus exclusively on new cases within a single week.
Statistical analysis
We first assessed the distribution of each outcome to determine the most appropriate analytic approaches. We next examined unadjusted associations between nursing home star ratings and each of the three outcomes. To model each outcome, we used a zero‐inflated negative binomial regression approach. This type of model is appropriate for count outcomes with a variance substantially larger than the mean and a larger number of zeros than a simple negative binomial distribution. To account for variations in the number of residents and time at risk across nursing homes, the models for cumulative incidence and cumulative mortality included an offset term, defined as the log of resident‐weeks, with resident‐weeks calculated as the average resident census times the number of weeks of valid data the nursing home provided.
For each of the three outcomes, we estimated regression models to examine the association between the outcome and the overall quality rating and ratings in each domain (health inspections, nurse staffing, and QMs). Each model adjusted for facility size based on the number of certified beds, urban or rural location, percent of facility residents with Medicaid as primary payer, community incidence of COVID‐19, and the county ADI. We estimated community incidence for each county as the number of cases per 1000 population, including cases reported from May 24, 2020, to January 3, 2021. Because the star ratings included in the models are already risk‐adjusted at the facility level, 21 we did not further risk adjust our models beyond the covariates previously mentioned. For zero‐inflated models, one also specifies covariates in the “zero” portion of the model, which is a logit model with the outcome being the log‐odds of having zero cases, deaths, or high incidence weeks for a nursing home. For this portion of the model, we included factors that we hypothesized to be associated with the initial susceptibility of a nursing home to the introduction of COVID‐19. Specifically, we included number of certified beds, cumulative county COVID incidence, urban location, and county ADI. We conducted all analyses at the nursing home level, and the measure of association is the incidence rate ratio. For the number of high‐incidence weeks, this can be interpreted as the percent increase in number of high‐incidence weeks associated with each one‐unit increase in the independent variable (or compared with the reference group).
RESULTS
As of January 10, 2021, almost all nursing homes (93.6%) had reported at least one confirmed case of COVID‐19 among their residents (Table 1); among those reporting at least one case, the average cumulative incidence was 588.5 cases per 1000 current residents (interquartile range = 235.1–883.2). This cumulative incidence represents the total number of confirmed resident COVID‐19 cases reported through January 10, 2021, relative to the nursing home population on January 10, 2021. More than three‐quarters (76.9%) of the nursing homes included in this study reported at least one COVID‐19 death, with a mean mortality rate of 141.6 deaths per 1000 current residents (IQR: 49.2–189.2). Most nursing homes (83.5%) had experienced at least 1 week in the top decile of weekly incidence, with a mean of 3.3 (SD = 2.6) weeks during the span of 28 weeks. Table 2 provides the distribution of star ratings in each domain.
TABLE 1.
Description of facility sample (N = 14,693)
| Mean | SD, IQR, or % | |
|---|---|---|
| Nursing home and community characteristics | ||
| Facility % Medicaid residents, mean (SD) | 59.6 | (24.1) |
| Facility number of certified beds, mean (SD) | 107.0 | (60.7) |
| Urban facility, N (%) | 10,589 | (72.1%) |
| COVID‐19 cases per 1000 county population, a mean (IQR) | 60.7 | (44.4–74.4) |
| County area deprivation index (1–100), mean (SD) | 54.2 | (20.5) |
| COVID‐19 among residents | ||
| Incidence of confirmed COVID‐19 among residents (cumulative, through 1/10/2021) | ||
| Any confirmed COVID‐19 among residents, N (%) | 13,692 | (93.6%) |
| COVID‐19 cases per 1000 residents (all), b mean (IQR) | 550.6 | (172.4–860.5) |
| COVID‐19 cases per 1000 residents (conditional), c mean (IQR) | 588.5 | (235.1–883.2) |
| COVID‐19 deaths among residents (cumulative, through January 10, 2021) | ||
| Any COVID‐19 deaths among residents, N (%) | 11,247 | (76.9%) |
| COVID‐19 deaths per 1000 residents (all), b mean (IQR) | 108.9 | (11.4–160.0) |
| COVID‐19 deaths per 1000 residents (conditional), c mean (IQR) | 141.6 | (49.2–189.2) |
| Weeks in top decile of resident COVID‐19 incidence | ||
| Any weeks in top decile, N (%) | 12,268 | (83.5%) |
| Number of weeks in top decile, mean (SD) | 3.3 | (2.6) |
Abbreviations: IQR, interquartile range; N, number; SD, standard deviation.
Cumulative, 5/24/20–1/3/2021.
Includes all participating nursing homes, including those with 0 cases/deaths.
Includes only those nursing homes with one or more cases/deaths.
TABLE 2.
Distribution of nursing home star ratings a
| Rating domain | ★ | ★★ | ★★★ | ★★★★ | ★★★★★ |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Overall quality | 2050 (14.1) | 2740 (18.9) | 2637 (18.2) | 3196 (22.1) | 3868 (26.7) |
| Health inspections | 2794 (19.3) | 3508 (24.2) | 3318 (22.9) | 3378 (23.3) | 1493 (10.3) |
| Nurse staffing | 852 (6.4) | 2920 (21.9) | 3737 (28.0) | 3403 (25.5) | 2417 (18.1) |
| Resident quality measures | 781 (5.4) | 1738 (12.0) | 2906 (20.1) | 3766 (26.0) | 5286 (36.5) |
Ratings are those publicly reported in January 2021 on Care Compare. Excludes nursing homes that are not rated, including special focus facilities (N = 83); those too new to rate (N = 119); or those that have insufficient data to calculate a rating (N = 1162 for staffing, 14 for resident quality measures).
In unadjusted analyses, resident COVID‐19 average cumulative incidence and mortality rates, as well as the number of high‐incidence weeks, were lowest among nursing homes receiving five‐star ratings in each domain (Figure 1). For example, on average, nursing homes with a one‐star overall quality rating experienced about 3.6 weeks in the top decile of confirmed cases, compared with 2.8 weeks for five‐star nursing homes.
FIGURE 1.
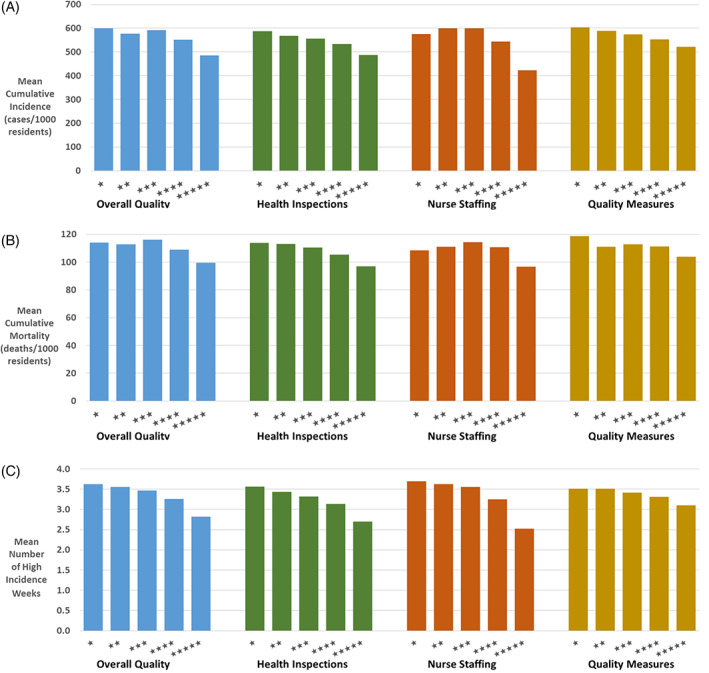
Unadjusted association of nursing home star ratings with (A) mean cumulative confirmed resident cases per 1000 residents, (B) mean cumulative resident COVID‐19 deaths per 1000 residents, and (C) mean number of weeks in the top decile of weekly resident incidence
In adjusted analyses accounting for facility size, urbanity, percent Medicaid residents, ADI, and the county COVID‐19 rate, the relationships between higher star ratings and lower rates of COVID‐19 were modest in magnitude but generally consistent and statistically significant (Table 3). For the overall star rating, nursing homes rated at less than 5 stars had greater COVID‐19 incidence, mortality, and high‐incidence weeks. For example, nursing homes with a 1‐ to 3‐star overall rating had about 10% more weeks with high COVID‐19 incidence (all p < 0.001) than 5‐star homes, and nursing homes with an overall star rating of 1 to 3 stars also had about 13%–16% higher incidence (p < 0.0001) and 8%–10% higher cumulative COVID‐19 mortality than 5‐star nursing homes (p = <0.01). With respect to staffing, facilities with 1 to 3 stars for nurse staffing had 18%–22% more weeks with high COVID‐19 incidence (all p < 0.0001) than 5‐star staffed nursing homes. Though the confidence intervals overlap across the 1‐ to 4‐star categories, the number of high incidence weeks declines with each additional star received on the health inspection rating, and all are significantly higher than for 5‐star nursing homes (all p < 0.001). For the QM rating, 1‐ to 3‐star homes had 5%–7% higher cumulative incidence (all p < 0.05). Higher County COVID‐19 incidence was also strongly and consistently associated with higher nursing home COVID‐19 incidence and mortality, as well as number of high‐incidence weeks. County ADI was strongly and consistently associated with cumulative COVID‐19 incidence and number of high‐incidence weeks but not with mortality (Table S1).
TABLE 3.
Multivariable regression of nursing home resident COVID‐19 on facility star ratings
| Rating domain | Cumulative resident incidence | Cumulative resident mortality | Number of weeks with high resident incidence | |||
|---|---|---|---|---|---|---|
| IRR a | (95% CI) | IRR a | (95% CI) | IRR a | (95% CI) | |
| Overall quality | ||||||
| ★ | 1.16 | (1.11–1.21)**** | 1.10 | (1.03–1.17)** | 1.08 | (1.04–1.13)*** |
| ★★ | 1.13 | (1.08–1.18)**** | 1.08 | (1.02–1.14)** | 1.10 | (1.06–1.15)**** |
| ★★★ | 1.15 | (1.11–1.20)**** | 1.10 | (1.04–1.17)*** | 1.09 | (1.05–1.14)**** |
| ★★★★ | 1.08 | (1.04–1.12)**** | 1.04 | (0.99–1.10) | 1.06 | (1.02–1.09)** |
| ★★★★★ | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Health inspections | ||||||
| ★ | 1.13 | (1.07–1.19)**** | 1.08 | (1.00–1.17)* | 1.13 | (1.07–1.18)**** |
| ★★ | 1.09 | (1.04–1.15)*** | 1.08 | (1.01–1.16)* | 1.12 | (1.06–1.17)**** |
| ★★★ | 1.08 | (1.02–1.13)** | 1.06 | (0.98–1.14) | 1.11 | (1.06–1.17)**** |
| ★★★★ | 1.03 | (0.97–1.08) | 1.01 | (0.94–1.09) | 1.07 | (1.02–1.12)*** |
| ★★★★★ | 1.00 | Reference | 1.000 | Reference | 1.00 | Reference |
| Nurse staffing | ||||||
| ★ | 1.23 | (1.15–1.31)**** | 1.03 | (0.94–1.13) | 1.18 | (1.11–1.26)**** |
| ★★ | 1.30 | (1.24–1.37)**** | 1.06 | (0.99–1.13) | 1.21 | (1.15–1.26)**** |
| ★★★ | 1.30 | (1.24–1.36)**** | 1.07 | (1.01–1.14)* | 1.22 | (1.17–1.28)**** |
| ★★★★ | 1.21 | (1.15–1.26)**** | 1.06 | (1.00–1.00)* | 1.17 | (1.12–1.22)**** |
| ★★★★★ | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Quality measures | ||||||
| ★ | 1.07 | (1.00–1.14)* | 1.10 | (1.01–1.19)* | 1.01 | (0.95–1.01) |
| ★★ | 1.07 | (1.02–1.12)** | 1.04 | (0.98–1.11) | 1.04 | (1.00–1.09) |
| ★★★ | 1.05 | (1.01–1.08)* | 1.05 | (1.00–1.10) | 1.02 | (0.98–1.06) |
| ★★★★ | 1.05 | (1.01–1.08)* | 1.06 | (1.02–1.11)** | 1.01 | (0.98–1.05) |
| ★★★★★ | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
Abbreviations: CI, confidence interval; IRR, incidence rate ratio.
IRR modeled using zero‐inflated negative binomial regression. Each rating domain is modeled separately. Estimates adjusted for the following covariates: county cumulative COVID‐19 case count per 1000 population, % Medicaid residents, number of certified beds, urban versus rural, and county area deprivation index. The zero portion of the model is a logit model predicting the likelihood of having zero cases or deaths or high incidence weeks and includes the following covariates: county cumulative COVID‐19 case count per 1000 population, number of certified beds, urban versus rural, and county area deprivation index.
p < 0.05;
p < 0.01;
p < 0.001;
p < 0.0001.
DISCUSSION
In this study using national data on nursing home quality of care and COVID‐19 incidence, mortality, and persistent burden, we found a consistent relationship between higher quality ratings for all domains of the Five‐Star Quality Rating System and lower COVID‐19 incidence, mortality, and the number of high‐incidence weeks. The findings suggest that nursing homes can adopt practices associated with improved quality that are empirically associated with a lower COVID incidence. For example, nursing homes that ensure better compliance with federal regulations, or facilities that have higher staffing ratios, have a lower COVID incidence. The findings underscore the importance of health inspection surveys and suggest a modest relationship between higher overall ratings and lower rates of COVID‐19 cases and deaths. Our results are consistent with previous research showing that community incidence is a strong predictor of COVID‐19 outcomes in nursing homes.
This study has several limitations. First, our use of cumulative incidence and mortality may obscure temporal patterns in the relationships between nursing home quality star ratings and COVID‐19 outcomes in nursing homes. Nonetheless, the consistency of the findings for these cumulative outcomes with those for persistent burden indicates the durability of these relationships. Second, our measures of nursing home COVID‐19 outcomes depend on the reporting by individual nursing homes to the CDC and may represent an undercount, particularly due to variability in the availability of testing. Additionally, our use of cumulative incidence and mortality does not account for the dynamic shifts in the number of nursing home residents over time. While it depicts the cumulative number of confirmed COVID‐19 nursing home cases/deaths through January 10, 2021, it is compared with a static, noncumulative count of current nursing home residents rather than all residents residing in the nursing home during this period. Finally, there may remain unmeasured confounding factors for the relationship between nursing home star ratings and COVID‐19 incidence and mortality, and low star ratings may simply be a marker of other measures of inferior quality. However, we deliberately chose to control primarily for factors outside of nursing home control, such as county‐level COVID‐19 rates, urban location, and the case‐mix adjustments incorporated in the star rating algorithms.
Nevertheless, our findings suggest that policymakers can use star ratings, along with information on county infection rates and nursing home size and payor mix, to identify nursing homes more at risk of COVID‐19 or potentially other infectious outbreaks. Nursing homes with lower star ratings or residing in counties with higher infection rates may benefit from additional resources, such as technical assistance on infection control practices. We note that the practices that reduce the spread of COVID‐19 (e.g., effective hand hygiene, screening for symptoms of infection, appropriate use of personal protective equipment [PPE]) are also effective at preventing the transmission of other viruses and are requirements for compliance with federal infection control standards; further, assuring compliance with these standards is central to the focused infection control surveys, included in health inspection ratings as of January 2021. Therefore, facilities with lower star ratings may also be more susceptible to outbreaks of other communicable diseases than facilities with higher star ratings.
In addition, policies that promote improved compliance, higher staffing, or incentivize better performance on QMs may be effective in reducing the spread of COVID‐19. Our findings demonstrate that the Five Star Quality Rating System may be effective at identifying different levels of quality among nursing homes related to COVID‐19 outcomes. This supports the intent of the rating system in general, which is to provide useful information about each nursing home's quality, in a consumer‐friendly manner (e.g., the 5‐star rating). Future research can explore the relationship between nursing home quality ratings and other outcomes related to COVID‐19, such as vaccination rates for residents and staff.
Editor's Note.
This is a very important article for at least two reasons. First, it clearly demonstrates a relationship between the quality of nursing home (NH) care and the incidence of and mortality from COVID‐19. Second, it provides additional data to support, at least in part, the validity of the NH Five‐Star quality rating system. Several studies in JAGS and other journals with a much smaller sample of NHs have examined the relationship between NH quality and COVID‐19. While they have found variable associations with NH Five‐Star quality ratings, two things were clear from these studies. First, the incidence of COVID‐19 in NHs is related to the prevalence of the virus in the surrounding community. Second, nursing staffing is critical in preventing the spread of the virus throughout a NH. The current study, using data from almost all of the over 15,000 NHs in the United States documents a consistent and statistically significant association between Five‐Star quality ratings and cumulative incidence of and mortality from COVID‐19.
The Five‐Star rating system is controversial. On the one hand, NHs and many policy makers believe it lacks validity and needs to be substantially revised or replaced with measures that are not only more valid, but more person‐centered. Alternatively, CMS works with a contractor and a technical expert panel to carefully develop and validate the quality measures, at least from a statistical perspective. While it is true that an individual NH's Five‐Star rating may not accurately reflect that facility's quality of care, culture, clinical outcomes, and resident/family satisfaction with care, it is extremely challenging to develop valid measures of all these outcomes, and to mitigate the effects of “gaming the system” through documentation practices. Changing the way that post‐acute and long‐term care is provided and funded in United States and further developing valid, person‐centered quality measures are among the most important tasks for the field of Geriatrics. We need strong interprofessional participation and support from the NH industry and federal and state governments to do so.
—Joseph G. Ouslander, MD
CONFLICT OF INTEREST
The authors have no conflicts. Four of the co‐authors (Christianna S. Williams, Qing Zheng, Alan J. White, and Ariana I. Bengtsson) work for Abt Associates, which has helped CMS to develop and maintain the Five‐Star Quality Rating System since 2008. Three of the co‐authors (Evan T. Shulman, Kurt R. Herzer, and Lee A Fleisher) work for the Centers for Medicare & Medicaid Services, which developed and maintains the Five‐Star Quality Rating System.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to the study concept and design and/or analysis and interpretation of data. All authors participated in drafting the article and/or revising it critically for important intellectual content and gave final approval of the version to be submitted.
SPONSOR'S ROLE
Three of the co‐authors (Evan T. Shulman, Kurt R. Herzer, and Lee A. Fleisher) work for the Centers for Medicare & Medicaid Services.
FINANCIAL DISCLOSURE
This research was supported by the Centers for Medicare & Medicaid Services under contract GS‐00F‐252CA, Task Order No. 75FCMC18F0064. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Medicare & Medicaid Services.
Supporting information
Table S1 Full regression models of nursing home resident COVID‐19 on facility star ratings.
ACKNOWLEDGMENT
Funding was provided by the Centers for Medicare & Medicaid Services under Contract No. GS‐00F‐252CA, Task Order No. 75FCMC18F0064.
Williams CS, Zheng Q, White AJ, et al. The association of nursing home quality ratings and spread of COVID‐19. J Am Geriatr Soc. 2021;69(8):2070–2078. 10.1111/jgs.17309
Funding information Centers for Medicare & Medicaid Services, Grant/Award Number: GS‐00F‐252CA
Contributor Information
Christianna S. Williams, Email: christianna_williams@abtassoc.com.
Alan J. White, Email: alan_white@abtassoc.com.
REFERENCES
- 1. Panagiotou OA, Kosar CM, White EM, et al. Risk factors associated with all‐cause 30‐day mortality in nursing home residents with COVID‐19. JAMA Intern Med. 2021;181:439–448. 10.1001/jamainternmed.2020.7968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adams ML, Katz DL, Grandpre J. Population‐based estimates of chronic conditions affecting risk for complications from coronavirus disease, United States. Emerg Infect Dis. 2020;26(8):1831‐1833. 10.3201/eid2608.200679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mayo Clinic . COVID‐19: who's at higher risk of serious symptoms? 2021. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-who-is-at-risk/art-20483301. Accessed February 18, 2021.
- 4. Centers for Disease Control and Prevention . Preparing for COVID‐19 in Nursing Homes, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html. Accessed February 18, 2021.
- 5. Centers for Medicare & Medicaid Services . COVID‐19 Nursing Home Data, 2021. https://data.cms.gov/stories/s/bkwz-xpvg. Accessed February 18, 2021.
- 6. Centers for Disease Control and Prevention . COVID Data Tracker, 2021. https://covid.cdc.gov/covid-data-tracker/#cases_totalcases. Accessed February 18, 2021.
- 7. Bui DP, See I, Hesse EM, et al. Association between CMS quality ratings and COVID‐19 outbreaks in nursing homes—West Virginia, March 17–June 11, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1300‐1304. 10.15585/mmwr.mm6937a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Abrams HR, Loomer L, Gandhi A, Grabowski D. Characteristics of U.S. nursing homes with COVID‐19 cases. J Am Geriatr Soc. 2020;68(8):1653‐1656. 10.1111/jgs.16661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Figueroa JF, Wadhera RK, Papincolas I, et al. Association of nursing home ratings on health inspections, quality of care, and nurse staffing with COVID‐19 cases. JAMA. 2020;324(11):1103‐1105. 10.1001/jama.2020.14709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. He M, Li Y, Fang F. Is there a link between nursing home reported quality and COVID‐19 cases? Evidence from California skilled nursing facilities. J Am Med Dir Assoc. 2020;21(7):905‐908. 10.1016/j.jamda.2020.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bowblis J, Applebaum R. Prevalence of COVID‐19 in Ohio nursing homes: what's quality got to do with it? J Aging Soc Policy. 2020;11:1‐17. 10.1080/08959420.2020.1824542 [DOI] [PubMed] [Google Scholar]
- 12. Li Y, Temkin‐Greener H, Shan G, Cai X. COVID‐19 infections and deaths among Connecticut nursing home residents: facility correlates. J Am Geriatr Soc. 2020;68(9):1899‐1906. 10.1111/jgs.16689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gorges RJ, Konetzka RT. Staffing levels and COVID‐19 cases and outbreaks in US nursing homes. J Am Geriatr Soc. 2020;68(11):2462‐2466. 10.1111/jgs.16787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harrington C, Ross L, Chapman S, et al. Nurse staffing and coronavirus infections in California nursing homes. Policy Polit Nurs Pract. 2020;21(3):174‐186. 10.1177/1527154420938707 [DOI] [PubMed] [Google Scholar]
- 15. Centers for Medicare & Medicaid Services . COVID‐19 Nursing Home Data. CDC/CMS Nursing Home COVID‐19 Data Quality Assurance Process, 2020. https://data.cms.gov/download/bqa5-3dzf/application%2Fpdf. Accessed February 18, 2021.
- 16. USAFacts . US Coronavirus Cases & Deaths by State, 2021. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/. Accessed February 18, 2021.
- 17. Kind AJH, Buckingham WR. Making neighborhood‐disadvantage metrics accessible – the neighborhood atlas. N Engl J Med. 2018;378(26):2456‐2458. 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. University of Wisconsin School of Medicine Public Health . Area Deprivation Index v3.0. 2018. https://www.neighborhoodatlas.medicine.wisc.edu/. Accessed April 8, 2021.
- 19. Singh GK. Area deprivation and widening inequalities in US mortality, 1969‐1998. Am J Public Health. 2003;93(7):1137‐1143. 10.2105/AJPH.93.7.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30‐day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765‐774. 10.7326/M13-2946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Centers for Medicare & Medicaid Services . Nursing Home Care Compare Five‐Star Quality Rating System: Technical Users' Guide, 2021. https://www.cms.gov/Medicare/Provider‐Enrollment‐and‐Certification/CertificationandComplianc/downloads/usersguide.pdf. Accessed February 18, 2021.
- 22. Centers for Medicare & Medicaid Services . QSO‐20‐38‐NH, 2020. https://www.cms.gov/files/document/qso-20-38-nh.pdf. Accessed February 18, 2021. [PubMed]
- 23. Centers for Medicare & Medicaid Services . QSO 21‐06‐NH, 2020. https://www.cms.gov/files/document/qso-21-06-nh.pdf. Accessed February 18, 2021.
- 24. Centers for Medicare & Medicaid Services . Electronic Staffing Data Submission Payroll‐Based Journal: Long‐Term Care Facility Policy Manual, 2018. https://www.cms.gov/Medicare/Quality‐Initiatives‐Patient‐Assessment‐Instruments/NursingHomeQualityInits/Downloads/PBJ‐Policy‐Manual‐Final‐V25‐11‐19‐2018.pdf. Accessed February 18, 2021.
- 25. Centers for Medicare & Medicaid Services . Quality Measures, 2020. https://www.cms.gov/Medicare/Quality‐Initiatives‐Patient‐Assessment‐Instruments/NursingHomeQualityInits/NHQIQualityMeasures. Accessed February 18, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Full regression models of nursing home resident COVID‐19 on facility star ratings.


