Abstract
Background
This study evaluated two risk pathways that may account for increases in child internalizing and externalizing problems during the COVID‐19 pandemic: one pathway operating through pre‐existing family vulnerability and a second pathway operating through disruption in family functioning occurring in response to the pandemic. We assessed family disruption and family functioning with measures of key family‐level and parenting dimensions, including family cohesion, conflict and routines, and parents’ harsh discipline, lax discipline and warmth. In all models, pre‐pandemic parent emotional distress, financial strain and child maladjustment were included as covariates.
Methods
The sample included 204 families, comprised of parents who had children (M Age = 4.17; 45.1% girls). Parents (M Age = 27.43) completed the first survey prior to COVID‐19 onset in the United States, a second survey after COVID‐19 onset in May 2020 and a third survey two weeks later.
Results
Analyses were conducted in a model‐building fashion, first computing structural equation models for each family and parenting dimension separately, then advancing significant dimensions into one integrated model for the family‐level factors and a second model for parenting quality factors. Results provided more support for the family disruption hypothesis across all tests. In the family‐level domain, decreases in family cohesion and increases in family conflict each uniquely predicted subsequent child maladjustment. In the parenting domain, increases in harsh discipline and lax discipline each uniquely predicted subsequent child maladjustment. Family routines and parental warmth were not associated with child adjustment. However, parents’ emotional distress prior to the pandemic exhibited a robust association with children’s internalizing problems.
Conclusions
These findings indicate that efforts to support families in adapting to unique conditions of the pandemic will yield the greatest effect for child adjustment. Specifically, interventions should include efforts to help families maintain cohesion and manage conflict, and help parents minimize increases in harsh and lax discipline.
Keywords: Family functioning, parenting, adjustment problems
Introduction
The impact of the COVID‐19 pandemic on child mental health is a significant public health issue. Widely recognized as ‘unprecedented’ in nature, the COVID‐19 pandemic has resulted in social disruptions, including community, school and childcare closures that far exceeded anticipated durations (Qualls et al., 2017). Although critical in reducing disease spread, community mitigation strategies also have impacts in the form of job losses, financial insecurity, social isolation and confinement‐related stresses, that are expected to impact family and child well‐being (Prime, Wade, & Browne, 2020); these ideas stem largely from other studies of acute stress, such as family deterioration during the great recession (e.g. Brooks‐Gunn, Schneider, & Waldfogel, 2013). However, it is critical to understand the risk processes driving impacts on families and children during COVID‐19; in the absence of such research, practitioners must rely on developmental research conducted under typical circumstances that may not be applicable to the unique context of the COVID‐19 pandemic.
Emerging data confirm fears of the negative mental health impact of the pandemic. Early reports suggest increased prevalence of children’s depression, anxiety and behaviour problems during COVID‐19 (Liu et al., 2021; Marques de Miranda, da Silva Athanasio, Sena Oliveira, & Simoes‐e‐Silva, 2020). Findings regarding individuals age 16 and older from the UK Household Longitudinal Study document an increase in mental health problems relative to data collected prior to COVID‐19 to April 2020 (Pierce et al., 2020); corresponding results have emerged in cross‐national data from 59 countries (Alzueta et al., 2020). Regarding children’s mental health, 14% of parents in a June 2020 US national survey reported that their children’s mental health had worsened during the pandemic (Patrick et al., 2020). Recent longitudinal data indicated large effect sizes regarding increases in children’s externalizing (d = 1.59) and internalizing (d = 1.31) problems (Feinberg et al., 2021). Thus, a critical next step is to identify key pathways of risk that can guide interventionists seeking to minimize the immediate impact and forestall a long‐term increase in children’s mental health problems.
In this paper, we draw on ideas that social disruptions incurred during the COVID‐19 pandemic and caregiver well‐being may lead to disruptions in family‐level and parent–child relations, all of which may account for child maladjustment (Prime et al., 2020). We conceptualize family‐level functioning (cohesion, conflict and routines) and parenting quality (harshness, laxness and warmth) as proximal risk or protective factors for child mental health, each of which are amenable to existing evidence‐based interventions (e.g. Van Ryzin, Kumpfer, Fosco, & Greenberg, 2016). We further expand on these conceptualizations to examine whether pre‐existing difficulties or pandemic‐related disruptions in family and parenting factors predict declines in child adjustment with the onset of the pandemic.
Family cohesion, conflict and routines all have well‐established implications for child adjustment. Family cohesion refers to the quality of emotional bonds among family members (Olson, Waldvogel, & Schlieff, 2019) and is associated with reduced risk for youth externalizing problems (Lucia & Breslau, 2006; McKelvey, Conners‐Burrow, Mesman, Pemberton, & Casey, 2015; Richmond & Stocker, 2006) and internalizing problems (Deng et al., 2006; McKeown et al., 1997). Family conflict, including disagreements, anger and hostility among family members, is a robust risk factor for child maladjustment. Namely family conflict is associated with both internalizing and externalizing problems (Benson & Buehler, 2012; Formoso, Gonzales, & a, & Aiken, L. S., 2000; Jaycox & Repetti, 1993). Other work documents family cohesion and conflict as distinct constructs with unique implications for youth well‐being (Forgatch & DeGarmo, 1999; Fosco, Caruthers, & Dishion, 2012; Fosco & Lydon‐Staley, 2020). Family routines refer to regular practices in family life that are thought to promote predictability and organization (Fiese et al., 2002; Harrist, Henry, Liu, & Sheffield Morris, 2019), and in this study conceptualized as having regular family dinners, organized family activities, and regular wake and bedtimes for children. Developmental evidence from the Add Health study point to family connectedness (inclusive of the participation in daily routines around waking, regular meals together, and regular bedtimes) as highly protective against a number of long‐term risks in adolescence (Resnick et al., 1997). Maintaining family routines is protective for child developmental outcomes, even in contexts with elevated risk (Fiese et al., 2002; Kiser, Bennett, Heston, & Paavola, 2005). We propose that the degree to which families maintain routines during the COVID‐19 pandemic may thus may be a salient predictor of child well‐being (Harrist et al., 2019; Masten & Motti‐Stefanidi, 2020; Prime et al., 2020).
Parenting quality also impacts child adjustment; harsh and lax discipline conferring risk and parental warmth operating as a protective factor for children’s maladjustment. Harsh discipline refers to angry, coercive, over‐reactive responses to children’s misbehaviour (Arnold, O’Leary, Wolff, & Acker, 1993; Dishion & Snyder, 2015); whereas lax discipline refers to parenting that is overly permissive, failing to apply corrective feedback or consequences to misbehaviour (Arnold et al., 1993; Maccoby & Martin, 1983). Finally, parental warmth refers to supportive, responsive and affectionate parenting practices (Easterbrooks & Goldberg, 1984; Maccoby & Martin, 1983). Decades of empirical evidence, across well over 1000 published studies document the robust implications of each of these parenting dimensions for children’s adjustment, in both cross‐sectional and longitudinal studies (Pinquart, 2017a, 2017b).
The current study: Process models of risk for child maladjustment during COVID‐19
This study evaluated whether the above domains of family functioning reflect processes by which risk is conferred to children’s internalizing and externalizing problems in the unique context of the COVID‐19 pandemic. Through the study of process‐focused models, it is possible to identify key risk pathways to guide the selection and delivery of evidence‐based, family‐focused interventions with optimal effect. We evaluated two hypothesized pathways of risk for children’s maladjustment. First, we considered a pre‐existing vulnerabilities pathway, in which families already challenged with poor family relationship quality and/or lower‐quality parenting prior to COVID‐19 would be at elevated risk for child maladjustment during COVID‐19. Second, we tested a family disruption pathway, which posits that the degree to which family functioning and parenting quality deteriorate (e.g. decreases in cohesion, increases in harsh/lax parenting) from pre‐ to post‐COVID‐19 may predict subsequent child maladjustment during the COVID‐19 pandemic. Our analyses accounted for parents’ emotional distress and family financial strain prior to COVID‐19 as potentially important factors in children’s adjustment during the pandemic (Prime et al., 2020). Finally, we controlled for pre‐pandemic levels of children’s internalizing and externalizing problems to assess the role of family risk pathways in impacting children’s mental and behavioural health.
Method
Participants
We analysed a sample of families from a larger, intergenerational study already in progress prior to COVID‐19 onset in the United States. Of the 244 families who had participated in the larger study, 204 agreed to complete surveys during COVID‐19. No differences were found between these two samples on any demographic or study variables. Children (45.1% girls) in this sample were an average of 4.17 years old (SD Age = 2.17) at the time of the original study. Participating caregivers (M Age = 27.43, SD Age = 1.67) identified as the child’s mother (70.6%), father (22.5%), stepmother (1.5%), stepfather (2.5%) or other caregiver (1.0%); their racial background was White/Caucasian (90.7%), Black/African American (4.4%), American Indian, Eskimo, or Aleut (0.5%), or Other (4.4%); 10.8% reported that they were of Hispanic origin. Caregivers reported their child’s race as: White/Caucasian (91.7%), Black/African American (7.4%), American Indian, Eskimo, or Aleut (1.0%), Asian or Pacific Islander (0.5%), or Other (4.4%); 12.3% of children were of Hispanic origin. Most caregivers (79.4%; n = 162) reported that they lived with a second caregiving adult for the child (of these, 76.5% were the child’s other biological parent). Of those living with another caregiver, 68.5% were married, 24.1% were in a romantic relationship, 14.9% were cohabiting, and 6.2% were other family members. Of those not living with another caregiver, 45.2% were single, 16.7% were divorced or separated, 14.3% were in a romantic relationship but not living together, and 16.7% reported having another arrangement. Annual family income ranged from ‘0–$9,999’ to ‘$100,000 or more’ (Median: $50,000–59,999).
Procedure
The current sample was recruited from a larger project (Pathways to Health [P2H]; HD092439), an ongoing study evaluating the intergenerational transmission of parenting and family relationships. P2H was an extension of a community‐randomized trial of the PROmoting School‐community‐university Partnerships to Enhance Resilience intervention delivery system (PROSPER; Spoth et al., 2007), which recruited students (N = 10,845) in 28 rural and semi‐rural communities in 6th grade. PROSPER followed students through high school and then continued to follow a subset (N = 1,984) of the original sample in young adulthood. Young adults who were parents of children between the ages of 1.5–10 years old were invited to participate in home‐based data collection. In March of 2020, recruitment and data collection for P2H were paused due to the COVID‐19 pandemic.
Following COVID‐19 onset, all families already enrolled in P2H (N = 244) were invited to participate in biweekly surveys beginning 8 May 2020 to assess coping during the pandemic. Participating parents completed web‐based surveys. The first surveys were deployed during national stay‐at‐home orders. A second survey was sent out two weeks later, resulting in one pre‐pandemic assessment (T1) and two assessments conducted during the pandemic (T2, T3). To reduce participant burden, scales were abbreviated at T2 and T3. For repeated measures in the current study, only items from the shortened versions of each scale were used. Items for measures can be found in the Appendix S1.
Measures
All variables were scored so that higher values reflected higher levels of each construct.
Family‐level functioning (T1, T2)
Family cohesion (αT1 = .80, αT2 = .83) and family conflict (αT1 = .84, αT2 = .84) were each measured using 3 items from the shortened Family Environment Scale (Bloom, 1985). Family routines were measured using 4 items (αT1 = .63, αT2 = .71) from the Child Routines Inventory (Sytsma, Kelley, & Wymer, 2001). At T1, shortened scales were highly correlated with original scales (r’s = .84–.96), suggesting good validity.
Parenting quality (T1, T2)
Harsh discipline (αT1 = .67, αT2 = .71) and lax discipline (αT1 = .60, αT2 = .78) were each measured using 3 from the Parenting Scale (Arnold et al., 1993). Parental warmth was measured with 5 items (αT1 = .59, αT2 = .79) from the Parental Attitudes towards Child Rearing (PACR) warmth scale (Goldberg & Easterbrooks, 1984). At T1, shortened scales were highly correlated with original scales (r’s = .82–.88), suggesting good validity.
Child adjustment
At T1, children’s internalizing and externalizing problems were measured using the Child Behavior Checklist (Achenbach & Rescorla, 2000, 2001). Given the range in age, different versions were used (1½–5 and 6–18). These internalizing (1½–5 α = .87, 6–18 α = .76) and externalizing (1½–5 α = .90, 6–18 α = .86) scales demonstrated good reliability. Scores were converted into internalizing and externalizing T‐scores to allow for comparable scores across all children for analysis. To minimize participant burden brief, 5‐item assessments of child adjustment were developed for the T3 COVID‐19 survey using items adapted from the Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997) and the Child Adjustment and Parent Efficacy Scale (CAPES; Morawska, Sanders, Haslam, Filus, & Fletcher, 2014), which yielded reliable, measures of internalizing (α = .82) and externalizing problems (α = .72).
Covariates
Parent emotional distress was measured at T1 using the 20‐item Center for Epidemiological Studies‐Depression (Radloff, 1977; αT1 = .91) and the 7‐item Penn State Worry Questionnaire (Meyer, Miller, Metzger, & Borkovec, 1990; αT1 = .96). These were highly correlated (r = .62, p < .01), and thus were standardized and averaged to represent parent emotional distress. Financial strain was measured at T1 using four items (αT1 = .78) from the Financial Strain Index (Vinokur, Price, & Caplan, 1996). Time lapse was a measure of the number of weeks between T1 and T2 to capture spacing of measurements assessed in latent change scores (M = 37.9, Range = 8.3–70.7).
Results
Descriptive statistics and bivariate correlations among study variables are presented in Table 1. Variables exhibited acceptable levels of skew (<2.2). Correlations among variables were in the expected directions, with associations of small to moderate magnitude among family‐level and parenting quality variables, suggesting that these measures captured distinct facets of family life. We examined whether intervention condition (in P2H) was associated with any study variables; no significant intervention‐control differences were found. Thus, structural models were computed as planned and condition was omitted from analyses.
Table 1.
Correlations, means, and standard deviations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Fin T1 | |||||||||||||||||||
| 2 | P Distress T1 | .34 | ||||||||||||||||||
| 3 | Time Lapse | −.07 | .09 | |||||||||||||||||
| 4 | COH T1 | −.27 | −.22 | .08 | ||||||||||||||||
| 5 | CON T1 | .27 | .38 | .03 | −.35 | |||||||||||||||
| 6 | ROUT T1 | −.15 | −.06 | .08 | .23 | −.21 | ||||||||||||||
| 7 | HARSH T1 | .13 | .19 | .03 | −.18 | .24 | −.05 | |||||||||||||
| 8 | LAX T1 | .15 | .19 | −.19 | −.18 | .18 | −.16 | .26 | ||||||||||||
| 9 | WARM T1 | −.15 | −.03 | .09 | .18 | −.01 | .16 | −.20 | −.20 | |||||||||||
| 10 | INT T1 | .20 | .39 | −.03 | −.15 | .21 | −.13 | .17 | .17 | −.18 | ||||||||||
| 11 | EXT T1 | .17 | .32 | .06 | −.19 | .29 | −.14 | .26 | .22 | −.02 | .61 | |||||||||
| 12 | COH T2 | −.23 | −.30 | .01 | .32 | −.30 | .13 | −.21 | −.24 | .10 | −.29 | −.25 | ||||||||
| 13 | CON T2 | .22 | .23 | .15 | −.26 | .32 | −.14 | .20 | .12 | −.06 | .30 | .30 | −.22 | |||||||
| 14 | ROUT T2 | −.21 | −.21 | .02 | .36 | −.27 | .57 | −.14 | −.27 | .14 | −.14 | −.18 | .35 | −.22 | ||||||
| 15 | HARSH T2 | .20 | .19 | .17 | −.08 | .21 | −.05 | .60 | .12 | −.01 | .21 | .28 | −.29 | .38 | −.13 | |||||
| 16 | LAX T2 | .20 | .05 | −.21 | −.18 | .12 | −.18 | .19 | .60 | −.19 | .08 | .13 | −.17 | .08 | −.28 | .12 | ||||
| 17 | WARM T2 | −.15 | −.05 | .07 | .21 | −.25 | .12 | −.13 | −.11 | .27 | −.11 | −.13 | .29 | −.05 | .24 | −.07 | −.13 | |||
| 18 | INT T3 | .24 | .38 | .04 | −.14 | .17 | −.07 | .14 | −.06 | −.05 | .43 | .30 | −.33 | .25 | −.08 | .31 | .11 | −.06 | ||
| 19 | EXT T3 | .23 | .28 | .01 | −.11 | .13 | −.13 | .13 | .15 | −.03 | .31 | .40 | −.23 | .29 | −.12 | .28 | .28 | .00 | .60 | |
| N | 200 | 199 | 200 | 199 | 198 | 199 | 197 | 197 | 199 | 185 | 187 | 201 | 199 | 200 | 201 | 201 | 202 | 181 | 179 | |
| M | 1.40 | .00 | 37.90 | 7.96 | 2.72 | 3.44 | 3.25 | 2.47 | 5.57 | 48.43 | 48.27 | 7.82 | 2.18 | 3.45 | 3.45 | 2.54 | 5.46 | .83 | .86 | |
| SD | .53 | .90 | 16.17 | 1.87 | 2.01 | .58 | 1.20 | .97 | .51 | 10.06 | 9.68 | 1.98 | 1.91 | .60 | 1.24 | 1.09 | .66 | .56 | .59 |
T1 = Bold correlations indicate statistical significance (p < .05). Subscripts: T1 = Pre‐COVID‐19 assessment, T2 = First COVID‐19 assessment, T3 = Second COVID‐19 assessment. Fin = Financial strain, P Distress = Parent emotional distress, COH = Cohesion, CON = Conflict, ROUT = Routines, EXT = Externalizing problems, INT = Internalizing problems.
Structural models evaluating family indicators separately
All models were computed using Mplus 8.4 (Muthén & Muthén, 1998‐2019), using full information maximum likelihood estimation and evaluated following standard convention for model fit: chi‐square (p > .05), root mean square error of approximation (RMSEA < .08), Comparative Fit Index (CFI > .95), the Tucker–Lewis Index (TLI > .95) (Hu & Bentler, 1999). Analyses proceeded in a model‐building fashion. In the first step, three sets of separate structural models were computed in each of the two domains (family‐level and parenting quality) and totalling six preliminary models (see prototypical model in Figure 1). The direct pathways from T1 family functioning to children’s internalizing and externalizing problems at T3 (‘a’ pathways) reflect the pre‐existing vulnerabilities hypothesis. Latent change scores (LCS; Grimm, Ram, & Estabrook, 2016; McArdle, 2009) were calculated to model intra‐family change from T1 to T2. A family disruption hypothesis was supported when this latent change variable was associated with children’s internalizing and externalizing problems at the subsequent measurement occasion, T3 (‘b’ pathways). In all models, we included pre‐pandemic parent emotional distress, family financial strain as covariates, as well as pre‐COVID levels of children’s internalizing and externalizing problems. Between‐family differences in time lapse between pre‐COVID and the first post‐COVID controlled for in the latent change models. Autoregressive parameters predicting latent change reflect the degree to which change was proportional to the scores at T1. In the second step, we advanced risk or protective factors significant in the separate preliminary models to build final models for family‐level and parenting quality processes.
Figure 1.
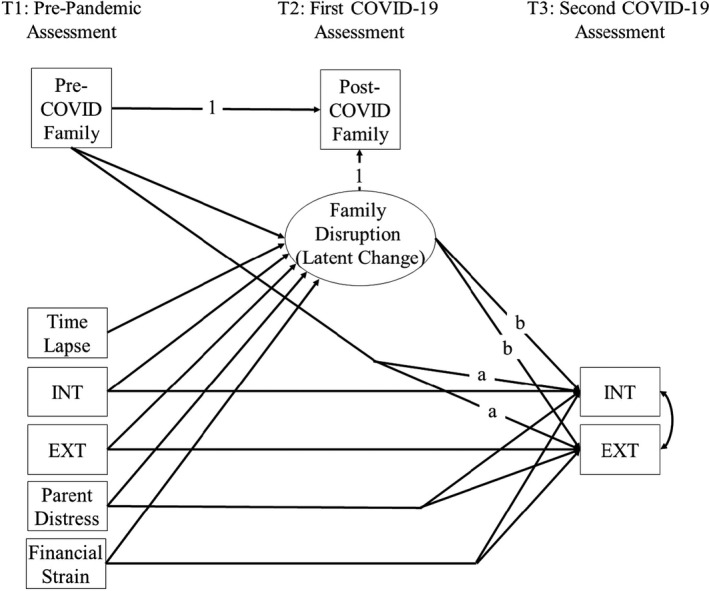
Prototypical structural equation model testing pre‐existing vulnerabilities and family disruption risk pathways
All of the preliminary models yielded satisfactory fit with the data (Table 2). The bottom two rows of the table report average change and variance in the LCS factors. All six LCS exhibited statistically significant variance, indicating meaningful between‐family differences in the degree of family disruption from T1 to T2. Mean LCS offer additional information: on average, there were small decreases in family conflict and parental warmth, and slight increases harsh discipline in the sample overall. Family cohesion, routines and lax discipline did not exhibit significant average levels of change. In the context of significant variance, cohesion, routines and lax discipline exhibited increases and decreases across families in a manner that averaged out to be zero overall.
Table 2.
Testing pre‐existing vulnerabilities and family disruption pathways to child maladjustment during COVID‐19
| Fit Statistics | Family Cohesion | Family Conflict | Family Routines | Harsh Discipline | Lax Discipline | Parental Warmth | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| fit | p | fit | p | fit | p | fit | p | fit | p | fit | p | ||
| Model Fit | Chi‐square (9): | 8.634 | .472 | 7.080 | .628 | 8.363 | .498 | 7.023 | .635 | 17.142 | .047 | 8.026 | .532 |
| CFI | 1.000 | 1.000 | 1.000 | 1.000 | .968 | 1.000 | |||||||
| CFI | 1.000 | 1.000 | 1.000 | 1.000 | .968 | 1.000 | |||||||
| RMSEA | .000 | .000 | .000 | .000 | .067 | .000 | |||||||
| (90% C.I.) | (.000–.077) | (.000–.067) | (.000–.076) | (.000–.067) | (.008–.115) | (.000–.073) | |||||||
| Path Coefficient | β | p | β | p | β | p | β | p | β | p | β | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre‐Existing Vulnerability | Pre‐Fam‐> INTT3 | −.150 | .073 | .102 | .259 | .016 | .843 | .164 | .026 | −.118 | .088 | .031 | .691 |
| Pre‐Fam‐>EXTT3 | −.062 | .488 | .073 | .446 | −.040 | .636 | .088 | .265 | .114 | .115 | .035 | .652 | |
| Family Disruption | LCS‐>INTT3 | −.192 | .019 | .175 | .043 | .045 | .551 | .255 | .001 | .170 | .016 | −.007 | .928 |
| LCS‐>EXT T3 | −.102 | .233 | .206 | .021 | .015 | .851 | .183 | .017 | .257 | .000 | .065 | .396 | |
| Covariates | P. Distress T1‐> INT T3 | .194 | .008 | .229 | .002 | .232 | .002 | .230 | .001 | .264 | .000 | .220 | .003 |
| P. Distress T1‐> EXT T3 | .110 | .147 | .144 | .060 | .129 | .087 | .126 | .085 | .154 | .035 | .123 | .098 | |
| Fin T1‐>INT T3 | .089 | .205 | .095 | .173 | .112 | .117 | .068 | .318 | .086 | .220 | .117 | .099 | |
| Fin T1‐> EXT T3 | .116 | .115 | .114 | .116 | .118 | .109 | .096 | .184 | .068 | .349 | .130 | .078 | |
| Time‐>LCS | .001 | .989 | .109 | .044 | −.012 | .854 | .163 | .009 | −.099 | .144 | .046 | .464 | |
| P. Distress T1 ‐> LCS | −.132 | .047 | .000 | .999 | −.170 | .018 | −.028 | .700 | −.132 | .083 | .018 | .806 | |
| Pre‐Fam ‐> LCS | −.621 | .000 | −.700 | .000 | −.470 | .000 | −.476 | .000 | −.360 | .000 | −.466 | .000 | |
| Fin T1‐>LCS | −.075 | .239 | .102 | .084 | −.067 | .329 | .135 | .050 | .197 | .006 | −.094 | .174 | |
| INT T1‐>LCS | −.115 | .155 | .125 | .092 | .074 | .407 | .086 | .312 | −.022 | .817 | .045 | .619 | |
| EXT T1‐>LCS | −.045 | .573 | .089 | .223 | −.085 | .324 | .083 | .325 | .043 | .626 | −.140 | .102 | |
| Autoregressive Paths | INT T1‐>INT T3 | .285 | .000 | .288 | .000 | .306 | .000 | .275 | .000 | .320 | .000 | .317 | .000 |
| EXT T1‐>EXT T3 | .321 | .000 | .313 | .000 | .326 | .000 | .322 | .000 | .312 | .000 | .341 | .000 | |
| Latent | LCS Mean | −.132 | .405 | −.551 | .001 | .021 | .598 | .186 | .017 | .085 | .200 | −.108 | .031 |
| Change | LCS Variance | 5.004 | .000 | 5.218 | .000 | .300 | .000 | 1.198 | .000 | .871 | .000 | .504 | .000 |
Standardized coefficients presented (except LCS Mean and Variance), bold indicates statistical significance.
Pre‐Fam = Pre‐COVID‐19 family variable; Fin = Financial strain; P. Distress = Parent emotional distress; Time = time between pre‐ and 1st post‐COVID assessment; LCS = Latent Change Score (Disruption); subscripts indicate measurement occasions T1‐3. LCS mean and variance were computed in unconditional models.
Parents’ emotional distress prior to COVID‐19 was a consistent predictor of change in children’s internalizing problems across all six models; in two of the six models, parent emotional distress was positively associated with externalizing problems. T1 financial strain was not associated with internalizing or externalizing problems (across models). Tests of the pre‐existing vulnerability hypothesis yielded no significant associations of T1 family cohesion, conflict, nor routines with children’s internalizing or externalizing problems at T3. LCS findings indicated that disruption to family cohesion (i.e. decreases) was associated with elevated risk for child internalizing problems during the pandemic (β = −.19). Disruption in family conflict was significantly associated with elevated risk for child internalizing (β = .18) and externalizing (β = .21) problems during the pandemic. Family routines LCS was not associated with children’s adjustment problems at T3.
Regarding parenting quality, pre‐COVID‐19 harsh discipline was associated with increases in children’s internalizing problems (β = .16); however, no support for pre‐existing vulnerabilities was found for lax parenting or parental warmth. Disruption LCS paths indicated that worsening harsh and lax parenting predicted T3 children’s internalizing (β’s =.26,.17 respectively) and externalizing (β’s = .18, .26 respectively) problems. Disruptions to parental warmth did not predict children’s maladjustment.
Evaluating family‐level and parenting quality models of risk
Significant indicators of risk or protection were integrated in subsequent models. The family‐level model is presented in Figure 2. Because only family cohesion and conflict were associated with child adjustment problems in prior models, both were included in the final model to evaluate their unique and relative impact. The model yielded good fit with the data (see Figure 2). Findings were consistent with prior models. No evidence was found for pre‐existing family vulnerability hypotheses. Cohesion and conflict disruption pathways were statistically significant. Specifically, families evidencing greater declines in family cohesion had children with increased levels of internalizing problems during the pandemic (β = −.20). Increases in family conflict also were positively associated with increases in internalizing (β = .17) and externalizing (β = .21) problems during the pandemic.
Figure 2.
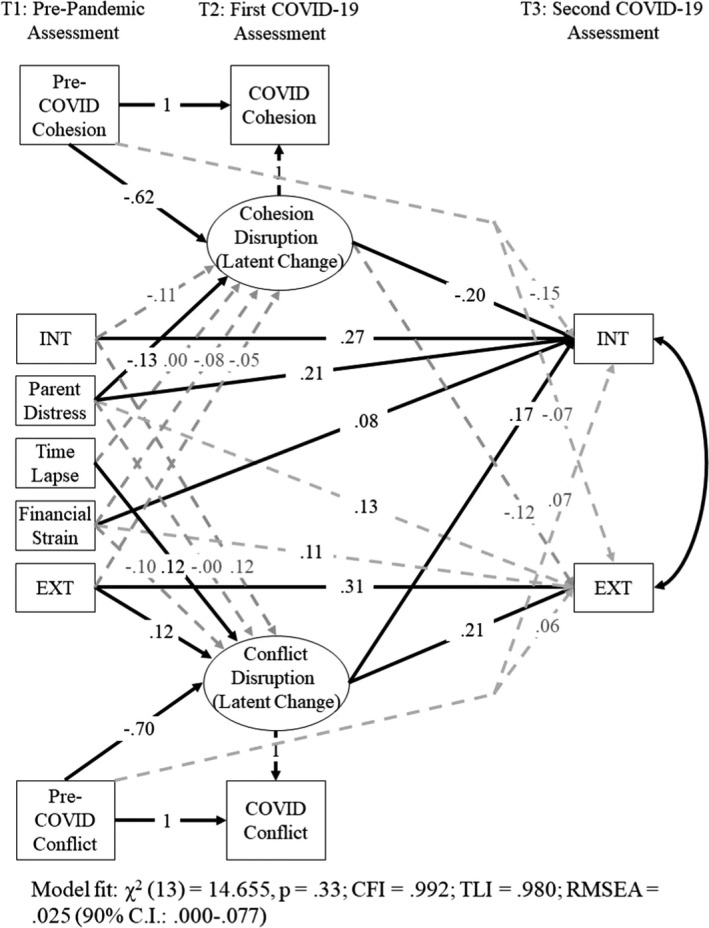
Integrated model testing family cohesion and conflict pathways to child maladjustment
As a post hoc analysis, we replaced T1 parent distress with T2 parent distress to see if parent distress during the pandemic had different effects (see Figure S1). Overall, models were largely consistent, only two paths regressing internalizing problems on conflict LCS and pre‐COVID‐19 financial strain not statistically significant.
The same approach was followed when building the final parenting quality model. Due to lack of evidence for parental warmth, only harsh and lax parenting were included in the model (Figure 3). The model yielded good fit with the data (see Figure 3). When accounting for both aspects of parenting simultaneously, findings mirrored those in the preliminary models. Harsh discipline, but not lax discipline, prior to the pandemic was associated with increased risk for children’s internalizing problems at T3 (β = .18). Disruptions in harsh and lax discipline were uniquely associated with child adjustment problems. Larger increases in harsh discipline were associated with increases in children’s internalizing (β = .24) and externalizing (β = .19) problems at T3. Likewise, increases in lax discipline were associated with increases in children’s internalizing (β = .16) and externalizing (β = .26) problems.
Figure 3.
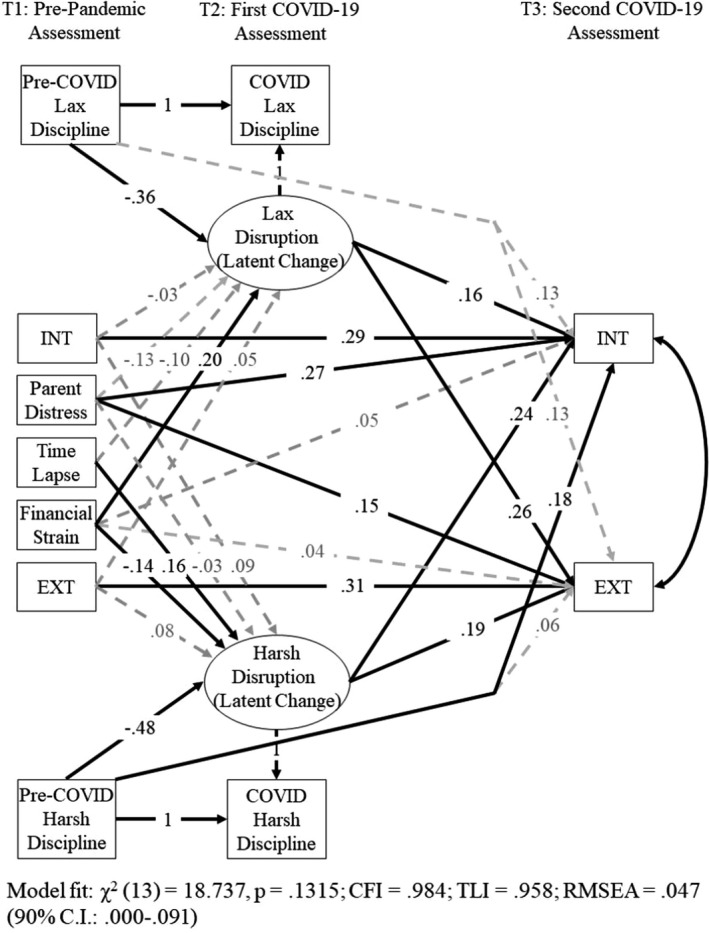
Integrated model testing harsh and lax discipline pathways to child maladjustment
Post hoc analyses were repeated for this model using T1 parent distress with T2 distress (see Figure S2). Most substantive findings were replicated in this model, except one path; parent emotional distress predicting T3 externalizing problems was nonsignificant.
Discussion
This study evaluated family risk and protection processes for children’s maladjustment during the COVID‐19 pandemic. Longitudinal tests of pre‐existing family vulnerability and family disruption hypotheses were conducted for family‐level cohesion, conflict and routines, as well as for harsh, lax and warm parenting practices. These analyses accounted for parent emotional distress, family financial strain and children’s maladjustment prior to COVID‐19. The results from these analyses offer insights into the aspects of family functioning that are most salient in predicting children’s maladjustment, as well as the processes of risk and protection.
Generally, our findings lend more support to a family disruption risk process than to the pre‐existing family vulnerability hypothesis. Declines in family cohesion and upsurges in family conflict, harsh discipline and lax discipline accounted for children’s internalizing and externalizing risk. Only one of six tested pre‐existing family vulnerability processes – harsh discipline – predicted greater children’s internalizing problems at T3. It may be that disruptions to family functioning reflect a family’s inability to adapt to the new circumstances and constraints during COVID‐19 (Masten & Motti‐Stefanidi, 2020), and these disruptions to family relationships and parenting quality are key signals of risk for child maladjustment (Prime et al., 2020).
The findings supporting the role of family disruption processes in undermining child adjustment offer guidance for prevention efforts aimed at minimizing the impact of the pandemic on children’s mental health. Namely, efforts to bolster family cohesion and to support effective family problem‐solving to resolve conflicts may help reduce disruptions to family relations that undermine well‐being. Additionally, parenting support around using effective discipline strategies – ensuring that they are upholding family rules and using reasonable consequences for misbehaviour – may be helpful support for parents who, when coping with the unique stressors from the pandemic, may resort overly harsh or overly lax parenting. As a whole, findings supporting family disruption risk pathways call for interventions that can help families return to baseline levels of cohesion, conflict management and effective parenting practices.
Parent’s emotional distress prior to COVID‐19 was an important predictor of child adjustment – particularly internalizing problems – over and above both pre‐existing and changes in family relationships and parenting quality. This is consistent with propositions from Prime and colleagues (2020) and cross‐sectional evidence of associations between parents’ distress and child well‐being (Luthar, Ebbert, & Kumar, 2020; Spinelli, Lionetti, Pastore, & Fasolo, 2020); our findings extend this work by providing prospective, longitudinal evidence of a direct link between parent’s emotional distress and child internalizing problems. Together these findings, underscore the importance of parent mental health in supporting child well‐being. Parent self‐care, mood management and resilience are important for children’s mental health during the pandemic.
Surprisingly, family routines and parental warmth did not predict children’s internalizing or externalizing problems through either hypothesized pathway. Our measure of family routines focused on day‐to‐day patterned family interactions, such as bedtime routines, organized family activities and regular family meals that generally are promotive of child well‐being (Fiese et al., 2002). However, during the COVID‐19 pandemic, particularly in the first three months when the study assessments were conducted, it is possible that such routines may be less essential for children’s well‐being. In the context of childcare closures, remote/asynchronous education and diminished structure to their daily activities, these types of routines may be less salient. Other findings might emerge later in the pandemic or in relation to disrupted rituals, such as disrupted family traditions, holidays and celebrations.
Parental warmth also did not predict children’s adjustment during the COVID‐19 pandemic. Instead, our findings point to increases in harsh and lax discipline practices as more salient dimensions of risk for children’s internalizing and externalizing problems during the pandemic. Again, it is possible that disruptions to parental warmth would be impactful on a longer timescale than was captured in this study, but our findings suggest that promoting effective discipline practices during the COVID‐19 pandemic may be a more fruitful avenue to supporting child well‐being.
Limitations
This study had important limitations. First, only parent self‐report data were available from families during the pandemic due to data collection limitations; such measures are vulnerable to subjectivity and reporter bias. To reduce participant burden, several scales were shortened, which may limit the breadth and reliability of measurement. Additionally, our sample was largely White and findings may not generalize to diverse families.
Conclusions
Family and parenting disruption during the COVID‐19 pandemic appears to be a key risk pathway for children’s internalizing and externalizing problems. Specifically, deteriorated family cohesion, and increases in family conflict, harsh discipline and lax discipline foreshadow increases in children’s internalizing and externalizing problems during the pandemic. Additionally, pre‐existing levels of parents’ poor mental health further elevates children’s risk for increased maladjustment during the pandemic. Family support practices that focus on helping families re‐establish positive relations, effectively manage conflicts and use effective discipline practices are expected to be effective strategies for mitigating risk from the COVID‐19 pandemic on children’s mental health problems.
Supporting information
Appendix S1. Measures.
Figure S1. Alternate Integrated Model Testing Family Cohesion and Conflict Pathways to Child Maladjustment.
Figure S2. Alternate Integrated Model Testing Harsh and Lax Discipline Pathways to Child Maladjustment.
Acknowledgements
The authors would like to thank participating families and Catrina Carlton for her assistance in project administration. Data collection for P2H was funded by the National Institute of Child Health and Human Development R01‐HD092439 (Co‐PIs: Fosco & Feinberg) and the Huck Institutes of the Life Sciences and the Social Science Research Institute at Pennsylvania State University (PI: Feinberg). The PROSPER study was funded by grant R01‐DA013709 (PI: Spoth) from the National Institute on Drug Abuse and co‐funded by the National Institute on Alcohol Abuse and Alcoholism. Authors were supported by additional funding sources: C.J.S. received support from the National Center for Advancing Translational Sciences TL1‐TR002016 and UL1‐TR002014. The funders had no role in study design; collection, analysis and interpretation of data; writing the report; and the decision to submit the report for publication. The authors have declared that they have no competing or potential conflicts of interest.
Key points .
The detrimental psychological impact of the COVID‐19 pandemic is gaining growing empirical support; however, pathways of risk not well understood.
After testing six potential family pathways for child maladjustment during the pandemic, our results suggest that it is disruptions to family functioning, rather than pre‐existing family vulnerability that predicts pandemic‐period increases in children’s maladjustment.
At the family level, changes in cohesion and conflict predicted change in child maladjustment.
In the parenting domain, increased harsh and lax discipline predicted change in child maladjustment.
Our findings offer guidance regarding key avenues of intervention that may mitigate the impact of the COVID‐19 pandemic on child adjustment.
Conflict of interest statement: No conflicts declared.
References
- Achenbach, T.M. , & Rescorla, L.A. (2000). Manual for ASEBA preschool forms & profiles. In University of Vermont (Vol. 30). 10.1007/s10826-014-9968-6 [DOI]
- Achenbach, T.M. , & Rescorla, L.A. (2001). Manual for the ASEBA school‐age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families. [Google Scholar]
- Alzueta, E. , Perrin, P. , Baker, F.C. , Caffarra, S. , Ramos‐Usuga, D. , Yuksel, D. , & Arango‐Lasprilla, J.C. (2020). How the COVID‐19 pandemic has changed our lives: A study of psychological correlates across 59 countries. Journal of Clinical Psychology, 77, 556–570. [DOI] [PubMed] [Google Scholar]
- Arnold, D.S. , O’Leary, S.G. , Wolff, L.S. , & Acker, M.M. (1993). The Parenting Scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment, 5, 137–144. [Google Scholar]
- Benson, M.J. , & Buehler, C. (2012). Family process and peer deviance influences on adolescent aggression: Longitudinal effects across early and middle adolescence. Child Development, 83, 1213–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom, B.L. (1985). A factor analysis of self‐reported measures of family functioning. Family Process, 24, 225–239. [DOI] [PubMed] [Google Scholar]
- Brooks‐Gunn, J. , Schneider, W. , & Waldfogel, J. (2013). The great recession and the risk for child maltreatment. Child Abuse and Neglect, 37, 721–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng, S. , Lopez, V. , Roosa, M.W. , Ryu, E. , Burrell, G.L. , Tein, J.Y. , & Crowder, S. (2006). Family processes mediating the relationship of neighborhood disadvantage to early adolescent internalizing problems. Journal of Early Adolescence, 26, 206–231. [Google Scholar]
- Dishion, T.J. , & Snyder, J. (2015). Coercion dynamics. In Dishion T.J., & Snyder J. (Eds.), The oxford handbook of coercive relationship dynamics (Vol. 1, Issue January 2019, pp. 1–14). 10.1093/oxfordhb/9780199324552.013.29 [DOI] [Google Scholar]
- Easterbrooks, M.A. , & Goldberg, W.A. (1984). Toddler development in the family: impact of father involvement and parenting characteristics. Child Development, 55, 740–752. [PubMed] [Google Scholar]
- Feinberg, M.E. , Mogle, J. , Lee, J.‐K. , Tornello, S.L. , Hostetler, M.L. , Cifelli, J.A. , … & Hotez, E. (2021). Impact of the COVID‐19 pandemic on parent, child, and family functioning. Family Process. 10.1111/famp.12649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiese, B.H. , Tomcho, T.J. , Douglas, M. , Josephs, K. , Poltrock, S. , & Baker, T. (2002). A review of 50 years of research on naturally occurring family routines and rituals: Cause for celebration? Journal of Family Psychology, 16, 381–390. [DOI] [PubMed] [Google Scholar]
- Forgatch, M.S. , & DeGarmo, D.S. (1999). Two faces of Janus: Cohesion and conflict. In Conflict and cohesion in families: Causes and consequences (pp. 167–184). Mahwah, NJ: Lawrence Earlbaum Associates. [Google Scholar]
- Formoso, D. , Gonzales, N. , & Aiken, L.S. (2000). Family conflict and children’s internalizing and externalizing behavior: Protective factors. American Journal of Community Psychology, 28, 175–199. [DOI] [PubMed] [Google Scholar]
- Fosco, G.M. , Caruthers, A.S. , & Dishion, T.J. (2012). A six‐year predictive test of adolescent family relationship quality and effortful control pathways to emerging adult social and emotional health. Journal of Family Psychology, 26, 565–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosco, G.M. , & Lydon‐Staley, D.M. (2020). Implications of family cohesion and conflict for adolescent mood and well‐being: Examining within‐ and between‐family processes on a daily timescale. Family Process, 59, 1672–1689. 10.1111/famp.12515 [DOI] [PubMed] [Google Scholar]
- Goldberg, W.A. , & Easterbrooks, M.A. (1984). Role of marital quality in toddler development. Developmental Psychology, 20, 504–514. [Google Scholar]
- Goodman, R. (1997). The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581–586. [DOI] [PubMed] [Google Scholar]
- Grimm, K. J. , Ram, N. , & Estabrook, R. (2016). Growth modeling: Structural equation and multilevel modeling approaches. New York, NY: Guilford Publications. [Google Scholar]
- Harrist, A.W. , Henry, C.S. , Liu, C. , & Sheffield Morris, A. (2019). Family resilience: The power of rituals and routines in family adaptive systems. In Fiese B.H., Celano M., Deater‐Deckard K., Jouriles E.N., & Whisman M.A. (Eds.), APA handbooks in psychology®. APA handbook of contemporary family psychology: Foundations, methods, and contemporary issues across the lifespan (pp. 223–239). Washington, DC: American Psychological Association. [Google Scholar]
- Hu, L. , & Bentler, P.M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. [Google Scholar]
- Jaycox, L.H. , & Repetti, R.L. (1993). Conflict in families and the psychological adjustment of preadolescent children. Journal of Family Psychology, 7, 344–355. [Google Scholar]
- Kiser, L.J. , Bennett, L. , Heston, J. , & Paavola, M. (2005). Family ritual and routine: Comparison of clinical and non‐clinical families. Journal of Child and Family Studies, 14, 357–372. [Google Scholar]
- Liu, Q. , Zhou, Y. , Xie, X. , Xue, Q. , Zhu, K. , Wan, Z. , … & Song, R. (2021). The prevalence of behavioral problems among school‐aged children in home quarantine during the COVID‐19 pandemic in china. Journal of Affective Disorders, 279, 412–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucia, V.C. , & Breslau, N. (2006). Family cohesion and children’s behavior problems: A longitudinal investigation. Psychiatry Research, 141, 141–149. [DOI] [PubMed] [Google Scholar]
- Luthar, S.S. , Ebbert, A.M. , & Kumar, N.L. (2020). Risk and resilience during COVID‐19: A new study in the Zigler paradigm of developmental science. Development and Psychopathology, 33, 565–580. [DOI] [PubMed] [Google Scholar]
- Maccoby, E.E. , & Martin, J.A. (1983). Socialization in the context of the family: Parent‐child interaction. In Mussen P.H., & Hetherington E.M. (Eds.), Handbook of child psychology (4th ed., pp. 1–101). New York: Wiley. [Google Scholar]
- Marques de Miranda, D. , da Silva Athanasio, B. , Sena Oliveira, A.C. , & Simoes‐e‐Silva, A.C. (2020). How is COVID‐19 pandemic impacting mental health of children and adolescents? International Journal of Disaster Risk Reduction, 51, 101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten, A.S. , & Motti‐Stefanidi, F. (2020). Multisystem resilience for children and youth in disaster: Reflections in the context of COVID‐19. Adversity and Resilience Science, 1, 95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle, J.J. (2009). Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology, 60, 577–605. [DOI] [PubMed] [Google Scholar]
- McKelvey, L.M. , Conners‐Burrow, N.A. , Mesman, G.R. , Pemberton, J.R. , & Casey, P.H. (2015). Promoting adolescent behavioral adjustment in violent neighborhoods: supportive families can make a difference!. Journal of Clinical Child and Adolescent Psychology, 44, 157–168. [DOI] [PubMed] [Google Scholar]
- McKeown, R.E. , Garrison, C.Z. , Jackson, K.L. , Cuffe, S.P. , Addy, C.L. , & Waller, J.L. (1997). Family structure and cohesion, and depressive symptoms in adolescents. Journal of Research on Adolescence, 7, 267–281. [Google Scholar]
- Meyer, T.J. , Miller, M.L. , Metzger, R.L. , & Borkovec, T.D. (1990). Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy, 28, 487–495. [DOI] [PubMed] [Google Scholar]
- Morawska, A. , Sanders, M.R. , Haslam, D. , Filus, A. , & Fletcher, R. (2014). Child adjustment and parent efficacy scale: Development and initial validation of a parent report measure. Australian Psychologist, 49, 241–252. [Google Scholar]
- Muthén, L. K. , & Muthén, B. O. (1998–2019). Mplus user's guide (8th edn). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Olson, D.H. , Waldvogel, L. , & Schlieff, M. (2019). Circumplex model of marital and family systems: An update. Journal of Family Theory and Review, 11, 199–211. [Google Scholar]
- Patrick, S.W. , Henkhaus, L.E. , Zickafoose, J.S. , Lovell, K. , Halvorson, A. , Loch, S. , … & Davis, M.M. (2020). Well‐being of parents and children during the COVID‐19 Pandemic: A national survey. Pediatrics, 146, e2020016824. [DOI] [PubMed] [Google Scholar]
- Pierce, M. , Hope, H. , Ford, T. , Hatch, S. , Hotopf, M. , John, A. , … & Abel, K.M. (2020). Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7, 883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart, M. (2017a). Associations of parenting dimensions and styles with externalizing problems in children and adolescents: An updated meta‐analysis. Developmental Psychology, 53, 873–932. [DOI] [PubMed] [Google Scholar]
- Pinquart, M. (2017b). Associations of parenting dimensions and styles with internalizing symptoms in children and adolescents: A meta‐analysis. Marriage and Family Review, 53, 613–640. [DOI] [PubMed] [Google Scholar]
- Prime, H. , Wade, M. , & Browne, D.T. (2020). Risk and resilience in family well‐being during the COVID‐19 pandemic. American Psychologist, 75, 631–643. [DOI] [PubMed] [Google Scholar]
- Qualls, N. , Levitt, A. , Kanade, N. , Wright‐Jegede, N. , Dopson, S. , Biggerstaff, M. , … & Uzicanin, A. (2017). Community Mitigation Guidelines to Prevent Pandemic Influenza — United States, 2017. In Marbidity and Mortality Weekly Report (Vol. 66, Issue 1). http://www.cdc.gov/mmwr/cme/conted.html. [DOI] [PMC free article] [PubMed]
- Radloff, L.S. (1977). The CES‐D Scale: A self‐report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Resnick, M.D. , Bearman, P.S. , Blum, R.W. , Bauman, K.E. , Harris, K.M. , Jones, J. , … & Udry, J.R. (1997). From harm longitudinal study. JAMA, 278, 823–832. [DOI] [PubMed] [Google Scholar]
- Richmond, M.K. , & Stocker, C.M. (2006). Associations between family cohesion and adolescent siblings’ externalizing behavior. Journal of Family, 20, 663–669. [DOI] [PubMed] [Google Scholar]
- Spinelli, M. , Lionetti, F. , Pastore, M. , & Fasolo, M. (2020). Parents’ stress and children’s psychological problems in families facing the COVID‐19 outbreak in Italy. Frontiers in Psychology, 11, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth, R. , Redmond, C. , Shin, C. , Greenberg, M. , Clair, S. , & Feinberg, M. (2007). Substance‐use outcomes at 18 months past baseline. The PROSPER community‐university partnership trial. American Journal of Preventive Medicine, 32, 395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sytsma, S.E. , Kelley, M.L. , & Wymer, J.H. (2001). Development and initial validation of the child routines inventory. Journal of Psychopathology and Behavioral Assessment, 23, 241–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin, M.J. , Kumpfer, K.K. , Fosco, G.M. , & Greenberg, M.T. (2016). Family‐based prevention programs for children and adolescents: theory, research, and large‐scale dissemination. Psychology Press. [Google Scholar]
- Vinokur, A.D. , Price, R.H. , & Caplan, R.D. (1996). Hard times and hurtful partners: How financial strain affects depression and relationship satisfaction of unemployed persons and their spouses. Journal of Personality and Social Psychology, 71, 166–179. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Measures.
Figure S1. Alternate Integrated Model Testing Family Cohesion and Conflict Pathways to Child Maladjustment.
Figure S2. Alternate Integrated Model Testing Harsh and Lax Discipline Pathways to Child Maladjustment.


