Recently, Gao et al. published a paper entitled “Association between tuberculosis and COVID‐19 severity and mortality: A rapid systematic review and meta‐analysis” in the Journal of Medical Virology. 1 Their findings demonstrated that tuberculosis was not significantly associated with the increased risk for severity (odds ratio [OR] = 2.10, 95% confidence interval (CI): 0.61–7.18) and mortality (OR = 1.40, 95% CI: 0.10–18.93) in a meta‐analysis on the basis of six studies with 2765 COVID‐19 patients. 1 This study was extremely interesting but had limited sample sizes. To our knowledge, a series of articles on this topic have been emerging since then. Therefore, we performed this updated meta‐analysis to clarify the association between tuberculosis and COVID‐19 severity and mortality based on the latest data.
This study followed the Preferred Reporting Items for Systematic Reviews and Meta‐analysis (PRISMA) guidelines. 2 The electronic databases including PubMed, Web of Science, and EMBASE were systematically searched to identify the eligible studies published between January 1, 2020 and May 14, 2021. The keywords used were: “coronavirus disease 2019”, “COVID‐19”, “severe acute respiratory syndrome coronavirus 2”, “SARS‐CoV‐2”, “2019‐nCoV”, and “tuberculosis”. The outcomes of interest were severity (severe, critical, intensive care unit [ICU] admission, invasive mechanical ventilation [IMV], intubation or death), and mortality. All peer‐reviewed articles written in the English language reporting the association between tuberculosis and COVID‐19 severity and mortality were eligibly included. Accordingly, repeated articles, case reports, review papers, comments, errata, and studies without sufficient data were excluded. The pooled OR and 95% CI were estimated using a random‐effects meta‐analysis model. 3 Heterogeneity across studies was evaluated using the I 2 statistic. 4 , 5 Egger's test and Begg's test were conducted to assess publication bias. 6 , 7 , 8 Leave‐one‐out sensitivity analysis was performed to evaluate the stability of our results. 9 The statistical analyses were performed by R software (Version 3.6.3). Statistical significance was defined as p < 0.05.
Thirty‐six full‐text articles with 60,103 COVID‐19 patients were included in this study. Among them, 26 studies were from Asia (20 from China, three from Korea, and one each from Qatar, Turkey, and the Philippines), six studies were from Africa (two from Congo, two from South Africa, one from Ethiopia, and one from Nigeria), three studies came from Americas (two from Brazil and one from the United States) and one study was from multi‐country. The baseline characteristics of the enrolled studies are summarized in Table 1.
Table 1.
General information of the included studies on the association between tuberculosis and severity and mortality among coronavirus disease 2019 (COVID‐19) patients
| Author | Country | Study design | Sample sizes | Male (%) | Age | Severe (TB/cases, %) | Non‐severe (TB/cases, %) |
|---|---|---|---|---|---|---|---|
| Du RH | China | Prospective study | 179 | 54.2 | 57.6 ± 13.7 | Deceased (0/21, 0%) | Survival (8/158, 5.1%) |
| Mo P | China | Retrospective study | 155 | 55.5 | 54 (42–66) | Refractory (3/85, 3.5%) | General (0/70, 0%) |
| Zeng JH | China | Retrospective study | 416 | 47.6 | 46.58 | ICU (0/35, 0%) | Non‐ICU (8/381, 2%) |
| Sy KTL | Philippines | Cohort study | 430 | NR | NR | Died (25/71, 35.2%) | Recovery (57/359, 15.9%) |
| Li X | China | Ambispective study | 548 | 50.9 | 60 (48–69) | Severe (4/269, 1.5%) | Non‐severe (5/279, 1.8%) |
| Chen T | China | Case series | 55 | 53.2 | 54 (20–91) | Died (1/19, 5.3%) | Survived (0/36, 0%) |
| Zhang JJ | China | Retrospective study | 140 | 50.7 | 57 (25–87) | Severe (2/58, 3.4%) | Non‐severe (0/82, 0%) |
| Pierrotti LC | Brazil | Retrospective study | 51 | 49 | 51.9 (17–78) | ICU (1/23, 4.3%) | Non‐ICU (1/28, 3.6%) |
| Song J | China | Retrospective study | 961 | 52 | 63 (49–70) | Severe (2/242, 0.8%) | Non‐severe (18/719, 2.5%) |
| Lee JY | Korea | Retrospective study | 694 | 30.5 | 55.91 | Severe (0/137, 0%) | Mild (2/557, 0.5%) |
| Miciel EL | Brazil | Cross‐sectional study | 416 | NR | NR | Death (0/217, 0%) | Discharge (1/199, 0.5%) |
| Zhang J | China | Retrospective study | 901 | 48.3 | 60.0 (49.0–69.0) | Severe/Critical (9/535, 1.7%) | Common (4/366, 1.1%) |
| Liu J | China | Retrospective study | 1190 | 53.4 | 57 (47–67) | Non‐survivor (5/157, 3.3%) | Survivor (10/1033, 1.4%) |
| Yu HH | China | Retrospective study | 1561 | 50 | 62 (50–70) | Severe (2/365, 0.5%) | Mild (18/1196, 1.5%) |
| Boulle A | South Africa | Cohort study | 22,308 | 31.6 | NR | Deceased (103/625, 16.5%) | Not deceased (2015/21683, 9.3%) |
| Yang C | China | Retrospective study | 104 | 61.5 | 44 (33–55) | Severe/Critical (0/36, 0%) | Moderate (2/68, 2.9%) |
| Nachega JB | Congo | Cohort study | 766 | 65.6 | 46 (34–58) | Severe (4/191, 2.1%) | Non‐severe (15/575, 2.6%) |
| AI Kuwari HM | Qatar | Case series | 5462 | 88.9 | 35.8 ± 1.2 | Severe/Critical (1/117, 0.9%) | Mild (12/5345, 0.2%) |
| Ibrahim OR | Nigeria | Retrospective study | 145 | 86.7 | 43 ± 16.0 | Non‐survivor (1/7, 14.3%) | Survivor (1/138, 2.6%) |
| Dai M | China | Retrospective study | 73 | 59 | 51 ± 13 | Severe (0/26, 0%) | Non‐severe (3/47, 6.4%) |
| Parker A | South Africa | Retrospective study | 113 | 38.9 | 48.5 | Death (6/28, 21.4%) | Survivor (7/85, 8.2%) |
| Lee SG | Korea | Retrospective study | 7339 | 40.1 | 47.1 ± 19.0 | Deceased (4/227, 1.8%) | Survivor (24/7112, 0.3%) |
| Tahtasakal CA | Turkey | Retrospective study | 534 | 56.4 | 59 (19–97) | Severe/Critical (1/136, 0.7%) | Mild/Moderate (1/398, 0.3%) |
| Li S | China | Retrospective study | 2924 | 50.6 | 61.9 (49.7–69.5) | Death (8/257, 3.1%) | Survival (44/2667, 1.6%) |
| Wang W | China | Retrospective study | 146 | 61.2 | 44 (33–50) | Severe (2/24, 8.3%) | Non‐severe (1/122, 0.8%) |
| Yan B | China | Retrospective study | 110 | 53.7 | 59.5 (14–86) | Critical (1/41, 2.4%) | Moderate (0/69, 0%) |
| Zheng B | China | Retrospective study | 198 | 40.4 | 49.5 | Severe (1/36, 2.8%) | Mild (0/162, 0%) |
| Lu Y | China | Retrospective study | 77 | 65 | 59 (54–63) | Non‐survivor (1/40, 2.5%) | Survivor (0/37, 0%) |
| Oh TK | Korea | Cohort study | 7780 | NR | NR | Mortality (OR = 1.65, 95% CI: 0.48 to 5.64) | |
| Bepouka BI | Congo | Retrospective study | 141 | 67.4 | 49.6 ± 16.5 | Non‐survivor (0/41, 0%) | Survivor (1/100, 1%) |
| Yitao Z | China | Retrospective study | 257 | 54 | 46 ± 17 | Deterioration (0/49, 0%) | Non‐deterioration (3/208, 1.4%) |
| Li G | Multi‐country | NR | 399 | 54 | 66 (58–74) | Non‐survivor (3/157, 1.9%) | Survivor (3/242, 1.2%) |
| Mollalo A | USA | NR | NR | NR | NR | Mortality (OR = 0.094, 95% CI: 0.012–0.761) | |
| Mortality (OR = 0.142, 95% CI: 0.026–0.784) | |||||||
| Zhang W | China | Retrospective study | 500 | 53.6 | 40.6 | Critical (1/300, 0.3%) | General (2/200, 1%) |
| Abraha HE | Ethiopia | Retrospective study | 2617 | 63.3 | 29 (24–38) | Severe (0/114, 0%) | Non‐severe (8/2503, 0.3%) |
| Meng M | China | Retrospective study | 413 | 58.8 | 62.6 ± 13.5 | Non‐survivor (5/218, 2.29%) | Survivor (3/195, 1.54%) |
Note: The value of age (years) was presented as mean ± SD or median with interquartile range (IQR).
Abbreviations: CI, confidence interval; ICU, intensive care unit; NR, not clearly reported; OR, odds ratio; TB, tuberculosis; USA, United States of America.
Overall, we found that COVID‐19 patients with tuberculosis tended to have an increased risk for the disease severity compared to those without tuberculosis (OR = 1.56, 95% CI: 1.13–2.16, Figure 1A). When we restricted the outcomes to mortality, the significant association was still present (OR = 1.94, 95% CI: 1.28–2.93, Figure 1B). Leave‐one‐out sensitivity analysis demonstrated that omitting each eligible study once had no obvious impacts on the overall results, which suggests that our results were robust and stable (Figure 1C for severity and 1D for mortality). There was no potential publication bias detected in Begg's test (p = 0.558) or Egger's test (p = 0.293).
Figure 1.
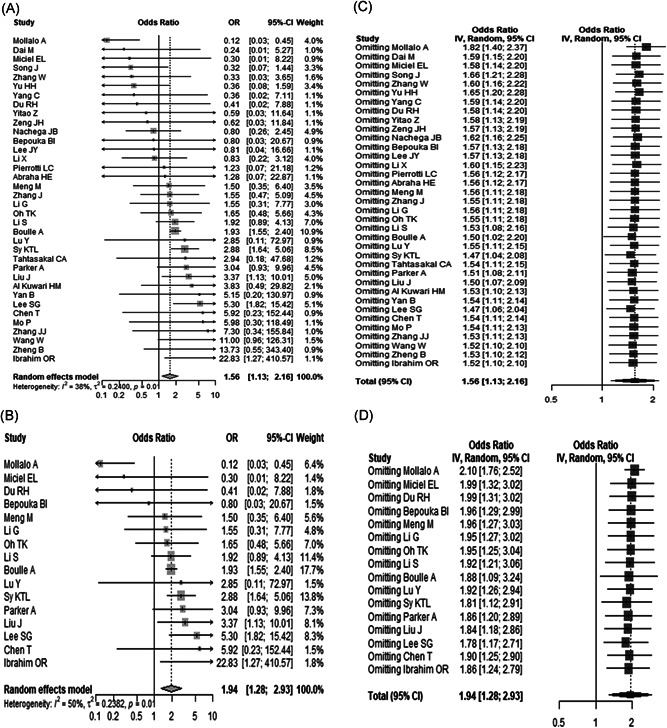
Forest plot indicated that there was a significant association between tuberculosis and the increased risk for severity (A) and mortality (B) among patients with coronavirus disease 2019 (COVID‐19); Leave‐one‐out sensitivity analysis demonstrated that our results were stable and robust ((C) for severity and (D) for mortality). For Mollalo et al.'s study, the combined odds ratio was used
There are several limitations in this current meta‐analysis. First, the majority of the included studies are from Asia, especially from China. Thus, the findings of the present meta‐analysis should be verified by future studies mainly from other regions. Second, the information on medications for tuberculosis is not available presently, thus we could not address the effects of medications on the association between tuberculosis and COVID‐19 severity and mortality. Third, the association between tuberculosis and COVID‐19 severity and mortality was estimated on the basis of crude OR. It is reported that age, gender, and several comorbidities had obvious effects on the clinical outcomes of COVID‐19 patients, 10 , 11 , 12 therefore, a meta‐analysis on this association based on risk factors adjusted‐effect estimates should be performed to verify our findings in the future. Fourth, most of the included studies (n = 25) were retrospectively designed and only one study was prospectively designed. Therefore, well‐designed studies with large sample‐sized prospective articles are warranted to verify our findings in the future when more data are available.
In conclusion, our updated meta‐analysis demonstrated that tuberculosis was significantly associated with an increased risk for severity and mortality among COVID‐19 patients. Thus, several preventive measures should be taken to protect individuals with tuberculosis from SARS‐CoV‐2 infection and more clinical intervention and treatment also should be allocated to COVID‐19 patients with tuberculosis to prevent disease progression. We hope that the updated data will contribute to the more accurate elaboration and substantiation of the findings reported by Gao et al. 1
AUTHOR CONTRIBUTIONS
Yadong Wang, Haiyan Yang, and Huifen Feng designed the study. Yadong Wang, Ruo Feng, Jie Xu, and Hongjie Hou searched articles and extracted the data. Jie Xu, Huifen Feng, and Haiyan Yang analyzed the data. Yadong Wang and Ruo Feng wrote and reviewed the manuscript. All the authors approved the final manuscript.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGEMENTS
We would like to thank Ying Wang, Li Shi, Wenwei Xiao, Xuan Liang, Jian Wu, Peihua Zhang, and Yang Li (All are from the Department of Epidemiology, School of Public Health, Zhengzhou University) for their kind help in searching articles and collecting data, and valuable suggestions for data analysis. This study was supported by grants from the National Natural Science Foundation of China (grant number 81973105), Key Scientific Research Project of Henan Institution of Higher Education (grant number 21A330008) and Joint Construction Project of Henan Medical Science and Technology Research Plan (grant number LHGJ20190679). The funders have no role in the data collection, data analysis, preparation of the manuscript, and decision to submit.
Yadong Wang and Ruo Feng contributed equally to this study.
DATA AVAILABILITY STATEMENT
All data relevant to this study are included in this article.
REFERENCES
- 1. Gao Y, Liu M, Chen Y, Sahi S, Geng J, Tian J. Association between tuberculosis and COVID‐19 severity and mortality: a rapid systematic review and meta‐analysis. J Med Virol. 2021;93(1):194‐196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264‐269. [DOI] [PubMed] [Google Scholar]
- 3. DerSimonian R, Laird N. Meta‐analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327(7414):557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang H, Xu J, Shi L, Duan G, Wang Y. Correspondence on 'Prevalence and clinical outcomes of COVID‐19 in patients with autoimmune diseases: a systematic review and meta‐analysis. Ann Rheum Dis. 2021. 10.1136/annrheumdis-2020-219821 [DOI] [PubMed] [Google Scholar]
- 6. Balduzzi S, Rucker G, Schwarzer G. How to perform a meta‐analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629‐634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088‐1101. [PubMed] [Google Scholar]
- 9. Kang X, Dong L, Yang T, Wang Z, Huang G, Chen X. Clinical and radiographic outcomes of upper thoracic versus lower thoracic upper instrumented vertebrae for adult scoliosis: a meta‐analysis. Brazilian J Med Biol Res [Revista Brasileira De Pesquisas Medicas E Biologicas]. 2018;51(4):e6651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li J, Huang DQ, Zou B, et al. Epidemiology of COVID‐19: a systematic review and meta‐analysis of clinical characteristics, risk factors, and outcomes. J Med Virol. 2021;93(3):1449‐1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Xu J, Xiao W, Liang X, et al. The association of cerebrovascular disease with adverse outcomes in COVID‐19 patients: a meta‐analysis based on adjusted effect estimates. J Stroke Cerebrovasc Diseases. 2020;29(11):105283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liang X, Shi L, Wang Y, et al. The association of hypertension with the severity and mortality of COVID‐19 patients: evidence based on adjusted effect estimates. J Infect. 2020;81(3):e44‐e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to this study are included in this article.


