Abstract
Introduction
COVID‐19 has seen a series of lockdowns and suspension on non‐urgent elective surgeries. Subsequently, there was a drop in the number of diagnostic imaging services billed in April, May, 2020. A survey was undertaken from March to June 2020 to determine the initial impact of COVID‐19 on Australasian Sonographers. This article, the first in a 3‐part series presents and discusses the results of this survey pertaining to changes in the number of scans performed, and changes in the working hours of sonographers. The remaining two articles in this series address other initial COVID‐19 impacts on Australasian Sonographers.
Methods
An online survey was conducted containing questions regarding changes to work hours and examination numbers.
Results
444 participants answered the survey. Seventy eight percent of sonographers reported a decrease in the number of examinations being performed in their department A decrease in work hours was reported by 68% of sonographers with almost a quarter of these reporting that they had lost all their hours. A higher percentage of work hours changes were seenin private practices. Many reductions in work hours were reported to be voluntary.
Conclusion
Scan numbers in ultrasound departments were affected by COVID‐19, as were sonographers' work hours.
Keywords: Australasian, COVID‐19, impact, scan‐numbers, sonographers, workhours
1. INTRODUCTION
The World Health Organisation (WHO) characterised COVID‐19 as a global pandemic on the 11th of March 2020. 1 A pandemic (also known as an epidemic) is defined as the worldwide spread of a new disease over several countries or continents. 2 COVID‐19 carried with it a substantial morbidity and mortality rate, was highly contagious and subsequently spread rapidly. 3 This resulted in worldwide governmental action including social distancing protocols, lockdowns and business and school closures.
Australia adopted an early public health response to COVID‐19 which proved successful in limiting community transmission and preventing the high numbers of acute hospitalisations seen in some countries. The first case of COVID‐19 was reported in Australia on the 25th of January 2020, with the Australian government issuing lockdown restrictions, business closures and school closures beginning March 2020. 4 Coupled with enforced lockdowns, the Australian Government temporarily suspended non‐urgent elective surgeries from the 26th of March 2020 in order to reduce the spread, preserve personal protective equipment (PPE) and allow the health system to prepare for an influx of expected patients. 5
A considerable drop in the Total Medicare Benefits (MBS) scheme service numbers for diagnostic imaging services was seen in April and May 2020 6 with a 30% reduction seen in April and a 19% reduction in May within non‐hospital settings and a 16% and 22% reduction in April and May, respectively, within hospital settings. July 2020 saw both non‐hospital and in‐hospital figures returned to pre‐pandemic levels. 6 .
The Medicare diagnostic imaging data presented in Figure 1 is from Australian only diagnostic imaging data and whilst it incorporates ultrasound procedures, does not capture them individually. New Zealand data was sought but is unavailable. It is unknown whether reductions in patient numbers were due to referrers choosing not to refer, patients choosing not to come or departments choosing not to perform scans. However, it is highly likely that there were impacts to ultrasound patient numbers and subsequently to staff employment. Barnett et al. 7 investigating the effects of lockdowns and suspension of non‐urgent elective surgeries amongst allied health workers in the United States reported that many hospitals laid off allied health employees or reduced their salaries. They also reported that small allied health practices were forced to reduce expenses by decreasing staff hours, reducing salaries, or laying off employees in the face of a large drop in revenue, suggesting that the significant fixed expenses of such practices with a relative lack of access to capital and other sources of liquidity compared to large hospitals made them more susceptible. 7
FIGURE 1.
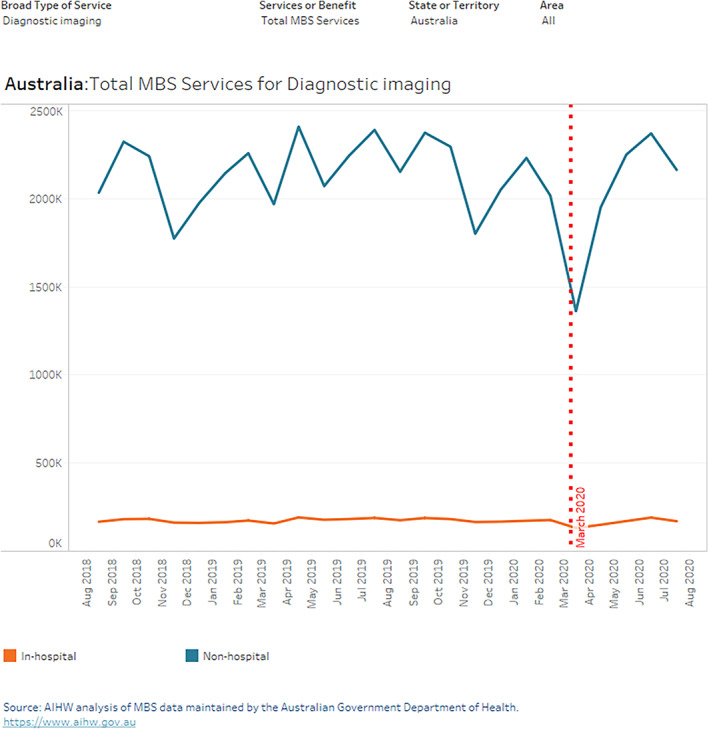
Total MBS benefits paid for Diagnostic imaging services, in‐hospital and non‐hospital, Australia, September 2018 to August 2020. 1 , 6
Whilst there have been many studies conducted into the impact of pandemics on various health care professionals, there are none that focus specifically on the Australian and New Zealand cohort of sonographers. 2 Australian research reports that perceived levels of job insecurity are high, with one in four employed Australians assessing the likelihood of losing their job in the next 12 months being greater than 50%. 8
In the Australasian Sonographic community, the Australasian Sonographers Association (ASA) and the Australian Society for Ultrasound in Medicine (ASUM) are the professional bodies responsible for releasing guidelines and policy and advocating for the sonographic community. In order for these societies to continue to advocate for the sonographic community and inform future policy and guidelines, it is necessary to capture data of the true impact of COVID‐19 on the Australasian Sonographic community. This study captures the initial impact of COVID‐19 on the Australian and New Zealand sonographer population. Data was collected between the eighth of May 2020 and the 14th of June 2020, with respondents asked to reflect on their experiences “since the 11th of March.”
This article is part one of a three‐part series of papers which report the initial impact of COVID‐19 on Australasian sonographers. The purpose of this article is to report the changes in work hours and scan numbers seen within ultrasound departments. The remaining two articles in this series address other initial COVID‐19 impacts on Australasian sonographers.
2. METHODS
Institutional ethics approval was granted prior to the commencement of the study (Protocol number 203084) .
A survey was developed to collect data relating to participant demographics and workplace type (ie, public, private), and to record changes to work hours, scan numbers, and workplace safety protocols. These questions were largely free answer questions, given the uncertain nature of the pandemic and answers expected. Following these questions, the status of the wellbeing and feelings of support in sonographers was captured in a series of Likert scale questions along with free answer responses relating to how well sonographers felt their workplace had dealt with the pandemic. The survey questions were developed and sent to the ASA and ASUM boards for comment and feedback, and subsequently adjusted accordingly.
The survey was distributed as an anonymous internet survey using an online survey tool (Survey Monkey Inc©, San Mateo, California). The survey was designed to be a cross‐ sectional study and capture the initial impact of COVID‐ 19 on the Australasian sonographic community. It was released on the eighth of May 2020 and closed on the 14th of June 2020.
The survey was distributed as an online link via the online newsletters, social media, and websites of the ASA and the ASUM. The members of the ASA were also sent an email from the Chief Executive Officer inviting them to participate. Participants were provided with an information sheet on the first page of the survey and informed that completion of the survey would be taken as consent. At the end of the survey, participants were invited to follow a link to a second Survey Monkey survey where they could provide their email address in order to be contacted to fill out the subsequent rounds of the project and enter to win a gift card. The separate data collection for email addresses allowed for anonymity of the survey round.
2.1. Statistical analysis
Data was extracted from Survey Monkey in html and SPSS files to capture the free text and allow for analysis using SPSS ([Version 23.0. Armonk, NY: IBM Corp]) statistical package, respectively. Descriptive and qualitative analysis was conducted on the free text responses by one of three members of the research team (BO, KL, SM) and then a fourth member of the research team (JC) reviewed the themes of each question. Disagreements were resolved via discussion with the team.
Fishers exact test was used to examine the relationship between the demographics and quantitative survey answers with a level of significance set at 0.05.
3. RESULTS
3.1. Response rate
There was a total of 444 participants who responded to all or part of the survey. A sample of 366 was required to achieve an accuracy of at least ±5% with 95% confidence.
3.2. Demographics
Table 1 shows the participant demographics. The 45‐54‐year age group saw the highest number of participants, making up 31% (n = 139/444) of the respondents. Only 2% (n = 8/444) of participants were in the 18‐24‐year age group and 3% (n = 15/444) in the 65 year + age group, with the remaining age groups making up around 20% each. By far the largest percentage of participants were sonographers with greater than 15 years' experience accounting for almost half of the responses.
TABLE 1.
Participant demographics
| Variable | Category | N (%) |
|---|---|---|
| Age | 18–24 | 8 (2) |
| 25–34 | 89 (20) | |
| 35‐44 | 104 (23) | |
| 45–54 | 139 (31) | |
| 55–64 | 84 (19) | |
| 65+ | 15 (3) | |
| Undisclosed | 5 (1) | |
| Sex | Male | 48 (11) |
| Female | 396 (89) | |
| Other | 0 | |
| Location of residence | ||
| South Australia | 40(9) | |
| New South Wales | 146 (33) | |
| Victoria | 103 (23) | |
| Queensland | 63 (14) | |
| Tasmania | 5 (1) | |
| Western Australia | 37 (8) | |
| Northern Territory | 3 (1) | |
| Australian Capital Territory | 13 (3) | |
| New Zealand | 23 (5) | |
| Varied | 11 (3) | |
| Location work | ||
| Capital City | 282 (64) | |
| Regional Town | 121 (27) | |
| Rural‐remote | 26 (6) | |
| Varied | 15 (3) | |
| Experience | ||
| Student | 43 (10) | |
| <2 years Clinical Experience | 13 (3) | |
| 2–5 years clinical experience | 37 (8) | |
| 6‐10 years clinical experience | 46 (10) | |
| 11‐15 years clinical experience | 57 (13) | |
| Great than 15 years clinical experience | 187 (42) | |
| Not reported | 61 (14) | |
| Position | ||
| Tutor Sonographer | 53 (12) | |
| Senior Sonographer | 127 (29) | |
| Management | 35 (8) | |
| Chief | 46 (10) | |
| Locum | 19 (4) | |
| Workplace | ||
| Public Hospital | 86 (20) | |
| Private Practice | 266 (60) | |
| Nonclinical | 5 (1) | |
| Mixed | 80 (18) | |
| Type of Sonographer | ||
| General | 317 (73) | |
| Vascular | 16 (4) | |
| Obstetric | 38 (9) | |
| Cardiac | 52 (12) | |
| MSK | 10 (2) | |
| Breast | 2 (1) | |
| Work Status | ||
| Full‐time | 235 (54) | |
| Part‐time | 170 (39) | |
| Casual | 31 (7) |
The highest number of respondents were from New South Wales (NSW) comprising 33% (n = 146/444) of respondents, with the Northern Territory (NT) having the lowest representation of less than 1% (n = 3/444). Around 64% (n = 282/444) of the data came from sonographers working in capital cities with around 30% (n = 121/444) from regional towns and the remainder from rural or remote areas (Table 1).
The demographic data of this study was well distributed. Reviewing Australian sonographer participants and their demographics with data from the Australian Sonographers Accreditation Registry (which does not account for New Zealand sonographers) there is a comparable weighting of participants by state, except for Queensland which was slightly under‐represented (Figure 2).
FIGURE 2.
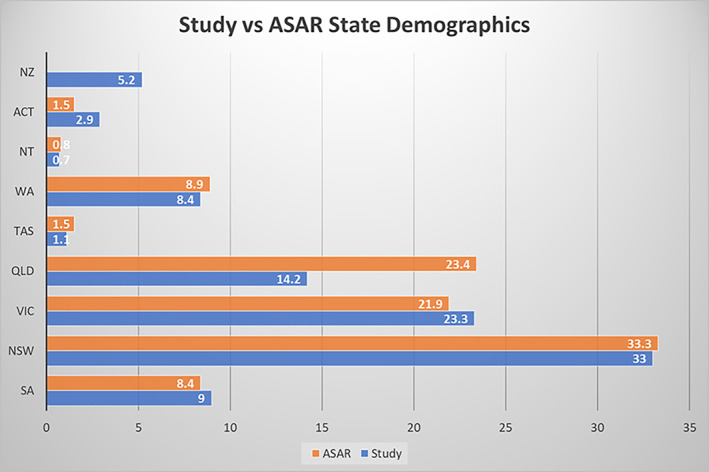
Participant location distribution compared to ASAR data for sonographer state distribution
These results are reflective of changes reported by sonographers between the 11th of March and the 14th of June 2020 comprising the initial stages of COVID‐19. This article discusses the results of the changes in scan numbers and types within departments and changes in work hours as reported by sonographers.
3.3. Change in scan numbers: enforced
Participants were asked whether they had seen a change in scan numbers within their departments and what types of scans they had seen a decrease in, 391 participants answered all or some of this series of questions.
Seventy eight percent (n = 305/391) participants reported they had seen a decrease in the number of scans being performed in their department, with 29% (n = 84/292) of respondents reporting that the decrease was uniform across all scan types. The most noticeable individual drop was seen in musculoskeletal scans with 21% (n = 61/292) of participants reported to have seen a drop in these types of scans, with the next largest reported drop being non urgent scans, outpatient scans and cardiac scans (Figure 3).
FIGURE 3.
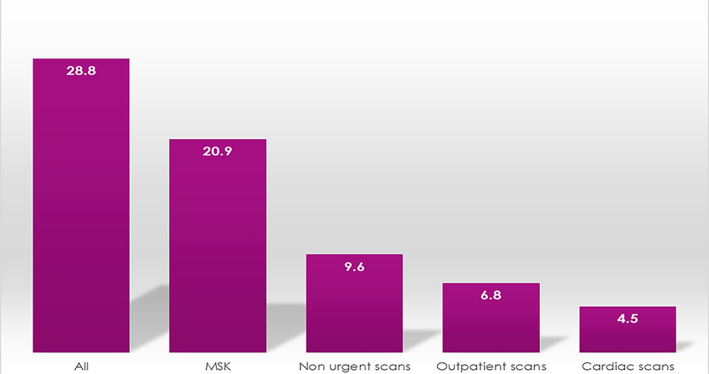
Percentage reported drop in scans by type
There was a statistically significant difference between those working in public hospitals and private practices in the types of scans where reductions were seen (p = <0.001). Those in private practice reported seeing the largest decrease individually in MSK (27%, n = 45/167)) and non‐urgent scans (11%, n = 19/17), whereas public practice saw the biggest individual drop in outpatient scans (18%, n = 12/67), MSK (10%, n = 7/67)) and obstetric scans (8%, n = 5/67).
Only 24/391 participants (6%) reported that scan numbers had increased rather than decreased, the biggest increase overall was seen in obstetrics where 51% (n = 34/67) of those who reported seeing an increase in specific scan types, reported that this increase was in obstetrics. Not surprisingly, given the statistics for scan decreases, the largest increase in obstetrics was seen in private practice (57%, n = 27/47) suggesting that these types of scans were being moved from public hospitals to private practices. Within public hospitals 25% (n = 2/8) of the reported increases were COVID‐19 lung scans, with 0% reported in private practice.
3.4. Change in scan numbers: voluntary
In order to capture whether scan reductions were a result of referrer/patient choice or a result of practice choice, participants were asked which scans (if any) their workplace specifically had made the choice to cease or reduce scanning. Details around the rationale for the response was also collected. There were 144 open ended responses to this question. Table 2 represents a summary of the scan types that were reduced or ceased and number of sonographers who reported this change in their workplace (please note some respondents indicated more than one type of scan). The reasons column provides details on the justification for limiting or ceasing a scan type. Many participants did not give a reason.
TABLE 2.
A summary of the scan types that were reduced or ceased
| Scan | No. | Reasons |
|---|---|---|
| All scans reduced | 4 |
To allow for thorough cleaning between patients To reduce the number of people in the waiting room |
| Only inpatient scans performed | 4 |
Exposing staff/patients to as few people as possible Reduce the number of people in the waiting room Limit contamination by outpatient Increase availability for COVID‐19 patients |
| Only urgent scans performed | 8 |
Minimise community transmission of COVId‐19 Allow department to organise safety protocols Reduce the number of people within the hospital Increase availability for COVID‐19 surge Allow for illness amongst staff Triaging patients reduces amount of people in clinic |
| Screening scans ceased | 2 | Nil |
| Research patients cease | 1 | Nil |
| Long scans assessed on a patient‐by‐patient basis | 1 | Nil |
| Scans without proper clinical information or blood results attached not performed | 1 | Nil |
| Annual review scans ceased | 4 |
Ability to be deferred until later in the year Reduce risk of exposure to staff/patients |
| All scans on patients with any COVID symptoms/suspected of COVID ceased | 4 | Reduce the risk of contracting COVID‐19 |
| All scans on patients with isolation requirements of awaiting COVID‐19 test results ceased | 8 |
Reduce the risk of contracting COVID‐19 |
| All scans on patients with confirmed COVID ceased | 6 | Reduce the risk of contracting COVID‐19 |
| Non urgent gyanecological scans ceased | 2 | Nil |
| Tv scanning ceased | 1 | Reduce exposure to possible faecal contamination |
| Deep infiltrating Endometriosis scans ceased | 2 | Nil |
| Routine obstetrics ceased | 7 |
Expectation that private practice would perform instead Increase availability for COVID‐19 surge Allow for illness amongst staff |
| Pregnancy scans purely for patient reassurance ceased | 1 | Nil |
| Precautionary obstetric scans due to issues in previous pregnancy ceased | 1 | Nil |
| Only obstetric scans that would directly impact patient management performed | 1 | Reduce the number of scans being performed to enable work team to be split in base someone got COVID‐19 |
| Only third trimester scans deemed necessary booked | 1 | Reduce number of people coming into the hospital |
| 3D/4D baby scans ceased | 4 | Nil |
| Prostate biopsies ceased | 1 | Nil |
| Penile doppler scans ceased | 1 | Nil |
| Arterial leg studies ceased | 7 | Length of time for procedure, reduce contact time for sonographer |
| Venous incompetence ceased | 7 |
Reduced contact time Sonographer position relative to patient increases risk of respiratory droplets |
| Bilateral DVT ceased | 2 | Reduce face to face contact time for sonographer |
| Abdominal Doppler ceased | 1 | Reduce face to face contact time for sonographer |
| ? Hernia scans ceased | 1 | Could be performed by Computer Tomography (CT) |
| ? Renal calcification scans ceased | 1 | Could be performed by CT |
| Non urgent breast imaging ceased | 4 |
Increase availability for COVID‐19 surge Allow for illness amongst staff |
| Neck/thyroid/carotid scans ceased | 2 | Droplet precautions |
| Musculoskeletal scans ceased | 1 |
Could be postponed Limit exposure to staff |
| Non‐essential Musculoskeletal scans ceased | 4 |
Redirected to private practice that needed the work Reduced exposure risk as would not alter patient management |
| Interventional procedures reduced | 1 | Nil |
| Interventional procedures ceased | 9 |
Reduce number of people in scanning room Able to be postponed Risk of procedure results in patient hospitalisation Increase availability for COVID‐19 surge No radiologist on site Impact on immunity for some procedures Preserve PPE |
| High risk procedures ceased | 1 | Nil |
| Stress echocardiograms ceased | 6 |
Risk of droplets Reduce time with patient Room re‐purposed as area for possible COVID‐19 patients |
| Stress echocardiograms only performed when essential | 4 | Reduce need for patients to be out in the community |
| Echocardiograms in the elderly and vulnerable people ceased | 1 | Reduce the need for vulnerable patients to be out in the community |
| Echocardiographs whose outcome would not change patient management ceased | 1 | Nil |
| Transoesophageal echocardiograms ceased | 1 | Risk of respiratory transfer of disease |
| Increased threshold put on transthoracic echocardiographs, transoesophageal echocardiogram, and stress echocardiograms | 2 |
Potential aerosolization |
| Stress echocardiograms and transoesophageal echocardiograms scans reduced | 3 | Extra cleaning required due to aerosolization |
Note: Key: No. = Number of sonographers who indicated change.
The largest change was seen where departments made the decision to cease all non‐ urgent scans (22%, n = 31/144), performing only essential ultrasounds. The reasons given included exposing the staff and patient to as few people as possible, to reduce the number of people within a department or hospital and to minimise the risk of community transmitted COVID‐19. Where the aim was to reduce scan numbers rather than specific scan types, there were reports of scans being triaged and booked in order of urgency. Reasons for this were given as allowances for time to increase cleaning, and to reduce the number of patients in a waiting room at any one time.
Cessation of interventional procedures was the second highest reported change (19%, n = 27/144) with participants citing reasons such as radiologists no longer being on site, too many people being required to be in one room to perform the procedures, the potential impact on immunity following cortisone injections and the preservation of personal protective equipment (PPE).
There was a cessation in longer scans such as arterial leg studies and venous incompetence because of the extended amount of patient to sonographer contact time required for these studies. Procedures with high risks of droplets and aerosolization such as stress echocardiograms and trans thoracic echocardiograms were also reported to be ceased in some departments. Understandably many departments chose to cease scanning patients with suspected, confirmed, awaiting test results for or at high risk of having COVID‐19. Many also chose to defer annual surveillance or review scans.
Other notable changes were a reduction in outpatient scans for reasons such as limiting potential contamination, hospital directives and to clear the decks for an influx of COVID‐19 patients.
3.5. Changes in sonographer work hours
Participants were asked to report whether they had experienced an increase or decrease in work hours because of the COVID‐19 pandemic. There were changes in work hours seen with 68% (n = 291/426) of participants reporting that their work hours had decreased during the initial stages of COVID‐19 while only 6% (n = 27/426) reported an increase in work hours. In those who reported a decrease, the mean decrease in hours was 51% and in those who reported that their hours had increased, the mean increase in hours was 37%. The majority who reported a reduction in work hours reported it being between 26% and 50%. However almost a quarter of those who reported a reduction in work hours reported that they had lost all their hours (Figure 4). Only one of the 40 student sonographers who answered this section of the survey reported an increase in hours and 60% (n = 24/40) reported a decrease in hours. Of those students whose reported a decrease in hours 38% (n = 9/24) lost all of their scanning hours, whilst the remaining 15 who reported a reduction in hours reported that reduction being between 5 and 80%. The average reduction was 71%.
FIGURE 4.
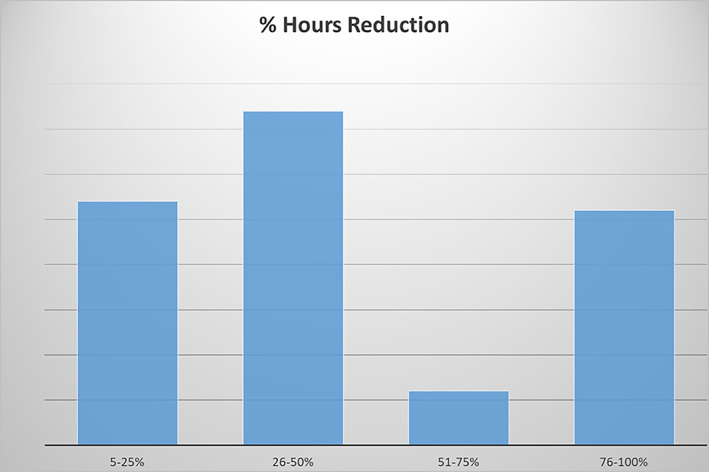
Percentage hours reduction of participants
Of those who reported a reduction in work hours (n = 291), 70% (n = 227/291) reported that this reduction was voluntary with home responsibility or caring duties influencing the decision of 65% of these respondents. There was a statistically significant difference (p = 0.005) with respect to age and whether home responsibility or caring duties influenced their decision. The 18‐24‐year age group was evenly split. Within the 25‐34‐year age group 75% of respondents (n = 12/16) were influenced by responsibility or caring duties whilst 40% (n = 8/20) were influenced in the 34‐44‐year age group. Numbers increased in the older age groups with 56% of 45‐54‐year‐olds (n = 19/34), 93% (n = 14/15) in the 55‐64‐ year age group, and 89% (n = 8/9) in the 65+ age group being influenced by responsibility or caring duties.
Statistically significant differences were seen with regard to work hour changes between sonographers working in the public hospitals and private practice. There was a much higher percentage of sonographers in private practice who reported a change in their work hours with 85% (n = 229/270) of private practice sonographers reporting a change compared to 39% (n = 33/85) in public hospitals (p = <0.001). When looking at the nature of these changes, a decrease in hours was most common within private practices, with 78% (n = 211/271) of private sonographers compared to 22% (19/86) of those working in public hospitals (p = <0.001). Increases in hours were more commonly reported by sonographers in public hospitals (12%, n = 10/86) than sonographers in private practices (5%, n = 13/271). There was a further statistically significant difference (p= 0.029) when looking at the percentage of sonographers who chose to alter their hours, with 47% (n = 15/32) choosing the change in public hospitals compared to 26% (n = 58/225) in private practice.
There was a statistically significant difference (p = 0.034) between locations of those who did and did not choose their change in work hours. Figure 5 shows a comparison by location of those whose work hours changes were voluntary and involuntary. The largest percentage of involuntary change in work hours was seen in New Zealand and the Australian Capital Territory, where just under 50% of hours changes were involuntary. Sonographers in the Northern Territory, Tasmania and Western Australia were seen to have much higher percentages of voluntary change.
FIGURE 5.
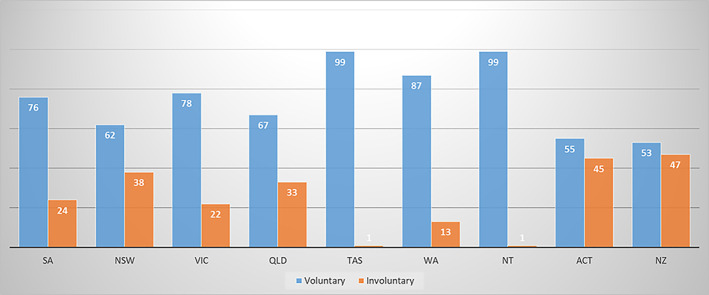
Percentage change of voluntary (blue) versus involuntary (orange) in work hours by location. [Correction added on 3 September July 2021, after first online publication: figure 5 legend color has been corrected to blue]
4. DISCUSSION
This study demonstrates that scan numbers in departments were affected along with corresponding changes to sonographers work hours. Seventy five percent of participants noted a decrease in the number of scans being performed in their department, corresponding to the drop seen in Medicare figures. Interestingly it is noted that a number of these reductions in scan numbers were voluntary with departments making the choice to cease scanning certain types of examinations. Subsequently the corresponding change to sonographer work hours was seen with 68% (n = 291/426) of sonographers reporting they had experienced a reduction in their work hours.
There were large changes in work hours seen, with larger reductions than increases reported. A quarter of participants who reported a reduction stated they had lost all their work hours. A much higher percentage of those whose hours changed was seen in private practice, consisting of 85% (n = 229/270)% of private practice sonographers compared to 39% (n = 33/85) of sonographers working in public hospitals reporting a decrease in hours. Many of those who reported a reduction in work hours stated that this was voluntary, with home and caring responsibility or duties being the main reason. The largest amount of involuntary hours reductions was seen in New Zealand and the Australian Capital Territory, the reasons for this are unknown.
The free text responses reflected the voluntary nature of work hour reductions and the appreciation of sonographers for those employers who let them decide whether to work or not. Free text responses acknowledged the management of some practices who aimed to retain as many jobs as possible by issuing an even spread of work hour reductions across all staff, rather than favouritism of a particular few. The highest number of negative comments in the free text responses with respect to work hours was the voice of the student sonographers, many of whom suffered large reductions due to restrictions on the number of people allowed in scanning rooms. Some students reported the cessation of training positions all together. Increases in hours were reported by only 6% of sonographers and a higher percentage of these worked within public hospitals. Only one student sonographer reported an increase in hours.
Reductions in scan numbers were reported as expected by the MBS diagnostic imaging reductions. Some of these reductions were a result of patient/referrer choice, and some a result of departments choosing to cease certain scans or numbers of scans for various reasons. There was a trend for obstetric scans to be moved from public hospitals to private practice. Potential reasons for this were captured in the free text responses where those who worked in public practice expressed the need to free up space for the anticipated COVID‐19 patient influx, as well as reducing the exposure risk of outpatients to hospital inpatients, through the cessation of scanning non urgent cases. Potentially pregnant women who fell into a high‐risk category for COVID‐19 were the first to be steered away from the public hospitals.
Many departments were seen to cease or reduce all non‐urgent scans to reduce patient exposure to staff, limit the number of people being scanned, or simply to triage patients to enable spacing in the waiting room and department. Interventional procedures were often halted due their non‐urgent nature, and as a result of the number of people required in the scanning room to conduct the procedures.
Limitations of this survey may include the relatively small representation of Tasmania, the Northern Territory and New Zealand, and data specific to these locations should be viewed with caution, however the overall required sample size of the study was met. This survey also did not account for those who worked between public hospitals and private practices who may have found some of the survey questions difficult to answer. Finally, different geographical regions were under different conditions at different times resulting in answers potentially changing across the time span of the survey being open or a prevalence for those who were most impacted to be those who were more likely to respond. The authors acknowledge that New Zealand is a separate country, and the data was analysed as a geographic location along with the states in Australia. All statistically significant differences were reported within the article. The small number of participants from New Zealand reduces the ability for these results to be translated to be representative of all sonographers in the country.
Future surveys will determine whether there has been shifts in employment between private and public practice and whether the return to normal in number of MBS services is reflected. Two future surveys have been scheduled to capture a longitudinal data set; 16 months following the declaration of the pandemic and another after a vaccine for COVID‐19 has been distributed.
The results of the survey regarding protocol changes and sonographer wellbeing can be seen in parts 2 and 3, respectively, of the initial impact of COVID‐19 on Australasian sonographers.
5. CONCLUSION
This survey confirms that the work hours of sonographers were affected in the initial stages of the COVID‐19 pandemic, with a reduction in work hours prominently reported. Sixty eight percent of sonographers overall reported a decrease in work hours and 60% of student sonographers reported a decrease in work hours. Approximately a quarter of qualified sonographers and 38% of student sonographers had all of their work hours cut completely. The average decrease in hours was 51% amongst all sonographers and 71% amongst student sonographers.
The survey also identifies that the number and types of scans performed in ultrasound departments were also affected. Reductions in varying types of scans were seen across private practices and public hospitals with private practices seeing either a uniform reduction in all scans or more individually, musculoskeletal scans, non‐urgent scans and interventional procedures, whilst public hospitals saw a reduction in outpatient scans, musculoskeletal scans and obstetric scans. Future research will involve capturing the impact on sonographers work hours and scan changes over time throughout the pandemic, and after life finds its new normal. These results will assist advocating bodies in future policy development.
CONFLICT OF INTEREST
Jessie Childs is an editorial board member for Sonography and a co‐author on this article. JC was blinded and not involved in the peer review process; management of the peer review process and decision‐making for this article was undertaken by the Editor‐in‐Chief, Kerry Thoirs, acting as Handling Editor. [Correction added on 8 July 2021, after first online publication: Conflict of Interest has been revised]
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Australasian Sonographers Association and the Australasian Society for Ultrasound in Medicine for their assistance in promoting this survey. The authors would like to acknowledge $5000 in funding from the Australasian Sonographers Association.
Childs J, Lamb K, Osborne B, Maranna S, Esterman A. The initial impact of COVID‐19 on Australasian Sonographers Part 1: Changes in scan numbers and sonographer work hours. Sonography. 2021;8:90–99. 10.1002/sono.12263
REFERENCES
- 1. Cucinotta D, Vanellie M. WHO declares COVID‐19 a pandemic. Acta Biomed. 2020;91(1):157–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cabarkapa S, Nadjidai SE, Murgier J, Chee N. The physiological impact of COVID‐19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. BBI Health. 2020;8:100144–100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Piroth L, Cottenet J, Mariet A, et al. Comparison of the characteristics, morbidity and mortality of COVID‐19 and seasonal influenza; a nationalwide, population‐based retrospective cohort study. Lancet Respir Med. 2020;9(3):251–259. 10.1016/S2213-2600(20)30527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Department of Parliamentary Services [homepage on the internet] COVID‐19; a chronology of state and territory government announcements. Parliament of Australia. https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp2021/Chronologies/COVID‐19StateTerritoryGovernmentAnnouncements#_Toc52275794.
- 5. Government Australia [Media Release page on the internet]. Primary minister of Australia 2020 Media release 25 March. https://www.pm.gov.au/media/elective-surgery.
- 6. Australian Government Australian Institute of Health and Welfare (AIHW) [homepage on the internet]. Impacts of COVID‐19 on medicare benefits scheme and pharmaceutical benefits scheme service use report December 17, 2020. https://www.aihw.gov.au/reports/health‐care‐quality‐performance/covid‐impacts‐on‐mbs‐and‐pbs/contents/impact‐on‐mbs‐service‐use.
- 7. Barnett ML, Mehrotra A, Landon BE. Covid‐19 and the upcoming financial crisis in health care. NEJM Catalyst Innov Care Deliv. 2020. 10.1056/CAT.20.0153. [DOI] [Google Scholar]
- 8. Shakespeare‐Finch J, Bowen‐Salter H, Cashin M, et al. COVID‐19: an Australian perspective. J Loss Trauma. 2020;25(8):662–672. [Google Scholar]


