Abstract
Asthma is the most common respiratory disease observed in pregnancy and is estimated to occur in approximately 5–8% of pregnant women. The course of asthma during gestation may be affected by normal physiologic changes associated with the pregnancy, environmental exposures, and adherence to medical therapy. Uncontrolled asthma poses serious risks not only to the mother but also to the fetus. However, if asthma is controlled, then most women have outcomes at or near that of the general population. Appropriate management of asthma during pregnancy includes evaluation of symptoms, regular monitoring of pulmonary function, and patient education with regard to the risks and benefits of medications. Overall, the advantages of treating asthma in pregnancy markedly outweigh any potential risks of standard medical therapies. Comorbid conditions, including allergic rhinitis or vasomotor rhinitis of pregnancy, should also be managed during pregnancy.
An estimated 15% of women of childbearing age reported having had asthma at some point in their lifetime while another 5% reported having had allergic rhinitis and/or hay fever.1 As such, asthma and allergic diseases are frequently encountered during pregnancy, and appropriate management is critical for the well-being of both the mother and the fetus. This article focuses on asthma and allergic rhinitis in pregnancy, whereas maternal risk factors associated with the development of asthma in the offspring are reviewed elsewhere.2,3
NORMAL RESPIRATORY PHYSIOLOGY IN PREGNANCY
Normal physiologic changes during pregnancy affect the respiratory system.2–4 Although the respiratory rate remains relatively unaffected, minute ventilation and tidal volume increase starting in the first trimester. This increase in ventilation is secondary to high levels of progesterone and carotid body sensitivity to hypocarbia and contributes to a compensated respiratory alkalosis. Vital capacity and total lung capacity typically are preserved during pregnancy due to an enlarged chest wall and increased diaphragmatic excursion. In contrast, residual volume and functional residual capacity decrease during gestation, in part, due to elevation of the diaphragm from the enlarging uterus. Functional residual capacity can decrease by 20–30%. Despite these respiratory and anatomic changes, pregnancy has no significant effect on forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), or the ratio of FEV1 to FVC. Peak expiratory flow rates also remain unchanged throughout the majority of pregnancy but can be slightly decreased if measured when the advanced gravida is supine. The fraction of exhaled nitric oxide also does not significantly change in a normal pregnancy.
The physiologic changes observed during pregnancy as well as the upward pressure from the fetus onto the diaphragm can contribute to a sensation of shortness of breath. It is estimated that as many as 75% of women will experience physiologic dyspnea during their pregnancy.4 Symptoms typically are defined as shortness of breath at rest or with mild exertion and are thought to be due to an increased drive to breathe and increased respiratory load. It is important for the clinician to distinguish between physiologic dyspnea and other causes of dyspnea in pregnancy, e.g., asthma.
ASTHMA AND PREGNANCY
Asthma is the most common respiratory disease observed in pregnancy and, in the United States, is estimated to occur in approximately 5–8% of pregnant women.5 In general, asthma is thought to improve in one-third, worsen in one-third, and remain unchanged in one-third of gravidas with asthma.6 Factors that may contribute to worsening asthma are numerous and include exposures to environmental triggers (e.g., respiratory pathogens, allergens, pollutants) and noncompliance with medications. Typically, the more severe the asthma was before pregnancy, the more likely the asthma will be exacerbated during the pregnancy. If asthma medications are continued, then the degree of asthma control should be similar to what was observed in the year preceding the pregnancy. However, if medications are stopped, then asthma of any severity may worsen. Also, the course of asthma during the first pregnancy tends to be similar in successive gestations.
As mentioned above, certain airway mechanics do not significantly change during pregnancy. As such, peak flows, FEV1, and FEV1/FVC should be measured during pregnancy and compared with prepregnancy values to assess asthma control. According to the National Asthma Education and Prevention Program,7 it is recommended that spirometry be completed monthly, but, if this is not possible, then peak flow measurements can be used as a substitute. These values will be decreased during acute asthma exacerbations or with poor asthma control. Fraction of exhaled nitric oxide levels can be elevated in pregnant women with asthma and can correlate with the degree of asthma control. Importantly, given the underlying respiratory alkalosis in pregnancy, a partial pressure of carbon dioxide of >35 mm Hg and a partial pressure of oxygen of <70 mm Hg represents more-severe respiratory compromise in a pregnant woman with asthma versus a nonpregnant woman with asthma.
Just as pregnancy can affect the gravida's asthma, asthma can affect outcomes of the gravida's pregnancy. If the asthma is severe and/or uncontrolled, it can cause detrimental effects not only to the mother but also to the fetus.5 Complications to the mother from uncontrolled asthma may include preterm labor, preeclampsia, antepartum or postpartum hemorrhage, gestational hypertension, placental previa, placental abruption, and an increased need for cesarean delivery. Complications to the fetus may include low birth weight, small for gestational age, congenital malformations, and neonatal death. Most of these outcomes have been attributed to fetal hypoxia, but other factors may also contribute. Prevention and appropriate treatment of acute and severe asthma lead to a decreased risk of adverse events in the gravida. It is imperative that gravidas with asthma be treated appropriately to maintain good asthma control throughout their pregnancy. With effective asthma control, most women have outcomes at or near that of the general population.
MANAGEMENT OF ASTHMA IN PREGNANCY
Medical therapy remains an integral part of treating the gravida with asthma because it can prevent potential complications of pregnancy due to fetal oxygen impairment. However, many pregnant patients are fearful of taking medications due to potential harm to their fetus. Education is vital to ensure an understanding of the disease process, potential complications of uncontrolled asthma, and the safety of medications (Table 1). The advantages of treating asthma in pregnancy markedly outweigh the potential risks of standard medical therapies.6
Table 1.
Appropriate drug therapies during gestation
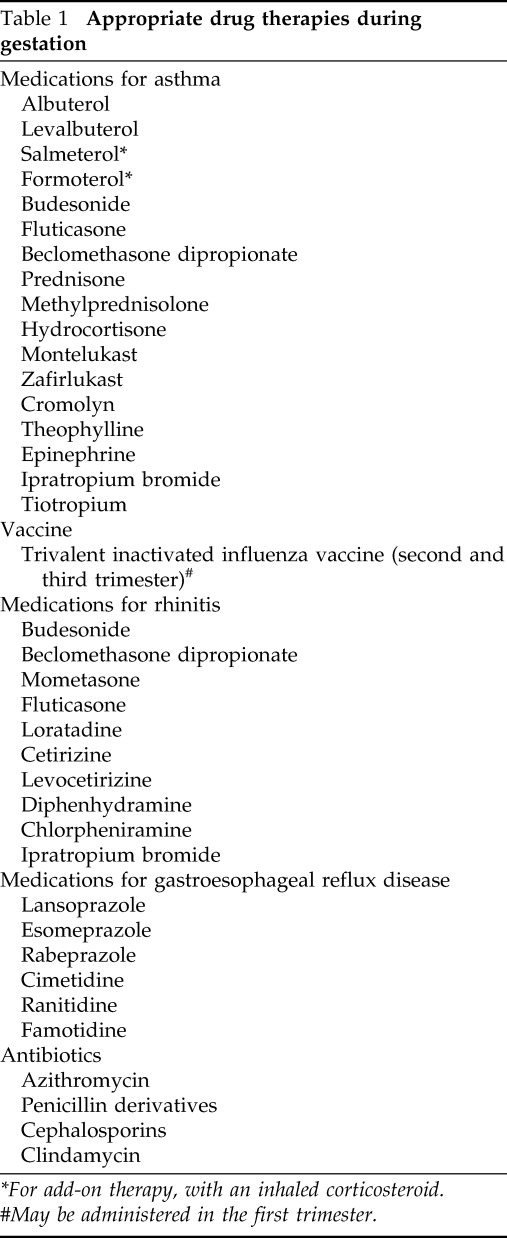
*For add-on therapy, with an inhaled corticosteroid.
#May be administered in the first trimester.
A stepwise approach to treatment according to asthma severity is recommended. Short-acting β2-agonists, e.g., albuterol, are appropriate during pregnancy. Budesonide is the most studied inhaled corticosteroid (ICS) and, therefore, is considered first-line therapy for the gravida with persistent asthma. However, no differences in perinatal safety were observed between inhaled fluticasone and budesonide in a large retrospective study.8 If asthma control is not achieved despite ICS therapy alone, it is recommended to add a long-acting β-agonist, such as salmeterol or formoterol.8 Leukotriene receptor antagonists may also be used because they are considered appropriate in pregnancy, but zileuton should be avoided given animal studies that were not reassuring.
In the past several years, a variety of novel biologic agents have been approved as add-on therapy for patients with uncontrolled moderate-to-severe persistent asthma. Given the risk of anaphylaxis, omalizumab should not be started in pregnancy. However, if previously started, omalizumab may be continued through pregnancy because the risks of congenital abnormalities, low birth weight, and prematurity were reported as similar to other asthma studies in pregnancy.9 At the time of this publication, data from large human clinical trials with regard to the safety of other biologics (e.g., mepolizumab, reslizumab, dupilumab, benralizumab) in pregnancy were insufficient to assess for any drug-associated risks. However, registries have been established to monitor patients who become pregnant while taking these agents.
For patients whose asthma continues to be uncontrolled or for patients with severe acute exacerbations, treatment may require the addition of oral corticosteroids. Acute asthma exacerbations can lead to severe consequences for the fetus; therefore, it is imperative to treat quickly and aggressively because doubling or quadrupling the ICS often is not adequate. During labor and delivery, the goal is that the gravida should have no limitations to vaginal delivery. Fortunately, asthma exacerbations during labor are rare. However, when the gravida has used moderate-to-high dose ICS or systemic corticosteroids during gestation, hydrocortisone 100 mg may be administered intravenously every 8 hours until postpartum, and prednisone may be used before surgery if a cesarean section is planned.2
RHINITIS AND PREGNANCY
It is estimated that as many as 65% of women experience nasal symptoms during their pregnancy.5 As with asthma, control of rhinitis symptoms during pregnancy is variable. In one study, nasal symptoms worsened in 34%, improved in 15%, and remained unchanged in 45% of pregnant women.3 There are several etiologies for rhinitis that should be considered during pregnancy. Nasal symptoms that develop in the second and third trimesters and resolve within 5 days postpartum are most consistent with vasomotor rhinitis of pregnancy. This form of rhinitis is limited to the gestational period and is thought to be secondary to influences of estrogen and progesterone.2 Preexisting allergic rhinitis may also contribute to nasal symptoms during pregnancy and can be exacerbated by environmental exposures.
MANAGEMENT OF RHINITIS IN PREGNANCY
Allergic skin testing is often avoided but is not contraindicated during pregnancy. Analysis of various specific immunoglobulin E (IgE) levels in the peripheral blood may be performed to help evaluate which specific allergens are contributing to symptoms. For patients with an allergic component to their disease, the first step in management is to recommend avoidance of their known allergens. This can be achieved, for example, through purchasing dust mite covers to limit exposure to dust mites, by removing pets from the household, and by exterminating cockroaches in the home. Subcutaneous immunotherapy is not typically initiated during pregnancy but may be continued at the same prepregnancy dose, especially if the patient is already at maintenance dosing.10 As with all therapies, the risks of subcutaneous immunotherapy (including anaphylaxis) must be weighed against the benefits of continuing treatment. In contrast, it is not recommended that sublingual immunotherapy be continued in pregnancy.11
First- or second-generation H1 antihistamines (with the exception of fexofenadine) may be advised to patients with milder nasal symptoms that are inadequately controlled. Intranasal cromolyn may also be used and is regarded as safe. A more-effective strategy for treating allergic rhinitis in pregnancy, however, is intranasal corticosteroids (INS). Although there is a lack of published safety data for INS in pregnant patients, the reassuring data available for ICS use in asthma suggest that INS can be considered for those with moderate-to-severe rhinitis. Some clinicians choose budesonide as the initial agent based on the asthma data, but fluticasone and mometasone can also be considered. In contrast, there is insufficient evidence for the use intranasal H1 antihistamines, e.g., azelastine, in pregnancy. For those patients with vasomotor rhinitis of pregnancy, a buffered saline solution nasal spray may alleviate nasal dryness, and intranasal oxymetazoline can reduce congestion. However, the latter treatment should not be used for > 3 days so to avoid the risk of rebound rhinitis or rhinitis medicamentosa. Oral decongestants such as pseudoephedrine and phenylephrine should be avoided in pregnancy.
OTHER CONSIDERATIONS IN PREGNANCY
Acute and chronic rhinosinusitis treatment is discussed by Kwah and Peters within this issue.12 It is important to inquire about upper airway symptoms during pregnancy because acute rhinosinusitis may aggravate asthma and lead to severe coughing and wheezing. Gastroesophageal reflux disease is another condition that should be evaluated during pregnancy because it also can aggravate asthma symptoms. Lifestyle and diet modifications are the recommended first-line therapy for gastroesophageal reflux disease. However, if symptoms persist, then certain antacids (i.e., those that do not contain sodium bicarbonate or magnesium trisilicate), sucralfate, and H2 antihistamines (ranitidine, cimetidine) may be advised. Proton-pump inhibitors are generally considered safe in pregnancy, with the longest experience being with pantoprazole, lansoprazole, and omeprazole.13
IMMUNOLOGY
The fetus is not rejected during pregnancy in part due to the lack of vascular continuity between the fetus and the mother and to a physical layer of separation provided by the trophoblast.3
The trophoblast does not express major histocompatibility complex class II molecules, which helps to make it resistant to direct recognition by maternal T cells.
Uterine epithelial cells and the trophoblast secrete the immunosuppressive cytokines transforming growth factor β and interleukin 10, which can help prevent rejection of the fetus.
Maternal IgG is the only immunoglobulin subtype transported across the placenta. This is accomplished via the neonatal Fc receptor. All subclasses of IgG are transported, especially IgG1, IgG3, and IgG4.
Maternal IgA is secreted in breast milk and transferred to the infant's gut on breast-feeding.
Pregnant women who are rhesus D negative and who are exposed to fetal rhesus D positive red blood cells are at risk for developing anti-D antibodies. With subsequent pregnancies, there then is an increased risk of developing hemolytic disease of the fetus and the newborn. In mothers who are Rh D−, anti-D immune globulin prophylaxis (e.g., RhoGAM, Kedrion Biopharma Inc., Fort Lee, NJ) is typically administered to reduce the frequency of anti-D antibody development and fetal complications.
CLINICAL PEARLS
The course of asthma may improve, remain the same, or worsen during pregnancy. In gravidas with moderate and severe persistent asthma, frequent monitoring with examinations and pulmonary function should be done.
FEV1, FVC, and FEV1/FVC do not significantly change during pregnancy and can thus be compared with nonpregnant reference values.
The advantages of treating asthma in pregnancy markedly outweigh any potential risks of standard medical therapies. When ICS or ICS plus a long-acting β-agonist are inadequate during exacerbations of asthma, short courses of oral corticosteroids should be administered earlier rather than later.
Asthma should be treated aggressively to prevent complications of pregnancy. If asthma is well controlled during pregnancy, then outcomes can be similar to those of the general population.
Vasomotor rhinitis of pregnancy consists of nasal congestion and vasomotor instability that typically develops in the second and third trimesters, and resolves within 5 days postpartum.
Footnotes
Funded by the Ernest S. Bazley Grant to Northwestern Memorial Hospital and Northwestern University
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Centers for Disease Control and Prevention. Summary health statistics: national health interview survey, 2017. [2019 Mar 19], Philadelphia. Available from: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2015_SHS_Table_A-2.pdf.
- 2. Greenberger PA. Allergic diseases in pregnancy. In: Grammer LC, Greenberger PA, editors. Patterson's allergic disease. 8th ed. Philadelphia: Lippincott Williams & Wilkins, 2018; p. 799–814. [Google Scholar]
- 3. Schatz M, Zeiger RS, Falkoff R, Chambers C, Macy E, Mellon MH. Asthma and allergic diseases during pregnancy. In: Adkinson NF, Jr, Bochner B, Burks AW, Busse WW, Holgate ST, Lemanske RF, et al., editors. Middleton's allergy principles and practice. Philadelphia, PA: Elsevier, 2014; p. 951–969. [Google Scholar]
- 4. Wise RA, Polito AJ, Krishnan V. Respiratory physiologic changes in pregnancy. Immunol Allergy Clin North Am. 2006; 26:1–12. [DOI] [PubMed] [Google Scholar]
- 5. Bonham CA, Patterson KC, Strek ME. Asthma outcomes and management during pregnancy. Chest. 2018; 153:515–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Global Initiative for Asthma. Global strategy for asthma management and prevention-2018 update [cited 2019 Mar 19]. Available from: https://ginasthma.org/wp-content/uploads/2018/04/wms-GINA-2018-report-V1.3-002.pdf.
- 7. National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program Asthma and Pregnancy Working Group. NAEPP expert panel report. Managing asthma during pregnancy: recommendations for pharmacologic treatment-2004 update. J Allergy Clin Immunol. 2005; 115:34–46. [DOI] [PubMed] [Google Scholar]
- 8. Cossette B, Beauchesne MF, Forget A, Lemière C, Larivée P, Rey E, et al. Relative perinatal safety of salmeterol vs formoterol and fluticasone vs budesonide use during pregnancy. Ann Allergy Asthma Immunol. 2014; 112:459–464. [DOI] [PubMed] [Google Scholar]
- 9. Namazy J, Cabana MD, Scheuerle AE, Thorp JM, Jr, Chen H, Carrigan G, et al. The Xolair Pregnancy Registry (EXPECT): the safety of omalizumab use during pregnancy. J Allergy Clin Immunol. 2015; 135:407–412. [DOI] [PubMed] [Google Scholar]
- 10. Cox L, Nelson H, Lockey R, Calabria C, Chacko T, Finegold I, et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol. 2011; 127:S1–S55. [DOI] [PubMed] [Google Scholar]
- 11. Epstein TG, Calabria C, Cox LS, Dreborg S. Current evidence on safety and practical considerations for administration of sublingual allergen immunotherapy (SLIT) in the United States. J Allergy Clin Immunol Pract. 2017; 5:34–40.e2. [DOI] [PubMed] [Google Scholar]
- 12. Kwah JH, Peters AT. Nasal polyps and rhinosinusitis. Allergy Asthma Proc. 2019; 40:380–384. [DOI] [PubMed] [Google Scholar]
- 13. Gill SK, O'Brien L, Einarson TR, Koren G. The safety of proton pump inhibitors (PPIs) in pregnancy: a meta-analysis. Am J Gastroenterol. 2009; 104:1541–1545; quiz 1540, 1546. [DOI] [PubMed] [Google Scholar]


