Abstract
Objectives
The goal of this retrospective cohort study was to investigate the multiple sclerosis-osteoarthritis relationship in adults followed in general practices in Germany.
Methods
Patients aged 18-70 years who were diagnosed for the first time with multiple sclerosis in one of 1,193 general practices in Germany between 2005 and 2018 (index date) were included in this retrospective cohort study. Patients without multiple sclerosis were matched (1:1) to those with multiple sclerosis by sex, age, index year, general practice, obesity, injuries, and other types of arthritis (index date: a randomly selected visit date). The association between multiple sclerosis and the 10-year incidence of osteoarthritis was analyzed using Cox regression models.
Results
There were 4,300 patients with multiple sclerosis and 4,300 patients without multiple sclerosis included in this study. The proportion of women was 69.3% and mean (SD) age was 43.6 (12.6) years. There was no significant association between multiple sclerosis and incident osteoarthritis in the overall sample (HR = 0.95, 95% CI: 0.83-1.09) as well as sex and age subgroups.
Conclusions
Based on these findings, multiple sclerosis is not significantly associated with osteoarthritis. Further studies of longitudinal nature are warranted to corroborate or invalidate these results.
Keywords: Multiple sclerosis, osteoarthritis, retrospective cohort study, epidemiology, Germany
Introduction
Multiple sclerosis is a chronic and autoimmune disease of the central nervous system. 1 Approximatively 2.2 million people are affected by multiple sclerosis in the world. 2 Major advances have been made in the treatment of multiple sclerosis in the past decades, 3 and these therapeutic advances have been associated with a significant decrease in the worldwide mortality rate (-11.5% between 1990 and 2016). 2 In this context, long-term quality of life has become one of the most important aspects of the management of people with multiple sclerosis. 4
Several chronic physical conditions are known to negatively affect quality of life, and one of these conditions is osteoarthritis. 5 Osteoarthritis is a common disorder of the joints characterized by several pathological changes such as degradation of the articular cartilage, synovial inflammation and osteophyte formation. 6 The age-standardized prevalence of osteoarthritis was 3,754 cases per 1,00,000 people in 2017, and the burden associated with this condition is estimated to increase in the next decades. 7 To date, no study has investigated the association between multiple sclerosis and osteoarthritis, although several factors may predispose people with multiple sclerosis to develop osteoarthritis. First, altered gait patterns are frequent in multiple sclerosis,8,9 and some joints of the lower extremity may be overused, potentially increasing the odds of cartilage degradation and osteoarthritis. Second, joint overuse may also involve the upper extremity in patients with severe multiple sclerosis who are using a manual wheelchair. 10 Third, multiple sclerosis is a risk factor for depression 11 and anxiety disorder, 12 and these psychiatric conditions can lead to an increase in the incidence of osteoarthritis.13,14
Therefore, the goal of this retrospective cohort study was to investigate the association between multiple sclerosis and osteoarthritis in a sample of 8,600 adults living in Germany. Given that osteoarthritis affects approximatively one out of five adults in Germany, 15 research identifying risk factors for osteoarthritis in this country should be prioritized.
Materials and methods
Database
Data from the Disease Analyzer database (IQVIA) were used for this study. This database contains demographic, clinical and therapeutical data anonymously collected from general and specialized practices from Germany. 16 In this country, general practices play a crucial role in patient referrals to specialized practices and in the overall management of these patients when specialized evaluation is done. 17 Clinical data were obtained with the German version of the International Classification of Diseases, 10th revision (ICD-10), while the European Pharmaceutical Market Research Association (EPhMRA) Anatomical Therapeutic Chemical Classification (ATC) system was used to compile therapeutical data. A number of criteria such as completeness of documentation or linkage between diagnoses and prescriptions were used to assess the quality of reported data. The sampling method for the Disease Analyzer database relies on statistics from all practices in Germany, and several strata (e.g., age of physician, community size category and region) are used to determine the panel composition of practices included in the database. Finally, it has previously been found that the panel of practices included in the Disease Analyzer database is representative of general and specialized practices in Germany. 16
Study population
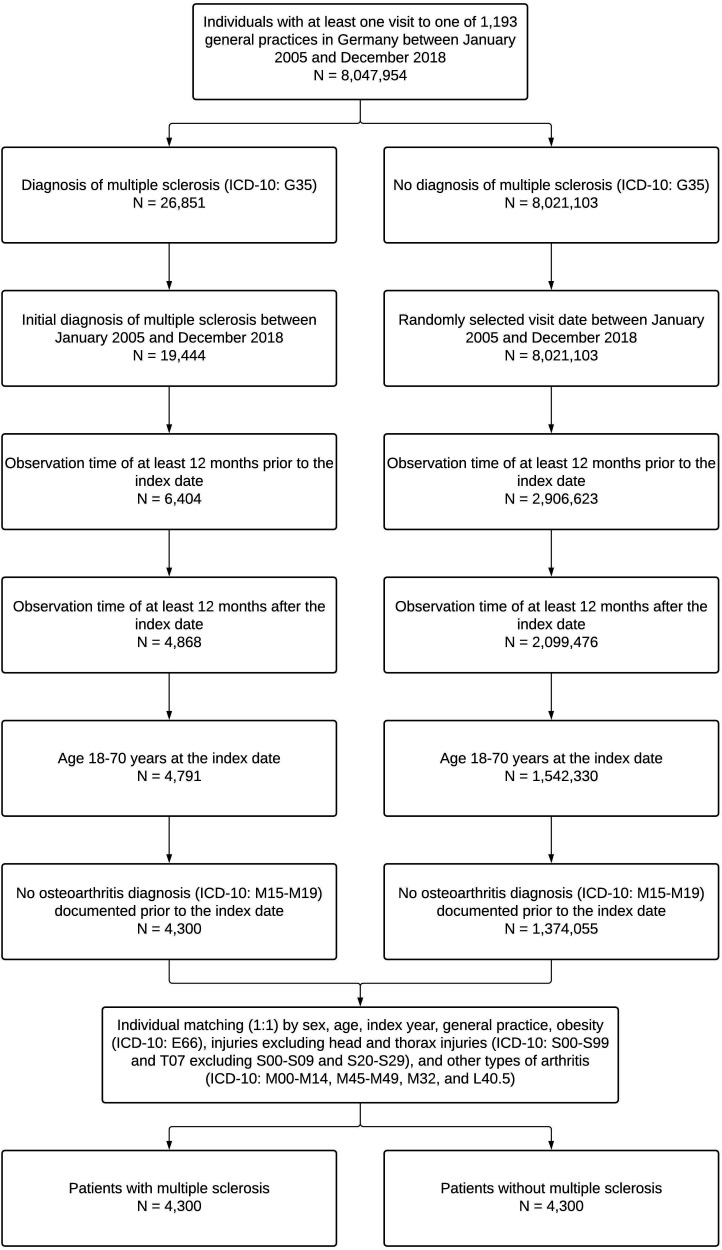
This retrospective cohort study included patients who had received for the first time a confirmed diagnosis of multiple sclerosis (ICD-10: G35) in one of 1,193 general practices in Germany between January 2005 and December 2018 (index date). Inclusion criteria were as follows: observation time of at least 12 months prior to the index date; observation time of at least 12 months after the index date; age 18-70 years at the index date; and no osteoarthritis diagnosis (ICD-10: M15-M19) documented prior to the index date. After applying similar inclusion criteria, individuals without multiple sclerosis were matched (1:1) to those with multiple sclerosis by sex, age, index year, general practice, obesity (ICD-10: E66), injuries excluding head and thorax injuries (ICD-10: S00-S99 and T07 excluding S00-S09 and S20-S29), and other types of arthritis (ICD-10: M00-M14, M45-M49, M32, and L40.5). The index date was a randomly selected visit date for individuals without multiple sclerosis. The selection of study patients is displayed in Figure 1.
Figure 1.
Selection of study patients.
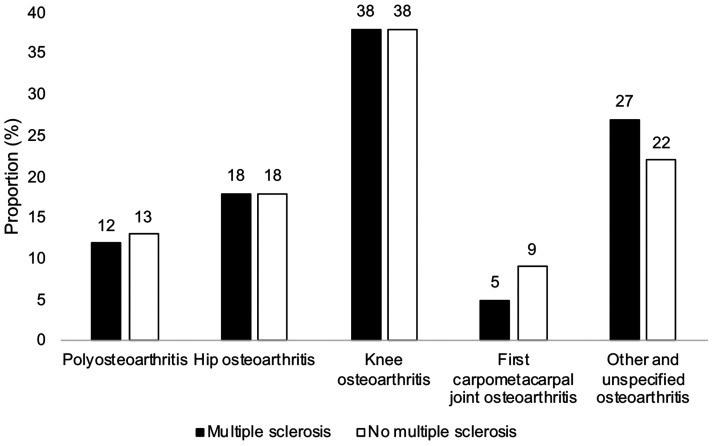
Figure 2.
Distribution of the different types of osteoarthritis in patients with and without multiple sclerosis. There was no significant difference in the distribution of the different types of osteoarthritis between the multiple sclerosis and the no multiple sclerosis group (p-value=0.130).
Study variables
Study variables included osteoarthritis (dependent variable), multiple sclerosis (independent variable), sex, age, obesity, injuries excluding head and thorax injuries, and other types of arthritis. Obesity, injuries and other types of arthritis were documented prior to the index date. All disorders included in this study corresponded to “confirmed diagnoses”, i.e., diagnoses most of the time confirmed by specialists or confirmed at hospital.
Statistical analyses
Baseline characteristics (i.e., sex, age, obesity, injuries excluding head and thorax injuries, and other types of arthritis) were compared between patients with multiple sclerosis and patients without multiple sclerosis using McNemar tests for all variables except continuous age (Wilcoxon signed-rank test). The distribution of the different types of osteoarthritis (i.e., polyosteoarthritis, hip osteoarthritis, knee osteoarthritis, first carpometacarpal joint osteoarthritis, and other and unspecified osteoarthritis) was further compared between the multiple sclerosis and the no multiple sclerosis group using a McNemar test. Finally, the association between multiple sclerosis and the 10-year incidence of osteoarthritis was analyzed in the overall sample and in sex (i.e., female and male) and age subgroups (i.e., 18-30, 31-40, 41-50, 51-60, and 61-70 years) using Cox regression models. Results from the Cox regression analyses are presented as hazard ratios (HRs) and 95% confidence intervals (CIs). P-values < 0.05 were considered statistically significant. All analyses were performed using SAS 9.4.
Results
This retrospective cohort study included 4,300 patients with multiple sclerosis and 4,300 patients without multiple sclerosis. There were 69.3% of women, and mean (standard deviation) age was 43.6 (12.6) years (Table 1). The prevalence of obesity, injuries excluding head and thorax injuries, and other types of arthritis was 7.0%, 16.8%, and 10.2%, respectively. The distribution of the different types of osteoarthritis was not significantly different between the multiple sclerosis and the no multiple sclerosis group (p-value = 0.130), and knee osteoarthritis was the most frequent type of osteoarthritis in both groups (38%) (Figure 2). The results of the Cox regression analyses are displayed in Table 2. There was no significant association between multiple sclerosis and the 10-year incidence of osteoarthritis in the overall sample (HR = 0.95, 95% CI: 0.83-1.09). Similar findings were obtained in sex (i.e., female and male) and age subgroups (i.e., 18-30, 31-40, 41-50, 51-60, and 61-70 years).
Table 1.
Baseline characteristics of study patients after 1:1 matching.
| Variable | Multiple sclerosis (N = 4,300) | No multiple sclerosis (N = 4,300) | P-value |
|---|---|---|---|
| Sex | |||
| Female | 2,980 (69.3) | 2,980 (69.3) | 1.000 |
| Male | 1,320 (30.7) | 1,320 (30.7) | |
| Age (in years) | |||
| Age, mean (standard deviation) | 43.6 (12.6) | 43.6 (12.6) | 1.000 |
| Age 18–30 | 789 (18.4) | 789 (18.4) | 1.000 |
| Age 31–40 | 941 (21.9) | 941 (21.9) | |
| Age 41–50 | 1,237 (28.8) | 1,237 (28.8) | |
| Age 51–60 | 909 (21.1) | 909 (21.1) | |
| Age 61–70 | 424 (9.8) | 424 (9.8) | |
| Comorbidities documented prior to the index date | |||
| Obesity | 301 (7.0) | 301 (7.0) | 1.000 |
| Injuries excluding head and thorax injuries | 722 (16.8) | 722 (16.8) | 1.000 |
| Other types of arthritis | 439 (10.2) | 439 (10.2) | 1.000 |
Note: Data are N (%) unless otherwise specified.
Table 2.
Association between multiple sclerosis and the incidence of osteoarthritis in patients followed in general practices in Germany for up to 10 years.
| Population | Incidence in patients with multiple sclerosis | Incidence in patients without multiple sclerosis | HR (95% CI) | P-value |
|---|---|---|---|---|
| Total | 16.1 | 16.9 | 0.95 (0.83–1.09) | 0.497 |
| Sex | ||||
| Female | 16.5 | 17.3 | 1.00 (0.85–1.18) | 0.992 |
| Male | 15.2 | 15.7 | 0.85 (0.66–1.10) | 0.212 |
| Age (in years) | ||||
| 18–30 | 3.0 | 6.2 | 0.83 (0.43–1.62) | 0.592 |
| 31–40 | 8.5 | 9.7 | 0.86 (0.57–1.28) | 0.450 |
| 41–50 | 16.8 | 17.1 | 0.96 (0.76–1.23) | 0.758 |
| 51–60 | 23.4 | 28.7 | 0.89 (0.70–1.14) | 0.364 |
| 61–70 | 35.7 | 29.3 | 1.03 (0.75–1.39) | 0.877 |
HR: hazard ratio; CI: confidence interval.
Discussion
Main findings
This retrospective cohort study including 8,600 adults from Germany revealed that the 10-year incidence of osteoarthritis was around 16% in those with multiple sclerosis and around 17% in those without multiple sclerosis. The Cox regression analysis further showed that multiple sclerosis was not significantly associated with osteoarthritis in the overall population (HR = 0.95, 95% CI: 0.83-1.09). Similar findings were obtained in the sex and age subgroups.
Interpretation of the findings
To the best of the knowledge of the authors, this is the first study to have analyzed the potential relationship between multiple sclerosis and osteoarthritis. Interestingly, data on the association between multiple sclerosis and other types of arthritis are also relatively scarce. One nationwide cohort study of 11,818 patients found that the incidence of rheumatoid arthritis was significantly higher in those with than in those without multiple sclerosis (adjusted HR = 1.78). 18 It was observed in another study, including 155 patients with multiple sclerosis and 200 controls, that rheumatoid arthritis, psoriasis and goitre were more frequent in the group with than in the group without multiple sclerosis. 19 However, rheumatoid arthritis and osteoarthritis are two joint disorders with very different etiologies. Rheumatoid arthritis is an autoimmune condition affecting synovial joints, 20 whereas osteoarthritis is an age-related disorder potentially affecting all types of joint and likely favored by mechanical stress and low-grade inflammation. 6 Given that multiple sclerosis is also an autoimmune disease, it is not surprising that this neurological condition is associated with rheumatoid arthritis and not osteoarthritis.
The lack of significant association between multiple sclerosis and osteoarthritis in this study conducted in Germany may be explained by several hypotheses. First, it is possible that multiple sclerosis indeed is not a risk factor for osteoarthritis. Although gait patterns are frequently altered8,9 and the use of wheelchair is common in people with multiple sclerosis, 10 levels of physical activity may not be sufficient enough to lead to cartilage destruction and to favor the occurrence of osteoarthritis. For example, a recent systematic review and meta-analysis including 32 studies revealed that the number of steps per day was significantly lower in individuals with than in those without multiple sclerosis (mean difference: -3,845). 21 Second, a significant association may exist between multiple sclerosis and osteoarthritis for more severe forms of multiple sclerosis. Given that this study only included patients followed in general practices and, as patients with a more severe form of the disease are likely to be followed in specialized settings (e.g., neurological practices and hospital settings), this could explain the lack of significant results reported in the present study. Third, there may also be a relationship between multiple sclerosis and radiographic osteoarthritis and not clinical osteoarthritis. Unfortunately, the diagnosis of osteoarthritis relied on ICD-10 codes and not on radiographic data.
Directions for future research
The lack of significant association between multiple sclerosis and the 10-year incidence of osteoarthritis was the main finding of this study. Before drawing any conclusion, further research of longitudinal nature and conducted in other settings is needed to corroborate or invalidate the study results. In addition, more data on multiple sclerosis and osteoarthritis may allow to better understand the potential relationship between these two chronic conditions.
Strengths and limitations
The strengths of this study are the large sample size, the length of follow-up and the use of data obtained in general practices. However, these findings should be interpreted in the light of several limitations. First, there was a lack of data on the severity of multiple sclerosis, although a higher risk for osteoarthritis may exist in patients with severe multiple sclerosis only. Second, more information on osteoarthritis (e.g., clinical symptoms and radiographic abnormalities) would have allowed more detailed analyses. Third, this study included patients followed in general practices from Germany, and the findings may not be generalizable to other settings. Of note, most patients with multiple sclerosis are treated in neurological practices, although some symptomatic medications (e.g., nonsteroidal anti-inflammatory drugs) may be prescribed in general practices. 22 Fourth, patients who visited another practice could not be followed and were considered as lost to follow-up, potentially introducing a bias in the analyses. Fifth, multiple sclerosis is frequently misdiagnosed, 23 and it is possible that the rate of misdiagnosis of multiple sclerosis was substantial in the present study. Sixth, although previous research has showed that the panel of practices included in the Disease Analyzer database accurately represents primary care practices in Germany, 16 it remains possible that the findings of this study may not be generalizable to the German general population.
Conclusions
Overall, there was no significant association between multiple sclerosis and osteoarthritis in this sample of 8,600 patients followed for up to 10 years in general practices in Germany. Before any conclusion is drawn, these results should be corroborated or invalidated by further studies conducted in other settings and other countries.
Footnotes
Conflict of Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical statement: German law allows the use of anonymous electronic medical records for research purposes under certain conditions. According to this legislation, it is not necessary to obtain informed consent from patients or approval from a medical ethics committee for this type of observational study that contains no directly identifiable data. Because patients were only queried as aggregates and no protected health information was available for queries, no IRB approval was required for the use of this database or the completion of this study.
ORCID iDs: Marcel Konrad https://orcid.org/0000-0001-6798-5092
Karel Kostev https://orcid.org/0000-0002-2124-7227
Contributor Information
Louis Jacob, Research and Development Unit, Parc Sanitari Sant Joan de Déu, CIBERSAM, Barcelona, Spain; Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Madrid, Spain; Faculty of Medicine, University of Versailles Saint-Quentin-en-Yvelines, Montigny-le-Bretonneux, France.
Lee Smith, The Cambridge Centre for Sport and Exercise Sciences, Anglia Ruskin University, Cambridge, UK.
Ai Koyanagi, Research and Development Unit, Parc Sanitari Sant Joan de Déu, CIBERSAM, Barcelona, Spain; Institució Catalana de Recerca i Estudis Avançats (ICREA), Barcelona, Spain.
Josep Maria Haro, Research and Development Unit, Parc Sanitari Sant Joan de Déu, CIBERSAM, Barcelona, Spain.
Marcel Konrad, Health & Social, FOM University of Applied Sciences for Economics and Management, Frankfurt am Main, Germany.
Christian Tanislav, Department of Geriatrics and Neurology, Diakonie Hospital Jung Stilling, Siegen, Germany.
Karel Kostev, Epidemiology, IQVIA, Frankfurt, Germany.
References
- 1.Dobson R, Giovannoni G. Multiple sclerosis – a review. Eur J Neurol 2019; 26: 27–40. [DOI] [PubMed] [Google Scholar]
- 2. Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2019; 18: 269–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hauser SL, Cree BAC. Treatment of multiple sclerosis: a review. Am J Med 2020; 133: 1380–1390.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gil-González I, Martín-Rodríguez A, Conrad R, et al. Quality of life in adults with multiple sclerosis: a systematic review. BMJ Open 2020; 10: e041249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vitaloni M, Botto-van Bemden A, Sciortino Contreras RM, et al. Global management of patients with knee osteoarthritis begins with quality of life assessment: a systematic review. BMC Musculoskelet Disord 2019; 20: 493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cucchiarini M, de Girolamo L, Filardo G, et al. Basic science of osteoarthritis. J Exp Orthop 2016; 3: 1--18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Safiri S, Kolahi A-A, Smith E, et al. Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis 2020; 79: 819–828. [DOI] [PubMed] [Google Scholar]
- 8.Kelleher KJ, Spence W, Solomonidis S, et al. The characterisation of gait patterns of people with multiple sclerosis. Disabil Rehabil 2010; 32: 1242–1250. [DOI] [PubMed] [Google Scholar]
- 9.Dujmovic I, Radovanovic S, Martinovic V, et al. Gait pattern in patients with different multiple sclerosis phenotypes. Mult Scler Relat Disord 2017; 13: 13–20. [DOI] [PubMed] [Google Scholar]
- 10.Rankin JW, Kwarciak AM, Mark Richter W, et al. The influence of altering push force effectiveness on upper extremity demand during wheelchair propulsion. J Biomech 2010; 43: 2771–2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fornelos A, Espírito Santo V, Silva M, et al. Association between multiple sclerosis and depression. Eur Psychiatr 2017; 41: S632–S632. [Google Scholar]
- 12.Butler E, Matcham F, Chalder T. A systematic review of anxiety amongst people with multiple sclerosis. Mult Scler Relat Disord 2016; 10: 145–168. [DOI] [PubMed] [Google Scholar]
- 13.Seavey WG, Kurata JH, Cohen RD. Risk factors for incident self-reported arthritis in a 20 year followup of the alameda county study cohort. J Rheumatol 2003; 30: 2103–2111. [PubMed] [Google Scholar]
- 14.Aguilar-Gaxiola S, Loera G, Geraghty EM, et al. Associations between DSM-IV mental disorders and subsequent onset of arthritis. J Psychosom Res 2016; 82: 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fuchs J, Rabenberg M, Scheidt-Nave C. [ Prevalence of selected musculoskeletal conditions in Germany: results of the german health interview and examination survey for adults (DEGS1)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013; 56: 678–686. [DOI] [PubMed] [Google Scholar]
- 16.Rathmann W, Bongaerts B, Carius H-J, et al. Basic characteristics and representativeness of the German disease analyzer database. Int J Clin Pharmacol Ther 2018; 56: 459–466. [PubMed] [Google Scholar]
- 17.Rosemann T, Wensing M, Rueter G, et al. Referrals from general practice to consultants in Germany: if the GP is the initiator, patients’ experiences are more positive. BMC Health Serv Res 2006; 6: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tseng C-C, Chang S-J, Tsai W-C, et al. Increased incidence of rheumatoid arthritis in multiple sclerosis: a nationwide cohort study. Medicine 2016; 95: e3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Midgard R, Grønning M, Riise T, et al. Multiple sclerosis and chronic inflammatory diseases. A case-control study. Acta Neurol Scand 1996; 93: 322–328. [DOI] [PubMed] [Google Scholar]
- 20.Guo Q, Wang Y, Xu D, et al. Rheumatoid arthritis: pathological mechanisms and modern pharmacologic therapies. Bone Res 2018; 6: 1--14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Casey B, Coote S, Galvin R, et al. Objective physical activity levels in people with multiple sclerosis: meta-analysis. Scand J Med Sci Sports 2018; 28: 1960–1969. [DOI] [PubMed] [Google Scholar]
- 22.Höer A, Schiffhorst G, Zimmermann A, et al. Multiple sclerosis in Germany: data analysis of administrative prevalence and healthcare delivery in the statutory health system. BMC Health Serv Res 2014; 14: 381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaisey M, Solomon AJ, Luu M, et al. Incidence of multiple sclerosis misdiagnosis in referrals to two academic centers. Mult Scler Relat Disord 2019; 30: 51–56. [DOI] [PubMed] [Google Scholar]