Abstract
Objectives:
The purpose of this study is to examine the effects of coronavirus disease 2019 pandemic on the prevalence of anxiety, depression, stress, insomnia, and social dysfunction among pregnant and/or lactating women and to measure the global pooled prevalence of mental health effects among these populations in the era of coronavirus disease 2019 pandemic.
Methods:
Comprehensive literature searching was conducted and studies published from 1 January 2020 to 30 September 2020 reporting the prevalence of anxiety, depression; stress, insomnia, and social dysfunctions were included. The pooled prevalence of anxiety, depression, stress, insomnia, and social dysfunctions was estimated using a random-effect model. In this study, all statistical analyses were performed using STATA (version 15) software.
Results:
There were a total of 19 studies included in the meta-analysis, of which 16, 14, 4, 2, and 2 studies were included in computing the pooled prevalence of anxiety, depression, stress, insomnia, and social dysfunction, respectively. The pooled prevalence of anxiety was 33% (95% confidence interval: 50%−61%), with significant heterogeneity between studies (I2 = 99.68%, p = 0.001). The pooled prevalence of depression was 27% (95% confidence interval: 9%−45%), with remarkable heterogeneity between studies (I2 = 99.29%, p = 0.001). Likewise, the pooled prevalence of stress was 56% (95% confidence interval: 30.07%−82.22%), with significant heterogeneity between studies (I2 = 98.8%, p = 0.0001). The pooled prevalence of social dysfunction was 24.3% (95% confidence interval: 13.41%−62.03%), with significant heterogeneity between studies (I2 = 97.5%, p = 0.0001) and finally, the pooled prevalence of insomnia was 33.53% (95% confidence interval: 3.05%−64.0%), with significant heterogeneity between studies (I2 = 99.6%, p = 0.0001).
Conclusions:
In this study, the mental health effects of the COVID-19 pandemic among pregnant and lactating women were found to be significant. Stress was the most common mental health problem in these population groups. Therefore, policymakers and health planners should give great emphasis to addressing maternal mental well-being during and after this global health crisis. Maternal mental health must be one of the international and national public health priority agendas to enhance the well-being of pregnant and lactating women. Besides, giving psychological support to pregnant and lactating women may reduce the long-term negative effects of this pandemic.
Keywords: Mental health, Coronavirus disease 2019, pregnant, lactating women, anxiety, depression, stress, insomnia, social dysfunctions
Introduction
Coronavirus disease 2019 (COVID-19) is a disease caused by a novel coronavirus (2019-nCoV) that was first reported in Wuhan, Hubei Province, China in December. Since then, there have been over 1,203,459 cases of COVID-19 infections worldwide, with 64,754 deaths. 1
COVID-19 has both mental/emotional and social implications for pregnant and postpartum women who have been physically separated from families, relatives, and society all around the world. Understanding the maternal mental health implications of the COVID-19 pandemic is becoming increasingly necessary to best avoid the occurrence of severe mental disorders as a secondary consequence during the postpartum period.2,3
A study conducted in Toronto, Canada, revealed that 29% of individuals had symptoms of posttraumatic stress disorder and 31% had depression during severe acute respiratory syndrome (SARS) outbreak. 4 During the current pandemic, a study was done in China’s Wuhan region reported that 53.8% of respondents were in moderate or severe mental health problems, of which 17% and 29% had moderate to severe depression and anxiety, respectively. 5 During pregnancy and the postpartum period are vulnerable times for mothers themselves to more likely have cognitive and behavioral issues, while psychological distress can have negative consequences for both the mother and the baby. Studies showed that symptoms of anxiety and depression were higher among pregnant women than men during the COVID-19 pandemic.5,6 A study undertaken among prenatal women indicates that “elevated prenatal anxiety and depression symptoms” might increase the risk of postpartum depression as well as prenatal infection and illness rates.7,8 Besides, previous studies revealed that prenatal anxiety and depression can cause changes in physical activity, nutrition, sleep pattern, maternal mood, and fetal health which may increase the risk of miscarriage, preterm birth, lower birth weight, and lower Apgar scores at birth.9–13 Children of mothers who have endured elevated stress are at greater risk of subsequent mental health problems.13–17 Prenatal anxiety and depression are also correlated with changes in brain development and function in infants and children.18–21 These long-lasting psychological and neurological effects underscore the significance of alleviating prenatal discomfort for both pregnant women and their infants. A meta-analysis conducted in the general population reported that the pooled prevalence of depression during the COVID-19 outbreak is 25% (95% confidence interval (CI): 18%–33%) with significant heterogeneity between studies (I2 = 99.60%, p < 0.001). 22
It is also necessary to identify possible resilience factors that can help guard against high prenatal stress. Social reinforcement may minimize the impact of prenatal stress and has been shown to alleviate the effects of prenatal anxiety and depression symptoms of maternal and infant stress response systems. 23 Physical exercise is often correlated with decreased depressive and anxiety symptoms in pregnant women 24 considering the possible negative psychological effects of psychological, health, and financial instability coupled with social exclusion, there is an immediate need to evaluate the prevalence of psychological distress in pregnant women during this pandemic and to establish a protective factor.
To date, there is no systematic study or meta-analysis in the mental health effects of the COVID-19 pandemic in terms of anxiety, depression, stress, insomnia, and social dysfunction in pregnant and lactating women. This systematic review and meta-analysis will focus on a growing array of articles on mental well-being and COVID-19 published after the outbreak of the COVID-19 pandemic in different countries. To provide a more global viewpoint, we conducted a comprehensive systematic review and meta-analysis of available research findings examining anxiety, depression, stress, insomnia, and social instability in pregnant and lactating women during the COVID-19 pandemic.
Methods
Eligibility criteria and search strategies
We followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guideline 25 to prepare the whole document. National surveys, published and unpublished articles were explored from different databases. In addition, the reference lists of included articles were cross-checked to identify articles that were not assessed in the search strings. We sought comprehensive literature research published on PubMed, CINAHL (EBSCOhost), Global Health (CABI), Medline (EBSCOhost), and other sources (Google Scholar and Google) from 01 January 2020 to 30 September 2020 that reported prevalence of anxiety, depression; stress, insomnia, and social dysfunctions. Studies conducted among pregnant and lactating women to validate the psychological consequences of COVID-19 have been included in this systematic review and meta-analysis.
Inclusion and exclusion criteria
The inclusion criteria in this meta-analysis were as follows: (1) population (pregnant women, lactating women, breastfeeding women, women in antenatal care, and puerperal women); (2) exposure (novel coronavirus, COVID-19, nCoV, severe acute respiratory syndrome coronavirus 2, and SARS-CoV-2); (3) outcome (impact, effect, mental health, psychology, anxiety, depression, stress, and social dysfunction); (4) study design (cohort studies, cross-sectional studies, epidemiology, and observational studies); (5) study setting (community-based surveys, health institutions, and Web-based surveys). The data from each study were verified for eligibility using study area, study setups, assessment methods, study designs, title, abstract, and full texts.
Eventually, observational studies reporting the magnitude of different forms of psychological disorders among pregnant or lactating women were included.
Exclusion criteria: (a) the same patients were enrolled in different articles; (b) commentaries, editorials, case reports, letters, and family-based studies; and (c) short communications.
Nonetheless, studies with incomplete or unclear diagnostic methods and without full texts were excluded. Letters to editors, conference proceedings, and qualitative studies were also excluded. The EndNote X8 reference manager was used to manage articles.
The appropriateness of the key terms was checked prior to conducting searches in each database. Example of search string in PubMed: ((“Psychology”(Mesh) OR (“Mental Health”(Mesh) OR (“Anxiety”(Mesh) OR (“Depression”(Mesh)) OR “Depression, Postpartum”(Mesh) OR (“well-being”) OR (“social instability”) OR (“Stress, Psychological”(Mesh) AND (“COVID-19” (Supplementary Concept))) OR (“severe acute respiratory syndrome coronavirus 2” (Supplementary Concept))) OR (novel coronavirus)) OR (nCoV)) AND (“Pregnant Women”(Mesh) OR (prenatal)) OR (perinatal)) OR (postpartum)) OR (antenatal)) OR (postnatal)) OR (puerperal)) OR (peurperal)) OR (lactating women) Journal Article, Observational Study, in the last 1 year, Humans, English, Adult: 19–44 years.
Data extraction process
A standardized data extraction checklist was prepared using Microsoft Excel 2016, and the data were extracted by two investigators (Z.W.B. and D.B.D.), independently. Name of the author(s), publication year, study country, sample size, study population, diagnostic methods, anxiety, depression, stress, insomnia, and social dysfunction were used in the extraction process. There were no discrepancies between ZWB and DBD on the inclusion of studies. The extracted data were cross-checked interchangeably by the two authors and inconsistencies were solved accordingly.
Quality assessment of studies
Critical appraisal of the included studies was performed by two authors (Z.W.B. and D.B.D.), independently using Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Observational Studies was used for quality assessment. 26 The scores were added up and changed to percentages. The minimum score was 0 and 8 was the maximum one since all included studies were cross-sectional studies. Articles with >50% quality scores were included in this systematic review and meta-analysis (Supplemental Table 2). The inter-rater agreement was computed by an author (ZWB) before the decision of inclusion in this study was made. We computed inter-rater agreement using Cohen’s kappa coefficient (κ). The findings revealed that there were substantial agreement 27 between the two raters (κ = 0.652, p ⩽ 0.001).
Summary measures
The primary outcome of this research was to determine the mental health consequences of the COVID-19 pandemic in pregnant and lactating women using various diagnostic methods. The pooled prevalence was computed for depression, anxiety, stress, insomnia, and social dysfunction. Subgroup analyses were also done using diagnostic methods and the country where the original studies were performed. The prevalence was calculated by dividing the total number of mental disorders by the total sample size and multiplying it by 100. The binomial distribution formula was used to compute the standard error for each original study. The pooled estimates of depression, anxiety, and stress were computed using “meta pop” using a sample size as a weight (wgt) variable. This was done due to significant variability in the sample size of the included studies. The pooled estimates were presented with their 95% CIs. The effect sizes were prevalence of each component of mental disorders.
All studies measured anxiety using standardized scales, the most common being the Generalized Anxiety Disorder 7-item (GAD-7) scale and Hospital Anxiety and Depression Scale (HADS). Similarly, all studies measured depression among pregnant and lactating women using standardized scales, the most common being the Edinburgh Postnatal Depression Scale (EPDS) and HADS. Stress was also assessed based on the Perceived Stress Scale (PSS), while insomnia and social dysfunction were diagnosed based on standardized self-rating scale, respectively.
Statistical methods and analysis
The pooled estimates were calculated using STATA Version 15 (STATA Corporation, College Station, Texas) software in this meta-analysis. Both random- and fixed-impact methods were used to measure the pooled estimates. The pooled estimates were computed using random-effects models and weighted using the inverse variance method in the presence of high heterogeneity among studies. Subgroup analyses were done using different parameters (diagnostic methods and study country). We verified the appropriateness of each datum before the analysis of each datum. Forest plots, summary tables, and texts were used to present the findings of this study.
Publication bias and heterogeneity
The funnel plot Sterne and Egger’s 28 regression test were used to measure publication bias at a 5% significant level. In addition, heterogeneities among studies used to compute the pooled estimates in this meta-analysis were explored using forest plot, I2 test, and the Cochrane Q statistics. 29 The I2 values of 25%, 50%, and 75% were interpreted as low, medium, and high heterogeneity, respectively. 30 In the current meta-analysis, significant heterogeneity was considered when the I2 value was ⩾50%, with a p value < 0.05. The possible sources of significant heterogeneity were addressed through sub-group and sensitivity analyses.
Results
Selection of studies
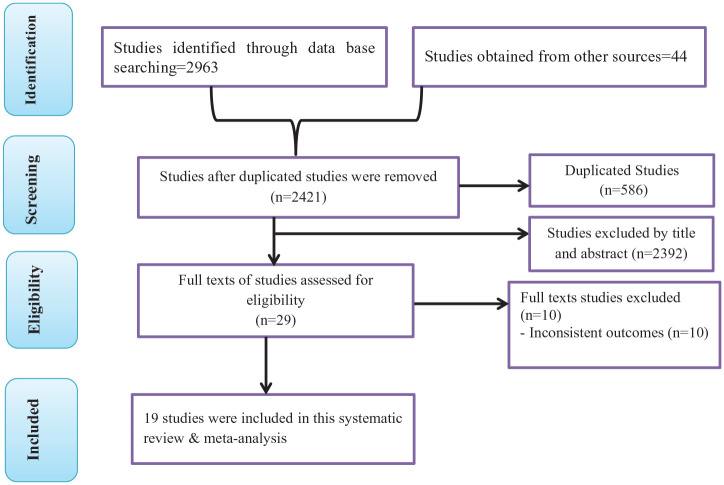
In the initial search, 3007 studies were obtained from databases and gray literature sources. Primarily, 586 studies were excluded due to duplication. Then, 2392 studies were screened using titles and abstracts and 2421 were removed. Finally, the full texts of 29 studies were assessed for eligibility. Of the total 29 studies, 10 were excluded due to inconsistency of results.31–40 Eventually, 19 eligible studies were used in the final analysis of the current systematic review and meta-analysis41–59 (Figure 1).
Figure 1.
PRISMA flow chart showing study selection process.
Study characteristics
Of total of 19 studies included in the final analysis, four studies were done in Canada,42,47,52,57 three studies in China,48,50,56 two in Iran,41,45 six in European countries (Belgium, 55 United Kingdom, 44 Turkey, 58 Ireland, 51 Bosnia and Herzegovina and Serbia, 46 and Italy 49 ), and the rest were conducted in the United States, 59 Colombia, 53 and Sri Lanka. 54 All studies were cross-sectional studies and critical appraisal of cross-sectional studies conducted revealed that about 95% of studies scored more than 75%, only one scored lowest scored 62.5%. The majority of the studies were conducted among pregnant women alone, except studies done in United States, 59 Belgium, 55 and Iran 45 were conducted in both pregnant and lactating women (Table 1).
Table 1.
Detailed description of the included studies for computing the prevalence of stress, anxiety, depression, and social dysfunctions among pregnant women and lactating women 2020.
| Author | Study pop | Study area | Sample size | Diagnostic method | Anxiety | Depression | Stress | Insomnia | Social dysfunction | Quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Parra-Saavedra et al. 53 | PW | Colombia | 946 | SAQ | 50.4 | 25 | 49.1 | 6/8 (75%) | ||
| Patabendige et al. 54 | PW | Sri Lanka | 257 | HADS | 17.5 | 19.5 | 28.4 | 6/8 (75%) | ||
| Ceulemans et al. 55 | PW | Belgium | 2421 | EDS & GAD-7 | 42.6 | 25.3 | 5/8 (62.5%) | |||
| Ceulemans et al. 55 | LW | Belgium | 3445 | EDS & GAD-7 | 42.4 | 23.6 | 8/8 (100%) | |||
| Liu et al. 50 | PW | China | 1947 | SAS | 17.15 | 8/8 (100%) | ||||
| Lebel et al. 57 | PW | Canada | 1987 | EDPS | 59 | 37 | 6/8 (75%) | |||
| Gharagozloo et al. 45 | LW & PW | Iran | 403 | CDAS | 5.7 | 5.5 | 8/8 (100%) | |||
| Durankuş and Aksu 58 | PW | Turkey | 260 | EPDS | 35.4 | 6/8 (75%) | ||||
| Dib et al. 44 | PW | The United Kingdom | 1329 | SAQ | 71 | 18 | 6/8 (75%) | |||
| Tutnjević and Lakić 46 | PW | Bosnia and Herzegovina and Serbia | 152 | SAS | 44.1 | 38.2 | 6/8 (75%) | |||
| Alijanpour et al. 41 | PW | Iran | 261 | HADS and CDAS | 10.29 | 11.3 | 8/8 (100%) | |||
| Milne et al. 51 | PW | Ireland | 70 | SAQ | 14 | 44 | 8/8 (100%) | |||
| Wu et al. 48 | PW | China | 4124 | EPDS | 34.2 | 8/8 (100%) | ||||
| Farewell et al. 59 | PW & LW | The United States | 27 | PHQ-2 & GAD-7 | 60 | 12 | 88 | 8/8 (100%) | ||
| Berthelot et al. 47 | PW | Canada | 1754 | EPDS | 10.9 | 6 | 6/8 (75%) | |||
| Saccone et al. 49 | PW | Italy | 100 | STAI | 68 | 7/8 (87.5%) | ||||
| Davenport et al. 52 | PW | Canada | 900 | EPDS & STAI | 72 | 40.7 | 8/8 (100%) | |||
| Yue et al. 56 | PW | China | 308 | SAS | 14.3 | 6/8 (75%) | ||||
| Cameron et al. 42 | LW | Canada | 641 | CESD & AMHDC. | 36.27 | 33.16 | 6/8 (75%) | |||
| Chen et al. 43 | PW | China | 1160 | SAS & SDS | 10.34 | 28.62 | 6/8 (75%) |
HADS: Hospital Anxiety and Depression Scale; GAD: generalized anxiety disorder; SAS: Self-Rating Anxiety Scale; EPDS: Edinburgh Postnatal Depression Scale; PHQ: Patient Health Questionnaire; SDS: Self-Rating Depression Scale.
Keynotes.
BDI-I = Beck Depression Inventory—I.
CES-D = Center for Epidemiological Studies—depression.
DASS-21 = Depression, Anxiety, and Stress scales.
EPDS = Edinburgh Postnatal Depression Scale.
GAD-7 = Generalized Anxiety Disorder 7-items.
HADS = Hospital Anxiety and Depression Scale.
PHQ-9 = Patient Health Questionnaire.
PSS = Perceived Stress Scale.
SAS = Self-Rating Anxiety Scale.
SDS = Self-Rating Depression Scale.
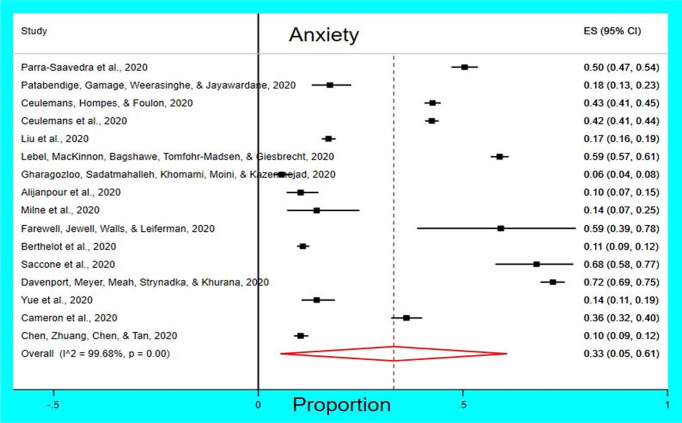
Prevalence of anxiety among pregnant and lactating women
A total of 16 studies were used to compute the pooled prevalence of anxiety among pregnant and lactating women.41–43,45,47,49–57,59 A total of 16 627 pregnant and lactating women were used to compute the pooled estimate of anxiety, 33 cases per 100 pregnant and lactating women (95% CI: 50%–61%) using the DerSimonian and Laird random-effects model (I2 = 99.68%, p = 0.001; Figure 2).
Figure 2.
Forest plot showing the pooled prevalence of anxiety per 100 pregnant and lactating Women.
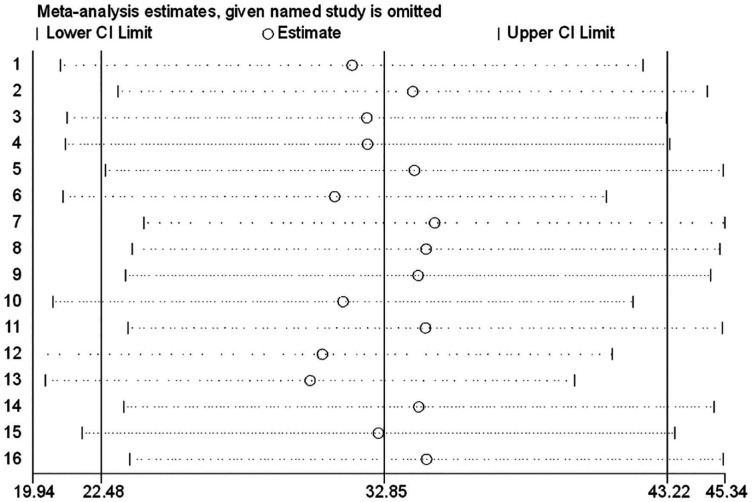
Publication bias was checked using funnel plot, and it was objectively verified using Egger’s regression test. Hence, the funnel plot seems asymmetric despite the Egger’s regression test (p = 0.098) did not confirm the asymmetry of funnel plot (Figure 3). The funnel plots report an upward pattern with no point falling within the predicted 95% CI for anxiety. Sensitivity analysis was also performed to identify the possible source of heterogeneity among the included studies. However, there was no single study having a remarkable effect on the heterogeneity of the pooled estimate (Figure 4). Finally, the funnel plots look asymmetric for anxiety (see Figure 3) which is congruency with Rosenthal’s method of finding of fail-safe-N analysis warrants acknowledgment of possible publication bias within the article, which revealed that the current existed body of literature.
Figure 3.
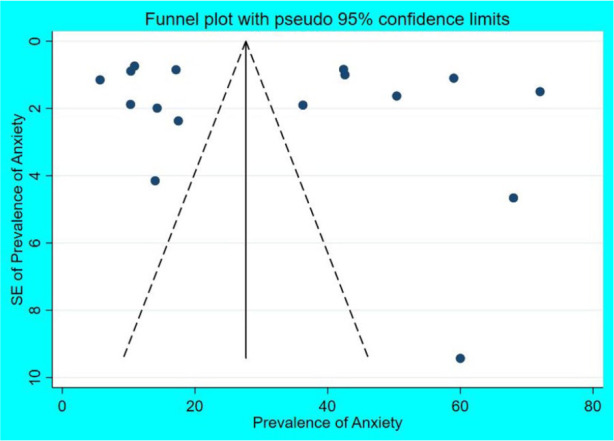
Funnel plot showing the distribution of included studies for prevalence of anxiety among pregnant and lactating women.
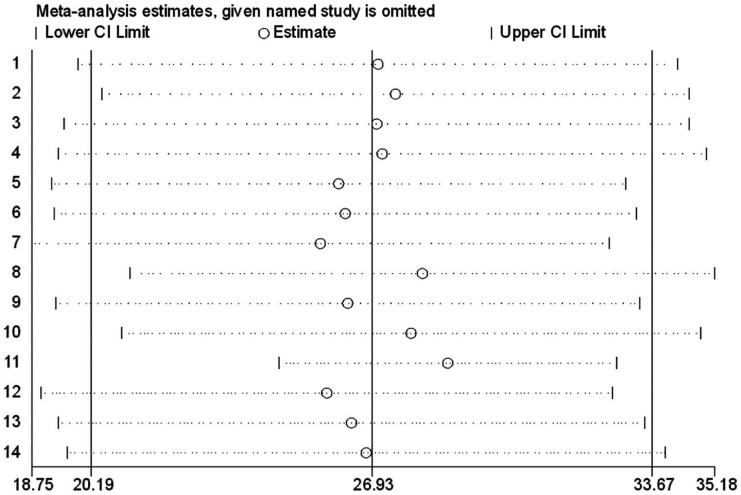
Figure 4.
Sensitivity analysis of studies used to compute pooled prevalence of anxiety.
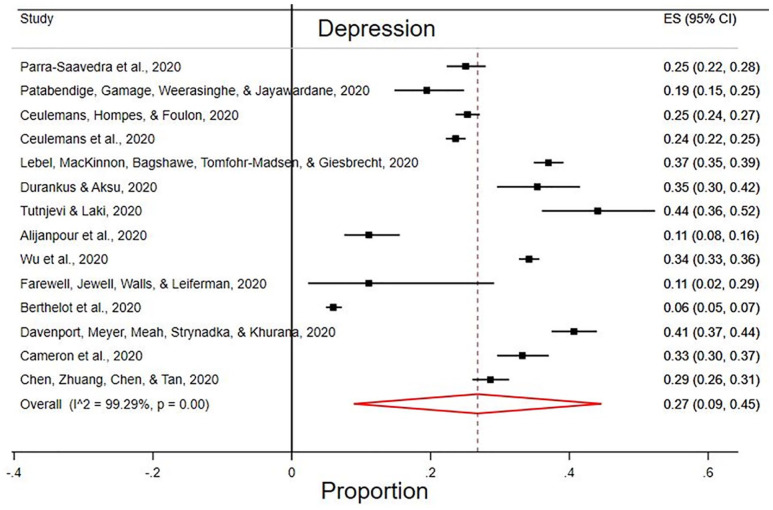
Prevalence of depression among pregnant and lactating women
A total of 18,335 pregnant and lactating women from 14 studies were used to compute the pooled prevalence of depression41–43,46–48,52–55,57–59 was 27% (95% CI: 9%, 45%) by using the DerSimonian and Laird random-effects model (I2 = 99.29%, p = 0.001) (Figure 5).
Figure 5.
Forest plot showing the pooled prevalence of depression among pregnant and lactating women in the era of COVID-19.
The possible source of higher heterogeneity among the included studies was identified using funnel plot and Egger’s regression test. Thus, the funnel plot pinpointed that no publication bias, which was confirmed by an objective test (Egger’s test, p = 0.208; Figure 6).
Figure 6.
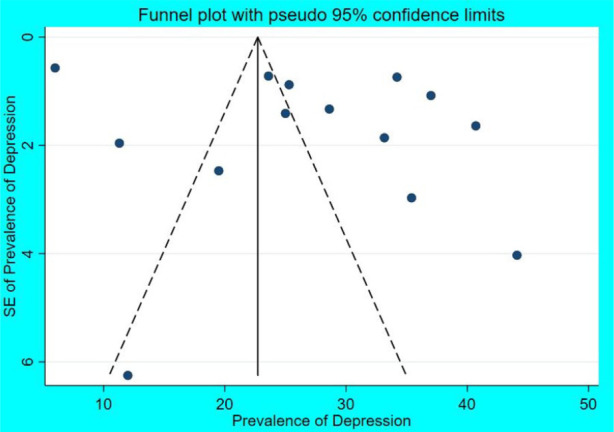
Funnel plot showing the distribution of included studies for prevalence of depression among pregnant and lactating women.
Finally, sensitivity analysis was done to identify the possible source of heterogeneity among the studies used in the pooled estimates. The figure showed that all studies contributed to the higher heterogeneity in the pooled prevalence of depression among pregnant and lactating women (Figure 7).
Figure 7.
Sensitivity analysis of studies used to compute pooled prevalence of depression.
The funnel plots report a rightward shift with very few points falling within the predicted 95%CI for depression (Figure 6). But an objective test (Egger’s test, p = 0.208) for depression confirmed that no publication bias. Finally, the funnel plots look asymmetric for depression (see Figure 2) which is congruency with Rosenthal’s method of finding of fail-safe-N analysis warrants acknowledgment of possible publication bias within the article, which revealed that the current existed body of literature.
Prevalence of stress, insomnia, and social dysfunction among pregnant and lactating women
Out of four eligible studies, a total of 1765 pregnant and lactating women were used to compute the pooled estimate of stress.44,46,54,59 The pooled prevalence of stress was 56% (95% CI: 30.07%–82.2%) using the DerSimonian and Laird random-effects model (I2 = 98.8%, p = 0.0001). Similarly, the pooled prevalence of insomnia was computed from two eligible articles with a total of 2275 study subjects.44,53 Thus, 34% (95% CI: 3.05%–64.0%) of pregnant and lactating women were found to have insomnia in the DerSimonian and Laird random-effects model (I2 = 99.6%, p = 0.0001). Besides, the pooled prevalence of social dysfunction among pregnant and lactating women was estimated from two eligible studies with a total sample of 473.45,51 The pooled prevalence of social dysfunction was found to be 24.3% (95% CI: 13.41%–62.03%) using the DerSimonian and Laird random-effects model (I2 = 97.5%, p = 0.0001).
Subgroup analysis based on country and diagnostic methods was not found plausible result due to scant reports in each diagnostic method. The performed subgroup analysis based on country and diagnostic methods with null results for anxiety and depression.
Discussion
In this meta-analysis, 16 studies were used to compute the pooled prevalence of anxiety among pregnant and lactating women during the COVID-19 outbreak is 33% (95% CI: 50%–61%) with high heterogeneity between studies (I2 = 99.68%, p = 0.001). Sensitivity analysis was also performed to identify the possible source of heterogeneity among the included studies. However, there was no single study having a remarkable effect on the heterogeneity of the pooled estimate. This suggested that the source of this high heterogeneity in the prevalence rates of anxiety among the studies included in this meta-analysis was maybe the scale used for its diagnoses, with the highest prevalence rates in studies used the Anxiety GAD-7 scale and HADS and the lowest in those using the PHQ-9 and Self-Rating Anxiety Scale. This may be due to the use of self-reported online survey data may imply the presence of social desirability bias. This pooled prevalence is higher than a study done in China’s Wuhan region reported that 29% anxiety symptoms. 5 This difference may be due to present pooled prevalence and pregnant women during the COVID-19 pandemic may be particularly affected, prolonged, increased prenatal anxiety symptoms increase the risk of prenatal infection and illness rates.7,8
The current meta-analysis of 14 studies revealed that the pooled prevalence of depression among pregnant and lactating women during the COVID-19 outbreak is 27% (95% CI: 9%–45%) with heterogeneity between studies (I2 = 99.29%, p = 0.001), which is higher than the pooled prevalence in the general population 25% (95% CI: 18%–33%). 59 This difference may be due to study population difference, this study among pregnant and lactating women and pregnant women in particular, prolonged, intensified prenatal depression symptoms may raise the risk of postpartum depression, as well as prenatal infection and disease rates during the COVID-19 pandemic.7,8
On the present meta-analysis, the possible source of higher heterogeneity among the included studies was identified using funnel plot and Egger’s regression test. Thus, the funnel plot pinpointed that no publication bias, which was confirmed by an objective test (Egger’s test, p = 0.208). Finally, sensitivity analysis was done to identify the possible source of heterogeneity among the studies used in the pooled estimates. The figure showed that all studies contributed to the higher heterogeneity in the pooled prevalence of depression among pregnant and lactating women. This suggested that the source of this high heterogeneity in the prevalence rates of depression among the studies included in this meta-analysis was maybe the scales used for its diagnoses, with the highest prevalence rates in studies used the EPDS scale and HADS and the lowest in those using the CES-D (Center for Epidemiological Studies—depression and Self-Rating Depression Scale. This may be due to the use of self-reported online survey data may suggest the presence of social desirability bias.
Out of four eligible studies, a total of 1765 pregnant and lactating women were used to compute the pooled estimate of stress.44,46,54,59 The pooled prevalence of stress was 56% (95% CI: 30.07%–82.2%) with heterogeneity between studies (I2 = 98.8%, p = 0.0001). The pooled prevalence of stress among pregnant and lactating women is the highest of all psychological impact of COVID 19 among these populations as identified in this meta-analysis which the pooled prevalence of anxiety 33%, depression 27%, and social dysfunction was 24.3% (95% among pregnant and lactating women). It is also important to search for possible resistance factors that can help to defend against high prenatal stress. Social reinforcement can alleviate the impact of prenatal stress and has been found to minimize the effects of prenatal anxiety and depressive symptoms on maternal and child stress response systems. 23 Similarly, the pooled prevalence of insomnia was computed from two eligible articles with a total of 2275 study subjects.44,53 Thus, 34% (95% CI: 3.05%–64.0%) of pregnant and lactating women were found to have insomnia in the DerSimonian and Laird random-effects model (I2 = 99.6%, p = 0.0001). Besides, the pooled prevalence of social dysfunction among pregnant and lactating women was estimated from two eligible studies with a total sample of 473.45,51 The pooled prevalence of social dysfunction was found to be 24.3% (95% CI: 13.41%–62.03%) by using the DerSimonian and Laird random-effects model (I2 = 97.5%, p = 0.0001). Despite the likely negative psychological sequelae of psychological, health, and financial instability combined with social alienation, physical exercise is often correlated with decreased depressive and anxiety symptoms in pregnant individuals 24 Pregnancy is an especially sensitive period when psychiatric depression may have detrimental effects on both mother and child. Considering recent meta-analysis conducted in general population revealed that the overall global prevalence of depressive disorders is 25% in the general population 22 which is lower, as compared to 27% among pregnant women and lactating, in addition, this, the present meta-analysis findings identified higher pooled proportion of anxiety 34% and stress 56% during the COVID-19 outbreak. This implies a substantial impact of the current pandemic situation on mental health among pregnant and lactating women that should be targeted during antenatal care and postpartum care-level strategies.
This is the first systematic review and meta-analysis undertaken of all available studies of anxiety, depression, stress, and social dysfunctions among pregnant and lactating women during the COVID-19 outbreak. Meta-analysis revealed that greater power than individual studies to estimate more accurate rates of anxiety, depression, stress, and social dysfunctions, by considering a much larger population drawn from different countries. However, limitations should be considered when interpreting these results. For example, randomization of the sample was not available in certain situations, and data had to be gathered by Internet surveys, which may have led to selection biases, such as oversampling of younger and more qualified individuals. 60 Ultimately, the latest meta-analysis relies on studies that involve pregnant and lactating women only. The effect of COVID-19 on the psychological well-being of disadvantaged populations, such as health staff, outpatients, or elderly persons, is projected to be high. Future epidemiological trials performed in these subpopulations, as well as systemic analyses of evidence pooling, are also especially required to adjust public health strategies.
Limitation of the study Letters to editors, short communications, and preprints were not considered in this study which may be the limitation of this study. Another weakness may be revealed that a small fail-safe N suggests that the conclusion of the meta-analysis may be susceptible to publication bias. Lack of reporting metrics that are known to influence anxiety and depression symptoms is a limitation to the study.
Conclusion
The mental health effects of COVID-19 among pregnant and lactating women were determined in terms of anxiety, depression, stress, social dysfunction, and insomnia. This systematic review and meta-analysis determined the overall global pooled prevalence of anxiety 33%, depression 27%, stress 56%, insomnia 34%, and social dysfunction 24% during the COVID-19 pandemic outbreak in the globe among pregnant and lactating women. This implies a substantial impact of the current pandemic situation on mental health among pregnant and lactating women that should be targeted during antenatal care and postpartum care-level strategies. This embryonic condition involves collaborative efforts by the research community to add to the monitoring of pregnant and lactating women during the COVID-19 epidemic and to examine the short- and long-term detrimental effects on the mental health well-being of mothers and infants. Therefore, policymakers and health planners should give great emphasis to addressing maternal mental well-being during and after this global health crisis. Maternal mental health must be one of the international and national public health priority agendas to enhance the well-being of pregnant and lactating women. Besides, giving psychological support to pregnant and lactating women may reduce the long-term negative effects of this pandemic.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211026195 for Mental health effect of COVID-19 pandemic among women who are pregnant and/or lactating: A systematic review and meta-analysis by Dereje Bayissa Demissie and Zebenay Workneh Bitew in SAGE Open Medicine
Acknowledgments
The authors would like to address their gratitude to the authors of the included studies for this systematic review and meta-analysis and St. Paul’s Hospital Millennium Medical College.
Footnotes
Author contributions: D.B.D. and Z.W.B. conceived and designed the review. Z.W.B. prepared the draft of the manuscript. The final version of the manuscript was approved by all the authors.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from INSTITUTIONAL REVIEW BOARD (APPROVAL NUMBER/ID) (SPHMMC 202/21/2019) from the ethical review board of St. Paul’s Hospital Millennium Medical College (Or) Ethical approval for this study was waived by INSTITUTIONAL REVIEW BOARD* because *REASON FOR WAIVER*. For printing and secretarial services only.
Informed consent: Written informed consent was obtained from all subjects before the study. Not applicable.
Informed consent was not sought for this study because this study was a systematic review and meta-analysis.
ORCID iD: Dereje Bayissa Demissie  https://orcid.org/0000-0003-1006-4318
https://orcid.org/0000-0003-1006-4318
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Health Organization (WHO). Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance. Geneva: WHO, 2020, p. 21. [Google Scholar]
- 2. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM 2020; 113(5): 311–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Da Silva AG, Miranda DM, Diaz AP, et al. Mental health: why it still matters in the midst of a pandemic. Braz J Psychiatry 2020; 42: 229–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hawryluck L, Gold WL, Robinson S, et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis 2004; 10(7): 1206–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020; 17(5): 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Al-Rabiaah A, Temsah M-H, Al-Eyadhy AA, et al. Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J Infect Public Health 2020; 13: 687–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bayrampour H, Tomfohr L, Tough S. Trajectories of perinatal depressive and anxiety symptoms in a community cohort. J Clin Psychiatry 2016; 77(11): e1467–e1473. [DOI] [PubMed] [Google Scholar]
- 8. Coussons-Read ME. Effects of prenatal stress on pregnancy and human development: mechanisms and pathways. Obstet Med 2013; 6(2): 52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Accortt EE, Cheadle AC, Schetter CD. Prenatal depression and adverse birth outcomes: an updated systematic review. Matern Child Health J 2015; 19(6): 1306–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grigoriadis S, Graves L, Peer M, et al. Maternal anxiety during pregnancy and the association with adverse perinatal outcomes: systematic review and meta-analysis. J Clin Psychiatry 2018; 79(5): 17r12011. [DOI] [PubMed] [Google Scholar]
- 11. Qu F, Wu Y, Zhu Y-H, et al. The association between psychological stress and miscarriage: a systematic review and meta-analysis. Sci Rep 2017; 7(1): 1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rondó PHC, Ferreira RF, Nogueira F, et al. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur J Clin Nutr 2003; 57(2): 266–272. [DOI] [PubMed] [Google Scholar]
- 13. Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. The Lancet 2014; 384(9956): 1800–1819. [DOI] [PubMed] [Google Scholar]
- 14. Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol 2014; 28(1): 25–35. [DOI] [PubMed] [Google Scholar]
- 15. MacKinnon N, Kingsbury M, Mahedy L, et al. The association between prenatal stress and externalizing symptoms in childhood: evidence from the Avon Longitudinal Study of Parents and Children. Biol Psychiatry 2018; 83(2): 100–108. [DOI] [PubMed] [Google Scholar]
- 16. Van den Bergh BR, Van den Heuvel MI, Lahti M, et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehav Rev 2020; 117: 26–64. [DOI] [PubMed] [Google Scholar]
- 17. Van den Bergh BR, Dahnke R, Mennes M. Prenatal stress and the developing brain: risks for neurodevelopmental disorders. Dev Psychopathol 2018; 30(3): 743–762. [DOI] [PubMed] [Google Scholar]
- 18. Adamson B, Letourneau N, Lebel C. Prenatal maternal anxiety and children’s brain structure and function: a systematic review of neuroimaging studies. J Affect Disord 2018; 241: 117–126. [DOI] [PubMed] [Google Scholar]
- 19. Lebel C, Walton M, Letourneau N, et al. Prepartum and postpartum maternal depressive symptoms are related to children’s brain structure in preschool. Biol Psychiatry 2016; 80(11): 859–868. [DOI] [PubMed] [Google Scholar]
- 20. Sandman CA, Buss C, Head K, et al. Fetal exposure to maternal depressive symptoms is associated with cortical thickness in late childhood. Biol Psychiatry 2015; 77(4): 324–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Qiu A, Rifkin-Graboi A, Chen H, et al. Maternal anxiety and infants’ hippocampal development: timing matters. Transl Psychiatry 2013; 3(9): e306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bueno-Notivol J, Gracia-García P, Olaya B, et al. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol 2021; 21: 100196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thomas JC, Letourneau N, Campbell TS, et al. Social buffering of the maternal and infant HPA axes: mediation and moderation in the intergenerational transmission of adverse childhood experiences. Dev Psychopathol 2018; 30(3): 921–939. [DOI] [PubMed] [Google Scholar]
- 24. Demissie Z, Siega-Riz AM, Evenson KR, et al. Physical activity and depressive symptoms among pregnant women: the PIN3 study. Arch Womens Ment Health 2011; 14(2): 145–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151(4): 264–269. [DOI] [PubMed] [Google Scholar]
- 26. Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 2015; 13(3): 147–153. [DOI] [PubMed] [Google Scholar]
- 27. Belur J, Tompson L, Thornton A, et al. Interrater reliability in systematic review methodology: exploring variation in coder decision-making. Sociol Method Res 2021; 50: 837–865. [Google Scholar]
- 28. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 2001; 54(10): 1046–1055. [DOI] [PubMed] [Google Scholar]
- 29. Rücker G, Schwarzer G, Carpenter JR, et al. Undue reliance on I2 in assessing heterogeneity may mislead. BMC Med Res Methodol 2008; 8(1): 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21(11): 1539–1558. [DOI] [PubMed] [Google Scholar]
- 31. Kotabagi P, Fortune L, Essien S, et al. Anxiety and depression levels among pregnant women with COVID-19. Acta Obstet Gynecol Scand 2020; 99: 953–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ali NA, Feroz AS. Maternal mental health amidst the COVID-19 pandemic. Asian J Psychiatr 2020; 54: 102261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Diamond RM, Brown KS, Miranda J. Impact of COVID-19 on the perinatal period through a biopsychosocial systemic framework. Contemp Fam Ther. Epub ahead of print 20 July 2020. DOI: 10.1007/s10591-020-09544-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Corbett GA, Milne SJ, Hehir MP, et al. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol 2020; 249: 96–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zanardo V, Manghina V, Giliberti L, et al. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynaecol Obstet 2020; 150(2): 184–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhang Y, Ma ZF. Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int J Soc Psychiatry 2021; 67: 344–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Suzuki S. Psychological status of postpartum women under the COVID-19 pandemic in Japan. J Matern Fetal Neonatal Med. Epub ahead of print 18 May 2020. DOI: 10.1080/14767058.2020.1763949. [DOI] [PubMed] [Google Scholar]
- 38. Taubman-Ben-Ari O, Chasson M, Abu Sharkia S, et al. Distress and anxiety associated with COVID-19 among Jewish and Arab pregnant women in Israel. J Reprod Infant Psychol 2020; 38(3): 340–348. [DOI] [PubMed] [Google Scholar]
- 39. Franchi M, Del Piccolo L, Bosco M, et al. Covid-19 and mental health in the obstetric population: a lesson from a case of puerperal psychosis. Minerva Ginecol 2020; 72: 355–357. [DOI] [PubMed] [Google Scholar]
- 40. Chandra PS, Shiva L, Nagendrappa S, et al. COVID 19 related Psychosis as an interface of fears, socio-cultural issues and vulnerability- case report of two women from India. Psychiatry Res 2020; 290: 113136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Alijanpour M, Sadatmahalleh SJ, Samaneh Y, et al. Influence psycho-sexual factors on the quality of life in pregnant women during the COVID-19 pandemic: a path analysis, 2020, https://www.researchsquare.com/article/rs-45196/v2
- 42. Cameron EE, Joyce KM, Delaquis CP, et al. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J Affect Disord 2020; 276: 765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chen S, Zhuang J, Chen Q, et al. Psychological investigation on pregnant women during the outbreak of COVID-19, 2020, https://www.researchsquare.com/article/rs-28455/v1
- 44. Dib S, Rougeaux E, Vázquez-Vázquez A, et al. Maternal mental health and coping during the COVID-19 lockdown in the UK: data from the COVID-19 New Mum Study. Int J Gynaecol Obstet 2020; 151: 407–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gharagozloo M, Sadatmahalleh SJ, Khomami MB, et al. Mental health and marital satisfaction changes of pregnant and lactating women during the COVID-19 pandemic, 2020, https://www.researchsquare.com/article/rs-49590/v1
- 46. Tutnjević S, Lakić S. Psychological impact of the COVID-19 pandemic on pregnant women in Bosnia and Herzegovina and Serbia, 2020, https://psyarxiv.com/su3nv/
- 47. Berthelot N, Lemieux R, Garon-Bissonnette J, et al. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand 2020; 99: 848–855. [DOI] [PubMed] [Google Scholar]
- 48. Wu Y, Zhang C, Liu H, et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol 2020; 223(2): 240.e1–240.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Saccone G, Florio A, Aiello F, et al. Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol 2020; 223: 293–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Liu X, Chen M, Wang Y, et al. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: a cross-sectional study. BJOG 2020; 127(10): 1229–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Milne SJ, Corbett GA, Hehir MP, et al. Effects of isolation on mood and relationships in pregnant women during the covid-19 pandemic. Eur J Obstet Gynecol Reprod Biol 2020; 252: 610–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Davenport MH, Meyer S, Meah VL, et al. Moms are not ok: COVID-19 and maternal mental health. Front Glob Women’s Health. Epub ahead of print 19 June 2020. DOI: 10.3389/fgwh.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Parra-Saavedra M, Villa-Villa I, Pérez-Olivo J, et al. Attitudes and collateral psychological effects of COVID-19 in pregnant women in Colombia. Int J Gynaecol Obstet 2020; 151: 203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Patabendige M, Gamage MM, Weerasinghe M, et al. Psychological impact of the COVID-19 pandemic among pregnant women in Sri Lanka. Int J Gynaecol Obstet 2020; 151: 150–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ceulemans M, Hompes T, Foulon V. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic: a call for action. Int J Gynaecol Obstet 2020; 151: 146–147. [DOI] [PubMed] [Google Scholar]
- 56. Yue C, Liu C, Wang J, et al. Association between social support and anxiety among pregnant women in the third trimester during the coronavirus disease 2019 (COVID-19) epidemic in Qingdao, China: the mediating effect of risk perception. Int J Soc Psychiatry 2021; 67: 120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lebel C, MacKinnon A, Bagshawe M, et al. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord 2020; 277: 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J Matern Fetal Neonatal Med. Epub ahead of print 18 May 2020. DOI: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- 59. Farewell CV, Jewell J, Walls J, et al. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. J Prim Care Community Health. Epub ahead of print 16 July 2020. DOI: 10.1177/2150132720944074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wang Y, Di Y, Ye J, et al. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med 2021; 26: 13–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211026195 for Mental health effect of COVID-19 pandemic among women who are pregnant and/or lactating: A systematic review and meta-analysis by Dereje Bayissa Demissie and Zebenay Workneh Bitew in SAGE Open Medicine