Abstract
Background:
There have been conflicting results about the theoretical advantages of anatomic double-bundle anterior cruciate ligament (ACL) reconstruction.
Purpose:
To evaluate the clinical and functional outcomes comparing anatomic single- versus double-bundle techniques, anatomic versus nonanatomic techniques, and transportal versus outside-in tunnel drilling for ACL reconstruction.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
A search was performed in the MEDLINE and EMBASE databases up to August 2018 for clinical trials comparing anatomic ACL reconstruction (with tunnel positioning demonstrated using gold standard radiologic techniques) with another technique, with a minimum functional and biomechanical follow-up of 6 months. A meta-analysis was performed to compare clinical and functional outcomes between anatomic single- versus double-bundle reconstruction and between anatomic versus nonanatomic techniques, using the risk difference or the mean difference. Risk of bias of the included studies was assessed using the Newcastle-Ottawa Scale for cohort and case-control studies and the Cochrane Risk of Bias tool and Jadad Score for randomized controlled trials.
Results:
Included were 15 studies comprising 1290 patients (follow-up, 12-36 months). No significant differences favoring anatomic double-bundle over anatomic single-bundle reconstruction or outside-in over transportal techniques were found. The meta-analyses showed significant differences in the International Knee Documentation Committee (IKDC) objective score (risk difference, –0.14; 95% confidence interval, –0.27 to –0.01) favoring anatomic over nonanatomic reconstruction. No statistically significant differences were found between anatomic and nonanatomic surgical techniques on other functional scores or clinical examination outcomes, including the IKDC subjective score, Lysholm score, Tegner score, KT-1000 arthrometer test, or pivot-shift test.
Conclusion:
Double-bundle reconstruction was not superior to the single-bundle technique in clinical and functional outcomes. Anatomic ACL reconstruction shows significantly superior results over nonanatomic ACL reconstruction, reinforcing the anatomic technique as the gold standard choice for clinical practice.
Keywords: anatomic ACL reconstruction, double-bundle ACL reconstruction, transportal reconstruction, outside-in reconstruction
The standard technique for anterior cruciate ligament (ACL) reconstruction is the arthroscopic single-bundle reconstruction using autografts. 23,41 There has been a growing interest in an anatomic approach to ACL reconstruction 8,45 that aims to replicate the native knee anatomy and restore knee kinematics while protecting the knee from further injuries or the onset of knee osteoarthritis. Cadaveric studies have shown benefits of using anatomic ACL reconstruction on restoring sagittal and rotational stability and improving knee function. 22,28
Anatomic ACL reconstruction mainly consists of functional restoration of the ACL to its native dimensions, collagen orientation, and insertion sites, positioning tunnels in the ACL footprint, which has 2 distinct portions or “bundles”: an anteromedial bundle and a posterolateral bundle. 41,44 The anteromedial bundle is the primary restraint against anterior tibial translation, with more knee flexion, while the posterolateral bundle secures the knee when near full extension, particularly against rotational loads. 41
However, use of the term “anatomic” with regard to ACL reconstruction can be misleading, as it has been used interchangeably with several ACL reconstruction techniques. 3 A systematic review of cadaveric studies by van Eck et al 45 has found that the anatomic ACL reconstruction was poorly defined and there is a gross underreporting of the surgical technique methods; thus, to be considered anatomic, the ACL reconstruction tunnels must be positioned in the center of the femoral and tibial footprints. Only two-thirds of studies visualized the tibial and femoral ACL insertion sites, and none had measured the insertion sites or visualized the bony ridges. 45 Studies reporting anatomic ACL reconstruction in adult human patients have shown heterogeneity and underreporting of the ACL insertion site and femoral intercondylar notch measurement, individualization of surgery, knee flexion angle during femoral tunnel drilling, graft tensioning pattern, and intraoperative/postoperative imaging. 47
Correct characterization of the insertion site anatomy in ACL reconstruction with precise radiologic methods, such as computed tomography (CT) or magnetic resonance imaging (MRI) evaluating the 3 axes, can be performed with high intra- and interobserver reliability and small standard errors of measurement. 7 However, despite the development of contemporary techniques and experienced orthopaedic surgeons, positioning of the femoral tunnel is often imprecise. 10
The purpose of this systematic review was to compare the outcomes of anatomic single-bundle (ASB) versus anatomic double-bundle (ADB) ACL reconstruction with tunnel positioning demonstrated using gold standard radiologic techniques. As a secondary objective, we aimed to compare anatomic versus nonanatomic techniques and transportal to outside-in tunnel drilling in anatomic ACL reconstruction. The hypothesis was that ADB reconstruction would result in superior clinical outcomes over nonanatomic or ASB reconstruction techniques.
Methods
Protocol and Registration
This systematic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. 13 The review was a priori registered at the international prospective register of systematic reviews (PROSPERO; identification No. CRD42016042603).
Search Strategy
A comprehensive database search using the MEDLINE and EMBASE was conducted on August 28, 2018. The following search terms were used: “anterior cruciate ligament” OR “ACL” AND “anatomic” OR “anatomical” AND “reconstruction” OR “surgery.” The reference lists of the selected studies and other relevant studies were screened to identify potential additional studies that were not found through the electronic search.
Study Selection
All titles and abstracts were screened, and the full text of all potentially relevant studies identified was retrieved and analyzed according to the following inclusion criteria: (1) prospective or retrospective cohort studies, (2) studies comparing anatomic with nonanatomic reconstruction or ASB to ADB reconstruction techniques, (3) minimum functional and biomechanical postoperative evaluation of 6 months, and (4) tunnel positioning demonstrated using gold standard radiologic techniques. For inclusion purposes, “anatomic ACL reconstruction” was defined as the identification and insertion of the femoral tunnel at the ACL native footprint. The population of interest was skeletally mature patients with documented ACL deficiency of the knee, requiring arthroscopically assisted ACL reconstruction. All arthroscopic tunnel drilling techniques were included, as well as any method of fixation of the graft. Excluded were studies without confirmation of tunnel positioning using MRI or CT scan, ACL reconstruction using allografts or synthetic materials, and ACL revision surgeries.
Titles and abstracts were reviewed by 2 independent authors (T.L.F., S.U.S.), who applied the eligibility criteria and retrieved the full text of potential articles to be included. If the abstract did not provide enough data to make an immediate decision, the full text was also retrieved. The same 2 independent authors analyzed the full texts using the previously described criteria. Any disagreement between the 2 reviewers was resolved via consensus.
Data Collection Process
Data were extracted according to a predefined standardized data sheet. The same independent authors compared the data extracted for each study to achieve consensus.
Continuous outcomes were extracted as mean and standard deviation and included the following parameters. Because ACL reconstruction is usually an operation performed in active patients, we evaluated return to activity/level of sports participation, including Tegner and Lysholm scores 42 and clinical composite scores of the International Knee Documentation Committee (IKDC) subjective knee form. 15 The static stability measures (KT arthrometer or other stability assessment devices, including stress tests and an open MRI or 3-dimensional CT scan).
Categorical outcomes were collected as the total number of events for clinical composite scores (IKDC objective knee form) 15 and clinical stability examination (pivot-shift test). The IKDC objective scores were defined as positive (if rated A or B) or negative (if rated C or D). Pivot shift of the operated knee was compared with that of the contralateral knee and was graded as 0 (no laxity) to 3 (maximum laxity). An event was defined as positive (if rated 0 or 1) or negative (if rated 2 or 3).
Outcome assessment was analyzed based on a minimum 6-month postsurgical state, and measurements obtained at time zero (intraoperatively) were excluded.
Methodological Quality and Risk of Bias in Individual Studies
The methodological quality of cohort and case-control studies was appraised using the Newcastle-Ottawa Scale (NOS), which judges studies on 8 items, divided into 3 groups: the selection of the study groups, the comparability of the groups, and the ascertainment of either the exposure or the outcome of interest. Stars are given for the evaluated items, up to a maximum of 9, with 7 being the cutoff point for high-quality studies. 26
The risk of bias of randomized trials was evaluated using the Cochrane Collaboration Risk of Bias tool 11 and the Jadad scale. 16 The Risk of Bias tool evaluated the following domains of bias as high or low risk: focal question, random sequence generation, allocation concealment, blinding, completeness of outcome data, demographic aspect, outcomes, intention to treat, and sample calculation. The quality of the study was based on the sum of the risks assessed in each domain. A study with a single domain with a high risk of bias was considered to be moderate quality, and a study having >1 domain was considered to be low quality. The Jadad scale is a procedure to independently assess the methodological quality of a clinical trial, judging the effectiveness of blinding and scoring between 0 (very poor) and 5 (rigorous). Two review authors (T.L.F., S.U.S.) independently scored the methodological quality of included studies. Any disagreements were resolved via consensus.
Quantitative Synthesis
Data were extracted on an intention-to-treat basis. The level of statistical significance was set at a P value <.05. The differences between the outcome measures using the risk difference for dichotomous variables and the mean difference for continuous variables with a 95% confidence interval were calculated. Data were analyzed using Review Manager software Version 5.3 (RevMan 5.3; Cochrane Collaboration), using the Mantel-Haenszel method for categorical variables and the inverse variance method for continuous variables. Fixed and random effects based on the heterogeneity statistic I2 were considered, and a cutoff point of 50% was used. When an I2 ≥50% was found, a sensitivity analysis was performed to identify any studies with a higher probability of a publication bias (outliers), using a funnel plot with a fixed-effects model. The objective of the sensitivity analysis was to identify publication bias that explains the heterogeneity observed using the Egger test (funnel plot). When there was no publication bias, a random-effects model was used for the analysis. To further investigate heterogeneity, subgroup analyses were performed according to the type of study design of the studies. In the conflict between randomized controlled trials (RCTs) and cohort studies, the results of RCTs were considered.
Results
Study and Population Characteristics
From the initial 2755 articles found in the literature search, 15 studies, all published between 2011 and 2018, were included in this systematic review (Figure 1). ∥∥ A total of 1290 patients were followed for a period between 12 and 36 months after surgery. The characteristics of participants comparing ASB versus ADB, anatomic versus nonanatomic, and transportal versus outside-in are presented in Tables 1 to 3, respectively. There were no apparent statistically significant differences in characteristics between the different surgical techniques.
Figure 1.
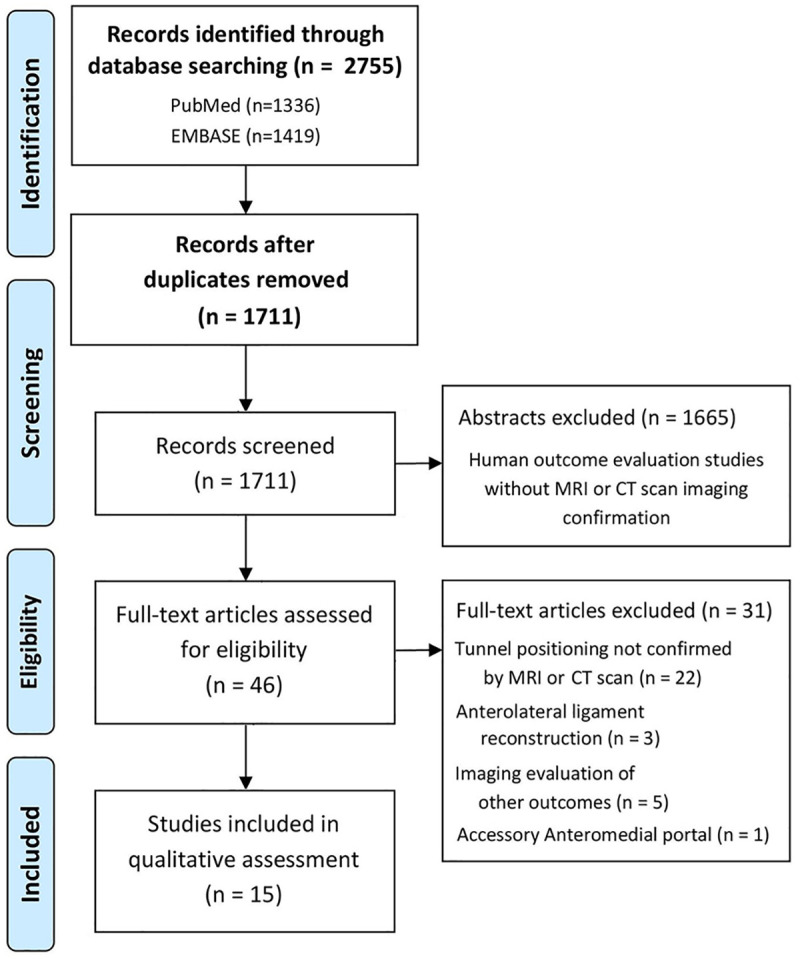
Flowchart of literature search process using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. CT, computed tomography; MRI, magnetic resonance imaging.
Table 1.
Characteristics of Studies on Anatomic Single- Versus Double-Bundle ACL Reconstruction a
| Study (Year) | Anatomic Single-Bundle | Anatomic Double-Bundle | ||||
|---|---|---|---|---|---|---|
| No. of Patients | Age, y | Male/Female | No. of Patients | Age, y | Male/Female | |
| Aga (2018) 1 | 62 | 27.1 ± 5.5 | 41/21 | 54 | 27.4 ± 6.3 | 47/7 |
| Hussein (2012) 12 | 30 | 28.1 | NR | 64 | 26 | NR |
| Sadoghi (2011) 32 | 17 | NR | NR | 16 | NR | NR |
| Suomalainen (2013) 38 | 25 | 30 ± 8 | 18/7 | 25 | 32 ± 11 | 16/9 |
| Taketomi (2014) 39 | 26 | 26 | 24/2 | 26 | 31 | 14/12 |
| Xu (2013) 47 | 32 | 33.3 ± 12.8 | 25/7 | 34 | 30.2 ± 7.7 | 24/10 |
| Zhang (2016) 50 | 20 | 22.3 ± 5.3 | 13/7 | 20 | 28.3 ± 6.1 | 14/6 |
a Data are presented as number of patients or mean ± SD. ACL, anterior cruciate ligament; NR, not reported.
Table 2.
Characteristics of Studies on Nonanatomic Versus Anatomic Techniques a
| Nonanatomic | Anatomic | |||||
|---|---|---|---|---|---|---|
| Study (Year) | No. of Patients | Age, y | Male/Female | No. of Patients | Age, y | Male/Female |
| Lee (2014) 20 | 52 | NR | NR | 52 | NR | NR |
| Pande (2017) 30 | 49 | 29.35 ± 7.95 | 47/2 | 43 | 31.16 ± 7.73 | 41/2 |
| Sadoghi (2011) 32 | 33 | NR | NR | 20 | NR | NR |
| Seo (2013) 33 | 41 | 30.6 ± 11.14 | 32/9 | 48 | 32.4 ± 13.3 | 40/8 |
| Sukur (2016) 36 | 49 | 26.8 ± 5.7 | 45/4 | 56 | 25.5 ± 5 | 52/4 |
| Tashiro (2017) 40 | 20 | 29 ± 9 | NR | 30 | 27 ± 9 | NR |
| Youm (2014) 49 | 20 | 29.7 ± 11.9 | 20/0 | 20 | 27.6 ± 9.9 | 19/1 |
a Data are presented as number of patients or mean ± SD. NR, not reported.
Table 3.
Aspects Comparing the Groups Undergoing the Transportal Versus Outside-In Technique a
| Study (Year) | Transportal | Outside-In | ||||
|---|---|---|---|---|---|---|
| No. of Patients | Age, y | Male/Female | No. of Patients | Age, y | Male/Female | |
| Kim (2018) 18 | 53 | 36.4 ± 10.1 | 40/13 | 58 | 35 ± 10.1 | 51/7 |
| Sim (2018) 35 | 32 | 23.9 ± 0.2 | 27/5 | 32 | 24.8 ± 8 | 23/9 |
a Data are presented as number of patients or mean ± SD.
ASB Versus ADB ACL Reconstruction
There were 7 studies with 451 patients on ASB versus ADB, with 212 patients undergoing ASB and 239 undergoing ADB reconstruction (Table 1). 1,12,32,38,39,47,50 The postoperative assessment ranged between 12 months 32,39,50 and 30 months. 12 Meta-analysis showed no statistically significant differences on all outcomes evaluated: Tegner score (3 studies 32,47,50 ; 139 patients), Lysholm score (5 studies 12,38,39,47,50 ; 294 patients), IKDC objective (3 studies 12,32,38 ; 169 patients) and subjective (4 studies 12,32,47,50 ; 233 patients) scores, pivot-shift test (6 studies 1,12,32,38,39,47 ; 400 patients), and KT-1000 arthrometer test (7 studies 1,12,32,38,39,47,50 ; 440 patients). Forest plots are available online as Supplementary Material (Supplemental Figures S1-S6).
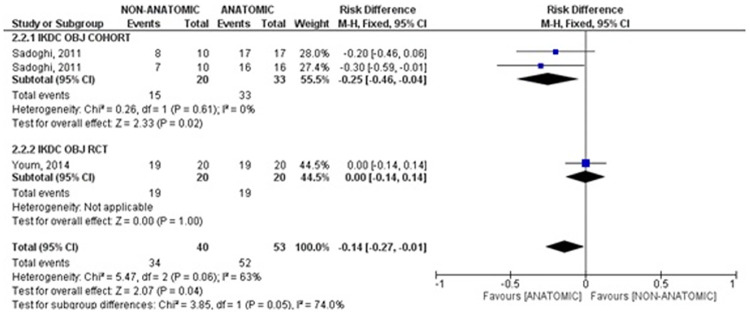
Anatomic Versus Nonanatomic ACL Reconstruction
Seven studies compared anatomic with nonanatomic ACL reconstruction, with 269 patients having the anatomic technique and 264 undergoing the nonanatomic technique (Table 2). Three studies 32,33,40 had a minimum 12-month follow-up, while the other 4 studies 20,30,36,49 were at least 24 months. The meta-analysis showed statistically significant differences in the IKDC objective score favoring the anatomic reconstruction (risk difference, –0.14; 95% confidence interval, –0.27 to –0.01) (Figure 2). Sadoghi 32 evaluated two groups, and made comparisons between anatomical versus non-anatomical reconstruction using both the bone-patellar tendon-bone graft and the semitendinous-gracilis graft technique. As only Sadoghi et al 32 and Youm et al 49 evaluated this outcome, the result is because of the samples from the cohort studies, whereas the RCT 49 did not show a statistically significant difference. No statistically significant superiority was found between the anatomic and nonanatomic surgical techniques for other functional scores or physical examination, including the IKDC subjective score (4 studies 20,30,32,50 ; 289 patients), KT-1000 arthrometer test (4 studies 20,32,33,40 ; 296 patients), Lysholm score (5 studies 20,30,33,40,49 ; 375 patients), Tegner score (5 studies 20,30,32,33,49 ; 378 patients), and pivot-shift test (5 studies 20,32,33,36,49 ; 395 patients). Forest plots are available as supplementary material (Supplemental Figures S7-S11).
Figure 2.
Meta-analysis of nonanatomic versus anatomic anterior cruciate ligament (ACL) reconstruction evaluating the International Knee Documentation Committee (IKDC) objective score. The results indicated a significant difference in favor of anatomic reconstruction. M-H, Mantel-Haenszel; OBJ, objective; RCT, randomized controlled trial.
Transportal Versus Outside-In Tunneling
Two studies 18,35 compared transportal to outside-in tunneling, totaling 85 patients having the transportal technique and 90 patients undergoing the outside-in technique (Table 3). Both studies performed anatomic ACL reconstruction; however, Sim et al 35 used the ASB technique, and Kim et al 18 used the ADB technique. No statistically significant differences were found between tunneling techniques for the IKDC subjective score, Tegner score, or pivot-shift test (2 studies 18,35 ; 175 patients). Forest plots are available online as Supplementary Material (Supplemental Figures S12-S14).
Risk of Bias
The risk of bias of RCTs was evaluated using the Cochrane Collaboration Risk of Bias tool, and 1 study was considered low quality 40 ; 1, moderate 47 ; and the other 3, high quality. 1,18,49 The domain with a higher risk of bias was blinding (high risk in 3 studies) because of the nonblinding of outcome assessors. When the Jadad scale was applied to the articles, the average score was 3.2 points out of 5 possible (Table 4).
Table 4.
Risk-of-Bias Assessment for RCTs: Cochrane Tool, Jadad Scale a
| Cochrane Risk-of-Bias Tool: Scale Item a | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Jadad Score |
| Aga (2018) 1 | Low | Low | Low | Low | Low (2.5%) | Low | Low | Low | Low | 5 |
| Tashiro (2017) 40 | Low | High | High | High | Low (20%) | Low | Low | Low | High | 0 |
| Youm (2014) 49 | Low | Low | Low | Low | Low (0%) | Low | Low | Low | Low | 5 |
| Xu (2013) 47 | Low | Low | High | High | Low (17.5%) | Low | Low | Low | High | 3 |
| Kim (2018) 18 | Low | Low | Low | High | Low (7.8%) | Low | Low | Low | Low | 3 |
a Items: 1 = focal question; 2 = random sequence generation; 3 = allocation concealment; 4 = blinding; 5 = completeness of outcome data (<20% lost); 6 = demographic or prognostic characteristics; 7 = outcomes; 8 = intention to treat; 9 = sample calculation; RCT, randomized controlled trial.
The methodological quality of nonrandomized (cohort and case-control) studies evaluated using NOS was high (mean NOS score, 7.6), with 6 studies 12,20,30,33,36,38 considered high quality (NOS = 8) and 4 studies 32,35,39,50 considered moderate quality (NOS = 7) (Table 5).
Table 5.
Risk-of-Bias Assessment for Cohort and Case-Control Studies: Newcastle-Ottawa Scale a
| Selection Bias | Comparability | Outcome/Exposure | ||||||
|---|---|---|---|---|---|---|---|---|
| Study (Year) | 1 | 2 | 3 | 4 | 1 | 1 | 2 | 3 |
| Pande (2017) 30 | * | * | * | ** | * | * | * | |
| Sukur (2016) 36 | * | * | * | ** | * | * | * | |
| Lee (2014) 20 | * | * | * | ** | * | * | * | |
| Sim (2018) 35 | * | * | * | ** | * | <24 mo | * | |
| Zhang (2016) 50 | * | * | * | ** | * | <24 mo | * | |
| Sadoghi (2011) 32 | * | * | * | ** | * | <24 mo | * | |
| Seo (2013) 33 | * | * | * | ** | * | * | * | |
| Hussein (2012) 12 | * | * | * | ** | * | * | * | |
| Suomalainen (2013) 38 | * | * | * | ** | * | * | * | |
| Taketomi (2014) 39 | * | * | * | ** | * | <24 mo | * | |
a In this scale, each item is scored either 0 or 1 stars, except for comparability, which can score 0, 1, or 2 stars, totaling 9 stars.
Discussion
The main finding of this study was that there was significant superiority in the IKDC objective score of anatomic compared with nonanatomic ACL reconstruction; however, ADB reconstruction was not superior to ASB reconstruction, and the outside-in technique was not superior to the transportal tunnel drilling technique in any of the clinical and functional outcomes assessed.
Anatomic ACL reconstruction presents theoretical advantages despite many patients reporting some residual knee instability, not returning to their previous level of sports activity, and the development of knee degenerative changes. 2,21,37 The anatomic reconstruction aims to restore knee anatomy and kinematics as close as possible and places the graft more horizontal to better control the rotational laxity. 4 The anatomic placement of the graft reduces the risk of impingement at the intercondylar notch, loss of range of motion, and failure of the fixation or the graft itself, which may cause suboptimal results. 29 Yasuda et al 48 showed significantly better results in patients operatively treated using anatomic reconstruction regarding side-to-side anterior laxity; these results were subsequently corroborated in laboratory studies, restoring the uninjured knee to levels of stability. 9 In our systematic review, we found a significant superiority of anatomic over nonanatomic ACL reconstruction in the IKDC objective score but not in other clinical and functional outcomes.
The potential superiority of ADB has been debated in the literature within the past decade. The main advantages of ADB reconstruction are that ADB better re-creates the double-bundle native ACL anatomy and knee kinematics and provides better control of postoperative knee stability. 24 Despite these advantages, there are some indications that the ASB technique should be performed instead of the double-bundle technique: tibial insertion site <14 mm in length (measured arthroscopically), concomitant arthritic changes (Kellgren-Lawrence grade ≥3), knee multiligament injury, severe bone bruising, open physes, and a narrow and/or shallow intercondylar notch (<14 mm each). 14,34,44 When the posterior bundle is reconstructed, there is theoretical benefit of improved rotational stability, but recent studies have indicated that despite requiring more surgical time and greater technical difficulty, 6 ADB ACL reconstruction does not result in superior clinical and functional outcomes compared with ASB ACL reconstruction (when grafts are placed at the center of the anatomic position and the femoral tunnel is lower than it is when the standard technique is used). 17,24,27
In the present systematic review, there was no significant superiority of the ASB or ADB technique over the other. A considerable amount of research has been published in the past few decades comparing ADB with ASB ACL reconstruction techniques, and other systematic reviews have been published on this topic. A systematic review reported that ADB reconstruction can eliminate pathologic findings in the pivot-shift test, 49 which was not corroborated in the present meta-analysis. Mascarenhas et al 24 performed a systematic review overlapping 9 meta-analyses and found that the ADB technique resulted in superior KT-1000 arthrometer and pivot-shift test outcomes. Similarly, a meta-analysis performed by Xu et al 47 found that the ADB technique resulted in superior pivot-shift tests and IKDC objective scores. The meta-analysis by Björnsson et al 3 did not show superiority of the technique in clinical evaluation at short- and long-term follow-ups, such as the preoperative level and performance of return to sports activity. In a meta-analysis, van Eck et al 43 presented positive results for double-bundle reconstruction for anterior and rotational laxity, assessed using arthrometer and physical examination (Lachman and pivot-shift tests), while Mundi and Bhandari 27 showed faster return to the sports and a reduced risk of new ACL injuries. However, even when the comparison between ADB and ASB techniques showed significant differences in prospective studies, they were limited to objective evaluations because in the postoperative period, patients had similar opinions regardless of the surgical technique, as exemplified in the study by Kondo et al 19 according to Massey et al, 25 in which the patients had superior results in ADB reconstruction via the KT-2000 arthrometer but no statistically different scores, such as the IKDC subjective. We must consider that physical and noninstrumented examination is highly subjective and can present great variation among examiners. Despite all the theoretical advantages of the ADB technique, the literature has shown inconsistent results, and there is no convincing and consistent evidence that ADB would be superior to ASB ACL reconstruction, which is underpinned by the present study.
The transportal and outside-in femoral drilling techniques are both able to obtain an anatomic graft placement. The transportal technique allows one to perform the ACL reconstruction all-inside but has the risk of posterior wall blowout. In turn, the outside-in technique prevents the risk of posterior wall blowout but requires increased operative time and a second incision that can lead to further morbidity. 14,31 Recently, researchers have questioned if there are differences in the functional results of these 2 techniques because the graft is placed at a sharper angle when using outside-in drilling, which may increase the stress to which it is submitted. 18 Although Kim et al 18 found a difference in the IKDC objective score favoring the outside-in technique, no significant differences for functional, clinical, and imaging postoperative outcomes have been reported. 5,18 The present meta-analysis corroborates the finding that there are no significant differences between transportal and outside-in techniques.
The results of this systematic review and meta-analysis are relevant for the clinical practice, as they reinforce anatomic ACL reconstruction as standard of care, using only studies that demonstrated the graft placement using gold standard radiologic imaging techniques. When comparing outcomes of ACL reconstruction techniques, it is important to have confirmation of the tunnel positions to ensure that the comparison is valid. No recommendation can be made on the choice between ADB or ASB technique and transportal or outside-in femoral drilling, as there were no statistically significant differences, and which technique is superior remains elusive. The choice of technique should thus be guided based on surgeon experience, available equipment, patient characteristics, and graft choice. 14
There are some limitations in the present study. The small number of published randomized clinical trials comparing anatomic reconstruction verified using gold standard postoperative imaging using different techniques limited the robustness of the meta-analyses. In addition, the follow-up was short in some studies, and there was no discrimination regarding the specific sport or level of competition of the patients. More high-quality studies using gold standard tunnel positioning evaluation methods are warranted to confirm the robustness of the results because even in ADB ACL reconstruction, making 2 tunnels in the femur and tibia does not necessarily guarantee that they are in the proper position to consider the anatomic technique. 46
Conclusion
The current systematic review demonstrated that there were no significant differences in functional or clinical outcomes comparing ASB versus ADB ACL reconstruction and comparing transportal versus outside-in femoral drilling. Anatomic ACL reconstruction had a significant superior IKDC objective score compared with nonanatomic ACL reconstruction, but other functional and clinical outcomes showed no significant differences.
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671211013327 for Clinical Outcome Evaluation of Anatomic Anterior Cruciate Ligament Reconstruction With Tunnel Positioning Using Gold Standard Techniques: A Systematic Review and Meta-analysis by Tiago Lazzaretti Fernandes, Hugo Henrique Moreira, Renato Andrade, Sandra Umeda Sasaki, Wanderley Marques Bernardo, André Pedrinelli, João Espregueira-Mendes and Arnaldo José Hernandez in Orthopaedic Journal of Sports Medicine
Footnotes
Supplemental material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671211013327.
References
- 1. Aga C, Risberg MA, Fagerland MW, et al. No difference in the KOOS quality of life subscore between anatomic double-bundle and anatomic single-bundle anterior cruciate ligament reconstruction of the knee: a prospective randomized controlled trial with 2 years’ follow-up. Am J Sports Med. 2018;46(10):2341–2354. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. [DOI] [PubMed] [Google Scholar]
- 3. Björnsson H, Desai N, Musahl V, et al. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):696–739. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Selby RM, Altchek DW. Augmentation of primary vertical graft. Arthroscopy. 2006;22(6):1–5. [DOI] [PubMed] [Google Scholar]
- 5. Cury RP, Sprey JW, Bragatto AL, Mansano MV, Moscovici HF, Guglielmetti LG. Comparative evaluation of the results of three techniques in the reconstruction of the anterior cruciate ligament, with a minimum follow-up of two years. Rev Bras Ortop. 2017;52(3):319–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Desai N, Alentorn-Geli E, van Eck CF, et al. A systematic review of single- versus double-bundle ACL reconstruction using the anatomic anterior cruciate ligament reconstruction scoring checklist. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):862–872. [DOI] [PubMed] [Google Scholar]
- 7. Forsythe B, Kopf S, Wong AK, et al. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am. 2010;92(6):1418–1426. [DOI] [PubMed] [Google Scholar]
- 8. Fu FH, van Eck CF, Tashman S, Irrgang JJ, Moreland MS. Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):640–648. [DOI] [PubMed] [Google Scholar]
- 9. Gadikota HR, Wu JL, Seon JK, Sutton K, Gill TJ, Li G. Single-tunnel double-bundle anterior cruciate ligament reconstruction with anatomical placement of hamstring tendon graft: can it restore normal knee joint kinematics? Am J Sports Med. 2010;38(4):713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hart A, Sivakumaran T, Burman M, Powell T, Martineau PA. A prospective evaluation of femoral tunnel placement for anatomic anterior cruciate ligament reconstruction using 3-dimensional magnetic resonance imaging. Am J Sports Med. 2018;46(1):192–199. [DOI] [PubMed] [Google Scholar]
- 11. Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. The Cochrane Library. Issue 3. John Wiley & Sons; 2005. [Google Scholar]
- 12. Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Individualized anterior cruciate ligament surgery. Am J Sports Med. 2012;40(8):1781–1788. [DOI] [PubMed] [Google Scholar]
- 13. Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–784. [DOI] [PubMed] [Google Scholar]
- 14. Irarrázaval S, Kurosaka M, Cohen M, et al. Anterior cruciate ligament reconstruction. J ISAKOS. 2016;1:38–52. [Google Scholar]
- 15. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 16. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. [DOI] [PubMed] [Google Scholar]
- 17. Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013;25(4):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim JG, Kang SH, Kim JH, Lim CO, Wang JH. Comparison of clinical results, second-look arthroscopic findings, and MRI findings between the transportal and outside-in techniques for double-bundle anatomic anterior cruciate ligament reconstruction: a prospective, randomized controlled trial with a minimum 2-year follow-up. Am J Sports Med. 2018;46(3):544–556. [DOI] [PubMed] [Google Scholar]
- 19. Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T. Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med. 2008;36(9):1675–1687. [DOI] [PubMed] [Google Scholar]
- 20. Lee JK, Lee S, Seong SC, Lee MC. Anatomic single-bundle ACL reconstruction is possible with use of the modified transtibial technique: a comparison with the anteromedial transportal technique. J Bone Joint Surg Am. 2014;96(8):664–672. [DOI] [PubMed] [Google Scholar]
- 21. Lie MM, Risberg MA, Storheim K, Engebretsen L, Øiestad BE. What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med. 2019;53:1162–1167. [DOI] [PubMed] [Google Scholar]
- 22. Lim HC, Yoon YC, Wang JH, Bae JH. Anatomical versus non-anatomical single bundle anterior cruciate ligament reconstruction: a cadaveric study of comparison of knee stability. Clin Orthop Surg. 2012;4(4):249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Malempati CS, Metzler AV, Johnson DL. Single-bundle anatomic anterior cruciate ligament reconstruction: surgical technique pearls and pitfalls. Clin Sports Med. 2017;36(1):53–70. [DOI] [PubMed] [Google Scholar]
- 24. Mascarenhas R, Cvetanovich GL, Sayegh ET, et al. Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31(6):1185–1196. [DOI] [PubMed] [Google Scholar]
- 25. Massey PR, Tjoumakaris FP, Bernstein J. Eminence-based medicine versus evidence-based medicine: is anterior cruciate ligament reconstruction optimally performed with the double-bundle technique? Phys Sportsmed. 2013;41(1):102–106. [DOI] [PubMed] [Google Scholar]
- 26. Ministério da Saúde, Secretaria de Ciência, Tencnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia. Methodological Guideline: How to Conduct a Systematic Review and Meta-analysis of Observational Comparative Studies of Risk Factor and Prognosis. Brasilia Ministério da Saúde; 2014. [Google Scholar]
- 27. Mundi R, Bhandari M. Cochrane in CORR®: double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Clin Orthop Relat Res. 2016;474(5):1099–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Musahl V, Plakseychuk A, Vanscyoc A, et al. Varying femoral tunnels between the anatomical footprint and isometric positions: effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med. 2005;33(5):712–718. [DOI] [PubMed] [Google Scholar]
- 29. Nakayama H, Yamaguchi M, Yoshiya S. Comparison of transportal inside-out and outside-in femoral drilling techniques in anatomic ACL reconstruction. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2014;1(1):26–30. [Google Scholar]
- 30. Pande H, Prabahkara A, Singh CM, et al. A 3DCT scan based assessment of femoral tunnel placement in arthroscopic ACL reconstruction by modified transtibial and anteromedial portal technique and its relation with the functional outcome: a retrospective comparative study. J Arthrosc Joint Surg. 2017;4(2):72–78. [Google Scholar]
- 31. Robin BN, Jani SS, Marvil SC, et al. Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2015;31:1412–1417. [DOI] [PubMed] [Google Scholar]
- 32. Sadoghi P, Kröpfl A, Jansson V, Müller PE, Pietschmann MF, Fischmeister MF. Impact of tibial and femoral tunnel position on clinical results after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(3):355–364. [DOI] [PubMed] [Google Scholar]
- 33. Seo SS, Kim CW, Kim JG, Jin SY. Clinical results comparing transtibial technique and outside in technique in single bundle anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013;25(3):133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shen W, Forsythe B, Ingham SM, et al. Application of the anatomic double-bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. J Bone Joint Surg Am. 2008;90:20–34. [DOI] [PubMed] [Google Scholar]
- 35. Sim J, Jong S, Kim M, Lee S, Kyoo E, Seon JK. No difference in graft healing or clinical outcome between trans-portal and outside-in techniques after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2338–2344. [DOI] [PubMed] [Google Scholar]
- 36. Sukur E, Emre Y, Senel A, Ayhan E, Nevzat H. Comparing transtibial and anteromedial drilling techniques for single-bundle anterior cruciate ligament reconstruction. Open Orthop J. 2016;10:481–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sundemo D, Sernert N, Kartus J, et al. Increased postoperative manual knee laxity at 2 years results in inferior long-term subjective outcome after anterior cruciate ligament reconstruction. Am J Sports Med. 2018;46(11):2632–2645. [DOI] [PubMed] [Google Scholar]
- 38. Suomalainen P, Moisala AS, Paakkala A, Kannu P, Järvelä T. Comparison of tunnel placements and clinical results of single-bundle anterior cruciate ligament reconstruction before and after starting the use of double-bundle technique. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):646–653. [DOI] [PubMed] [Google Scholar]
- 39. Taketomi S, Inui H, Nakamura K, et al. Clinical outcome of anatomic double-bundle ACL reconstruction and 3D CT model-based validation of femoral socket aperture position. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2194–2201. [DOI] [PubMed] [Google Scholar]
- 40. Tashiro Y, Okazaki K, Murakami K, et al. Anterolateral rotatory instability in vivo correlates tunnel position after anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft. World J Orthop. 2017;8(12):913–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11(11):CD008413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 43. van Eck CF, Kopf S, Irrgang JJ, et al. Single-bundle versus double-bundle reconstruction for anterior cruciate ligament rupture: a meta-analysis—does anatomy matter? Arthroscopy. 2012;28(3):405–424. [DOI] [PubMed] [Google Scholar]
- 44. van Eck CF, Lesniak BP, Schreiber VM, Fu FH. Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy. 2010;26(2):258–268. [DOI] [PubMed] [Google Scholar]
- 45. van Eck CF, Samuelsson K, Vyas SM, van Dijk CN, Karlsson J, Fu FH. Systematic review on cadaveric studies of anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;9(suppl 1):S101–S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. van Eck CF, Schreiber VM, Mejia HA, et al. “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy. 2010;26(9 suppl):S2–S12. [DOI] [PubMed] [Google Scholar]
- 47. Xu M, Gao S, Zeng C, et al. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29(2):357–365. [DOI] [PubMed] [Google Scholar]
- 48. Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy. 2006;22(3):240–251. [DOI] [PubMed] [Google Scholar]
- 49. Youm YS, Cho S, Lee SH, Youn CH. Modified transtibial versus anteromedial portal technique in anatomic single-bundle anterior cruciate ligament reconstruction: comparison of femoral tunnel position and clinical results. Am J Sports Med. 2014;42(12):2941–2947. [DOI] [PubMed] [Google Scholar]
- 50. Zhang H, Qiu M, Zhou A, Zhang J, Jiang D. Anatomic anterolateral ligament reconstruction improves postoperative clinical outcomes combined with anatomic anterior cruciate ligament reconstruction. J Sports Sci Med. 2016;15(4):688–696. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671211013327 for Clinical Outcome Evaluation of Anatomic Anterior Cruciate Ligament Reconstruction With Tunnel Positioning Using Gold Standard Techniques: A Systematic Review and Meta-analysis by Tiago Lazzaretti Fernandes, Hugo Henrique Moreira, Renato Andrade, Sandra Umeda Sasaki, Wanderley Marques Bernardo, André Pedrinelli, João Espregueira-Mendes and Arnaldo José Hernandez in Orthopaedic Journal of Sports Medicine