Abstract
AIM
To compare the differences and consistency of IOL-Master 700 biometers applying swept optical coherence tomography with the conventional IOL-Master 500 applying partial coherence interference in terms of the ocular biological parameters in adolescents with ametropia.
METHODS
A total of 110 adolescents (110 eyes) with ametropia were collected, including 55 males and 55 females; age 10.69±2.81y. Ocular biological measurements were taken by IOL-Master 700 and IOL-Master 500 respectively to obtain biological parameters including axial length (AL), mean corneal anterior surface keratometry (Km), anterior chamber depth (ACD), and horizontal corneal diameter (WTW). Paired t-test was used to compare the differences between the two instruments. The intra-group correlation coefficient (ICC) and the Bland-Altman analysis were used to evaluate the consistency of parameter measurements between the two instruments for the four biological parameters.
RESULTS
Statistical analysis showed that there was no significant difference in the Km value measured by IOL-Master 700 and IOL-Master 500 (t=-1.644, P=0.116). The average differences of the AL, ACD, and WTW distances between the two instruments are 0.028, 0.101 and 0.064 mm respectively, and the differences are statistically significant (t=2.644, 12.505, 3.911, P<0.001). The consistency study results indicated high correlation in the measurement of AL, Km, ACD and WTW between the two instruments (ICC=0.994, 0.873, 0.927, 0.912).
CONCLUSION
The novel biometric instrument IOL-Master 700 makes no difference with IOL-Master 500 in the measurement of Km. There are some differences in the values of AL, ACD, and WTW. However, the two instruments show good consistency in these four biological measurements. The measured values of Km are interchangeable between the instruments. These two types of biometrics can be used as mutual reference in consideration of that the differences in AL, ACD, and WTW measurements are not sufficient to produce clinically meaningful differences.
Keywords: myopia, adolescents, axial length, IOL-Master 700, IOL-Master 500
INTRODUCTION
In the developed cities of China, the age at which myopia occurs in adolescents is getting younger while the incidence of myopia increases significantly with age, and evidence of this trend is accumulating[1]–[2]. The monitoring of myopia development and the evaluation of myopia control effect are not only limited to the examination of visual acuity and diopter, but also the measurement of ocular biological parameters, such as axial length (AL) and keratometry, etc, among which the change of AL is regarded as the crucial basis for myopia progression as well as an indispensable index for observing the changes of diopter[3]–[4]. Previous studies have shown that each 1 mm increase in the AL will give rise to a myopia aggravation of nearly -2.50 D[5]–[6]. Therefore, ocular biological parameters are essential for assessing risk factors for myopia onset and can serve as an important clinical basis for assessing the effectiveness of any control measures to delay myopia progression. AL can be used to predict the change of diopter and myopia progression[7]. Many studies have sought effective myopia prevention and control methods through demonstrating the correlation between AL and myopia-related factors[8]. Meanwhile, previous research also mentioned other refractive parameters associated with refractive outcome on adolescents, including mean corneal anterior surface keratometry (Km), anterior chamber depth (ACD), and horizontal corneal diameter (WTW)[9]. Therefore, accurate measurement of AL and other ocular biological parameters in adolescents is essential to identify potential risk factors in the progression of ametropia[5].
At present, the commonly used non-contact ophthalmological parameter measuring instrument in clinic is IOL-Master 500, and a considerable number of studies have compared the consistency and reliability of IOL-Master 700 and IOL-Master 500[10]. Previous studies tend to focus on older patients with cataract[11]–[13], while few published research evaluated the consistency of these two instruments in adolescents. Therefore, the aim of this study was to compare the differences and consistency between the two biological instruments in the main ocular biological parameters of the same adolescents, and further to verify whether the measurements of these two biological measuring instruments are interchangeable in clinical practice.
SUBJECTS AND METHODS
Ethical Approval
This study conformed to the principles of the Helsinki Declaration, and the study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Xi'an Jiaotong University. Informed consent was signed.
A total of 110 adolescents (55 males and 55 females) with myopic (110 eyes) were enrolled in the Department of Ophthalmology, the First Affiliated Hospital of Xi'an Jiaotong University from February 2018 to April 2018. The age ranged from 8 to 18y and the spherical equivalent ranged from -0.75 to -6.00 D. The right eye of each subject was chosen as the study object. Exclusion criteria included accompanied by other eye diseases except ametropia, including keratitis, glaucoma, retinal diseases and previous history of ocular trauma and surgery. All the research subjects underwent routine ocular examinations including visual acuity, intraocular pressure, slit-lamp examination, fundus examination, mydriatic optometry and corneal topography.
All the examinations were performed by the same physician in the same darkroom. The examined eye was in natural pupil size. Subject was seated with mandible placed in the mandibular bracket and the forehead close to the forehead bracket. Two eyes are located in the same horizontal position, staring at the indicator. The AL, Km, ACD, and WTW of the subjects were obtained. All the four parameters are measured three times and averaged. The instrument's own software was applied to automatically identified and rejected the abnormal values of the AL. Km is defined as the average value of the keratometry in the flat and steep position of the anterior corneal surface (keratometric index: 1.3375). ACD is defined as the distance from the anterior surface of the corneal epithelium to the anterior surface of the lens. Before measurement, subject was instructed to open eyes after blink three times quickly to form a smooth tear film optical surface on the corneal. The quality of each examination was qualified. The measurement method of the two instruments was comparable.
Instruments
IOL Master 500 (Carl Zeiss Meditec, Jena, Germany) is a non-invasive optical biometer that uses partial coherence interferometry (PCI) with a wavelength of 780 nm to measure the AL of the eye. Axis data are obtained from the optical path distance from the anterior surface of the cornea to the retinal pigment epithelium[14]. It has replaced traditional ultrasound measurement as the gold standard for ocular axis measurement because of its advantages of high accuracy and efficiency[15].
IOL-Master 700 (Carl Zeiss Meditec, Jena, Germany) is a novel non-invasive optical biometer that uses swept source optical coherence tomography (SS-OCT) with a wavelength of 1050 nm. It can obtain three-dimensional anterior segment data of eye tissue quickly and has high lateral and axial resolution. IOL-Master 700 provides the longitudinal sections of each optical interface, and determines the measurement position as the true optic axis length by imaging the fovea centralis[16]. At the same time, it obtains information of corneal anterior and posterior surface as well as lens anterior and posterior surface, macular neuroepithelium and pigment epithelium interface[17]. Accurate data of ACD, lens thickness, and vitreous length are obtained. The acquired anterior segment biometrics are more advantageous than other non-contact biometrics[18]. Except for WTW distance, SS-OCT is applied to obtain the length information of the longitudinal section of the eye (AL, ACD, central corneal thickness, and lens thickness)[19]; keratometry measurement is based on 18 reflective points in three corneal regions (refractive index 1.3375); and WTW is measured using a light-emitting diode light source to detect the edge image of the iris[16]. The IOL-Master 500 examination required that the signal-to-noise ratio (SNR) of the axial measurements be greater than 2.1 while the IOL-Master 700 required the fovea to be observed on fundus OCT images to ensure that the AL was the distance from the corneal apex to the fovea.
Statistical Analysis
Statistical analysis was performed using SPSS 23.0 (IBM Corp., USA) and MedCalc 16.2 (MedCalc Software Ltd., BEL) statistical software. The measurements were expressed as mean±SD. Paired t-test was used to compare the difference of the same parameter obtained by the two measuring instruments. Intraclass correlation coefficient (ICC) and Bland-Altman plot were used to plot the difference between measurements (y-axis) and mean value (x-axis) to assess the consistency and calculate the 95% limit of agreement (95% LoA).The difference was statistically significant when assessed by P<0.05.
RESULTS
One hundred and ten adolescents were included with myopic on an average age of 10.69±2.81 years old (range from 8 to 18 years old) with a gender ratio of 1:1. The mean spherical equivalent was -3.0195 D, ranging from -0.75 to -6.00 D.
Differences of Measurements Between IOL-Master 700 and IOL-Master 500
The mean value and difference of biometric parameters measured by the two devices were shown in Table 1. Paired t-test analysis indicates that there was no significant difference in the measurement of Km between the two instruments (t=-1.583, P=0.116) while there was statistical difference in AL, ACD and WTW measurements (t=2.664, 12.505, 3.911, P<0.01; Table 1).
Table 1. Comparison of biometric measurements of adolescents with ametropia by two biometric instruments.
| Instrument | No. of eyes | AL (mm) | Km (D) | ACD (mm) | WTW (mm) |
| IOL-Master700 | 110 | 24.805±0.969 | 42.642±1.365 | 3.777±0.224 | 12.138±0.415 |
| IOL-Master500 | 110 | 24.777±0.959 | 42.774±1.295 | 3.676±0.219 | 12.075±0.383 |
| difference | 110 | 0.028±0.110 | -0.102±0.674 | 0.101±0.085 | 0.064±0.171 |
| t | 2.664 | -1.583 | 12.505 | 3.911 | |
| P | 0.009 | 0.116 | 0.000 | 0.000 |
AL: Axial length; Km: Mean corneal anterior surface keratometry; ACD: Anterior chamber depth; WTW: Horizontal corneal diameter.
mean±SD
Agreement of Measurements Between IOL-Master 700 and IOL-Master 500
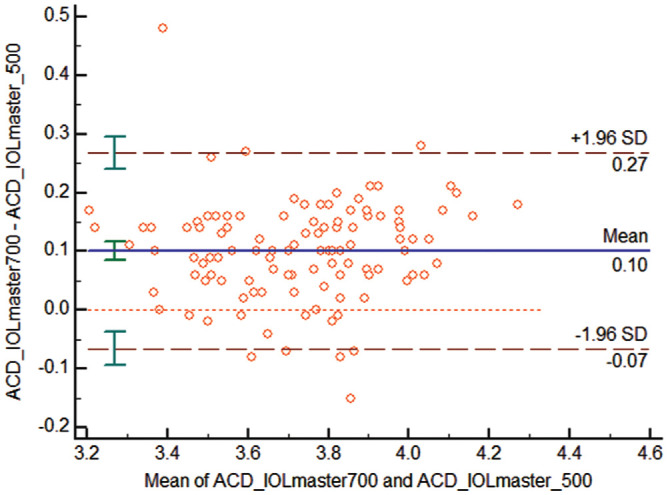
In the consistency analyze between IOL-Master 700 and IOL-Master 500, the ICC value for AL measurements showed high reliability (ICC=0.994); Bland-Altman plots also showed excellent consistency between the two groups, with only 4/110 (3.6%) points located outside 95% LoA, and 95% LoA ranging from -0.19 mm to 0.24 mm (Figure 1). The ICC value of Km, ACD, and WTW were 0.873, 0.927, 0.912, respectively, and the Bland-Altman plot showed that the 95% LoA for all parameters was narrow (Figures 2–4), which indicates a good agreement between the two devices.
Figure 1. Bland-Altman scatter plots of IOL-Master 700 and IOL-Master 500 measuring AL, with dashed lines above and below representing 95% agreement boundaries.
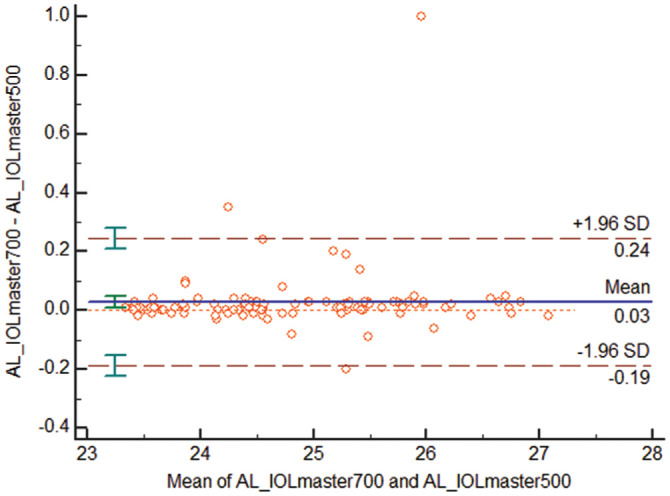
Figure 2. Bland-Altman scatter plot of Km by IOL-Master 700 and IOL-Master 500, with dashed lines above and below representing 95% agreement boundaries.
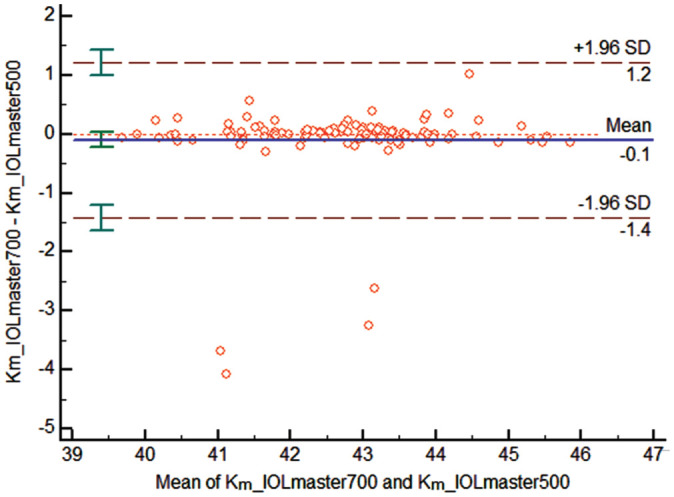
Figure 4. Bland-Altman scatter plots of WTW measured by IOL-Master 700 and IOL-Master 500, with dashed lines above and below representing 95% agreement boundaries.
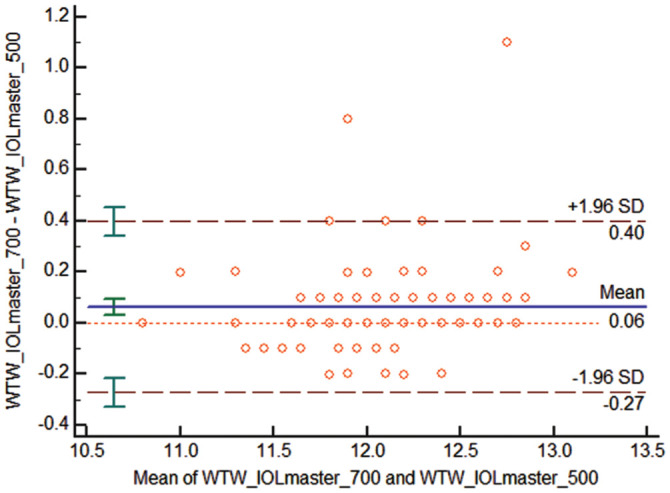
Figure 3. Bland-Altman scatter plot of ACD measured by IOL-Master 700 and IOL-Master 500, with dashed lines above and below representing 95% agreement boundaries.
DISCUSSION
As a newly marketed biometer, IOL-Master 700 is completely different from the traditional biometer IOL-Master 500 in the principle of ocular AL, ACD, and keratometry measurement. The purpose of this study is to compare the consistency of the measurement results of these two biometers on ocular biology parameters of adolescents with myopic and estimate whether their measurements can be interchanged in clinical application.
Yang et al[13] reported that the AL measured by IOL-Master 700 is significantly longer than IOL-Master 500, which is consistent with the results of this study. The difference between the two instruments in measuring the axial values may be related to the device technology of the two instruments and the difference in the gaze fixation[13]. Although the techniques for measuring AL differentiated, there is still a good agreement between the two instruments. Research has shown that each 0.1 mm inaccurate in AL measurement will lead to approximately 0.27 D error[20], therefore, the slight difference between the results in AL measurement (0.028±0.110 mm) in this study is not clinically important in practical application.
Regarding the measurement of Km, both devices applied a distance-independent telecentric keratometric system. The measurements of Km in this study indicates that there was no significant difference between the two instruments, and almost all the keratometry measurements acquired by these two instruments were within 0.4 D. In this study, the average difference between IOL-Master 700 and IOL-Master 500 was -0.102 D. In previous studies, Symes and Ursell[21] showed a result of -0.11 D, which is in accordance with the results of this study, thus the Km values of the two instruments can be interchanged clinically.
In terms of the measurement of ACD, the two instruments measure the depth of the anterior chamber in different principles: IOL-Master 700 is measured by SS-OCT, while IOL-Master 500 is based on image evaluation of the anterior chamber optical cross section through a slit illumination system, which is prone to cause operator errors, and our results showed that ACD measurements using IOL-Master 700 are highly correlated with IOL-Master 500 (ICC=0.927). Interestingly, when comparing the mean differences between the two groups, we found that the ACD measured by IOL-Master 700 was 0.101 mm shorter than IOL-Master 500. Although this finding was statistically significant, this difference was within the acceptance range in clinical practice. Hoffer et al[22] reported that the difference between the two instruments in ACD was -0.16 mm, which is close to the result of this study.
In the measurement of WTW, the difference between the two instruments was statistically significant, nevertheless the ICC and Bland-Altman plot analysis indicated that the consistency of the two instruments on WTW measurement were good. Therefore, the difference between IOL-Master 700 and IOL-Master 500 in measuring WTW cannot lead to an unequivocal clinical significance.
IOL-Master 700 forms macular image by scanning OCT to ensure that the measured AL is the optical path through macular fovea, which is superior to IOL-Master 500. In addition, IOL-Master 700 also provides data of corneal thickness, ACD, lens thickness, and pupil diameter. It may gain a distinct edge when applied to pediatric patients because of faster acquisition speed. The limitations of this study include inadequate sample size, no random sample established in the community as well as absence of comparison in a larger range of people with ametropia. Further studies are needed to explore the effect of these measurement differences on clinical practice.
To sum up, our study demonstrated that IOL-Master 700 and IOL-Master 500 are interchangeable in measuring the ocular biological parameters Km in adolescent with ametropia. However, there are still differences between the two instruments for the measurement of AL, ACD, and WTW distance. The results of the consistency analysis in this study show that the distance of AL, Km, ACD, and WTW between the two instruments have excellent correlation, and the difference between the results can be ignored for practical clinical application.
Acknowledgments
Conflicts of Interest: Shi Q, None; Wang GY, None; Cheng YH, None; Pei C, None.
REFERENCES
- 1.Liu SX, Ye S, Xi W, Zhang X. Electronic devices and myopic refraction among children aged 6-14 years in urban areas of Tianjin, China. Ophthalmic Physiol Opt. 2019;39(4):282–293. doi: 10.1111/opo.12620. [DOI] [PubMed] [Google Scholar]
- 2.Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, Meng M, Jonas JB. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120(2):277–283. doi: 10.1016/j.ophtha.2012.07.086. [DOI] [PubMed] [Google Scholar]
- 3.Jonas JB, Ohno-Matsui K, Panda-Jonas S. Myopia: anatomic changes and consequences for its etiology. Asia Pac J Ophthalmol. 2019;8(5):355–359. doi: 10.1097/01.APO.0000578944.25956.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khan AO. The relationship of axial length to cycloplegic refraction and keratometry in amblyopic eyes of hyperopic children. J Am Assoc Pediatr Ophthalmol Strabismus. 2012;16(1):46–48. doi: 10.1016/j.jaapos.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Zhang JY, Wang Q, Lin SS, Chen JW, Zhong HL, Ca DQ, Chen ZG. Analysis of myopia and axial length changes and relevant factors of children aged 7 to 14 years in Wenzhou. Zhonghua Yan Ke Za Zhi. 2016;52(7):514–519. doi: 10.3760/cma.j.issn.0412-4081.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Hou W, Norton TT, Hyman L, Gwiazda J, Group C. Axial elongation in myopic children and its association with myopia progression in the correction of myopia evaluation trial. Eye Contact Lens. 2018;44(4):248–259. doi: 10.1097/ICL.0000000000000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alimanović EH. Correlation between bulbar axis length and retinal ruptures in case of myopia eye. Bosn J Basic Med Sci. 2009;9(3):187–190. doi: 10.17305/bjbms.2009.2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, Leske MC, Manny R, Marsh-Tootle W, Scheiman M. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44(4):1492–1500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 9.Yu WH, Chen XL. Relationship between diopter and refractive factors in children at the age of 4-13. Chin J Pract Ophthalmol. 2003;21(4):288–290. [Google Scholar]
- 10.Hoffer KJ, Hoffmann PC, Savini G. Comparison of a new optical biometer using swept-source optical coherence tomography and a biometer using optical low-coherence reflectometry. J Cataract Refract Surg. 2016;42(8):1165–1172. doi: 10.1016/j.jcrs.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 11.An Y, Kang EK, Kim H, Kang MJ, Byun YS, Joo CK. Accuracy of swept-source optical coherence tomography based biometry for intraocular lens power calculation: a retrospective cross-sectional study. BMC Ophthalmol. 2019;19(1):30. doi: 10.1186/s12886-019-1036-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song JS, Yoon DY, Hyon JY, Jeon HS. Comparison of ocular biometry and refractive outcomes using IOL master 500, IOL master 700, and lenstar LS900. Korean J Ophthalmol. 2020;34(2):126–132. doi: 10.3341/kjo.2019.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang JY, Kim HK, Kim SS. Axial length measurements: Comparison of a new swept-source optical coherence tomography–based biometer and partial coherence interferometry in myopia. J Cataract Refract Surg. 2017;43(3):328–332. doi: 10.1016/j.jcrs.2016.12.023. [DOI] [PubMed] [Google Scholar]
- 14.Sheng H, Bottjer CA, Bullimore MA. Ocular component measurement using the Zeiss IOLMaster. Optom Vis Sci. 2004;81(1):27–34. doi: 10.1097/00006324-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Kaswin G, Rousseau A, Mgarrech M, Barreau E, Labetoulle M. Biometry and intraocular lens power calculation results with a new optical biometry device: comparison with the gold standard. J Cataract Refract Surg. 2014;40(4):593–600. doi: 10.1016/j.jcrs.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Bullimore MA, Slade S, Yoo P, Otani T. An evaluation of the IOLMaster 700. Eye Contact Lens. 2019;45(2):117–123. doi: 10.1097/ICL.0000000000000552. [DOI] [PubMed] [Google Scholar]
- 17.Hirnschall N, Varsits R, Doeller B, Findl O. Enhanced penetration for axial length measurement of eyes with dense cataracts using swept source optical coherence tomography: a consecutive observational study. Ophthalmol Ther. 2018;7(1):119–124. doi: 10.1007/s40123-018-0122-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akman A, Asena L, Güngör SG. Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500. Br J Ophthalmol. 2016;100(9):1201–1205. doi: 10.1136/bjophthalmol-2015-307779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shajari M, Sonntag R, Ramsauer M, Kreutzer T, Vounotrypidis E, Kohnen T, Priglinger S, Mayer WJ. Evaluation of total corneal power measurements with a new optical biometer. J Cataract Refract Surg. 2020;46(5):675–681. doi: 10.1097/j.jcrs.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 20.Vogel A, Dick BH, Krummenauer F. Reproducibility of optical biometry using partial coherence interferometry: intraobserver and interobserver reliability. J Cataract Refract Surg. 2001;27(12):1961–1968. doi: 10.1016/s0886-3350(01)01214-7. [DOI] [PubMed] [Google Scholar]
- 21.Symes RJ, Ursell PG. Automated keratometry in routine cataract surgery: Comparison of Scheimpflug and conventional values. J Cataract Refract Surg. 2011;37(2):295–301. doi: 10.1016/j.jcrs.2010.08.050. [DOI] [PubMed] [Google Scholar]
- 22.Hoffer KJ, Shammas HJ, Savini G, Huang J. Multicenter study of optical low-coherence interferometry and partial-coherence interferometry optical biometers with patients from the United States and China. J Cataract Refract Surg. 2016;42(1):62–67. doi: 10.1016/j.jcrs.2015.07.041. [DOI] [PubMed] [Google Scholar]


