Abstract
AIM
To review the demographics, clinical manifestations, and surgical experiences of patients with congenital ocular counter-roll, whose treatments were performed exclusively by ophthalmologists.
METHODS
A retrospective review was conducted consisting of patients who received strabismus surgery between 2017 to 2019. Patients with obvious ocular counter-roll were included.
RESULTS
A total of 7008 patients who received strabismus surgery, 28 (12 males, 16 females) were diagnosed as congenital ocular counter-roll, accounting for 0.40%. All patients were initially misdiagnosed: 21 patients were misdiagnosed as superior oblique palsy (SOP), 3 as inferior oblique overaction, 2 as dissociated vertical deviation (DVD), 1 as superior oblique overaction with A-pattern exotropia, and 1 as medial rectus palsy. The mean±SD age was 12.4±9.4y (range 2.5-36y). The most common clinical findings included ocular counter-roll, vertical deviation or vertical deviation combined with outward deviation and head tilt. At follow-up, an excellent surgical result was achieved in 20 patients. Preoperative horizontal deviation of 26±24 prism diopter (PD) and vertical deviation of 18±12 PD were reduced to 0±12 PD (P=0.0001) and 3±4 PD (P=0.001), respectively.
CONCLUSION
Congenital ocular counter-roll is a rare supranuclear vertical strabismus caused by congenital abnormalities involving vestibule-ocular reflex pathways. In addition to ocular counter-roll, the most salient clinical features included, but are not limited to, hyperdeviation, outward deviation, overelevation in adduction and head tilt.
Keywords: congenital ocular counter-roll, skew deviation, cyclovertical strabismus
INTRODUCTION
Ocular cyclotorsion can result from a functional imbalance of the cyclovertical extraocular muscles[1]. In patients with inferior oblique and inferior rectus palsy or superior oblique overaction, each eye is incyclotorted, often accompanying the A-pattern strabismus[2]; while in patients with superior oblique and superior rectus palsy or inferior oblique overaction, each eye is excyclotorted, often accompanying the V-pattern strabismus[3]–[4]. Or, a rare case of congenital superior oblique palsy (SOP), reported by Choi and Lee[5], showed intorsion of nonparalized eye. However, in none of these cyclovertical strabismus disorders is there an excyclotorsion of one eye and incyclotorsion of the contralateral eye, a condition termed ocular counter-roll. From the perspective of ophthalmologists, patients with no indication of individual cyclovertical muscle palsy or A-V pattern strabismus are considered as having ocular counter-roll. Skew deviation is a rare supranuclear vertical misalignment with ocular counter-roll, and is more often seen and treated by neurologists due to the presentation of predominantly neurological symptoms, such as ataxia and dysarthria[6]. As skew deviation often presents with vertical deviation, head tilt and a positive Bielschowsky test response, it is difficult to differentiate it from SOP, A-V patterns or other cyclovertical strabismus disorders[7]. Recently, within our ophthalmology clinic we have found that ocular counter-roll was present in some patients who were previously misdiagnosed as oblique muscle dysfunction, A-V patterns and dissociated vertical deviation (DVD). As all of these patients showed few symptoms and signs characteristic of neurological deficits, they were seen only by ophthalmologists. After excluding other ocular disorders with ocular counter-roll, and considering a congenital basis for this condition and the absence of the results of upright-supine test, we referred to it as congenital ocular counter-roll. In an attempt to better understand this condition, in this paper we performed a retrospective review of congenital ocular counter-roll cases as reported to reveal the demographics, clinical manifestations and surgical experiences in patients receiving treatment as administered exclusively by ophthalmologists.
SUBJECTS AND METHODS
Ethical Approval
The study approved by the Research Ethics Board of the Zhongshan Ophthalmic Center, of Sun Yat-sen University, China, and were compliant with the principles of the Declaration of Helsinki. Informed consent was obtained from every patient or one or both parents for children younger than 18 years of age.
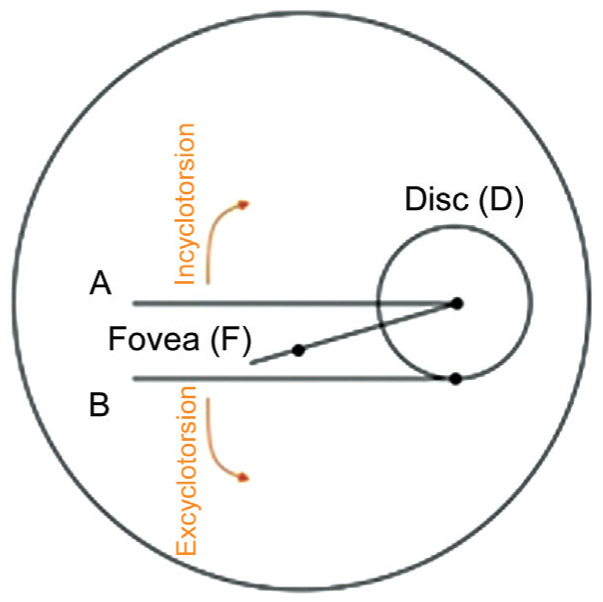
This study consisted of a retrospective review of the medical records of patients who received strabismus surgery between 2017 to 2019. Photographic documentation of the ocular fundi was performed in all patients by one technician using a TRC-50DX (Topcon, Japan) fundus camera. The subject's head was well aligned with the side marks and chin rest used as a guide to avoid any vestibule-ocular reflex (VOR). Disc-fovea angle (DFA) was calculated from a well-focused single still photograph using Photoshop software and a protractor. To obtain the DFA measurement three lines were drawn, two straight lines (horizontal meridian) passing through the geometric center and inferior margin of the optic disc (A and B) and a third line passing through point D (center of the disc) and the fovea (DF). The angle between the fovea and the geometric center of the disc (DFA) was then measured in order to obtain a value indicating the amount of ocular torsion. The eye was determined to have an incyclotorsion when the fovea was located above line A and an excyclotorsion if the fovea was located below line B (Figure 1)[3].
Figure 1. Ocular cyclotorsion as measured with use of the disc-foveal method (DFA).
Patients with obvious ocular counter-roll were considered for inclusion in the study. The following patients were excluded: 1) Those that had undergone previous strabismus surgery, especially cyclovertical muscle surgery, which might produce incyclotropia in one eye and excyclotropia in the contralateral eye; 2) Those that had an acquired skew deviation; 3) Those with an acquired ocular counter-roll, for example, a patients with acquired traumatic SOP in one eye and inferior rectus palsy in the contralateral eye; 4) Uncooperative patients during fundi photography, resulting from their heads failing to be aligned and the potential to produce a VOR; 5) Patients that had experienced any acquired lesions which might affect extraocular muscle function.
Data were collected including sex, age at surgery, complete ophthalmic examinations, systemic diseases, surgical treatments and outcomes. Pre- and post-operative ophthalmic examinations included best corrected visual acuity, cycloplegic refraction, intraocular pressure, slit-lamp biomicroscopy, and fundus examination. Ocular alignment measurements were assessed using the Hirschberg corneal reflection test, ocular motility function and the prism alternate cover test as performed at 6-m and 33-cm fixation. The Krimsky test was performed at 33-cm fixation for uncooperative patients and those with poor vision of 20/400 or worse. Ocular deviations of 25° in up- and down-gaze were measured to identify A-V patterns. Ocular motility function was graded on a 9-point scale, from -4 to +4. Abnormal head position was tested with use of a cervical range of motion device. Binocular function was measured with use of the Titmus stereoacuity test at near, and random dot stereograms and the synoptophore at distance.
Surgical Treatments
All surgeries were performed under general anesthesia. The selection of surgical procedures for these patients were similar to that used in the treatment of SOP, A-V patterns, DVD or other cyclovertical strabismus disorders. The selection of these procedures was based on the following considerations: 1) In patients showing an overelevation in adduction, an inferior oblique myectomy was the preferred choice; 2) A superior oblique tuck was used in patients with an underdepression in adduction; 3) If a DVD was coexistent, a superior rectus recession or inferior oblique anterior transposition was performed; 4) Horizontal recti muscle recession-resection surgery was included in cases of horizontal strabismus.
Statistical Analysis
A postoperative horizontal deviation of <10 prism diopters (PD) and vertical deviation of <5 PD in the primary position at final follow-up were considered a successful result. Statistical analyses were performed using the SPSS Statistics version 24.0 (IBM Corp., Armonk, NY, USA). Data were expressed as the mean±standard deviation. Parametric paired t-test and non-parametric Wilcoxon signed rank test were used for paired data. Non-parametric Mann-Whitney U test was used for unpaired data. A P value<0.05 was required for results to be considered statistically significant.
RESULTS
During the 2-year period included within our review, a total of 7008 patients received strabismus surgery. Of these, 28 patients (0.40%), including 12 males and 16 females met the criterion for inclusion in the study. The mean age at onset of strabismus was 3.0±3.7y (range 0.1-16y). The mean age at surgery was 12.4±9.4y (range 2.5-36y), with 21 of the patients being <20 years of age. Twelve patients had a history of wearing glasses. All patients had been previously misdiagnosed: 21 patients (2 with V-pattern exotropia) were misdiagnosed as SOP, 3 as inferior oblique overaction (2 with V-pattern exotropia and 1 with DVD), 2 as DVD (1 with V-pattern exotropia), 1 as superior oblique overaction with A-pattern exotropia and 1 as medial rectus palsy.
Clinical features included hyperdeviation (96.43%), outward deviation (82.14%), overelevation in adduction (75%), head tilt (46.43%), lateral eye deviation more prominent in up- versus down-gaze (17.85%), underdepression in adduction (17.85%), underelevation in adduction (17.85%), slow upward drift of either eye (10.71%), lateral eye deviation more prominent in down- versus up-gaze (3.57%) and limited adduction (3.57%). Anterior segment and fundus were normal in all patients. Preoperative exotropia was 26±24 PD (0 to 85 PD) and vertical deviation was 18±12 PD (range 0-40 PD) in the primary position. In addition to ocular counter-roll, other symptoms and signs were similar to that observed in SOP, A-V patterns, oblique overaction, DVD or medial rectus palsy. Thirteen patients displayed a head tilt toward the hypotropic eye, among whom one showed a face rotation toward the left side, with the remaining 15 patients showing no head tilt. None of the patients showed either vertical or horizontal diplopia or displacement of the visual world. Four (14.29%) patients had stereopsis (Cases 4, 12, 17, and 21), 22 (75%) lost binocular vision and 3 (10.71%) were uncooperative (Cases 2, 3, and 9).
Fundus photography revealed an incyclotorsion of the hypertropic eye and an excyclotorsion of the hypotropic eye in 14 patients, an excyclotorsion of the hypertropic eye and an incyclotorsion of the hypotropic eye (referred to as “reversed ocular torsion” in this report) in 13 patients and an incyclotorsion of the right eye and excyclotorsion of the left eye in 1 patient with no vertical misalignment. Mean degree of excyclotorsion was 12.2°±8.2° and incyclotorsion was 6.9°±5.8° (Table 1). The degrees of excyclotorsion were significantly greater than that of the contralateral incyclotorsion (Z=-0.624, P<0.05).
Table 1. The clinical characteristics in the patients with congenital ocular counter-roll.
| Case | Sex | Age at onset of strabismus (y) | Age at surgery (y) | BCVA (OD/OS) | Misdiagnosis | Preop. deviation (PD) | Bielschowsky head tilt test | AHP | Preop. fundus torsion | Surgery | Postop. deviation (PD) |
| 1 | F | 4 | 24 | 1.0/0.5 | SOP od | R/L 25 | Right+ | Toward left side | OD Ex15.1°, OS In5.1° | RSO tuck | ET2 R/L8 |
| 2 | F | 1 | 2.5 | Uncooperative | SOP os | XT8 L/R12 | Left + | Toward right side | OD Ex16°, OS In3.5° | LLR rec 10 mm+ LIO myectomy | Ortho |
| 3 | M | 1 | 5 | 0.8/0.8 | SOP os | XT13 L/R30 | Left+ | None | OD In20.3°, OS Ex12.9° | LIO anterior transposition | XT6 L/R6 |
| 4 | F | 1 | 5 | 0.9/0.9 | SOP od | R/L3 | Right+ | None | OD In0.3°, OS Ex11.6° | RSO tuck | Ortho |
| 5 | M | 8 | 14 | 1.5/1.5 | SOP os | XT40 L/R12 | Left+ | None | OD Ex11.3°, OS In3.3° | LLR rec 8.5 mm+LMR rec 7 mm+LIO posterior transposition | ET12 |
| 6 | F | 4 | 8 | 1.0/0.8 | SOP od | XT40 R/L25 | Right+ | None | OD In15.1°, OS Ex22.9° | BLR rec 8 mm+RIO anterior transposition | XT10 R/L10 |
| 7 | M | 4 | 7 | 1.0/1.0 | SOP os | XT30 L/R25 | Left+ | Toward right side | OD In7.0°, OS Ex20.4° | LIO myectomy+LSO tuck | ET6 |
| 8 | F | 1 | 9 | 1.0/1.0 | SOP os | L/R40 | Left+ | None | OD Ex13.2°, OS In19.5° | LIO myectomy+LSO tuck | R/L2 |
| 9 | M | 0.1 | 3 | Uncooperative | SOP ou | XT10 R/L40 | Right+ | Toward left side | OD In0.4°, OS Ex15.1° | RIO anterior transposition+LIO rec | Ortho |
| 10 | F | 1 | 17 | 1.0/1.0 | SOP od | XT35 R/L8 | Right+ | None | OD Ex14.8°, OS In2° | RLR rec 7 mm+RMR res 5 mm+ RIO myectomy | Ortho |
| 11 | F | 3 | 36 | 1.5/1.0 | SOP ou | XT50 R/L30 | Right+, left ± | Toward left side | OD Ex8°, OS In5° | BIO rec+BMR res 8 mm+LIR rec 6 mm | ET20 R/L10 |
| 12 | F | 0.1 | 5 | 1.0/0.9 | SOP od | XT5 R/L10 | Right+ | Head and face toward left side | OD Ex11.2°, OS In3.7° | RSO tuck | L/R3 |
| 13 | M | 0.1 | 32 | 1.0/1.0 | SOP od | XT50 R/L18 | Right+ | None | OD Ex8.7°, OS In4.1° | LLR rec 10 mm+LMR res 9 mm | Ortho |
| 14 | F | 3 | 6 | 1.0/1.0 | IOOA ou | XT35 | Negative | None | OD Ex13.2, OS In4.1° | RLR rec 8 mm+BIO myectomy | ET2 |
| 15 | M | 0.1 | 21 | 1.0/1.0 | Medial rectus palsy ou | XT66 R/L5 | Negative | None | OD Ex16.7°, OS In7.2° | LLR rec 14 mm+LMR res 10 mm | XT50 |
| 16 | F | 11 | 13 | 1.2/1.2 | IOOA od | XT45 R/L10 | Right+ | None | OD Ex9.1°, OS In0.4° | BLR rec 10 mm+RIO myectomy | Ortho |
| 17 | F | 1 | 9 | 1.0/1.0 | DVD ou | XT12 R/L3 | Negative | None | OD Ex16.9°, OS In1.6° | RIO anterior transposition | Ortho |
| 18 | F | 5 | 8 | 1.0/1.0 | DVD ou | XT20 R/L25 | Negative | None | OD Ex13.9°, OS In8.1° | RLR rec 7 mm+RSR rec 5 mm+LSO rec | Ortho |
| 19 | M | 2 | 4 | 0.6/0.6 | SOP os | L/R30 | Left+ | Toward right side | OD Ex14.2°, OS In9.1° | LIO anterior transposition | L/R5 |
| 20 | F | 1 | 5 | 1.0/1.0 | SOP os | XT8 L/R18 | Left+ | Toward right side | OD Ex13.4°, OS In5.4° | LIO myectomy | Ortho |
| 21 | M | 0.1 | 6 | 1.0/0.9 | SOP ou | R/L7 | Right+ | Toward left side | OD In13.5°, OS Ex15.3° | RSO tuck | L/R10 |
| 22 | M | 0.1 | 5 | 1.0/1.0 | SOP os | XT7 L/R30 | Left+ | Toward right side | OD Ex22.7°, OS In0.3° | LIO myectomy+LSO tuck | XT12 R/L6 |
| 23 | F | 0.1 | 23 | 1.0/FC30 cm | A-Exo+ SOOA ou | XT50 L/R20 | Negative | None | OD Ex13.7°, OS In4.7° | LLR rec 7 mm+LMR res 7 mm | ET12 |
| 24 | M | 5 | 12 | 1.0/1.0 | SOP os | XT7 L/R20 | Left+ | Toward right side | OD Ex13.3°, OS In7.1° | LIO anterior transposition | XT6 L/R8 |
| 25 | M | 16 | 28 | 1.0/0.9 | SOP os | XT66 L/R8 | Negative | None | OD Ex13.4°, OS In2° | BLR rec 8 mm+RMR res 6 mm+LIO myectomy | Ortho |
| 26 | F | 1 | 7 | 1.0/1.0 | SOP od | XT10 R/L20 | Right+ | Toward left side | OD Ex10.6°, OS In15° | LIO disinsertion+LSO tuck+LLR rec 6 mm | Ortho |
| 27 | F | 7 | 23 | 1.0/1.0 | IOOA od | XT85 R/L35 | Negative | None | OD Ex18.3°, OS In15.2° | LLR rec 10 mm+LMR res 7 mm | ET20 R/L15 |
| 28 | M | 3 | 6 | 1.0/1.0 | SOP os | XT40 L/R14 | Left+ | Toward right side | OD Ex10°, OS In9.1° | BLR rec 8 mm+LIO myectomy | ET10 L/R8 |
AHP: Abnormal head position; BCVA: Best-corrected visual acuity; BLR: Binocular lateral rectus; BMR: Binocular medial rectus; BIO: Binocular inferior oblique; ET: Esotropia; Ex: Excyclotorsion; FC: Finger counting; In: Incyclotorsion; IOOA: Inferior oblique overaction; L/R: Left eye is higher than right eye; LIO: Left inferior oblique; LIR: Left inferior rectus; LLR: Left lateral rectus; LMR: Left medial rectus; LSO: left superior oblique; Ortho: Orthotropia; od: Oculus dextrus; os: Oculus sinister; ou: Oculus uterque; PD: Prism dioptor, R/L: Right eye is higher than left eye; rec: Recession; res: Resection, RIO: Right inferior oblique; RLR: Right lateral rectus; RMR: Right medial rectus; RSO: Right superior oblique; RSR: Right superior rectus; SOOA: Superior oblique overaction; SOP: Superior oblique palsy; XT: Exotropia.
Physical examinations revealed one patient with scoliosis and one with a congenital ventricular septal defect that showed a developmental delay and underwent a repair surgery at 5 years of age. No other neurological symptoms and signs (e.g., dysarthria, hemiplegia ataxia, developmental delay, and mental retardation), hearing loss or spinal disease were observed in the remaining patients.
Surgical treatments included: 1) Lateral rectus recession combined with inferior oblique myectomy: 7 cases; 2) Lateral rectus recession and medial rectus resection: 4 cases; 3) Inferior oblique anterior transposition: 4 cases; 4) Superior oblique tuck surgery: 3 cases; 5) Inferior oblique myectomy combined with superior oblique tuck of the ipsilateral eye: 3 cases; 6) Inferior oblique myectomy-1 case; 7) Lateral rectus recession and medial rectus resection plus inferior oblique myectomy: 1 case; 8) Lateral rectus recession and medial rectus resection plus inferior oblique anterior transposition: 1 case; 9) Inferior oblique recession and medial rectus resection of both eyes plus inferior rectus resection of the right eye: 1 case; 10) Inferior oblique disinsertion and superior oblique tuck plus lateral rectus recession: 1 case; 11) Inferior oblique anterior transposition of one eye and inferior oblique recession of the contralateral eye: 1 case; 12) Lateral rectus recession and medial rectus resection combined with superior oblique tuck: 1 case.
At final follow-up, as performed over the period from 6mo to 2.5y after surgery, an excellent result was achieved in 20 patients. Horizontal deviation decreased by a mean of 26.0±27.6 PD and vertical deviation decreased by a mean of 15.1±10.4 PD. Torsion decreased by a mean of 4.0±4.1 degrees of excyclotorted eye and 6.6±6.8 degrees of incyclotorted eye, respectively. These results failed to achieve statistical significance as compared to preoperative torsion values (UEX=-1.133, P>0.05, UIN=-1.310, P>0.05). Most patients (n=23) developed normal ocular motility, while the remaining 5 showed mild motility defects. Of the 13 patients with abnormal head position, head tilt was no longer present in 9 cases after surgery, but 4 patients continued to show a residual head tilt. A typical case of congenital ocular counter-roll is presented in Figures 2 and 3.
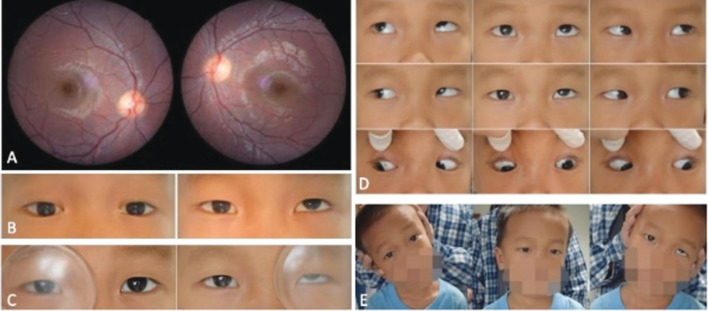
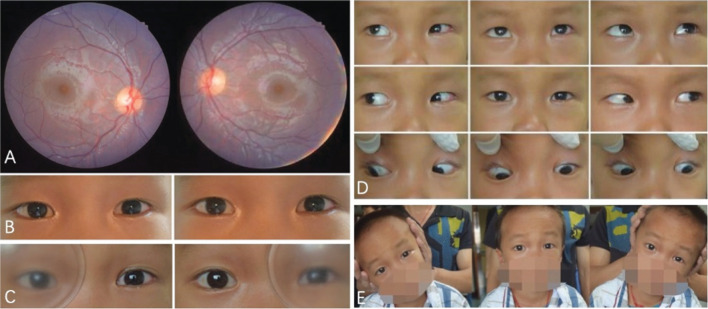
Figure 2. Preoperative clinical features of congenital ocular counter-roll (Case 3).
A: Fundus photography shows an incyclotorsion of the right eye and excyclotorsion of the left eye; B-E: The patient showed a left exotropia and hypertropia, head tilt to left, a scale of +2 overelevation in adduction of the left eye and a positive Bielschowsky head tilt test response.
Figure 3. Postoperative clinical features of Case 3.
A: The torsion was incyclotorsion in the right eye; B-D: The patient showed a residual exotropia of 6 PD and normal ocular motility; E: The head tilt dissipated and the Bielschowsky head tilt test response was negative.
DISCUSSION
In this study, we found that 0.4% of our strabismus surgery patients showed an excyclotorsion of one eye and incyclotorsion of the contralateral eye, as revealed with use of fundus photography. Guyton[8] proposed that ocular torsion was the key for understanding the different forms of cyclovertical strabismus disorders. Ocular torsion in patients with true unilateral congenital SOP is usually monocular with excyclotorsion of the hypertropic eye[7]. The clinical characteristics of true isolated SOP with excyclotorsion of the hypertropic eye would not change in different head positions (upright-supine test), and the contralateral eye should have no incyclotorsion due to normal intact VOR[9]. In fact, ocular counter-roll is a typical sign of skew deviation[10]. In addition to normal compensatory counter-roll, which occurs during head tilting[11]–[12], ocular counter-roll mainly presents in patients with skew deviation in normal upright positon. Skew deviation can result from any pathogenesis that may affect the VOR pathway, whereas only a congenital cause was found in our patients. Therefore, we diagnosed our patients as congenital ocular counter-roll.
In the absence of fundus photography, congenital ocular counter-roll might readily be misdiagnosed as any number of cyclovertical strabismus disorders (e.g., SOP, A-V patterns, DVD, and even medial rectus palsy). This point is quite evident in our current study, where all patients were initially misdiagnosed: 21 as SOP, 3 as inferior oblique overaction, 2 as DVD, 1 as A-pattern exotropia, and 1 as medial rectus palsy. Indeed, clinical ocular findings of congenital ocular counter-roll include symptoms similar to these conditions, such as hyperdeviation, outward deviation, overelevation in adduction, head tilt, lateral eye deviation more prominent in up- versus down-gaze, slow upward drift of either eye. In this regard, fundus photography represents a clinically valuable, if not indispensable, technique for the diagnosis of ocular counter-roll. Results from previous reports have indicated that a substantial amount of neurological damage and malformative syndromes were present in patients with A-V patterns, suggesting that some of these A-V patterns may, in fact, have been supernuclear disorders related to skew deviation[13]–[14]. Moreover, some cases with oblique muscle dysfunction and A-V patterns may possibly represent special subtypes of skew deviation[15]–[16]. The posterior semicircular canal has excitatory projections to the ipsilateral superior oblique and contralateral inferior rectus, and inhibitory projections to the ipsilateral inferior oblique and contralateral superior rectus. Thus, injury of posterior canal projections (on the right side, for example) would produce a left hypertropia (decreased excitation of left inferior rectus and inhibition of left superior rectus) and an right excyclotorsion (decreased excitation of right superior oblique and inhibition of right inferior oblique)[17]. Under such conditions, left hypertropia is greater in leftgaze. Further, head tilt to left would activate the left superior rectus and right inferior recuts, and thus increase the left hypertropia. All clinical features are consistent with the right inferior oblique palsy. It has been reported that lateral alternating acquired skew deviation can result from central otolithic dysfuncion[18]. Brodsky et al[6] reported that the subjective backward pitch, instead of the subjective tilt, would drive the eyes downgaze and mimic primary oblique muscle overaction and lateral alternating skew deviation. In this situation, torsional actions of the superior oblique muscle would produce ocular incyclotorsion, while vertical actions of both the inferior rectus and superior oblique muscles would result in overdepression. He also suggested that destruction of VOR pathways might present as DVD[19]. The mechanisms for this effect can include, but are not limited to, asymmetrical visual input rather than asymmetrical graviceptive input, pulley anomalies and sensory torsion[20]–[21]. Loss of binocular vision is considered as a possible reason for skew deviation in patients with accompanying sixth nerve palsy. That might be the same reason for our patients with the medial rectus palsy[22]–[23]. In addition, we found that one of our patients, who mimicked inferior oblique overaction with accompanying V-pattern exotropia, presented with ocular counter-roll without vertical deviation. To the best of our knowledge, no such case has ever been reported in the literature.
Of the 14 patients with an incyclotorsion of the hypertropic eye and excyclotorsion of the hypotropic eye, 12 showed a positive Bielschowsky head tilt test response. Such findings are similar to that of incomitant skew deviation and suggest an asymmetric injury within the otolithic pathways. Thirteen patients showed a reversed ocular torsion, indicating that a pathophysiological overlap with other disorders may be present. Dieterich and Brandt[24] reported that a prenuclear tegmental lesion could damage the cranial nerve nucleus or nerve fascicle and thus induce a combined prenuclear and fascicular lesion, leading to both skew deviation and superior oblique muscle palsy (Figure 4). Therefore, lesions involving VOR pathways, which extend from the medial longitudinal fasciculus to the ipsilateral trochlear nucleus, may result in an excyclotorsion of the ipsilateral eye due to superior oblique palsy[25]–[26]. An additional consideration, is that the fovea is located within the lower one third of the optic disc. The mean DFAs of normal control subjects were reported to be 6.3°[27]. When we evaluated fundus photographs using DFA, some located between center and the junction of lower one third of the optic disc were categorized into normal categories. This may provide a possible reason for the lower incyclotorting versus excyclotorting gain.
Figure 4. Anatomical structures of VOR and mechanisms of ocular tilt reaction.
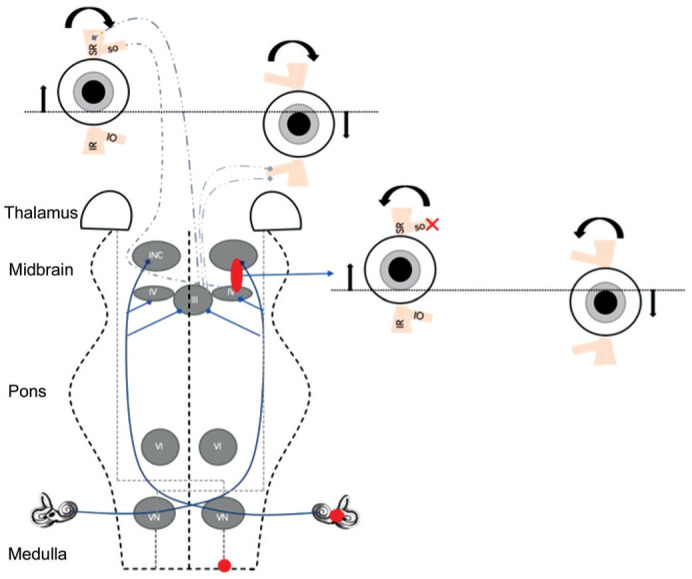
Lower brain stem lesions produce an inhibition of the ipsilateral graviceptive-ocular pathway (depression and excyclotorsion) and activation of the contralateral graviceptive-ocular pathway (elevation and incyclotorsion). INC: Interstitial nucleus of Cajal; III: Oculomotor nuclei; IV: Trochlear nuclei; VI: Abducens nuclei; VN: Vestibular nuclei; SO: Superior oblique; SR: Superior rectus; IO: Inferior oblique; IR: Inferior rectus.
For the ophthalmologist, congenital ocular counter-roll is quite different from that of acquired skew deviation (Table 2). When considering their etiologies, a number of salient differences exist between congenital ocular counter-roll versus acquired skew deviation. For example, age at onset of symptoms is younger in congenital cases and the head tilt in congenital ocular counter-roll is compensatory for vertical diplopia. Conversely, it is compensatory for altered subjective visual vertical in acquired skew deviation. Acquired skew deviation is transient and shows spontaneous recovery, whereas we found that none of our congenital ocular counter-roll patients showed such characteristics[28]. Moreover, a number of other neurological signs which are usually present in acquired skew deviation, remain absent or nondetectable in congenital cases.
Table 2. Congenital ocular counter-roll versus acquired skew deviation.
| Congenital ocular counter-roll | Acquired skew deviation |
| Congenital abnormality of VOR (possible) | Acute injury to VOR |
| Onset symptoms in childhood | Onset symptoms in adulthood |
| Incyclotorsion of one eye and excyclotorsion of another eye | Incyclotorsion of higher eye and/or excyclotorsion of the lower eye if present |
| No tilt of subjective visual vertical | Binocular tilt of subjective visual vertical |
| Head tilt compensatory for vertical diplopia (possible) | Head tilt secondary to a tilt of subjective visual vertical |
| Usually no other neurologic signs | Usually has other neurologic signs |
| Stable condition | Transient process and spontaneous recovery |
VOR: Vestibule-ocular reflex.
We hypothesize that the lesion associated with congenital ocular counter-roll mainly involves pathways corresponding with extraocular muscles and thus only produces ocular movement disorders. In our experience, the surgical procedures that were used to treat common vertical ocular misalignment also seemed to be effective and served as a stable treatment regime for congenital ocular counter-roll. An excellent surgical result was achieved in 71.4% of our patients.
The limitations in our study include: 1) The retrospective review nature of this study, can be subject to measurement and interpretation errors; 2) All our patients required strabismus surgery, which might introduce selection bias; 3) As the patients enrolled showed an obvious ocular counter-roll, this could underestimate the incidence of this condition. For example, some cases with a small degree of ocular counter-roll might also have a congenital ocular counter-roll; 4) Upright-supine test was not performed for our cases, therefore it fails to confirm whether it is a new form of skew deviation; 5) Detailed brain imaging information was not available due to the lack of neurological assessments and the congenital etiology of this condition; 6) Our patients were mainly Han Chinese who came from south China, which would introduce ethnic and geographical bias.
In conclusion, congenital ocular counter-roll is a rare supranuclear vertical strabismus. The possible mechanisms appear to involve congenital abnormalities which affects VOR pathways. However, neurological symptoms and signs are absent or inconspicuous in this condition. In addition to ocular counter-roll, the most salient clinical features include, but are not limited to, hyperdeviation, outward deviation, head tilt, lateral eye deviation more prominent in up- versus down-gaze, slow upward drift of either eye. Such symptoms may clinically mimic congenital SOP, primary oblique muscle dysfunction, A-V patterns and DVD. Fundus photography can be clinically useful, if not indispensable, for making a correct diagnosis after observing ocular counter-roll in both eyes.
Acknowledgments
Conflicts of Interest: Zhu BB, None; Wang F, None; Yan JH, None.
REFERENCES
- 1.Lee D, Kim WJ, Kim MM. Comparison of excyclotorsion following graded inferior oblique recession for primary versus secondary inferior oblique overaction. Int J Ophthalmol. 2020;13(8):1281–1286. doi: 10.18240/ijo.2020.08.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Donahue SP, Itharat P. A-pattern strabismus with overdepression in adduction: a special type of bilateral skew deviation? J AAPOS. 2010;14(1):42–46. doi: 10.1016/j.jaapos.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Kim DH, Kim H, Lim HT. The influence of ocular sighting dominance on fundus torsion in patients with unilateral congenital superior oblique palsy. Graefes Arch Clin Exp Ophthalmol. 2017;255(12):2473–2479. doi: 10.1007/s00417-017-3778-7. [DOI] [PubMed] [Google Scholar]
- 4.Anand K, Bharadwaj A, Dhiman S, Goel Y, Rastogi A, Agarwal R, Mishra M, Kumar P. Comparison of conventional and Hang-back methods of inferior oblique recession in V-pattern strabismus with inferior oblique overaction. Int J Ophthalmol. 2020;13(6):985–990. doi: 10.18240/ijo.2020.06.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi YY, Lee SY. A case of surgery for congenital superior oblique palsy with intorsion of nonparalized eye. Journal of The Korean Ophthalmological Society. 2003;44(4):1002–1009. [Google Scholar]
- 6.Brodsky MC, Donahue SP, Vaphiades M, Brandt T. Skew deviation revisited. Surv Ophthalmol. 2006;51(2):105–128. doi: 10.1016/j.survophthal.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Wong AM. Understanding skew deviation and a new clinical test to differentiate it from trochlear nerve palsy. J AAPOS. 2010;14(1):61–67. doi: 10.1016/j.jaapos.2009.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guyton DL. Ocular torsion reveals the mechanisms of cyclovertical strabismus: the Weisenfeld lecture. Invest Ophthalmol Vis Sci. 2008;49(3):847–857. 846. doi: 10.1167/iovs.07-0739. [DOI] [PubMed] [Google Scholar]
- 9.Parulekar MV, Dai S, Buncic JR, Wong AM. Head position-dependent changes in ocular torsion and vertical misalignment in skew deviation. Arch Ophthalmol. 2008;126(7):899–905. doi: 10.1001/archopht.126.7.899. [DOI] [PubMed] [Google Scholar]
- 10.Biotti D, Bidot S. Skew deviation and retinal photography. Neurology. 2011;77(24):2137. doi: 10.1212/WNL.0b013e31823d7698. [DOI] [PubMed] [Google Scholar]
- 11.Otero-Millan J, Treviño C, Winnick A, Zee DS, Carey JP, Kheradmand A. The video ocular counter-roll (vOCR): a clinical test to detect loss of otolith-ocular function. Acta Otolaryngol. 2017;137(6):593–597. doi: 10.1080/00016489.2016.1269364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramos de Miguel A, Zarowski A, Sluydts M, Ramos Macias A, Wuyts FL. The superiority of the otolith system. Audiol Neuro-Otol. 2020;25(1-2):35–41. doi: 10.1159/000504595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dickmann A, Parrilla R, Aliberti S, Perrotta V, Salerni A, Savino G, Petroni S. Prevalence of neurological involvement and malformative/systemic syndromes in A- and V-pattern strabismus. Ophthalmic Epidemiol. 2012;19(5):302–305. doi: 10.3109/09286586.2012.694553. [DOI] [PubMed] [Google Scholar]
- 14.Biglan AW. Strabismus associated with meningomyelocele. J Pediatr Ophthalmol Strabismus. 1995;32(5):309–314. doi: 10.3928/0191-3913-19950901-10. [DOI] [PubMed] [Google Scholar]
- 15.Fu T, Lu W. Clinical manifestations and treatment of skew deviation. Zhonghua Yan Ke Za Zhi. 2012;48(9):856–860. [PubMed] [Google Scholar]
- 16.Elavarasi A, Mani B. Vertical diplopia: skew deviation and medullary lesion. Ann Indian Acad Neurol. 2019;22(4):490. doi: 10.4103/aian.AIAN_46_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gufoni M, Vianini M, Casani AP. Analysis of the skew deviation to evaluate the period of onset of a canalolithiasis after macular damage. Front Neurol. 2020;11:572531. doi: 10.3389/fneur.2020.572531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biotti D, Barbieux M, Brassat D. Teaching Video NeuroImages: alternating skew deviation with abducting hypertropia following superior colliculus infarction. Neurology. 2016;86(9):e93–e94. doi: 10.1212/WNL.0000000000002425. [DOI] [PubMed] [Google Scholar]
- 19.Brodsky MC. Dissociated vertical divergence: a righting reflex gone wrong. Arch Ophthalmol. 1999;117(9):1216–1222. doi: 10.1001/archopht.117.9.1216. [DOI] [PubMed] [Google Scholar]
- 20.Demer JL. The orbital pulley system: a revolution in concepts of orbital anatomy. Ann N Y Acad Sci. 2002;956:17–32. doi: 10.1111/j.1749-6632.2002.tb02805.x. [DOI] [PubMed] [Google Scholar]
- 21.Moguel-Ancheita S, Castellanos-Pérez Bolde CG, Orozco-Gómez LP. Skew deviation. Strabismological diagnosis and treatment alternatives. Cir Cir. 2009;77(4):267–273. 249–255. [PubMed] [Google Scholar]
- 22.Slavin ML. Hyperdeviation associated with isolated unilateral abducens palsy. Ophthalmology. 1989;96(4):512–516. doi: 10.1016/s0161-6420(89)32865-x. [DOI] [PubMed] [Google Scholar]
- 23.Wong AM, Tweed D, Sharpe JA. Vertical misalignment in unilateral sixth nerve palsy. Ophthalmology. 2002;109(7):1315–1325. doi: 10.1016/s0161-6420(02)01067-9. [DOI] [PubMed] [Google Scholar]
- 24.Dieterich M, Brandt T. Ocular torsion and perceived vertical in oculomotor, trochlear and abducens nerve palsies. Brain. 1993;116(Pt 5):1095–1104. doi: 10.1093/brain/116.5.1095. [DOI] [PubMed] [Google Scholar]
- 25.Gold DR, Schubert MC. Ocular misalignment in dizzy patients-something's a-skew. J Neurol Phys Ther. 2019;43(Suppl 2):S27–S30. doi: 10.1097/NPT.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 26.Dresner SM, Kung NH, Palko JR, McJunkin JL, Goebel JA, van Stavern GP. Skew deviation and partial ocular tilt reaction due to intratympanic gentamicin injection, with review of the literature. Neuroophthalmology. 2017;41(5):268–270. doi: 10.1080/01658107.2017.1296469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim DH, Lim HT. Comparison of ocular torsion between congenital and acquired unilateral superior oblique palsy. Eye (Lond) 2019;33(10):1658–1663. doi: 10.1038/s41433-019-0476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hernowo A, Eggenberger E. Skew deviation: clinical updates for ophthalmologists. Curr Opin Ophthalmol. 2014;25(6):485–487. doi: 10.1097/ICU.0000000000000105. [DOI] [PubMed] [Google Scholar]