Abstract
Background
There is no universally accepted method to assess the pressure-generating capacity of inspiratory muscles in children on mechanical ventilation (MV), and no study describing its evolution over time in this population.
Methods
In this prospective observational study, we have assessed the function of the inspiratory muscles in children on various modes of MV. During brief airway occlusion maneuvers, we simultaneously recorded airway pressure depression at the endotracheal tube (ΔPaw, force generation) and electrical activity of the diaphragm (EAdi, central respiratory drive) over five consecutive inspiratory efforts. The neuro-mechanical efficiency ratio (NME, ΔPaw/EAdimax) was also computed. The evolution over time of these indices in a group of children in the pediatric intensive care unit (PICU) was primarily described. As a secondary objective, we compared these values to those measured in a group of children in the operating room (OR).
Results
In the PICU group, although median NMEoccl decreased over time during MV (regression coefficient − 0.016, p = 0.03), maximum ΔPawmax remained unchanged (regression coefficient 0.109, p = 0.50). Median NMEoccl at the first measurement in the PICU group (after 21 h of MV) was significantly lower than at the only measurement in the OR group (1.8 cmH2O/µV, Q1–Q3 1.3–2.4 vs. 3.7 cmH2O/µV, Q1–Q3 3.5–4.2; p = 0.015). Maximum ΔPawmax in the PICU group was, however, not significantly different from the OR group (35.1 cmH2O, Q1–Q3 21–58 vs. 31.3 cmH2O, Q1–Q3 28.5–35.5; p = 0.982).
Conclusions
The function of inspiratory muscles can be monitored at the bedside of children on MV using brief airway occlusions. Inspiratory muscle efficiency was significantly lower in critically ill children than in children undergoing elective surgery, and it decreased over time during MV in critically ill children. This suggests that both critical illness and MV may have an impact on inspiratory muscle efficiency.
Keywords: Mechanical ventilation, Diaphragm, Inspiratory muscle dysfunction, Electrical activity of the diaphragm, Children, Intensive care
Background
Critically ill children frequently require support with mechanical ventilation (MV) which allows for an improvement in gas exchange and a decrease in work of breathing. It is, however, imperative to limit its duration because of associated severe complications which can increase the duration of MV, length of intensive care unit stay, and therefore costs. In children, these complications classically include nosocomial infections, tracheal injury, lung injury, hemodynamic effects of positive intrathoracic pressures, impact of sedation, etc. [1]. The impact of MV on the function of respiratory muscles, previously overlooked, is now a growing concern. In ICU patients, the function of the diaphragm, as with other striated muscles, can be adversely affected by critical illness and therapies (ICU-acquired diaphragm dysfunction, ICU–DD) [2], and also more specifically by MV itself (ventilator-induced diaphragm dysfunction, VIDD) [3]. Diaphragm injury can result from insufficient respiratory effort secondary to over-assistance by MV [4], from excessive inspiratory effort due to under-assistance leading to fatigue [5], or finally from contractile activation, while the muscle is lengthening (e.g., during asynchrony or hyperinflation) [6]. Studies in both animal models and humans have shown that MV is associated with a series of molecular changes in the diaphragm muscle [7]. A decrease in its force-generating capacity ensues [8–10], which is then followed by the development of micro- [11, 12] and macroscopic atrophy [13–18] in muscle fibers leading to even greater muscle weakness [9, 12, 19].
ICU–DD is described in both early [10] and late [20, 21] phases of critical illness, and its risk factors are numerous. The majority of adult patients present severe diaphragmatic dysfunction on admission to the ICU, before any prolonged duration of MV [10]. VIDD is highly prevalent in adult critical care (63–84% of patients depending on the phase of critical illness) [10, 20–23] and is associated with worse outcomes such as ventilation weaning failure [20, 21, 24, 25], longer duration of MV [8, 23, 24, 26, 27], prolonged ICU admission [27], and increased mortality [21, 23, 26, 28].
Interestingly, respiratory physiology in children has some specific features which may render the diaphragm particularly susceptible to dysfunction. Because of a more compliant abdomen and a smaller area of apposition between the diaphragm and the rib cage, contraction of the diaphragm in infants does not result in the same degree of expansion of the lower ribs as in adults [29]. In addition, the highly compliant chest wall [30] and horizontal insertion of the ribs can result in chest wall distortion during inspiration in the context of rapid eye movement sleep [31] or respiratory distress. Combined with small distal airways, this relatively high parietal compliance in neonates and infants requires that end-expiratory lung volume be maintained above the relaxation volume of the respiratory system [32], referred to as dynamic hyperinflation. This is achieved by expiratory airflow retardation resulting from the contraction of laryngeal muscles (in children without an artificial airway) or by persistent activation of the diaphragm during expiration [32]. The diaphragm may therefore be active during both inspiration and expiration [33, 34]. In contrast, the diaphragm is very frequently inactive during pediatric conventional MV [35].
The methods used in the assessment of inspiratory muscle function in children are not well established [36] and—to the best of our knowledge—no study has described the evolution of the efficiency of these muscles in critically ill children on MV.
In the present study, our primary objective was to test the hypothesis that inspiratory muscle efficiency decreases over time in mechanically ventilated critically ill children during the first 3 days of invasive ventilation. We first developed a standardized method to measure inspiratory muscle function in this setting (objective 1a) using the airway pressure at the endotracheal tube (Paw), the electrical activity of the diaphragm (EAdi), and the Paw/EAdi ratio which provides an estimate of the ability to generate pressure normalized to neural drive (neuro-mechanical efficiency, NME) [37]. We subsequently determined the evolution of Paw and NME over time in critically ill children on MV in the PICU (objective 1b). As a secondary objective, we compared these indices of inspiratory muscle function in this population to a group of healthy children briefly ventilated during general anesthesia for elective surgery (objective 2).
Methods
This was a prospective single-center observational study performed in a tertiary academic center, in both the pediatric intensive care unit (PICU) and the operating room (OR). Approval by the Ethics Committee of the CHU Sainte-Justine Research Center was granted before initiating enrollment (2017–1534). Written informed consent was obtained from the parents/guardians by a member of the research team.
Study population
In the PICU group, inclusion criteria consisted of children (defined as age between 1 week and 18 years) on invasive ventilation for less than 24 h and for which extubation was not planned in the following 24 h. Inclusion criteria in the OR group consisted of children with no chronic or acute respiratory disease undergoing endotracheal intubation for elective otorhinolaryngological surgery without planned use of neuromuscular blockade. In both groups, we excluded pre-existing conditions with a possible impact on inspiratory muscle function (global neuromuscular disease, cervical spine injury, bi-hemispheric or brain stem lesions, known diaphragmatic disease, uni- or bi-lateral phrenic paralysis, recent thoracic surgery, recent multiple rib fractures), patients in whom the placement of a nasogastric tube was contraindicated (trauma or recent surgery in cervical or nasopharyngeal regions, severe coagulation disorder), in whom muscle function was artificially suppressed (use of neuromuscular blockade in the 2 h prior to inclusion), or in whom life-sustaining treatment was being withheld.
Study protocol
After enrollment, a dedicated 6Fr or 8Fr nasogastric catheter (Maquet critical care, Solna, Sweden) was inserted to a depth determined by a validated equation and adjusted using dedicated software on the Servo-i ventilator, which then processed and displayed the EAdi signal [38], as per the manufacturer’s recommendations. Patients were placed in a supine position, and the respiratory circuit was assessed for leaks (all had a cuffed endotracheal tube). If needed, an opioid dose was administered (as prescribed by the treating team) and the endotracheal tube was suctioned. A low dead space (3.2 ml) pneumatic occlusion valve (2820 Series, Hans Rudolph, Southport, UK) was installed between the ventilator circuit and the endotracheal tube. An expiratory occlusion maneuver was performed (at the current level of PEEP in the PICU group, without PEEP in the OR group), and we simultaneously recorded negative Paw generated by the patient and EAdi signal over 5 consecutive breaths (Fig. 1). The maneuvers were subsequently repeated three times with at least a 1-min interval. The first measurement of diaphragm contractile strength was conducted as soon as possible after inclusion, within 24 h of intubation. Measurements were then repeated as close as possible to the following time points after the first measurement: 12 h, 24 h, 48 h and 72 h or until extubation/death. In the OR group, only one measurement was performed immediately after intubation and before surgery. Clinical data were recorded at baseline and at each measurement. Relevant outcome measures including mortality, extubation failure, prolonged (> 72 h) post-extubation non-invasive ventilation (NIV), and PICU length of stay were later assessed at the time of discharge from PICU.
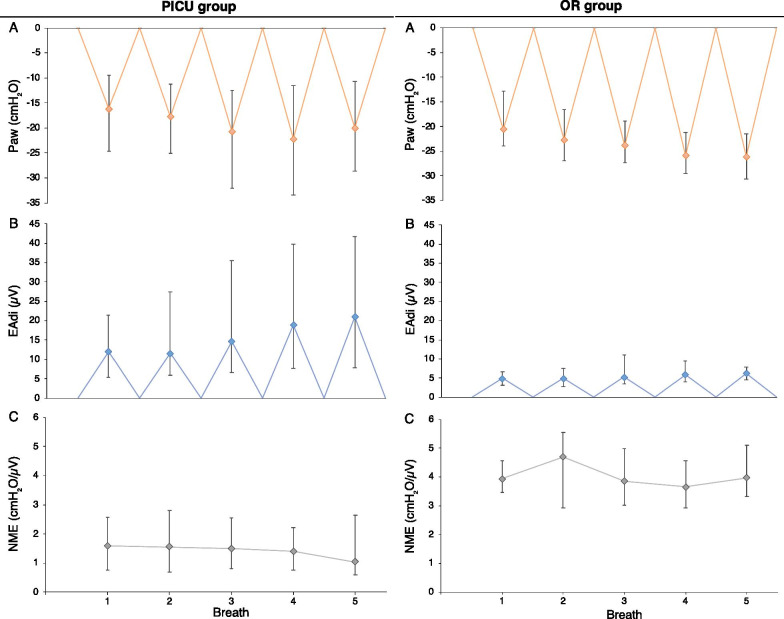
Fig. 1.
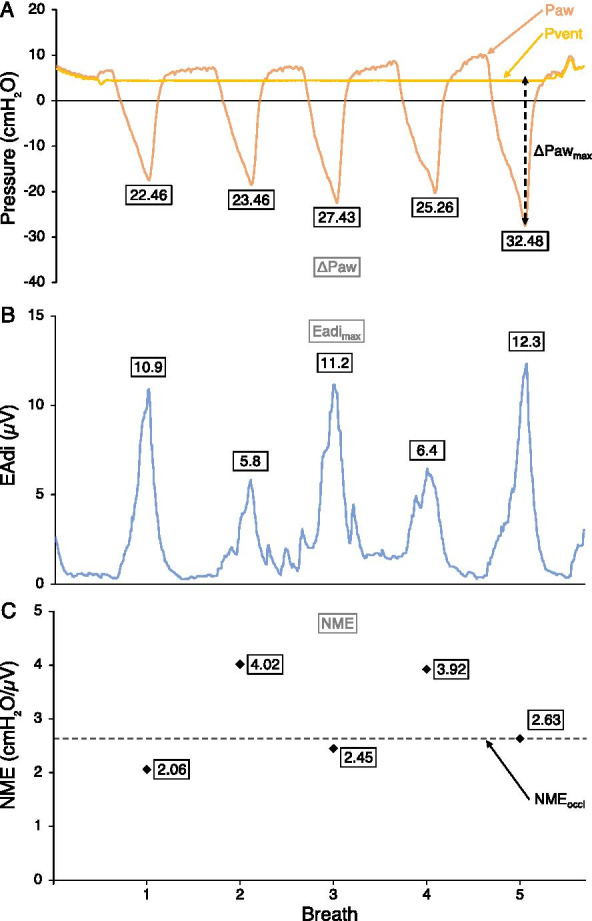
Example of recorded signals and calculated variables during an occlusion maneuver. Paw denotes airway pressure, Pvent pressure on ventilator circuit, EAdi electrical activity of the diaphragm, NME neuro-mechanical efficiency ratio (defined as ΔPaw divided by EAdimax). A Paw and Pvent over time, with ΔPaw values specified for each breath, dotted arrow shows ΔPawmax. B EAdi over time, with EAdimax values specified for each breath. C NME values for each breath, with the median of all 5 values (NMEoccl) as a dotted line
Data acquisition
EAdi waveforms were acquired from the Servo-i ventilator (Maquet critical care, Solna, Sweden) via a RS232 serial port. Pressure measurements were taken with a manometer connected to the endotracheal tube via the occlusion valve. The signals were simultaneously displayed and recorded using dedicated software (NeuroVent Research, Toronto, Canada). Baseline values of EAdi (maximum EAdi value in each minute) were also extracted from the ventilator for up to 60 min before each measurement in the PICU group. For each breath during each occlusion maneuver, the peak value of EAdi was recorded (EAdimax) as well as the difference in pressure between the lowest Paw and the preceding end-expiratory pressure (ΔPaw). In order to compensate for central respiratory drive, a neuro-mechanical efficiency ratio (NME) was computed by dividing ΔPaw by EAdimax for each breath (Fig. 1). The most reliable value of ΔPaw and NME to report for a given occlusion maneuver was determined by assessing, using coefficients of variation (CoV), the within-measurement variability of different metrics over three occlusion maneuvers (first breath, last breath, breath with largest ΔPaw deflection, breath with largest NME value, and median value over all breaths) in the PICU group. A summary of variables used in this article is provided to assist the reader (Table 1).
Table 1.
Nomenclature of variables used
| Paw | Pressure signal recorded at endotracheal tube |
| ΔPaw | Difference between the lowest Paw during an occluded breath and preceding end-expiratory Paw |
| ΔPawmax | Largest ΔPaw deflection amongst 5 breaths of an occlusion maneuver |
| Maximum ΔPawmax | Largest ΔPawmax deflection over 3 occlusion maneuvers of a single recording in time |
| ΔPawtwitch | Pressure decrease at occluded endotracheal tube generated by magnetic stimulation of the phrenic nerves |
| EAdi | Electrical signal recorded by electrodes in esophagus |
| EAdimax | Peak value of EAdi during an occluded breath |
| NME | Ratio of ΔPaw to EAdimax for an occluded breath |
| NMEoccl | Median NME value amongst 5 breaths of an occlusion maneuver |
| Median NMEoccl | Median NMEoccl value over 3 occlusion maneuvers of a single recording in time |
Sample size
At the time of designing the study, no data on inspiratory muscle efficiency in children on MV were available. In adult patients, data on VIDD are scant but Jaber et al. [9] demonstrated a strong and homogenous decrease in the strength of the diaphragm over 5–6 days of MV with only 6 patients. In this context, a sample size of 20 patients was chosen for the PICU group in order to improve external validity. In the OR group, low heterogeneity was expected and a convenient sample of 10 patients was selected.
Statistical analyses
Data were reported as median (first–third quartiles, Q1–Q3), unless stated otherwise. Linear mixed-effects models were then used to explore the effect of time on MV on maximum ΔPawmax and median NMEoccl, using time as variable with a fixed effect, and individual patient as variable with a random effect. Aiming to weigh the impact of critical illness on inspiratory muscle function, independently from MV, a Mann–Whitney U test was run to determine if there were significant differences in maximum ΔPawmax and median NMEoccl between the first measurement of the PICU group and the only measurement of the OR group. The level of significance for all statistical tests was set at p < 0.05. Statistical analysis was performed using SPSS (SPSS Statistics, Version 25. Armonk, NY: IBM Corp.) and Stata (Stata Statistical Software, Release 13. College Station, TX: StataCorp LLC.) software.
Results
Patients were recruited between October 2017 and September 2019. In the PICU group, 223 consecutive intubated patients were screened, 50 met the inclusion and exclusion criteria, 36 families provided consent, and the research team was available to make measurements in 20 patients. Table 2 describes patient characteristics in the PICU group. One patient had severe meningitis and was excluded from the analysis due to a lack of spontaneous breathing activity at any time point. Patients were on invasive ventilation for 63.9 h (Q1–Q3 50.4–77.4) and stayed in the PICU for 5.3 days (Q1–Q3 4–8.8). In the OR group, 12 consecutive eligible patients were approached, 10 families provided consent, and measurements were made in all 10 patients. Because of difficulties in promptly achieving appropriate nasogastric tube positioning between induction of anesthesia and surgery, EAdi signal could not be appropriately recorded for 3 patients in the OR group and NME was therefore not computed. Table 3 describes patient characteristics in the OR group. In total, 59 measurements were made, 147 occlusions performed and 625 breaths analyzed in the PICU group; 10 measurements were made, 30 occlusions performed and 150 breaths analyzed in the OR group.
Table 2.
Patient characteristics (PICU group, 19 patients)
| Age (months), median (Q1–Q3) | 13.7 (1.5–34) |
| Weight (kg), median (Q1–Q3) | 11 (3.8–17.3) |
| Sex, male (%) | 12 (63.2%) |
| Comorbidity, n (%) | |
| Prematurity | 6 (31.6%) |
| Previous episode of invasive ventilation (within 7 days of intubation) | 3 (15.8%) |
| Reason for PICU admission, n (%) | |
| Neurological (traumatic brain injury) | 1 (5.3%) |
| Neurological (excluding traumatic brain injury) | 4 (21.1%) |
| Respiratory-upper airway | 4 (21.1%) |
| Respiratory-lower airway/pulmonary | 7 (36.8%) |
| Sepsis/shock | 1 (5.3%) |
| Other | 2 (10.5%) |
| Reason for intubation, n (%) | |
| Neurological | 4 (21.1%) |
| Apnea | 3 (15.8%) |
| Respiratory-upper airway | 4 (21.1%) |
| Respiratory-lower airway/pulmonary | 6 (31.6%) |
| Hemodynamics | 1 (5.3%) |
| Procedure | 1 (5.3%) |
| Drugs used during study period, n (%) | |
| Paralysis (excluding for intubation) | 5 (26.3%) |
| Corticosteroids | 8 (42.1%) |
| Inotropes/vasodilators | 5 (26.3%) |
| Spontaneous mode used during MV episode (NAVA/PSV), n (%) | 14 (73.7%) |
| Number of measurements, median (Q1–Q3) | 3 (2.5–4) |
| PICU outcomes | |
| Duration of MV (hours), median (Q1–Q3) | 63.9 (50.4–77.4) |
| Reintubation within 24 h of extubation, n (%) | 0 (0%) |
| Rescue NIV for more than 72 h post-extubation, n (%) | 2 (10.5%) |
| PICU length of stay (days), median (Q1–Q3) | 5.3 (4–8.8) |
| Died during PICU admission, n (%) | 0 (0%) |
PICU pediatric intensive care unit, Q1–Q3 first and third quartiles, NAVA neurally adjusted ventilatory assist, PSV pressure-support ventilation, MV mechanical ventilation, NIV non-invasive ventilation
Table 3.
Patient characteristics (OR group, 10 patients)
| Age (months), median (Q1–Q3) | 59.3 (46.6–65.8) |
| Weight (kg), median (Q1–Q3) | 17.9 (13.6–23) |
| Sex, male (%) | 5 (50%) |
| Comorbidity, n (%) | |
| Prematurity | 1 (10%) |
| Pediatric-adapted ASA-PS score, median (Q1–Q3) | 2.5 (2–3) |
| Analgesia and sedation received for induction | |
| Sevoflurane, n (%) | 10 (100%) |
| Opioids-fentanyl, n (%), median dose (mcg/kg) (Q1–Q3) |
4 (40%) 1 (0.8–1.1) |
| Opioids-remifentanil, n (%), median dose (mcg/kg) (Q1–Q3) |
4 (40%) 1.5 (1.5–2.8)a |
| Benzodiazepines, n (%) | 0 (0%) |
| Propofol, n (%), median dose (mg/kg) (Q1–Q3) |
10 (100%) 1.9 (1.8–2.5)a |
| Dexmedetomidine, n (%), median dose (mcg/kg) (Q1–Q3) |
4 (40%) 0.5 (0.4–0.6) |
| Ketamine, n (%), dose (mg/kg) |
1 (10%) 0.5 |
| Other drugs received before measurement | |
| Dexamethasone, n (%), median dose (mg/kg) (Q1–Q3) |
10 (100%) 0.1 (0.1–0.1) |
| Duration of MV on first measurement (minutes), median (Q1–Q3) | 7.6 (2.6–12.4) |
| Maximum ΔPawmax on first measurement (cmH2O), median (Q1–Q3) | 31.3 (28.5–35.5) |
| Median NMEoccl on first measurement (cmH2O/µV), median (Q1–Q3) | 3.6 (3.5–4.2) |
| Hospital length of stay (days), median (Q1–Q3) | 1.5 (1–2.8) |
OR denotes operating room, Q1–Q3 first and third quartiles, ASA-PS American Society of Anesthesiologists physical status [61], MV mechanical ventilation, ΔPawmax maximum inspiratory airway pressure deflection over 5 occluded breaths, NMEoccl median neuro-mechanical efficiency ratio (defined as inspiratory airway pressure divided by peak electrical activity of the diaphragm) over 5 occluded breaths
aOne patient received drugs as continuous infusions and accurate doses could not be reported
Clinical parameters and ventilator settings at each measurement in the PICU group are shown in Table 4. First measurements for each patient were made at 20.7 h (Q1–Q3 13.9–21.7). A median of 39.2 h (Q1–Q3 22.9–44.9) elapsed between the first and the last measurement. The last measurement was obtained at a median of 4.8 h (Q1–Q3 1.5–25) before extubation. Spontaneous modes of ventilation (pressure-support ventilation, PSV or neurally adjusted ventilatory assist, NAVA) were increasingly used in the later measurements. Baseline EAdi in the 60 min before the last measurement was 9.3 µV (Q1–Q3 6.6–13.7) compared to 3.8 µV (Q1–Q3 2.9–7.2) before the first measurement.
Table 4.
Clinical condition, ventilatory parameters, and recorded values at each measurement (PICU group)
| All | Measurement 1 | Measurement 2 | Measurement 3 | Measurement 4 | |
|---|---|---|---|---|---|
| Number of measurements | 59 | 19 | 18 | 14 | 8 |
| Duration of MV at measurement (hours), median (Q1–Q3) | 34.7 (22.9–49.6) | 20.7 (13.9–21.7) | 33.5 (30.4–38.4) | 49.6 (43.1–59.7) | 69.3 (58.4–80.8) |
| PELOD-2 score, median (Q1–Q3) | 8 (6–9) | 9 (7.5–11.5) | 7 (5.3–8.8) | 7 (5.3–8) | 8 (6.5–8.3) |
| Sedation used within 4 h before measurements, n (%) | |||||
| Opioids | 52 (88.1%) | 18 (94.7%) | 17 (94.4%) | 11 (78.6%) | 6 (75%) |
| Benzodiazepines | 17 (28.8%) | 5 (26.3%) | 5 (27.8%) | 5 (35.7%) | 2 (25%) |
| Propofol | 1 (1.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (12.5%) |
| Dexmedetomidine | 32 (54.2%) | 11 (57.9%) | 11 (61.1%) | 9 (64.3%) | 1 (12.5%) |
| Total opioid received before measurements, n (%), median morphine equivalent dose (mg/kg) (Q1–Q3) | |||||
| Within 4 h before measurements |
52 (88.1%) 0.28 (0.15–0.53) |
18 (94.7%) 0.45 (0.15–0.54) |
17 (94.4%) 0.4 (0.17–0.53) |
11 (78.6%) 0.23 (0.16–0.34) |
6 (75%) 0.24 (0.18–0.34) |
| Within 30 min before measurements |
38 (64.4%) 0.08 (0.04–0.14) |
13 (68.4%) 0.08 (0.05–0.14) |
13 (72.2%) 0.08 (0.05–0.14) |
7 (50%) 0.03 (0.02–0.07) |
5 (62.5%) 0.12 (0.08–0.19) |
| Sedation scores at measurements, median (Q1–Q3) | |||||
| RASS | − 1 (− 2 to 1) | − 1 (− 3 to 0.5) | − 1 (− 1.5 to − 1) | − 1 (− 1.5 to − 0.8) | 2 (2–2) |
| COMFORT-B | 12 (10–14) | 12 (9–13) | 12 (9.8–13) | 12 (11–13.8) | 14 (12–17.3) |
| Ventilation mode, n (%) | |||||
| Assist, volume-control | 6 (10.2%) | 3 (15.8%) | 3 (16.7%) | 0 (0%) | 0 (0%) |
| Assist, pressure-control | 13 (22%) | 5 (26.3%) | 4 (22.2%) | 3 (21.4%) | 1 (12.5%) |
| Assist, pressure-regulated volume control | 13 (22%) | 6 (31.6%) | 4 (22.2%) | 1 (7.1%) | 2 (25%) |
| Support, pressure-control (PSV) | 15 (25.4%) | 4 (21.1%) | 4 (22.2%) | 5 (35.7%) | 2 (25%) |
| Support, neurally adjusted (NAVA) | 12 (20.3%) | 1 (5.3%) | 3 (16.7%) | 5 (35.7%) | 3 (37.5%) |
| Ventilation parameters | |||||
| Tidal volume (ml/kg), median (Q1–Q3) | 6.5 (5.2–7.8) | 6.5 (5.4–7.4) | 6.9 (6.2–8.6) | 6.6 (5.2–8.1) | 5.7 (5–6.6) |
| Respiratory rate above set, for non-spontaneous modes (%), median (Q1–Q3) | 12.4% (3.3–28.9%) | 8.7% (1.4–27.9%) | 13.3% (7.3–25.7%) | 2.2% (0–33.3%) | 24% (19.1–93.3%) |
| NAVA level (cmH2O/µV), median (Q1–Q3) | 0.6 (0.5–1) | 0.5 | 0.5 (0.5–1) | 0.8 (0.5–1) | 0.6 (0.6–0.8) |
| Delta pressure (cmH2O), median (Q1–Q3) | 11 (6–14.5) | 12 (8.5–18) | 11 (8.5–14.8) | 7.5 (5.3–12) | 5.5 (3.8–12) |
| PEEP (cmH2O), median (Q1–Q3) | 6 (5–8) | 6 (5–8.5) | 7 (5–8) | 6.5 (5.3–7) | 6 (5.8–6.3) |
| FiO2 (%), median (Q1–Q3) | 35% (25–45%) | 40% (25–55%) | 32.5% (22–49%) | 30.5% (25–40%) | 35.5% (30–43%) |
| Ventilation effectiveness | |||||
| SpO2 (%), median (Q1–Q3) | 99% (96–100%) | 98% (96–100%) | 100% (99–100%) | 96.5% (96–99%) | 99% (97–100%) |
| pH, median (Q1–Q3) | 7.39 (7.35–7.42) | 7.4 (7.36–7.43) | 7.37 (7.34–7.43) | 7.39 (7.35–7.41) | 7.39 (7.37–7.42) |
| PCO2 (mmHg), median (Q1–Q3) | 43.9 (37.8–52.5) | 42.1 (35.7–50.1) | 43.1 (37.6–50.2) | 44.9 (40.9–54.9) | 47.3 (43.1–55.4) |
| Median baseline EAdimax 60 min before measurement (µV), median (Q1–Q3) | 5.7 (2.9–10) | 3.8 (2.9–7.2) | 6.5 (2.7–10.5) | 5.3 (2.9–11.9) | 9.3 (6.6–13.7) |
| Maximum ΔPawmax (cmH2O), median (Q1–Q3) | 28.7 (20.8–55.4) | 35.1 (21–58) | 26.7 (21.1–43.1) | 27.8 (20.9–41.1) | 47.2 (22.2–73.1) |
| Median NMEoccl (cmH2O/µV), median (Q1–Q3) | 1.6 (0.9–2.6) | 1.8 (1.3–2.4) | 1.9 (1.4–2.6) | 1.3 (0.9–2.7) | 0.9 (0.7–1.6) |
PICU denotes pediatric intensive care unit, Q1–Q3 first and third quartiles, MV mechanical ventilation, PELOD pediatric logistic organ dysfunction, RASS Richmond agitation–sedation scale, PSV pressure-support ventilation, NAVA neurally adjusted ventilatory assist, PEEP positive end-expiratory pressure, FiO2 fractional concentration of inspired oxygen, SpO2 oxygen saturation, PCO2 blood carbon dioxide pressure, EAdimax peak electrical activity of the diaphragm, ΔPawmax maximum inspiratory airway pressure deflection over 5 occluded breaths, NMEoccl median neuro-mechanical efficiency ratio (defined as inspiratory airway pressure divided by peak electrical activity of the diaphragm) over 5 occluded breaths
Assessment of inspiratory muscle function (objective 1a)
To synthesize the evolution of ΔPaw, EAdimax and NME over 5 occluded breaths, medians of all recordings are represented in Fig. 2 for both groups. ΔPaw tends to increase progressively over each breath of the occlusion maneuver (Fig. 2A). This is matched by an increase in respiratory drive, EAdimax (Fig. 2B). The resulting NME value is therefore relatively stable (Fig. 2C, right). Of note, on the last breath, the increase in EAdimax was not paralleled by an increase in ΔPaw, resulting in a decrease in NME (Fig. 2C, left). The variability of the different metrics assessing ΔPaw and NME for each occlusion maneuver in the PICU group is shown in Table 5. For ΔPaw, the value corresponding to the breath with the largest maximum inspiratory airway pressure deflection (ΔPawmax) exhibited the lowest variability (CoV of 26.1%) and was used to represent ΔPaw for a single occlusion maneuver. The maximum value of the three occlusion maneuvers was then used to represent ΔPawmax for a given recording in time. For NME, the median value of the 5 breaths in each occlusion maneuver (NMEoccl) exhibited the lowest variability (CoV of 23.7%) and was used to represent NME for a single occlusion maneuver. The median value of the three occlusion maneuvers was then used to represent NMEoccl for a given recording in time. To assess the impact of the number of breaths on median NMEoccl, we repeated the calculation using only the first 4 breaths and obtained values that were very closely correlated to those calculated on 5 breaths (R2 0.98).
Fig. 2.
Median evolution of ΔPaw, Eadimax and NME over the 5 occluded breaths in both groups. Data represented as median (dots) and first–third quartiles (whiskers). A ΔPaw. B EAdimax. C NME. Left: pediatric intensive care unit (PICU) group, right: operating room (OR) group
Table 5.
Variability of different metrics of ΔPaw and NME in the PICU group
| Mean coefficient of variation | |||||
|---|---|---|---|---|---|
| ΔPaw | NME | ||||
| 1 | Maximum ΔPaw | 26.1% | 1 | Median NME | 23.7% |
| 2 | Median ΔPaw | 26.3% | 2 | Maximum ΔPaw | 26.8% |
| 3 | Last breath | 29.8% | 3 | Maximum NME | 29.8% |
| 4 | Maximum NME | 30.3% | 4 | Last breath | 33.8% |
| 5 | First breath | 35.5% | 5 | First breath | 36.8% |
PICU denotes pediatric intensive care unit, ΔPaw maximum inspiratory airway pressure deflection, NME neuro-mechanical efficiency ratio (defined as inspiratory airway pressure divided by peak electrical activity of the diaphragm)
Evolution of inspiratory muscle function over time (objective 1b)
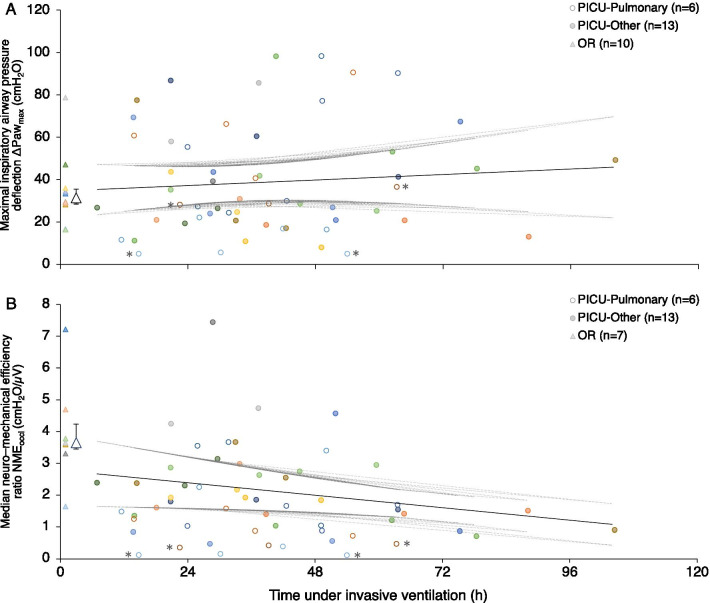
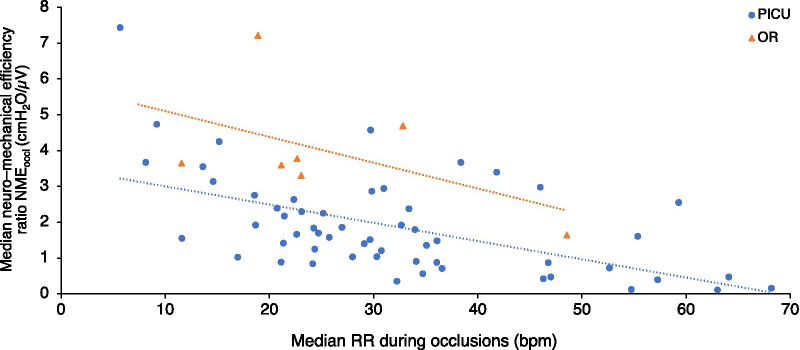
The evolution of inspiratory muscle strength (ΔPawmax) for patients in the PICU group is shown in Fig. 3A. There was no significant change in maximum ΔPawmax over time on MV, with a regression coefficient of 0.109 (95% confidence interval − 0.21 to 0.43, p = 0.50). Of the 8 patients (42%) in the PICU group who were not capable of generating a maximum ΔPawmax ≥ 30 cmH2O on their last measurement, only 3 could do so on their earliest measurement. The evolution of inspiratory muscles efficiency (NMEoccl) for patients in the PICU group is shown in Fig. 3B. There was a small but significant decrease in median NMEoccl over time on MV, with a regression coefficient of − 0.016 (95% confidence interval − 0.031 to − 0.002, p = 0.03). The evolution of inspiratory muscle function displayed similar patterns in patients intubated for a lower airway or pulmonary indication versus those intubated for other indications (Fig. 3). Of note, no association was observed between the respiratory rate or the EAdi recorded before measurements and the evolution of inspiratory muscle efficiency (data not shown). However, there was a significant negative correlation (r = − 0.55 in the PICU group and r = − 0.51 in the OR group) between the median frequency of respiratory efforts during occlusion maneuvers and the median NMEoccl (Fig. 4) for each measurement.
Fig. 3.
Inspiratory muscle function over time. A Maximum inspiratory airway pressure deflection ΔPawmax. B Median neuro-mechanical efficiency ratio NMEoccl. ΔPawmax denotes maximum inspiratory airway pressure deflection, NMEoccl median neuro-mechanical efficiency ratio, PICU pediatric intensive care unit (data points marked by empty circles for patients intubated for a lower airway or pulmonary indication and full circles for patients intubated for other indications), OR operating room (data points marked by triangles, group median by large triangle, and first–third quartiles by whiskers). Each color represents an individual patient. The fixed portion of the linear prediction of the mixed model is shown (solid black line) as well as the individual upper and lower 95% confidence intervals (dotted gray lines). *: patients who required non-invasive ventilation continuously for 72 h after extubation
Fig. 4.
Correlation between the median respiratory rate measured during occlusion maneuvers and the median NMEoccl for each measurement in both groups. NMEoccl denotes median neuro-mechanical efficiency ratio, PICU pediatric intensive care unit (data points marked by circles), OR operating room (data points marked by triangles). Dotted lines of best fit according to method of least squares
None of the 19 patients required reintubation within 24 h of extubation. Following extubation, 7 patients required NIV for ≤ 24 h, 1 patient required NIV for 32 h, and 2 patients required NIV for > 72 h. Interestingly, these 2 patients had the lowest median NMEoccl values of all patients (Fig. 3B).
Comparison between OR and PICU groups (objective 2)
Figure 3 also depicts individual and group values of maximum ΔPawmax (panel A) and median NMEoccl in the OR group (panel B). Maximum ΔPawmax for the first measurement of the PICU group (35.1 cmH2O, Q1–Q3 21–58) and the only measurement of the OR group (31.3 cmH2O, Q1–Q3 28.5–35.5) were not statistically significantly different, p = 0.982. On the other hand, median NMEoccl in the PICU group (1.8 cmH2O/µV, Q1–Q3 1.3–2.4) was lower than in the OR group (3.7 cmH2O/µV, Q1–Q3 3.5–4.2), p = 0.015.
Discussion
The main findings of the present study can be summarized as follows: (1a) recording ΔPawmax and computing a NMEoccl ratio during an occlusion maneuver is a simple and reliable functional assessment of inspiratory muscles at the bedside of mechanically ventilated children; (1b) inspiratory muscle efficiency (NMEoccl) decreased slightly over time during MV in a group of critically ill children with preserved respiratory drive; (2) inspiratory muscle efficiency (NMEoccl) in critically ill children after 21 h of MV was significantly lower than in children undergoing elective surgery.
Assessment of inspiratory muscle function
Paw is easy to measure in intubated patients and is directly correlated to esophageal pressure in children [39]. Magnetic stimulation has been used successfully by one group mainly [39–43]; however, our own experience (unpublished observations) is that obtaining reliable diaphragmatic contraction following bilateral anterior magnetic stimulation of the phrenic nerves is challenging in small children. Simply measuring ΔPawmax during a spontaneous breath can be done at the bedside with little additional equipment. However, whereas ΔPawtwitch reflects the function of the diaphragm specifically recruited by phrenic nerve magnetic stimulation, ΔPawmax results from the activity of all inspiratory muscles. ΔPawmax measurements require spontaneous breathing and maximal patient effort. Although this may represent a challenge when performed early in critical illness, including an assessment of respiratory drive results in a useful pre-extubation test [44]. In our PICU group, median ΔPaw increased progressively during an occlusion over the first four breaths but not on the last breath, which would suggest that inspiratory effort was maximal; this was not the case in our OR group, however, as median ΔPaw continuously increased until the last measured breath (Fig. 2A). Other authors have used a unidirectional valve that, unlike the occlusion valve used in this study, allows expiration but not inspiration [45, 46]. This results in larger values of ΔPaw because inspiration occurs from progressively smaller lung volumes and a gradually higher drive. Harikumar et al. [46] suggested that occlusions should be maintained for 12 s or 8 breaths in order to be maximal. We opted to aim for 5 consecutive breathing efforts against occlusion, to be minimally disruptive to patient condition and comfort, as commonly done [44, 45]. We have shown that selecting the maximum value of ΔPaw over up to 5 breaths was the least variable method (Table 5), corresponding to the maximum negative pressure the inspiratory muscles are capable of generating at that time.
By recording EAdi continuously throughout the occlusion maneuvers, we were also able to compute a NME ratio for each breath. The major advantage of using NME alongside ΔPaw resides in how it normalizes pressures generated to respiratory drive by using EAdi. The strength of the diaphragm and other inspiratory muscles can therefore be estimated whether or not the inspiratory effort is maximal, solving many of the issues raised previously. It has also been shown that the NME in any specific patient does not depend on ventilation mode or level of assistance, and that the NME value derived during an expiratory occlusion in the absence of flow is a good surrogate of the NME value measured during regular tidal ventilation [47]. As can be seen in Fig. 3, NMEoccl values seem more stable to varying patient conditions than ΔPawmax values.
Several limitations of using NME warrant discussion. First, EAdi measurement requires a dedicated catheter and monitoring device, both of which are associated with costs. Any technical difficulties in measuring the EAdi will result in a falsely low EAdi value and consequently an incorrectly high NME ratio. In this study, appropriate catheter positioning was therefore systematically confirmed before each recording using the dedicated software provided [38]. Furthermore, the relationship between ΔPaw and EAdimax may not be linear at very high breathing efforts. In Fig. 2, it is apparent that an increase in EAdimax between the fourth and the fifth breath does not result in a corresponding increase in ΔPaw, likely because the inspiratory muscles have reached maximum pressure-generating capacity that cannot be increased with additional respiratory drive, or because the diaphragm is unable to reach its fully relaxed configuration between breaths. As previously described by others, EAdi values during a specific recording can exhibit breath-to-breath variability (Fig. 1) [48]. Selecting the median value of NME over 5 breaths allowed to reduce this variability below any of the metrics using ΔPaw (Table 5). Finally, whereas EAdimax only measures diaphragm activity, ΔPawmax includes the pressure generated by the diaphragm as well as accessory muscles.
Evolution of inspiratory muscle function over time
In pediatrics, diaphragm atrophy on MV was only recently demonstrated in studies using ultrasound [13–18]. Although ultrasound overcomes some of the limitations of other imaging modalities such as radiography and fluoroscopy, it provides no information about actual force production. In the current study, which is—to the best of our knowledge—the first to longitudinally assess inspiratory muscle function in children on MV, a small decrease over time in pressure-generating capacity normalized to respiratory drive was found over the whole cohort. These findings taken together suggest that inspiratory muscle atrophy is also associated with a loss in inspiratory muscle efficiency, but the magnitude of the decrease observed was much smaller than that reported in adults [9]. There are various potential reasons why a larger decrease in inspiratory muscle efficiency has not been observed. Because of time required to screen and enroll patients, the first measurement occurred at a median of 20.7 h of MV. Animal data suggest that contractile dysfunction can occur after only 6–12 h of MV [49, 50] and studies in adult ICU patients show that ΔPawtwitch decreases early and in a logarithmic fashion [8]. It is possible that higher NMEoccl values would have been obtained with earlier initial measurements, resulting in a larger decrease over time. Our measurements were also limited to 72 h after intubation in most patients, but it is possible that a further decrease in efficiency would have been observed on measurements beyond that time in patients with prolonged critical illness and MV. If we consider that ICU–DD comprises two concomitant processes, one related to critical illness and its therapies, and the other related specifically to ventilation (VIDD), their respective impact on inspiratory muscle function may be in opposite directions. The cumulative negative impact of MV could be masked by progressive recovery from critical illness. Lastly, VIDD may not have been significant in our cohort because of a relatively preserved respiratory drive, which also tended to increase over time (Table 4). Low respiratory drive has been shown to be correlated with diaphragmatic atrophy [14]. We have previously reported that respiratory drive, as assessed by EAdi, was frequently blunted on conventional modes of ventilation [35]. EAdi values recorded in the current study were higher than observed in the past. This may be the consequence of a change in clinical practice, potentially compounded by the fact that clinicians were not blinded to the EAdi monitoring and may have aimed to preserve patients’ respiratory drive or transition them to assisted modes of ventilation.
Clinical implications
At present, there is no recognized definition of ICU–DD in critically ill children. Definitions based on ΔPawtwitch obtained after maximal magnetic stimulation have been proposed in adults [10, 20, 21, 25, 36], but this method is challenging in infants and thus most pediatric studies of diaphragm strength are based on variables comparable to ΔPawmax described here. In a recent study aiming to define normal value ranges in non-intubated healthy children aged 6–11 years old, maximum inspiratory pressure was 85 ± 30 cmH2O [51]. In 22 infants and children, ΔPawmax was 31 cmH2O after 4.4 days of MV [46]. Khemani et al. recently demonstrated the prognostic significance of ΔPawmax in the PICU: children with ΔPawmax ≤ 30 cmH2O at the time of extubation being more likely to be reintubated than those with preserved strength [44]. We report relatively similar ΔPawmax values in our series: from 35 cmH2O (Q1–Q3 21–58) on the first measurement to 47.2 cmH2O (Q1–Q3 22.2–73.1) on the last measurement. No patient failed extubation in our study and thus we cannot confirm the prognostic value of ΔPawmax.
However, our results provide new information by confirming the feasibility of using NMEoccl to dynamically assess the evolution of diaphragmatic efficiency in critically ill children over time. Several studies have recently reported values for NME in adult ICU patients [52–55]. In patients on conventional ventilation for ≥ 24 h, NME during a spontaneous breathing trial was significantly higher in patients successfully extubated (1.5 cmH2O/µV) compared with those who failed extubation (1 cmH2O/µV) [52]. In patients who were transitioned from controlled to assisted breathing, NME was 1 cmH2O/µV, but did not fluctuate over time and was not correlated with outcomes [53]. In patients on conventional ventilation for ≥ 72 h, NME increased from 1 to 2.6 cmH2O/µV after transition to NAVA [54]. Finally, in patients on NAVA for 10 h, NME was 1.2 cmH2O/µV and did not change over time [55]. It is important to note that pressure values used to compute NME in these adult studies were extracted directly from the ventilator, not measured through an occlusion valve and manometer, and were therefore impacted by circuit compliance.
There is—to the best of our knowledge—no study reporting NME values in children on conventional ventilation. Wolf et al. have used the related neuro-ventilatory efficiency ratio (NVE, tidal volume/EAdi) to predict successful extubation in PICU patients during a spontaneous breathing trial [56]. In their study, patients who passed an extubation readiness test on pressure support ventilation had a lower NVE than those who failed. Unlike NME, NVE is sensitive to changes in respiratory load (i.e., airway compliance and resistance) and to the work done by the ventilator.
As mentioned above, measuring NMEoccl (efficiency) provides valuable complementary information to ΔPawmax (strength), which may be of particular importance for longitudinal assessment of inspiratory muscle function by accounting for respiratory drive. Our study design and sample size did not, however, allow for evaluation of the prognostic value of NME in critically ill children. As no patient was re-intubated, we can only note that the only 2 patients in our PICU group who required continuous NIV for 72 h after extubation were also the only patients who had NMEoccl values < 0.5 cmH2O/µV at all timepoints. Although we observed lower neuro-mechanical efficiency (as measured by NMEoccl) in the PICU group, these patients were able to generate similar inspiratory pressures (as measured by ΔPawmax) than those in the OR group and none failed extubation. We may speculate that these children were able to compensate for inspiratory muscle weakness by an increase in respiratory drive. More studies are therefore warranted to assess the prognostic value of NME on outcomes such as extubation failure or ventilation duration.
When comparing critically ill children with children undergoing elective surgery, we report NMEoccl in the PICU group significantly lower than in the OR group. This suggests that inspiratory muscle efficiency seems to be affected rapidly following PICU admission, and therefore likely results from critical illness rather than its therapies. This finding is in line with data observed in adults [10]. Comparison between these two groups must, however, be interpreted with caution. The PICU group included patients that were younger, more patients born prematurely, and some patients who were recently intubated before the current episode. Age was not associated with the level of EAdi in a previous study conducted in similar population [35], but the potential impact of age on NMEoccl is not known. In terms of medication, only patients in the OR group received sevoflurane, but data suggest it does not have a significant effect on isometric skeletal muscle strength in humans at clinically relevant concentrations [57]. A notable difference in procedure was that occlusion maneuvers were performed without PEEP in the OR group for practical reasons (i.e., interruptions in OR procedural flow). ΔPawmax may vary with lung volume as a function of the force–length relationship of the diaphragm and the varying contribution of passive elastic recoil pressure of the respiratory system [58]. It is theoretically possible that these factors favored higher ΔPawmax (and therefore higher NMEoccl) values in the OR group due to lower initial lung volumes resulting from the absence of PEEP. Most importantly, even if we had initially planned to perform measurements rapidly after intubation in both groups to assess the impact of critical illness without a superimposed difference in time on MV, logistical constraints (e.g., out-of-hours intubation, research personnel availability, etc.) resulted in first measurements being performed only after a median 20.7 h of MV in the PICU group compared to minutes in the OR group.
Strengths and limitations
The strength of our work resides in the number of breaths analyzed at each time point, pressures measured directly at the endotracheal tube, and a rigorous protocol to maximize EAdi measurement validity. However, our PICU cohort was small, from a single center, and displayed significant heterogeneity in terms of baseline characteristics, indications for PICU admission and intubation, and modes of ventilation. Although this heterogeneity may have decreased the power of this study to detect changes over time, it also reflects the usual PICU population. This would favor clinical relevance and increase the external validity of our findings, together with the fact that measurements were successfully performed in two very different populations (PICU and OR groups). Because our sample did not include many patients with low respiratory drive, it is unclear how applicable these findings would be in such situations.
Conclusions
In this study, we have proposed and validated an innovative method to reliably measure inspiratory muscle function at the bedside of mechanically ventilated children on a sample aged 1 week to 10 years old. The efficiency of these muscles decreased slightly over time during MV in this PICU cohort with preserved respiratory drive, but was already low on the first measurement after intubation. Further research is needed to explore the relative roles that critical illness (ICU–DD) and MV (VIDD) play in this process and to assess the clinical utility of such monitoring in the PICU setting. This work nevertheless supports the emerging paradigm of aiming for lung-protective but also diaphragm-protective MV [59, 60].
Acknowledgements
The authors thank Mariana Dumitrascu, Djouher Nait Ladjemil, and Vincent Laguë for their help in the screening and enrollment process, the respiratory therapists for their logistic support, the ENT surgeons and anesthesiologists for their time and assistance in the OR, and the PICU fellows and attendings for their collaboration.
Abbreviations
- CoV
Coefficient of variation
- EAdi
Electrical activity of the diaphragm
- FiO2
Fraction of inspired oxygen
- ICU
Intensive care unit
- Q1–Q3
First and third quartiles
- MV
Mechanical ventilation
- NAVA
Neurally adjusted ventilatory assist
- NIV
Non-invasive ventilation
- NME
Neuro-mechanical efficiency ratio
- NVE
Neuro-ventilatory efficiency ratio
- OR
Operating room
- PCO2
Partial pressure of carbon dioxide
- Paw
Airway pressure
- PEEP
Positive end-expiratory pressure
- PELOD
Pediatric logistic organ dysfunction
- PICU
Pediatric intensive care unit
- PSV
Pressure-support ventilation
- SpO2
Oxygen saturation by pulse oximetry
Authors' contributions
GE, BP and JPP designed the study. GE and BC completed the literature review, redacted the protocol, submitted to the ethics committee. GE and BC performed the physiological measurements. BC undertook the clinical data collection, signal analysis, and statistical analysis, and wrote the manuscript. AK performed the advanced statistical analyses. All authors contributed to the interpretation of the data and approved the final manuscript.
Funding
BC would like to acknowledge the financial support of Fonds de recherche du Québec – Santé (FRQS) and the CHU Sainte-Justine Research Center. This work was supported by a team grant from the Quebec Respiratory Health research Network (QRHN) of the Fonds de recherche du Québec – Santé (FRQS).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request, providing approval by the ethics committee of the CHU Sainte-Justine Research Center.
Declarations
Ethics approval and consent to participate
Approval by the ethics committee of the CHU Sainte-Justine Research Center was granted before initiating enrollment (2017-1534). Written informed consent was obtained from the parents/guardians by a member of the research team.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Principi T, Fraser DD, Morrison GC, Farsi SA, Carrelas JF, Maurice EA, et al. Complications of mechanical ventilation in the pediatric population. Pediatr Pulmonol. 2011;46(5):452–457. doi: 10.1002/ppul.21389. [DOI] [PubMed] [Google Scholar]
- 2.Dres M, Goligher EC, Heunks LMA, Brochard LJ. Critical illness-associated diaphragm weakness. Intensive Care Med. 2017;43(10):1441–1452. doi: 10.1007/s00134-017-4928-4. [DOI] [PubMed] [Google Scholar]
- 3.Vassilakopoulos T, Petrof BJ. Ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med. 2004;169(3):336–341. doi: 10.1164/rccm.200304-489CP. [DOI] [PubMed] [Google Scholar]
- 4.Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, et al. Evolution of diaphragm thickness during mechanical ventilation: impact of inspiratory effort. Am J Respir Crit Care Med. 2015;192:1080–1088. doi: 10.1164/rccm.201503-0620OC. [DOI] [PubMed] [Google Scholar]
- 5.Laghi F, D'Alfonso N, Tobin MJ. Pattern of recovery from diaphragmatic fatigue over 24 hours. J Appl Physiol. 1995;79(2):539–546. doi: 10.1152/jappl.1995.79.2.539. [DOI] [PubMed] [Google Scholar]
- 6.Goligher EC. Myotrauma in mechanically ventilated patients. Intensive Care Med. 2019;45:881–884. doi: 10.1007/s00134-019-05557-6. [DOI] [PubMed] [Google Scholar]
- 7.Petrof BJ. Diaphragm weakness in the critically ill: basic mechanisms reveal therapeutic opportunities. Chest. 2018;154(6):1395–1403. doi: 10.1016/j.chest.2018.08.1028. [DOI] [PubMed] [Google Scholar]
- 8.Hermans G, Agten A, Testelmans D, Decramer M, Gayan-Ramirez G. Increased duration of mechanical ventilation is associated with decreased diaphragmatic force: a prospective observational study. Crit Care. 2010;14:R127. doi: 10.1186/cc9094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaber S, Petrof BJ, Jung B, Chanques G, Berthet J-P, Rabuel C, et al. Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans. Am J Respir Crit Care Med. 2011;183:364–371. doi: 10.1164/rccm.201004-0670OC. [DOI] [PubMed] [Google Scholar]
- 10.Demoule A, Jung B, Prodanovic H, Molinari N, Chanques G, Coirault C, et al. Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact-a prospective study. Am J Respir Crit Care Med. 2013;188:213–219. doi: 10.1164/rccm.201209-1668OC. [DOI] [PubMed] [Google Scholar]
- 11.Knisely AS, Leal SM, Singer DB. Abnormalities of diaphragmatic muscle in neonates with ventilated lungs. J Pediatr. 1988;113:1074–1077. doi: 10.1016/S0022-3476(88)80585-7. [DOI] [PubMed] [Google Scholar]
- 12.Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med. 2008;358:1327–1335. doi: 10.1056/NEJMoa070447. [DOI] [PubMed] [Google Scholar]
- 13.Lee EP, Hsia SH, Hsiao HF, Chen MC, Lin JJ, Chan OW, et al. Evaluation of diaphragmatic function in mechanically ventilated children: an ultrasound study. PLoS ONE. 2017;12:1–11. doi: 10.1371/journal.pone.0183560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glau CL, Conlon TW, Himebauch AS, Yehya N, Weiss SL, Berg RA, et al. Progressive diaphragm atrophy in pediatric acute respiratory failure. Pediatr Crit Care Med. 2018;19:1. doi: 10.1097/PCC.0000000000001368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson RW, Ng KWP, Dietz AR, Hartman ME, Baty JD, Hasan N, et al. Muscle atrophy in mechanically-ventilated critically ill children. PLoS ONE. 2018;13:e007720. doi: 10.1371/journal.pone.0207720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.IJland MM, Lemson J, van der Hoeven JG, Heunks LMA. The impact of critical illness on the expiratory muscles and the diaphragm assessed by ultrasound in mechanical ventilated children. Ann Intensive Care. 2020;10(1):115. doi: 10.1186/s13613-020-00731-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mistri S, Dhochak N, Jana M, Jat KR, Sankar J, Kabra SK, et al. Diaphragmatic atrophy and dysfunction in critically ill mechanically ventilated children. Pediatr Pulmonol. 2020;55:3457–3464. doi: 10.1002/ppul.25076. [DOI] [PubMed] [Google Scholar]
- 18.Valverde Montoro D, Garcia Soler P, Hernandez Yuste A, Camacho Alonso JM. Ultrasound assessment of ventilator-induced diaphragmatic dysfunction in mechanically ventilated pediatric patients. Paediatr Respir Rev. 2021. 10.1016/j.prrv.2020.12.002 [DOI] [PubMed]
- 19.Corpeno R, Dworkin B, Cacciani N, Salah H, Bergman H-M, Ravara B, et al. Time course analysis of mechanical ventilation-induced diaphragm contractile muscle dysfunction in the rat. J Physiol. 2014;592:3859–3880. doi: 10.1113/jphysiol.2014.277962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jung B, Moury PH, Mahul M, de Jong A, Galia F, Prades A, et al. Diaphragmatic dysfunction in patients with ICU-acquired weakness and its impact on extubation failure. Intensive Care Med. 2016;42:853–861. doi: 10.1007/s00134-015-4125-2. [DOI] [PubMed] [Google Scholar]
- 21.Dres M, Dube BP, Mayaux J, Delemazure J, Reuter D, Brochard L, et al. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med. 2017;195(1):57–66. doi: 10.1164/rccm.201602-0367OC. [DOI] [PubMed] [Google Scholar]
- 22.Watson AC, Hughes PD, Louise Harris M, Hart N, Ware RJ, Wendon J, et al. Measurement of twitch transdiaphragmatic, esophageal, and endotracheal tube pressure with bilateral anterolateral magnetic phrenic nerve stimulation in patients in the intensive care unit. Crit Care Med. 2001;29:1325–1331. doi: 10.1097/00003246-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Supinski GS, Callahan LA. Diaphragm weakness in mechanically ventilated critically ill patients. Crit Care. 2013;17:R120. doi: 10.1186/cc12792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim WY, Suh HJ, Hong S-B, Koh Y, Lim C-M. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med. 2011;39:2627–2630. doi: 10.1097/CCM.0b013e3182266408. [DOI] [PubMed] [Google Scholar]
- 25.Dres M, Goligher EC, Dube BP, Morawiec E, Dangers L, Reuter D, et al. Diaphragm function and weaning from mechanical ventilation: an ultrasound and phrenic nerve stimulation clinical study. Ann Intensive Care. 2018;8(1):53. doi: 10.1186/s13613-018-0401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Demoule A, Molinari N, Jung B, Prodanovic H, Chanques G, Matecki S, et al. Patterns of diaphragm function in critically ill patients receiving prolonged mechanical ventilation: a prospective longitudinal study. Ann Intensive Care. 2016;6:75. doi: 10.1186/s13613-016-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med. 2018;197:204–213. doi: 10.1164/rccm.201703-0536OC. [DOI] [PubMed] [Google Scholar]
- 28.Medrinal C, Prieur G, Frenoy E, Robledo Quesada A, Poncet A, Bonnevie T, et al. Respiratory weakness after mechanical ventilation is associated with one-year mortality—a prospective study. Crit Care. 2016;20(1):231. doi: 10.1186/s13054-016-1418-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hershenson MB, Colin AA, Wohl ME, Stark AR. Changes in the contribution of the rib cage to tidal breathing during infancy. Am Rev Respir Dis. 1990;141(4 Pt 1):922–925. doi: 10.1164/ajrccm/141.4_Pt_1.922. [DOI] [PubMed] [Google Scholar]
- 30.Papastamelos C, Panitch HB, England SE, Allen JL. Developmental changes in chest wall compliance in infancy and early childhood. J Appl Physiol (1985) 1995;78(1):179–184. doi: 10.1152/jappl.1995.78.1.179. [DOI] [PubMed] [Google Scholar]
- 31.Gaultier C, Praud JP, Canet E, Delaperche MF, D'Allest AM. Paradoxical inward rib cage motion during rapid eye movement sleep in infants and young children. J Dev Physiol. 1987;9(5):391–397. [PubMed] [Google Scholar]
- 32.Kosch PC, Stark AR. Dynamic maintenance of end-expiratory lung volume in full-term infants. J Appl Physiol Respir Environ Exerc Physiol. 1984;57(4):1126–1133. doi: 10.1152/jappl.1984.57.4.1126. [DOI] [PubMed] [Google Scholar]
- 33.Emeriaud G, Beck J, Tucci M, Lacroix J, Sinderby C. Diaphragm electrical activity during expiration in mechanically ventilated infants. Pediatr Res. 2006;59:705–710. doi: 10.1203/01.pdr.0000214986.82862.57. [DOI] [PubMed] [Google Scholar]
- 34.Larouche A, Massicotte E, Constantin G, Ducharme-Crevier L, Essouri S, Sinderby C, et al. Tonic diaphragmatic activity in critically ill children with and without ventilatory support. Pediatr Pulmonol. 2015;50:1304–1312. doi: 10.1002/ppul.23182. [DOI] [PubMed] [Google Scholar]
- 35.Emeriaud G, Larouche A, Ducharme-Crevier L, Massicotte E, Flechelles O, Pellerin-Leblanc A-A, et al. Evolution of inspiratory diaphragm activity in children over the course of the PICU stay. Intensive Care Med. 2014;40:1718–1726. doi: 10.1007/s00134-014-3431-4. [DOI] [PubMed] [Google Scholar]
- 36.Laveneziana P, Albuquerque A, Aliverti A, Babb T, Barreiro E, Dres M, et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. 2019;53(6):1801214. doi: 10.1183/13993003.01214-2018. [DOI] [PubMed] [Google Scholar]
- 37.Beck J, Sinderby C, Lindstrom L, Grassino A. Effects of lung volume on diaphragm EMG signal strength during voluntary contractions. J Appl Physiol. 1998;85(3):1123–1134. doi: 10.1152/jappl.1998.85.3.1123. [DOI] [PubMed] [Google Scholar]
- 38.Ducharme-Crevier L, Du Pont-Thibodeau G, Emeriaud G. Interest of monitoring diaphragmatic electrical activity in the pediatric intensive care unit. Crit Care Res Pract. 2013;2013:384210. doi: 10.1155/2013/384210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rafferty GF, Greenough A, Manczur T, Polkey MI, Harris ML, Heaton ND, et al. Magnetic phrenic nerve stimulation to assess diaphragm function in children following liver transplantation. Pediatr Crit Care Med. 2001;2:122–126. doi: 10.1097/00130478-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Dimitriou G, Greenough A, Moxham J, Rafferty GF. Influence of maturation on infant diaphragm function assessed by magnetic stimulation of phrenic nerves. Pediatr Pulmonol. 2003;35:17–22. doi: 10.1002/ppul.10209. [DOI] [PubMed] [Google Scholar]
- 41.Kassim Z, Jolley C, Moxham J, Greenough A, Rafferty GF. Diaphragm electromyogram in infants with abdominal wall defects and congenital diaphragmatic hernia. Eur Respir J. 2011;37:143–149. doi: 10.1183/09031936.00007910. [DOI] [PubMed] [Google Scholar]
- 42.Rafferty GF, Greenough A, Dimitriou G, Kavadia V, Laubscher B, Polkey MI, et al. Assessment of neonatal diaphragm function using magnetic stimulation of the phrenic nerves. Am J Respir Crit Care Med. 2000;162:2337–2340. doi: 10.1164/ajrccm.162.6.2004019. [DOI] [PubMed] [Google Scholar]
- 43.Rafferty GF, Mustfa N, Man WD, Sylvester K, Fisher A, Plaza M, et al. Twitch airway pressure elicited by magnetic phrenic nerve stimulation in anesthetized healthy children. Pediatr Pulmonol. 2005;40:141–147. doi: 10.1002/ppul.20241. [DOI] [PubMed] [Google Scholar]
- 44.Khemani RG, Sekayan T, Hotz J, Flink RC, Rafferty GF, Iyer N, et al. Risk factors for pediatric extubation failure: the importance of respiratory muscle strength. Crit Care Med. 2017;45:e798–e805. doi: 10.1097/CCM.0000000000002433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Manczur TI, Greenough A, Pryor D, Rafferty GF. Assessment of respiratory drive and muscle function in the pediatric intensive care unit and prediction of extubation failure. Pediatr Crit Care Med. 2000;1(2):124–126. doi: 10.1097/00130478-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Harikumar G, Moxham J, Greenough A, Rafferty GF. Measurement of maximal inspiratory pressure in ventilated children. Pediatr Pulmonol. 2008;43(11):1085–1091. doi: 10.1002/ppul.20905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bellani G, Mauri T, Coppadoro A, Grasselli G, Patroniti N, Spadaro S, et al. Estimation of patient's inspiratory effort from the electrical activity of the diaphragm. Crit Care Med. 2013;41(6):1483–1491. doi: 10.1097/CCM.0b013e31827caba0. [DOI] [PubMed] [Google Scholar]
- 48.de la Oliva P, Schuffelmann C, Gomez-Zamora A, Villar J, Kacmarek RM. Asynchrony, neural drive, ventilatory variability and COMFORT: NAVA versus pressure support in pediatric patients. A non-randomized cross-over trial. Intensive Care Med. 2012;38(5):838–846. doi: 10.1007/s00134-012-2535-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Powers SK, Shanely RA, Coombes JS, Koesterer TJ, McKenzie M, Van Gammeren D, et al. Mechanical ventilation results in progressive contractile dysfunction in the diaphragm. J Appl Physiol. 2002;92(5):1851–1858. doi: 10.1152/japplphysiol.00881.2001. [DOI] [PubMed] [Google Scholar]
- 50.Liang F, Emeriaud G, Rassier DE, Shang D, Gusev E, Hussain SNA, et al. Mechanical ventilation causes diaphragm dysfunction in newborn lambs. Crit Care. 2019;23(1):123. doi: 10.1186/s13054-019-2409-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lira M, Fregonezi G, Marcelino AA, Sarmento A, Resqueti VR. Normal range of values for contractility and relaxation parameters of inspiratory muscles in healthy children: an exploratory study. Pediatr Pulmonol. 2020;55(6):1512–1520. doi: 10.1002/ppul.24779. [DOI] [PubMed] [Google Scholar]
- 52.Liu L, Liu H, Yang Y, Huang Y, Liu S, Beck J, et al. Neuroventilatory efficiency and extubation readiness in critically ill patients. Crit Care. 2012;16(4):R143. doi: 10.1186/cc11451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bellani G, Coppadoro A, Pozzi M, Bronco A, Albiero D, Eronia N, et al. The ratio of inspiratory pressure over electrical activity of the diaphragm remains stable during ICU stay and is not related to clinical outcome. Respir Care. 2016;61(4):495–501. doi: 10.4187/respcare.04400. [DOI] [PubMed] [Google Scholar]
- 54.Di Mussi R, Spadaro S, Mirabella L, Volta CA, Serio G, Staffieri F, et al. Impact of prolonged assisted ventilation on diaphragmatic efficiency: NAVA versus PSV. Crit Care. 2016;20:1. doi: 10.1186/s13054-015-1178-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jansen D, Jonkman AH, Roesthuis L, Gadgil S, Van Der Hoeven JG, Scheffer GJJ, et al. Estimation of the diaphragm neuromuscular efficiency index in mechanically ventilated critically ill patients. Crit Care. 2018;22:1–8. doi: 10.1186/s13054-017-1923-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wolf GK, Walsh BK, Green ML, Arnold JH. Electrical activity of the diaphragm during extubation readiness testing in critically ill children. Pediatr Crit Care Med. 2011;12(6):e220–e224. doi: 10.1097/PCC.0b013e3181fe28fc. [DOI] [PubMed] [Google Scholar]
- 57.Ginz HF, Zorzato F, Iaizzo PA, Urwyler A. Effect of three anaesthetic techniques on isometric skeletal muscle strength. Br J Anaesth. 2004;92(3):367–372. doi: 10.1093/bja/aeh080. [DOI] [PubMed] [Google Scholar]
- 58.Grassino A, Goldman MD, Mead J, Sears TA. Mechanics of the human diaphragm during voluntary contraction: statics. J Appl Physiol Respir Environ Exerc Physiol. 1978;44(6):829–839. doi: 10.1152/jappl.1978.44.6.829. [DOI] [PubMed] [Google Scholar]
- 59.Schepens T, Dres M, Heunks L, Goligher EC. Diaphragm-protective mechanical ventilation. Curr Opin Crit Care. 2019;25(1):77–85. doi: 10.1097/MCC.0000000000000578. [DOI] [PubMed] [Google Scholar]
- 60.Goligher EC, Dres M, Patel BK, Sahetya SK, Beitler JR, Telias I, et al. Lung and diaphragm-protective ventilation. Am J Respir Crit Care Med. 2020;202:950–961. doi: 10.1164/rccm.202003-0655CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferrari L, Leahy I, Staffa SJ, Berry JG. The pediatric-specific American society of anesthesiologists physical status score: a multicenter study. Anesth Analg. 2021;132(3):807–817. doi: 10.1213/ANE.0000000000005025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request, providing approval by the ethics committee of the CHU Sainte-Justine Research Center.