Abstract
Unilateral right-sided varicocele is a rare and warning condition that should hint at a serious retroperitoneal disease such as renal cell neoplasm. Furthermore, its thrombosis is such an unusual entity that only a few cases have been described. We review the literature and report, to our knowledge, the second case of acute scrotal pain caused by unilateral right-sided varicocele thrombosis complicating an ipsilateral epididymo-orchitis, with no underlying coagulopathy or abdominal neoplasm, to illustrate the clinical, morphologic and therapeutic features of this entity.
Keywords: Acute scrotum, Pampiniform, Varicocele, Epididymo-orchitis, Thrombosis
Introduction
Varicocele is an abnormal dilatation of the pampiniform venous plexus and the internal spermatic vein. It occurs in approximately 15–20% of all males and in 40% of infertile males.1 It is mainly left-sided; however in rare cases the right side is involved. The presence of unilateral right-sided varicocele should hint at a serious retroperitoneal disease such as renal cell neoplasm.2 The thrombosis of varicocele is a very uncommon entity especially when it is right-sided.
We report the case of a 34-year-old man presenting with a right varicocele thrombosis that is associated with a right epididymo-orchitis, with no underlying coagulopathy or abdominal neoplasm, to illustrate the clinical, morphologic and therapeutic features of this entity. To our knowledge, this is the second case in the literature.
Case report
We report the case of a 34-year-old man with no medical history complaining of isolated right acute scrotal pain developing over three days with no fever or chills or dysuria or urethral discharge. Clinical examination found a firm nontender swelling of the right upper pole of the scrotum associated with a right testicular enlargement and induration.
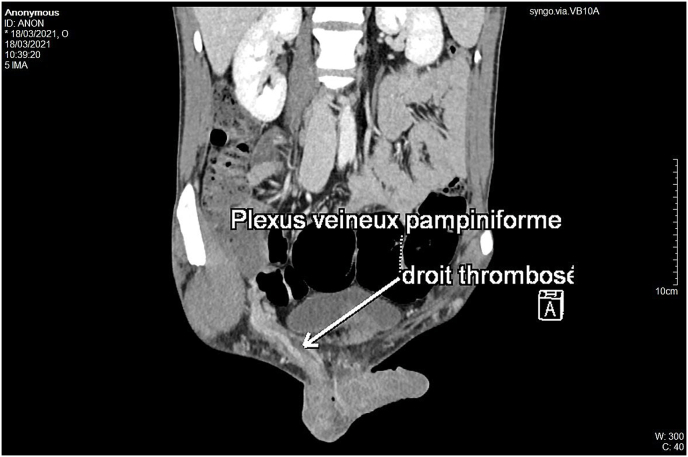
Doppler ultrasound examination revealed a right epididymo-orchitis associated with a right Grade II thrombosed varicocele (Fig. 1).
Fig. 1.
Color Doppler sonography showing (A) an increase in the right testicular vascularity with epididymal enlargement and (B) the right pampiniform plexus mild dilatation with the thrombosis inside. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
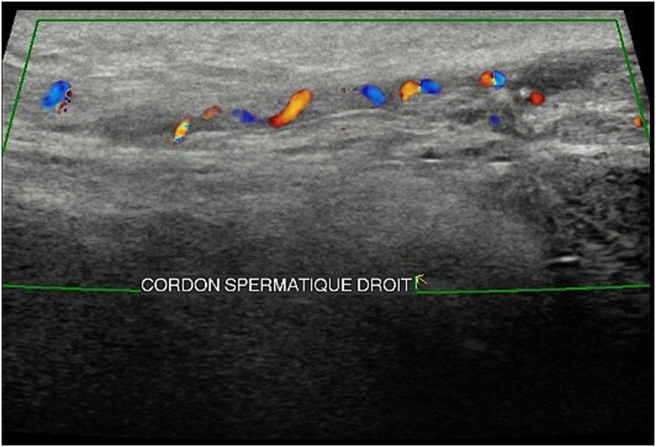
Computed tomography ruled out the presence of any right renal mass and found no thrombosis in right renal vein or inferior vena cava and confirmed the right pampiniform plexus dilatation and thrombosis (Fig. 2).
Fig. 2.
Abdominal CT-Scan showing the right varicocele thrombosis.
Basic laboratory tests were normal. The UTI was documented and an E. Coli was islolated. The patient was managed conservatively with intravenous antibiotics course targeting the epididymo-orchitis, in addition to parenteral and oral analgesics, scrotal elevation and bed rest. We additionally started anticoagulation therapy with subcutaneous enoxaparine then oral warfarin before we obtained the coagulation parameters results. Within four days, we obtained a clinical improvement though the patient's international normalized ration never reached level 2–3. We continued clinical and biological surveillance for one week. The evolution had been favourable, Warfarin was stopped since no underlying coagulopathy was found. The patient was discharged after seven days of hospitalization. He was given an additionnal two-week course of oral ciprofloxacin.
Ultrasonography study fifteen days later showed an improvement but incomplete resolution of the thrombosis of the right varicocele and no signs of epididymo-orchitis. One month later, repeated ultrasonography examination found a complete resolution of the thrombosis (Fig. 3).
Fig. 3.
Color Doppler sonography showing complete resolution of the thrombosis one month after conservative management. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Discussion
In our case, varicocele occurred on the right side. However, it commonly occurs on the left side due to various anatomical factors, such as the compression of the left renal vein by the superior mesenteric artery and the perpendicular disposition of the left testicular vein drains to the left renal vein, which predisposes to low blood flow and stasis.3
Spontaneous thrombosis of the pampiniform plexus is such an unusual condition that only 20 cases reported in the literature.4
In the etiology of isolated spermatic vein thrombosis, there are many possible predisposing factors, such as trauma to the vascular endothelium, slow venous flow, and hyper coagulability. We found no coagulopathy in our case.
Right unilateral varicocele warrants investigation to exclude retroperitoneal pathology and also anatomic variants, given association with situs inversus.
To our knowledge, we reported the second case of right varicocele thrombosis complicating an ipsilateral epididymo-orchitis to contribute to the illustration of this rare entity. The first one was reported in 2020 by Hussam M. Alshubaili et al.5 These latters managed conservatively their patient and prescribed antibiotics, analgesics and rest but no anticoagulation therapy since he was healthy with no significant risk.
Preoperative diagnosis of varicocele thrombosis is uncommon and strangulated inguinal hernia is the most common. Despite ultrasound examination, a surgical exploration for strangulated hernia was indicated on the basis of the finding of mass without blood flow.4
This entity is poorly described in the literature and available data are limited to a few cases. Hence, there is no unanimous guideline panel for its management. In our opinion, the surgical excision of the thrombosis is not suitable and the management of a varicocele thrombosis should be conservative. The conservative treatment in this particular condition we are describing should consist of a full course of antibiotics, rest and analgesics. Nonsteroidal anti-inflammatory drugs don't seem to be mandatory.
Anticoagulation is still controversial. To our opinion, it is not necessary for patient with no malignancy or thrombotic risk factors. Theoretically, the idea of thrombolysis and long-term anti-thrombus management could help in improving the outcome and decreasing the recurrence, especially in the high-risk group like patients with malignancy.5 In our case, no malignancy or other risk factor was found so we could have not prescribed anticoagualtion therapy.
Conclusion
There have been very few case reports of patients with right-sided varicocele thrombosis complicating an epididymo-orchitis and with no underlying renal neoplasm or coagulopathy. To our knowledge, we report the second case. It is a rare entity but needs to be considered since its preoperative diagnosis is uncommon as an etiology of acute scrotal pain. Color Doppler ultrasonography is the cornerstone of diagnostic imaging to establish the diagnosis. The management of this exceptional condition is typically conservative and anticoagulation seem to be indicated in the high-risk group for venous thrombosis.
Conflict of interest
All authors have no conflict of interest to declare.
Acknowledgements
None.
No Funding to declare.
References
- 1.Varicocele: Practice Essentials History of the procedure. https://emedicine.medscape.com/article/438591-overview Problem [Internet]. [cité 30 mars 2021]. Disponible sur.
- 2.Adhikari P., Neeli S.I., Mohan S. A rare case of right-sided varicocele in right renal tumor in the absence of venous thrombosis and IVC compression. Afr J Urol. 12 nov 2020;26(1):63. [Google Scholar]
- 3.Kurklinsky A.K., Rooke T.W. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc. 1 juin. 2010;85(6):552–559. doi: 10.4065/mcp.2009.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamel K., Gassen S., Mohamed M. Bilateral spontaneous thrombosis of the pampiniform plexus; A rare etiology of acute scrotal pain: a case report and review of literature. Afr J Urol. 1 mars. 2018;24(1):14–18. [Google Scholar]
- 5.Alshubaili H.M., Alharbi K.I., Elsirafy M.N., Abuanz S.M., Hasan R.M. Acute right epididymo-orchitis complicated by pampiniform plexus thrombosis. Urol Case Rep. juill. 2020;31:101171. doi: 10.1016/j.eucr.2020.101171. [DOI] [PMC free article] [PubMed] [Google Scholar]