Abstract
Objectives:
The number of older adults on methadone maintenance treatment (MMT) for opioid use disorder is increasing, but little is known about the characteristics and healthcare needs of this aging treatment population. This population may experience accelerated aging due to comorbidities and health behaviors. The aim of this study was to compare the prevalence of geriatric conditions among adults age ≥50 on MMT to a nationally representative sample of community dwelling older adults.
Methods:
We performed a geriatric assessment on 47 adults age ≥50 currently on MMT enrolled in two opioid treatment programs (OTPs), in New York City and in East Providence, Rhode Island. We collected data on self-reported geriatric conditions, healthcare utilization, chronic medical conditions, physical function, and substance use. The results were compared to 470 age, gender, and race/ethnicity-matched adults in the national Health and Retirement Study (HRS).
Results:
The mean age of the study sample was 58.8 years and 23.4% were female. The most common chronic diseases were hypertension (59.6%) and arthritis (55.3%) with 66% reporting ≥2 diseases. For geriatric conditions, adults on MMT had a significantly higher prevalence of mobility, hearing, and visual impairments as well as falls, urinary incontinence, chronic pain, and insomnia than the HRS sample.
Conclusion:
Older adults on MMT in two large OTPs have a high prevalence of geriatric conditions. An interdisciplinary, geriatric-based approach to care that focuses on function and addresses geriatric conditions is needed to improve the health of this growing population.
Keywords: Geriatrics, methadone, opioid treatment program, comorbidities
Introduction
The number of older adults with opioid use disorder (OUD) entering opioid treatment programs (OTPs) is increasing.1 In New York City (NYC) OTPs, adults age 50–59 increased by 425% and adults age ≥60 by 713% between 1996 to 2012.2 Methadone maintenance treatment (MMT) delivered through OTPs is responsible for many living longer lives.3 However, the population of adults with OUD has a high burden of chronic disease and often receive fragmented primary care.4 This could place adults with OUD at increased risk for premature aging and early functional decline.
Geriatric conditions have distinct features: they tend to appear in older age, are common among vulnerable populations, and often followed by a functional decline. Common geriatric conditions include falls, chronic pain, insomnia, and urinary incontinence.5 Addressing geriatric conditions decreases mortality risks and acute care utilization.6 This is relevant for adults with substance use disorders (SUDs) since problems associated with substance use may accelerate frailty.7 Thus adults with SUD, similar to populations that experience premature aging (i.e., prisoners8), may have geriatric needs earlier in life. Therefore, the objective of this study was to determine the prevalence of geriatric conditions among a sample of middle-aged and older adults on MMT.
Methods
This study was a descriptive cross-sectional study of adults currently on methadone through an OTP. The inclusion criteria included adults age 50–90 and English speaking. Patients were not enrolled if they lacked the capacity to provide informed consent.9 We enrolled patients from two OTPs, Bellevue Hospital in NYC and CODAC Behavioral Healthcare in East Providence, Rhode Island (RI) from January 2016 through August 2018. Bellevue’s OTP serves roughly 400 patients and CODAC’s serves approximately 900 patients. Participants were recruited through fliers and called research staff if interested, and upon study completion given $20. This study was approved by the Institutional Review Boards at NYU and Dartmouth-Hitchock.
Data was collected from a single 45-minute in-person interview by the principle investigators. Collected variables included demographics, self-rated health, chronic diseases, psychiatric diseases, health insurance type, and number of hospitalizations in the past two years confirmed with chart review. Substance use was ascertained by asking about past 3-month use of cannabis and cocaine, smoking, and unhealthy alcohol use defined as an AUDIT-C score of ≥3.10 Self-reported methadone treatment duration and current dose were collected as well as primary opioid used prior to the current OTP care.
The self-reported geriatric conditions collected included functional impairment (based on difficulty performing any of the Lawton-Brody instrumental activities of daily living11), mobility impairment (difficulty walking several blocks), hearing impairment (fair/poor hearing despite using a hearing aid), visual impairment (fair/poor eyesight despite using glasses/corrective lens), falls (last two years), urinary incontinence (assessed with “have you lost any amount of urine beyond your control in the past 12-months?”), chronic pain that limits function (assessed with positive responses to both “are you often troubled with pain” and “does the pain make it difficult for you to do your usual activities?”), insomnia (measured by a series of four questions12) and medical multimorbidity (≥2 chronic diseases).
We compared our cohort with a national population-based cohort, the Health and Retirement Survey (HRS), a nationally representative, longitudinal study of U.S. respondents ≥50 years. For this study we used participants from the 2016 wave of the HRS. Details on the HRS design and methods are found elsewhere.13 HRS is one of few studies that collects national data on geriatric conditions, and we used identical questions to allow for comparisons.
We used descriptive statistics to characterize the MMT cohort. To obtain the HRS comparison group we performed an age, gender, race/ethnicity 10 to 1 match to give an HRS cohort of 470 individuals. Comparisons were made using two-sample t-tests for continuous variables and two-sample chi-square tests for categorical variables. There were no missing data for the collected variables.
Results
Table 1 shows 33 participants were from NYC and 14 from RI. The NYC cohort was more racially/ethnically diverse and had a higher proportion of patients with heroin as their primary opioid, while the RI cohort had a longer mean of time on methadone. Combining the NYC and RI sites, compared to the HRS cohort, the MMT cohort had a higher prevalence of psychiatric disease (72.4% vs 27.7%, p<0.001), chronic lung disease (42.6% vs 7.7%, p<0.001), cancer (19.2% vs 8.9%, p=0.03), and a higher proportion with a hospitalization (57.5% vs 21.9%, p<0.001). Figure 1 shows differences in geriatric conditions between the MMT and the HRS cohorts, aside from functional impairment, the MMT cohort had a higher prevalence for all geriatric conditions.
Table 1:
Characteristics of adults age ≥50 on methadone maintenance treatment (MMT) and comparison with Health and Retirement Study (HRS) controls
| Characteristic | New York City site (n=33) | Rhode Island site (n=14) | p-value | Total MMT cohort (n=47) | HRS cohort (n=470) | p-value |
|---|---|---|---|---|---|---|
| Age | ||||||
| Age, years mean (sd) | 58.4 (5.8) | 59.8 (5.8) | 0.45 | 58.8 (5.8) | 58.8 (5.7) | 1.00 |
| Age range, years | 50–75 | 52–68 | 50–75 | 50–75 | ||
| Women, n (%) | 7 (21.2) | 4 (28.6) | 0.59 | 11 (23.4) | 110 (23.4) | 1.00 |
| Race, n (%) | ||||||
| African American | 13 (39.4) | 0 | 0.006 | 13 (27.7) | 130 (27.7) | 1.00 |
| White | 20 (60.6) | 13 (92.9) | 0.03 | 33 (70.2) | 330 (70.2) | |
| Multiracial/other | 0 | 1 (7.2) | 0.12 | 1 (2.1) | 10 (2.1) | |
| Hispanic or Latino, n (%) | 10 (30.3) | 0 | 0.02 | 10 (21.3) | 100 (21.3) | |
| Married or partnered, n (%) | 4 (12.1) | 5 (35.7) | 0.06 | 9 (19.2) | 103 (21.9) | <0.001 |
| < High school education, n (%) | 26 (78.8) | 10 (71.4) | 0.59 | 36 (76.6) | 398 (84.7) | 0.15 |
| Self-rated health, n (%) | ||||||
| Poor/Fair | 23 (69.7) | 9 (64.3) | 0.72 | 32 (68.1) | 133 (28.3) | <0.001 |
| Good | 5 (15.2) | 2 (14.3) | 0.94 | 7 (14.9) | 169 (36.0) | <0.001 |
| Very Good/Excellent | 5 (15.2) | 3 (21.4) | 0.61 | 8 (17.0) | 168 (35.7) | <0.001 |
| Chronic medical disease, n (%) | ||||||
| Hypertension | 19 (57.6) | 9 (64.3) | 0.67 | 28 (59.6) | 267 (56.8) | 0.72 |
| Diabetes | 5 (15.2) | 4 (28.6) | 0.29 | 9 (19.2) | 109 (23.2) | 0.78 |
| Heart diseasea | 4 (12.1) | 2 (14.3) | 0.84 | 6 (12.8) | 89 (18.9) | 0.55 |
| Stroke | 2 (6.1) | 2 (14.3) | 0.36 | 4 (8.5) | 21 (4.5) | 0.22 |
| Arthritis | 19 (57.6) | 7 (50.0) | 0.64 | 26 (55.3) | 193 (41.1) | 0.06 |
| Cancerb | 6 (18.2) | 3 (21.4) | 0.80 | 9 (19.2) | 42 (8.9) | 0.03 |
| Chronic lung diseasec | 15 (45.5) | 5 (35.7) | 0.54 | 20 (42.6) | 36 (7.7) | <0.001 |
| Psychiatric diseased | 26 (78.8) | 8 (57.1) | 0.13 | 34 (72.3) | 13 (27.7) | <0.001 |
| Hepatitis C | 14 (42.4) | 5 (35.7) | 0.67 | 19 (40.4) | N/Ae | |
| HIV/AIDS | 6 (18.2) | 1 (7.1) | 0.33 | 7 (14.9) | N/Ae | |
| Healthcare and insurance | ||||||
| Medicare, n (%) | 11 (33.3) | 8 (57.1) | 0.13 | 19 (40.4) | 134 (28.5) | 0.09 |
| Medicaid, n (%) | 31 (93.9) | 8 (57.1) | 0.002 | 39 (83.0) | 64 (13.6) | <0.001 |
| Hospitalized in past two years, n (%) | 18 (54.5) | 9 (64.3) | 0.54 | 27 (57.5) | 103 (21.9) | <0.001 |
| Mean number of hospitalizations (sd) | 2.3 (2.1) | 3.3 (3.0) | 0.20 | 2.6 (2.4) | 3.0 (8.9) | 0.84 |
| Total number of nights hospitalized (sd) | 15.5 (21.7) | 20.7 (29.1) | 0.50 | 17.2 (23.9) | 9.4 (15.9) | 0.04 |
| Primary opioid prior to MMT, n (%) | ||||||
| Heroin | 25 (75.8) | 4 (30.8) | 0.004 | 29 (63.0) | N/Ae | |
| Prescription opioids | 5 (15.2) | 5 (38.5) | 0.08 | 10 (21.7) | N/Ae | |
| Both | 3 (9.1) | 4 (31.8) | 0.05 | 7 (15.2) | N/Ae | |
| Mean duration MMT in months (sd) | 60.7 (100.4) | 131 (107.4) | 0.04 | 81.7 (106.4) | N/Ae | |
| Mean methadone dose in mg (sd) | 90.1 (46.1) | 107.6 (78.6) | 0.34 | 95.3 (57.4) | N/Ae | |
| Substance use (past 3-month), n (%) | ||||||
| Cannabis | 6 (18.2) | 5 (34.7) | 0.22 | 11 (23.4) | N/Ae | |
| Cocaine | 8 (24.2) | 0 | 0.05 | 8 (17.0) | N/Ae | |
| Current smoker | 21 (63.6) | 4 (28.6) | 0.03 | 25 (53.2) | 93 (19.8) | <0.001 |
| Positive AUDIT-c scoref | 5 (15.2) | 1 (7.1) | 0.45 | 6 (12.8) | N/Ae |
Coronary artery disease and/or congestive heart failure;
Excluding minor skin cancer;
Bronchitis or emphysema;
Defined as having emotional, nervous, or psychiatric problems;
Not available in HRS;
Score of ≥3
Figure 1:
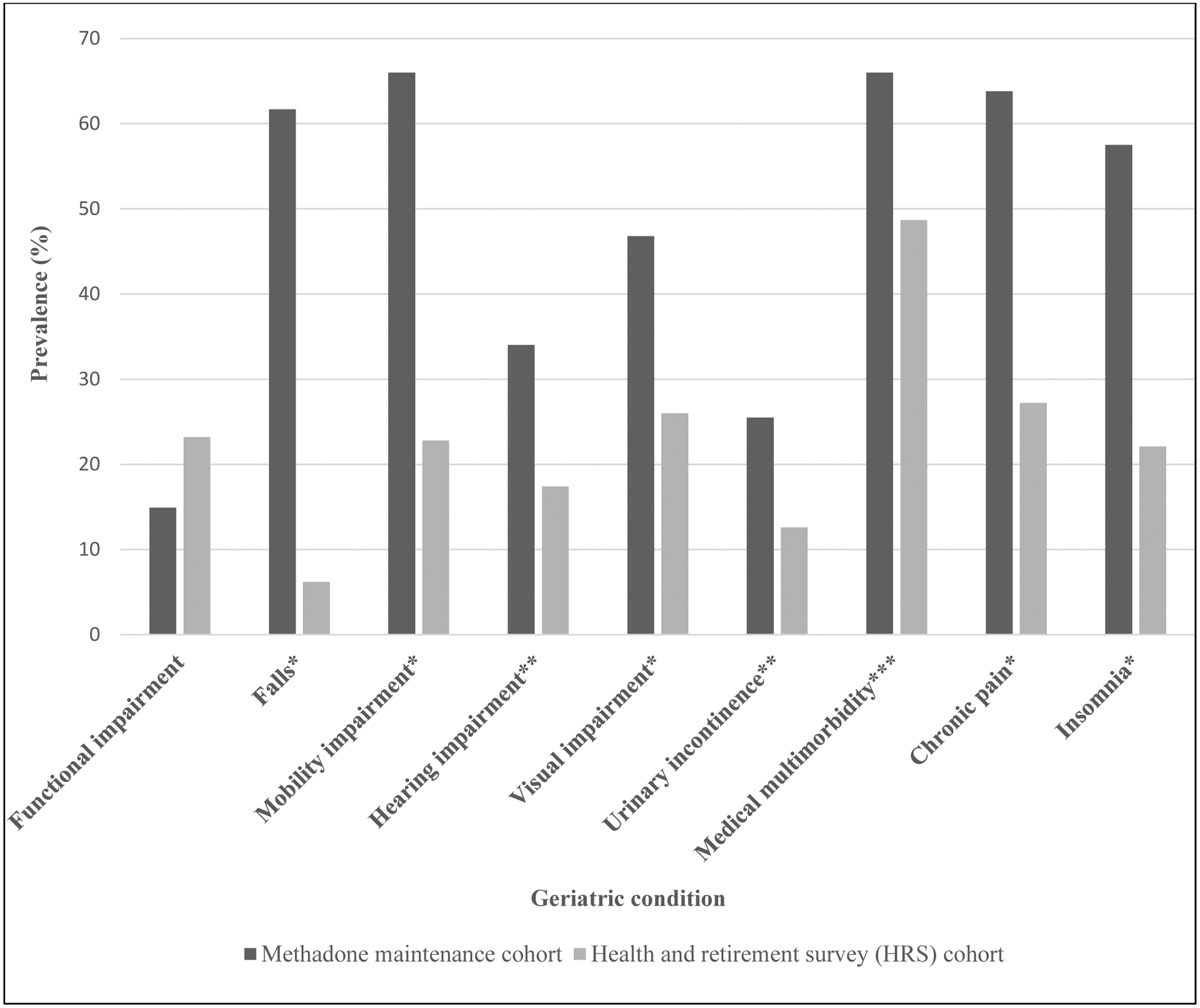
Geriatric conditions in methadone maintenance cohort vs. HRS cohort
*p<0.001; **p=0.01; ***p=0.02
Discussion
This is the first study to measure geriatric conditions among adults with OUD on MMT. We found that this cohort had a higher burden of geriatric conditions compared to adults of similar age, gender, and race/ethnicity. The results add to our understanding of age-related illness in this population. We found a much higher prevalence of falls among the MMT cohort. Falls can lead to functional disability and are usually multifactorial. The higher prevalence of falls could be related to methadone itself as opioids are a known risk factor as well as a higher prevalence of mobility impairment, diabetes, and chronic pain. It is important that OTPs consider implementing falls screening and assessment such as using the Centers for Disease Control and Prevention’s Stopping Elderly Accidents, Deaths, and Injuries (STEADI) initiative.14
Our study indicates that this population may benefit from a geriatric-based approach to care. Geriatric care focuses on maintaining function and independence, quality of life, and the management of geriatric conditions, through a patient-centered and team-based approach. There is a wealth of literature on the effects of geriatric interventions for vulnerable older populations that show improvements in mortality, nursing home use, and quality of care.6 OTPs may be an optimal setting for such interventions because patients have frequent and long-term contact with providers. Further, many patients may find OTPs a more comfortable setting to receive management of geriatric conditions given the stigma of OUD in medical care.15 Future research should focus on how best to integrate the evidence-based principles of geriatric-focused care in addiction medicine settings to improve the health of the growing population of older adults with SUDs.
Limitations
Our study enrolled a small number of patients from two OTPs and is not representative of other OTPs. We used HRS to compare to a nationally representative cohort to test our hypothesis that age ≥50 in OTPs have more geriatric conditions. However, there are limitations to using the HRS since its population is different from the MMT population. We attempted to address this by matching on age, gender, and race/ethnicity. Additionally, most of the variables collected were based on self-report, although some were confirmed by review of medical records. Finally, there is likely a selection bias of our cohort as participants in the study had to call to enroll, therefore we likely enrolled higher functioning patients.
Conclusions
Older adults with OUD have a high prevalence of geriatric conditions, chronic disease, and acute healthcare use. These results suggest that adults with OUD are susceptible to having geriatric conditions at a premature age. As the population of older adults with OUD increases, addressing the health needs of this population will require a geriatric-based approach that maintains function and independence.
Acknowledgements
This research is funded by grants from the National Institute of Health (Bethesda, Maryland): Drs. Benjamin Han and Scott Sherman were funded by grants from the National Institute on Drug Abuse: K23DA043651 (Han) and K24DA038345 (Sherman).
The authors wish to thank the participants and organizations involved in this research for making it possible.
Footnotes
Conflicts of Interest: None
References
- 1.Huhn AS, Strain EC, Tompkins DA, Dunn KE. A hidden aspect of the U.S. opioid crisis: Rise in first-time treatment admissions for older adults with opioid use disorder. Drug Alcohol Depend. 2018;193:142–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Han B, Polydorou S, Ferris R, Blaum CS, Ross S, McNeely J. Demographic Trends of Adults in New York City Opioid Treatment Programs--An Aging Population. Subst Use Misuse. 2015;50:1660–1667. [DOI] [PubMed] [Google Scholar]
- 3.Ward J, Hall W, Mattick RP. Role of maintenance treatment in opioid dependence. Lancet. 1999;353:221–226. [DOI] [PubMed] [Google Scholar]
- 4.Saitz R, Larson MJ. A case for enhanced linkage of substance abusers to primary medical care. Subst Abuse. 1996;17:181–192. [Google Scholar]
- 5.Cigolle CT, Langa KM, Kabeto MU, Tian Z, Blaum CS. Geriatric conditions and disability: the health and retirement study. Ann Intern Med. 2007;147:156–164. [DOI] [PubMed] [Google Scholar]
- 6.Counsell SR, Callahan CM, Clark DO et al. Geriatric care management for low-income seniors: a randomized control trial. JAMA. 2008;298:2623–33. [DOI] [PubMed] [Google Scholar]
- 7.Reece AS. Evidence of accelerated ageing in clinical drug addiction from immune, hepatic and metabolic biomarkers. Immun Ageing. 2007;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams BA, Goodwin JS, Baillargeon J, Ahalt C, Walter LC. Addressing the Aging Crisis in U.S. Criminal Justice Healthcare. J Am Geriatr Soc. 2012;60:1150–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. [DOI] [PubMed] [Google Scholar]
- 10.Bush K, Kivlahan DR, McDonell MB, et al. The AUDIT Alcohol Consumption Questions (AUDIT-C): An effective brief screening test for problem drinking. Arch Internal Med. 1998: 1789–1795. [DOI] [PubMed] [Google Scholar]
- 11.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 12.Kaufmann CN, Canham SL, Mojtabai R, et al. Insomnia and health services utilization in middle-aged and older adults: results from the Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2013;68:1512–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hauser R, Willis R. Survey design and methodology in the Health and Retirement Study and the Wisconsin Longitudinal Study. Popul Develop Rev. 2004;30:209–235. [Google Scholar]
- 14.Center for Disease Control. STEADI - Older Adult Fall Prevention. https://www.cdc.gov/steadi/. Accessed June 1, 2020.
- 15.Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Depend. 2007;88:188–96. [DOI] [PubMed] [Google Scholar]


