Abstract
Purpose:
This study compared differences in sociodemographic characteristics, personal risk perception of lung cancer, lung cancer worry, and synergistic risk perception among rural Appalachia residents who completed home radon testing with those who did not, after receiving a free long-term test kit at a rural primary care clinic. The study also examined the association between the Teachable Moment Model constructs and home radon testing.
Methods:
The study was an exploratory correlational design with a convenience sample of (N = 58) adult participants recruited from 2 rural primary care clinics in Appalachia Kentucky. Participants completed a brief survey and were given a free long-term home radon test kit. Multiple logistic regression was used to determine characteristics associated with home radon testing.
Findings:
Twenty-eight participants (48%) completed home radon testing. There were no differences in personal risk perception of lung cancer, lung cancer worry, or synergistic risk perception between those who completed home radon testing and those who did not. Age was the only significant factor associated with completion of radon testing (B = .077, P = .005). For every 5-year increase in age, participants were 47% more likely to test their home for radon.
Conclusion:
Providing free home radon test kits in the primary care setting shows promise in prompting radon testing in rural Appalachia. As radon-induced lung cancer risk increases with exposure over time, health care providers in rural Appalachia need to encourage patients of all ages to test their home for radon, especially those who smoke or report smoking in the home.
Keywords: Appalachian Region, lung neoplasms, primary health care, radon, rural
Lung cancer, which is highly preventable, is the second most commonly diagnosed cancer, and the leading cause of cancer mortality in the US.1 In 2020, the American Cancer Society estimates 228,820 new cases and approximately 135,720 deaths from lung cancer.1 Appalachian counties in the US, particularly those in Central Appalachia, carry a higher burden of lung cancer than their non-Appalachian counterparts.2
In the US, cigarette smoking is the leading cause of lung cancer, followed by radon gas and secondhand smoke (SHS) exposure.1 Radon exposure is associated with approximately 21,000 new cases of lung cancer each year in the US and of those, approximately 2,900 occur in never smokers.3 While radon exposure is a cause of lung cancer among smokers and non-smokers, a synergistic effect exists between tobacco smoke and radon exposure. Those who are exposed to both tobacco smoke and radon have a 10-fold greater risk of developing lung cancer than non-smokers and those not exposed to SHS.3 For example, when exposed to 4 pCi/L of radon over a lifetime, 62 per 1,000 smokers could develop lung cancer versus 7 of 1,000 never smokers.3
Human exposure to radon occurs largely in the home, and the Environmental Protection Agency (EPA) estimates that 1 in every 15 US homes has a high radon level.4 While there is no safe level of radon exposure, the EPA and the US Surgeon General advise all Americans to test for radon in their home and take action to reduce indoor radon when the level is ≥ 4.0 picocuries per liter of air (pCi/L).5,6 Various radon reduction methods exist; however, installing a mitigation system is the primary method.5
Testing one’s home for radon is necessary to determine exposure risk. Despite public awareness of radon, the proportion of people in the US who have tested remains low, ranging from 3%−15%.7,8 Factors contributing to home radon testing are: higher income,9–12 higher education,9,11–13 urbanicity,12 younger age,8,9 female sex,9 home ownership,8,10 presence of children in the home,14 health concerns,11,15 radon knowledge,8,16 perceived community radon risk,17 living in a high-risk radon zone,8,12 perceived severity,16,17 perceived susceptibility and social influence,15,17 availability of free or discounted test kits,11,13 discussion with a real estate agent,18 and physician recommendation.11
Two studies have examined radon risk perception and testing in a rural population.10,16 In a sample of 31 rural Montana residents, participants knew they could not taste, smell or see radon.10 However, more than one-third of them disagreed with, “health effects due to radon are likely to be serious.” The authors reported significant positive associations between home ownership, income, and radon testing.10 In a study of rural DeKalb County, Illinois, residents (N = 473), females and younger participants were more likely to perceive radon as a health hazard; perceiving radon as a serious health hazard was associated with planning to test for radon.16 There have been no studies examining variables associated with home radon testing in Appalachia.
Eliminating exposure to tobacco smoke and reducing exposure to radon are important primary prevention strategies to reduce incidence and mortality from lung cancer. In the Appalachian Region, the high burden of lung cancer is thought to be due to the disparate prevalence of adult smoking. In the Region’s rural counties, 22.5% of adult residents report smoking compared to 16.3% of the nation.19 However, the EPA labels the majority of Appalachian counties as having moderate to high radon risk potential,20 raising concern for the synergistic effect of tobacco and radon on the development of lung cancer in this region. Despite the alarming lung cancer rates in the region, there is little evidence of radon testing. For example, from 1986–2014, a total of 10,245 home radon values were collected in Appalachia Kentucky, representing a 2% testing rate over 28 years (total housing units, 539,633),21,22 underscoring the need for additional testing in the region.
Given the Appalachian region’s high rates of lung cancer and widespread tobacco use, the relative lack of radon testing is an environmental health concern that necessitates further exploration. To complicate this public health concern, Appalachian residents are disproportionately challenged by high levels of poverty, as well as low levels of income and postsecondary education.19 Exploring factors associated with home radon testing among rural Appalachia residents is needed to assist public health workers to engage residents in taking action to reduce indoor radon levels. Rural health care practitioners can influence radon testing by creating teachable moments during medical visits. Health care visits and events are prime opportunities for teachable moments as they can increase motivation for behavior change.23
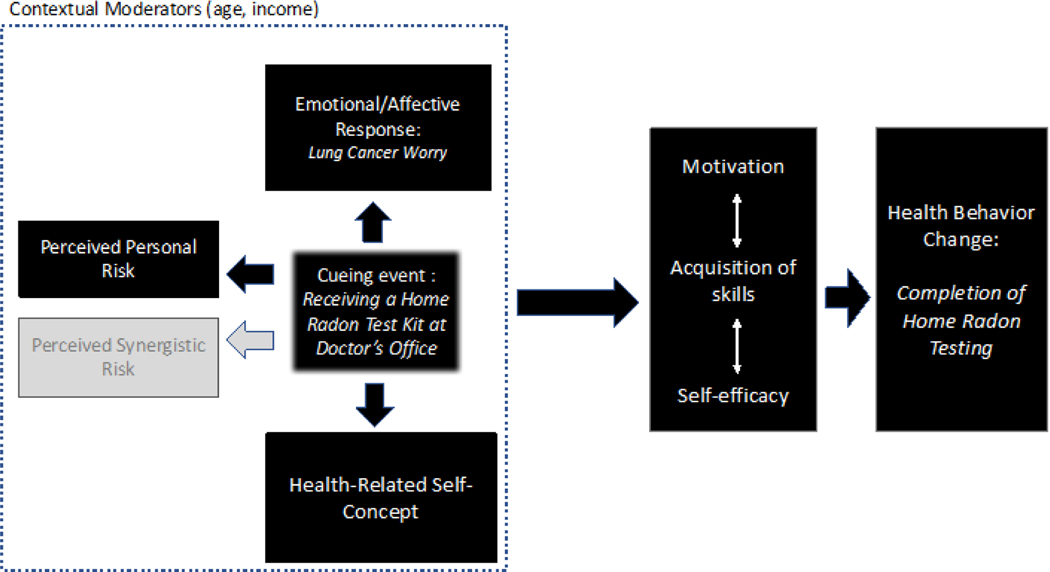
Knowing that not everyone who experiences a health event makes behavioral changes, McBride and associates developed the Teachable Moment Model (TMM) to guide research on individual health behavior change (Figure 1).23 The TMM suggests that individuals are more likely to take action when they experience a health event that causes them to reflect upon their beliefs and knowledge about their own health, increases their perception of personal risk, and creates a strong affective or emotional response.23 In addition, this subjective assessment of health events may be influenced by an individual’s sociodemographic characteristics.23 As such, we used the TMM to guide this research. As more radon-induced lung cancers occur in those with a history of tobacco smoke exposure, an additional construct, perceived synergistic risk, was added to the model to better understand its contribution to taking action to reduce residential radon in rural Appalachia.
Figure 1. Heuristic Model for Teachable Moment.
Note. Adapted from McBride et al., 2003. Original constructs are in black
This exploratory correlational study aimed to: 1) compare differences in sociodemographic characteristics, personal risk perception, emotional response as measured by lung cancer worry, and synergistic risk perception differences among rural Appalachia residents who completed home radon testing with those who did not, after receiving a free long-term test kit at a rural primary care clinic; and 2) examine the association between the TMM constructs of personal risk perception, emotional response, and synergistic risk perception and home radon testing in a small sample of rural Appalachian residents. It was hypothesized that participants with higher perceived personal lung cancer risk, greater lung cancer worry, and higher synergistic risk perception would be more likely to test their home for radon after receiving a free radon test kit at their primary care office compared to those with lower perceived personal lung cancer risk, less lung cancer worry, and lower synergistic risk perception.
Methods
Design and Sample
This was an exploratory correlational study. Quantitative methods were used to analyze findings from a self-report survey and environmental exposure assessment. A convenience sample of 58 adult participants was recruited from 2 rural primary care clinics affiliated with a regional medical center in Central Appalachian Kentucky. Healthy males and females aged 18–90 years and of all racial/ethnic groups who were able to speak and read English were invited to participate, regardless of whether they owned their home. Prior to recruitment, 2 investigators conducted a 45-minute lunch-and-learn session with clinic staff to review study procedures and provide basic information on lung cancer risks from radon, home radon testing, and mitigation. Each staff member received a Healthcare Providers & Radon Prevention pamphlet providing information on radon as a health risk and illustrating how health care providers can inform patients about radon, prescribe home radon testing, and encourage patients to test and mitigate if home radon concentrations are ≥ 4.0 pCi/L.24 In addition, the pamphlet provides health care providers with Kentucky-specific radon statistics and the EPA’s Kentucky Radon Zone Map.24
Procedures
Clinic staff approached all patients with clinic appointments at check-in and invited them to test their homes for radon and take a brief confidential paper-and-pencil survey to assess lung cancer risk factors and perceived risk. If the patient expressed interest, clinic staff provided a cover memo inviting them to take part in the study to help investigators understand how to help patients test and fix their home for radon, the survey, a free long-term radon test kit, and instructions on how to deploy the test kit in their home. Participants were instructed to complete the survey on site and place in an envelope stamped ‘Confidential’ and return to clinic staff. The University of Kentucky Institutional Review Board granted a waiver of documentation of informed consent due to the logistics of conducting research in busy clinic waiting rooms. Enrollment began in August 2015, was completed within 2 weeks, and participants were asked to deploy the radon test kit no later than mid-September 2015. Participants received 2 reminder phone calls. The first call was to remind participants to deploy their test kit 1 week after enrollment and to answer any questions about the testing process. Participants were called a second time 90 days after enrollment to remind them to return their test kit using the postage-paid envelope. Test kit results were mailed to the principal investigator and then to the participants with a letter explaining the results. For those with radon levels ≥ 4.0 pCi/L, the letter provided guidance on creating radon-free and, when applicable, smoke-free homes. The study was approved by the university’s Medical Institutional Review Board.
Measures
Sociodemographic/Personal Characteristics
We obtained self-report data on sociodemographic and personal characteristics including age, length of time at current residence, sex, education, marital status, race/ethnicity, employment, household income, home ownership, presence of children in the home, presence of SHS in the home, and personal smoking status.
Personal Risk Perception
Personal risk perception of lung cancer was assessed by asking participants to, “Rate your risk of developing lung cancer in your lifetime,” on a scale of 0–10 with “0” being lowest perceived risk and “10” being highest perceived risk.
Emotional Response
Emotional response was assessed by measuring lung cancer worry using the 4-question Lung Cancer Worry Scale.24 Butler and associates adapted the scale from the 3-item validated Cancer Worry Scale developed by Lerman and associates.24,25 The first question is, “How much do you currently worry about getting lung cancer some day?” (5-point Likert scale from (1) not at all to (5) almost all of the time). The remaining questions, “How much do worries about lung cancer impact your mood?”, “How much do worries about lung cancer impact your daily activities?”, and “When you worry about lung cancer, how difficult is it to control these worries?”, were measured on a 4-point Likert scale from (1) not at all to (4) a lot. The first item was multiplied by a factor of 0.8, resulting in a maximum possible value of 4 to ensure that each of the scale items received equal weight in the total score, representing the sum of the 4 items. The potential range of scores was 3.8–16.0, with higher scores indicating greater lung cancer worry. According to Butler and associates, the Lung Cancer Worry Scale has good internal consistency, with a Cronbach alpha coefficient of 0.82.24 In the study reported here, the Cronbach alpha coefficient for this 4-item scale was 0.79.
Synergistic Risk Perception
Synergistic risk perception was assessed by asking participants to “Rate the risk from being exposed to radon AND smoking a pack of cigarettes per day, compared to the risk of only smoking a pack of cigarettes a day with no radon exposure” (5-point Likert scale ranging from (1) “much less risky” to (5) “much more risky”).15,25,27–28
Home Radon Testing
At baseline, participants were asked “Have you ever tested your home for radon?” (yes/no). Home radon levels were measured using Radon Safety Services Inc. Alpha-track Radon Detectors (RSSI, Morton Grove, IL), commercially available long-term radon gas detectors.29 We asked participants to deploy their detector for a minimum of 90 days. As results were received, participants were classified as “yes” for testing, and radon concentrations ≥ 4.0 pCi/L were considered high.4
Data Analysis
Descriptive statistics using means and standard deviations or frequency distributions were used to summarize study variables. Bivariate analysis, including 2-sample t test and chi-square test for independence was used, as appropriate, to compare study variables between those who completed home radon testing and those who did not.
Multiple logistic regression was used to examine personal risk perception, lung cancer worry, and synergistic risk perception as factors associated with home radon testing among rural Appalachia residents, controlling for sociodemographic variables. With the goal of having at least 10 observations per predictor,30 the sample size limited the number of predictor variables included in the regression model to 5 variables. Two sociodemographic variables, including age and income, were included in the regression model based on significant findings from the bivariate analysis and previous research finding an association between age,8,9 higher income9–12 and completion of home radon testing. The Hosmer-Lemeshow goodness-of-fit test assessed model fit. Preliminary analyses using variance inflation factors were conducted to ensure no multicollinearity. All quantitative data analysis was conducted using Statistical Package for the Social Science (SPSS) version 25 (IBM Corp., Armonk, NY), with an alpha level of 0.05 throughout.
Results
Sample Characteristics
Table 1 summarizes sample sociodemographic and personal characteristics by group. The mean age of the sample was 46 years (SD = 14). The reported mean length in years at their current residence was 11 (SD = 10). Overall, most were female (71%), with at least a high school education (86%), married (66%), White/non-Hispanic (86%), and either employed or retired (69%). Forty-one percent reported an income less than $30,000 and 77% reported owning their home. Half of participants reported the presence of children in the home. Sixty percent reported living in a smoke-free home, and nearly three-fourths indicated they did not currently smoke cigarettes (74%). Overall, personal risk perception of lung cancer ratings indicated low perceived risk with an average rating of 3.5 (SD = 3.0; range 0–10). Very few respondents indicated they worry much about lung cancer, with an average score of 6 (SD= 2.5; range 3.8–13.4). Synergistic risk perception scores indicated the majority of respondents perceived the synergistic risk to be more risky than exposure to tobacco alone without radon exposure (M = 3.6, SD = 1.2; range 1–5). Lastly, 2 (3%) of the 58 participants reported that they had previously tested their homes for radon.
Table 1.
Sample Characteristics of the Total Sample and by Home Radon Testing Group Using Two-Sample t test or Chi Square Test for Independence
| Total Sample N=58 | Completed Radon Testing n = 28 | Did Not Complete Radon Testing n = 30 | ||
|---|---|---|---|---|
|
| ||||
| Characteristic | Mean ± SD | Mean ± SD | Mean ± SD | P |
|
| ||||
| Age (years) | 46 ± 14 | 51 ± 11 | 40 ± 17 | .008 |
|
| ||||
| Length of time at current residence (years) | 11 ± 10 | 12 ± 10 | 11 ± 10 | .626 |
|
| ||||
| Personal risk perception | 3.5 ± 3.0 | 3.3 ± 2.9 | 3.6 ± 3.0 | .690 |
|
| ||||
| Lung cancer worry | 6.0 ± 2.5 | 6.1 ± 2.7 | 5.9 ± 2.3 | .824 |
|
| ||||
| Synergistic risk perception | 3.6 ± 1.2 | 3.7 ± 1.2 | 3.5 ± 1.3 | .493 |
|
| ||||
| n (%) | n (%) | n (%) | P | |
|
| ||||
| Sex | >.99 | |||
| Male | 15 (26%) | 7 (25%) | 8 (27%) | |
| Female | 41 (71%) | 21 (75%) | 20 (67%) | |
| Missing data | 2 (3%) | 0 (0%) | 2 (7%) | |
|
| ||||
| Level of education | .410a | |||
| < High school | 8 (14%) | 4 (14%) | 4 (13%) | |
| HS graduate/GED | 18 (31%) | 11 (39%) | 7 (23%) | |
| > High school | 32 (55%) | 13 (46%) | 19 (63%) | |
|
| ||||
| Marital status | .623 | |||
| No | 18 (31%) | 7 (27%) | 11 (37%) | |
| Yes | 38 (66%) | 19 (73%) | 19 (63%) | |
| Missing | 2 (3%) | 2 (7%) | 0 (0%) | |
|
| ||||
| Race and ethnicity | .493a | |||
| White and non-Hispanic | 50 (86%) | 24 (86%) | 26 (93%) | |
| Other | 2 (3%) | 0 (0%) | 2 (7%) | |
| Missing data | 6 (10%) | 4 (14%) | 2 (7%) | |
|
| ||||
| Employment status | .642 | |||
| Employed/Retired | 40 (69%) | 18 (64%) | 22 (73%) | |
| Unemployed/Disabled | 16 (28%) | 9 (32%) | 7 (23%) | |
| Missing data | 2 (3%) | 1 (4%) | 1 (3%) | |
|
| ||||
| Income | 24 (41%) | 13 (46%) | 11 (37%) | .427 |
| <$30,000 | 24 (41%) | 13 (46%) | 11 (37%) | |
| ≥$30,000 | 28 (48%) | 11 (39%) | 17 (57%) | |
| Missing | 6 (10%) | 4 (14%) | 2 (7%) | |
|
| ||||
| Home ownership | .441 | |||
| Own | 45 (77%) | 23 (82%) | 22 (73%) | |
| Rent | 12 (21%) | 4 (14%) | 8 (27%) | |
| Missing data | 1 (2%) | 1 (4%) | 0 (0%) | |
|
| ||||
| Children present in the home | .292 | |||
| No | 27 (47%) | 15 (54%) | 12 (40%) | |
| Yes | 29 (50%) | 11 (39%) | 18 (60%) | |
| Missing | 2 (3%) | 2 (7%) | 0 (0%) | |
|
| ||||
| SHS in the home | >.99 | |||
| No | 35 (60%) | 17 (61%) | 18 (60%) | |
| Yes | 23 (40%) | 11 (39%) | 12 (40%) | |
|
| ||||
| Current smoker | .263 | |||
| No | 43 (74%) | 23 (82%) | 20 (67%) | |
| Yes | 13 (22%) | 4 (14%) | 9 (30%) | |
| Missing | 2 (3%) | 1 (4%) | 1 (3%) | |
|
| ||||
| Previous Home Radon Testing | .229a | |||
| No | 56 (97%) | 26 (93%) | 30 (100%) | |
| Yes | 2 (2%) | 2 (7%) | 0 (0%) | |
Note.
Fisher’s Exact Test used as an alternate to the chi-square test of association due to small expected cell counts.
Home Radon Testing and Self-Reported Tobacco Smoke Exposure
Twenty-eight of the 58 (48%) home radon test kits distributed were returned for analysis. Home radon levels for the sample averaged 4.2 pCi/L (SD = 4.4). Eight of those who tested (29%) had radon levels at or above the EPA action level, with values ranging from 4.7– 19.5 pCi/L. Of the 8 with high radon levels, 3 (38%) reported smoking in the home.
Bivariate Relationships with Home Radon Testing
Age was the only variable significantly associated with completion of home radon testing (Table 1). Compared to those who did not complete home radon testing, participants who tested their homes for radon were older (M = 51 years, SD = 11 years versus M = 40, SD = 17 years, respectively; P = .008).
Multivariable Relationships with Home Radon Testing
The logistic regression to assess factors associated with home radon testing was statistically significant, x2(5, N = 48) = 11.1, P = .05. As shown in Table 2, age was the only independent variable to make a unique statistically significant contribution to the model, with an odds ratio of 1.080 [CI: 1.023–1.140]. For each 1-year increase in age, the odds of testing for radon in the home increased by 8%. For every 5-year increase in age, participants were 47% more likely to test their home for radon, controlling for other factors in the model. Personal risk perception, lung cancer worry, synergistic risk perception, and income did not make statistically significant contributions to the model in this sample of rural Appalachia Kentucky residents. All variance inflation factors for this model were smaller than 2.1, indicating multicollinearity did not distort regression parameters.
Table 2.
Logistic Regression Examining the Association Between the Teachable Moment Model Constructs and Completion of Home Radon Testing (n=48)
| Variable | B | SE | OR | 95% CI | Wald Statistic | P |
|---|---|---|---|---|---|---|
| Age (years) | .077 | .027 | 1.080 | 1.023–1.140 | 7.862 | .005 |
| Income | −1.149 | .739 | .317 | .074–1.350 | 2.415 | .120 |
| Personal risk perception | −.039 | .157 | .962 | .707–1.309 | .062 | .804 |
| Lung cancer worry | −.035 | .193 | .966 | .662–1.410 | .032 | .858 |
| Synergistic risk perception | .116 | .297 | 1.123 | .627–2.011 | .152 | .696 |
Discussion
Overall, distributing free radon test kits in the primary care setting prompted nearly half of the study participants to test their homes for radon. This is promising, as only 65 observed radon values had been documented from 1986–2014 in the same 2 study counties.22 This one-time distribution of free radon test kits in 2 primary care clinics yielded one-third as many observed radon values as were documented over 28 years in this 2-county area.22 While the positive impact of providing free radon test kits at the point-of-care may not be surprising, this practice is not standard practice in the US.31 Yet, our finding is consistent with previous research which found the availability of free or discounted test kits was associated with completion of home radon testing11,13 and provides support for the in-person provision of free test kits in primary care offices as a primary lung cancer prevention strategy. In contrast to several other studies, neither sex,9 education,9,11–13 income,9–12 home ownership,8,10 nor the presence of children in the home14 were associated with home radon testing in this sample. Additionally, length of home residency, marital status, race/ethnicity, employment, and smoking variables were not associated with home radon testing in this rural Appalachian sample. It is promising that several of the variables historically regarded as social determinants of health (ie, income and educational attainment) were not associated with home radon testing. Further research on home radon testing in rural Appalachia is needed, but findings from this exploratory study suggest that many residents may test their homes for radon if radon test kits are made readily accessible.
When comparing those who tested their homes for radon and those who did not, age was the only variable significantly associated with home radon testing. Participants who tested their home for radon were older (M = 51 years vs. M = 40 years, respectively). Similarly, in the model, the only independent variable associated with completion of home radon testing was age. As age increased, participants were more likely to test their home for radon, controlling for other factors in the model. Our findings are in contrast to previous studies in which younger age was associated with home radon testing.8,9 This unexpected finding may be related to the age composition of different study samples. Whereas 36% of the participants in our study were 44 years or younger, 45% of those in the study by Wang and associates8 were in this category. Similarly, 29% of the participants in our study were 39 years or younger, compared with 47% in the Halpern and associates9 study. This suggests that the prior finding of younger participants being more likely to test for radon may have been observed in a sample that is skewed toward younger adults, which did not apply to our study.
In our sample, the 25th percentile for age was 38 years and the 75th was 57 years. Within this range of ages, the observation that younger participants in rural Appalachia were less likely to test their home for radon is of particular concern, potentially exposing individuals and their families to the environmental carcinogen in the home for many years. Additionally, young adults in the US have significantly lower rates of office-based health care utilization than all other age groups,32 demonstrating the need for public health officials to develop novel ways to disseminate primary prevention strategies to younger, rural Appalachian populations. As radon-induced lung cancer risk increases with exposure over time, health professionals need to stress the importance of radon testing with all patients when discussing health promotion strategies, particularly among those who smoke or are exposed to SHS. More research is needed to understand the association between age and radon testing in Appalachia.
Contrary to the hypothesis, higher perceived personal lung cancer risk, greater lung cancer worry, and higher synergistic risk perception scores were not associated with testing one’s home for radon in this sample of rural Appalachian participants. Although the statistical model including these variables was significant overall, none of these factors made a significant contribution individually. One explanation for this finding is that average scores for personal risk perception and lung cancer worry were low in this sample, suggesting relatively little variability among respondents. This may have been due to the fact that the majority of participants were non-smokers living in smoke-free homes. In previous research, current smokers and those reporting smoking in the home rated their personal risk perception of lung cancer and lung cancer worry significantly higher than non-smokers and those not exposed to SHS in the home.24 Without exposure to tobacco, a widely known lung carcinogen, participants may not have perceived themselves at risk for lung cancer and, therefore, may not have experienced a strong emotional response to the cue to action. Additionally, little to no education on radon testing was provided to participants prior to completing the survey. It is possible some participants in this study lacked knowledge of the health hazards associated with radon exposure and therefore did not perceive themselves at risk for lung cancer and would thus not express worry about developing the disease. In a study by Duckworth and associates,16 473 participants from rural Illinois were surveyed about their knowledge of radon as a health hazard. While the majority identified radon as a gas, 44% did not know that radon was associated with lung cancer. Furthermore, Hill and associates10 found that many rural families underestimate the seriousness of the long-term health effects related to radon exposure, possibly contributing to the lack of perceived personal lung cancer risk and lung cancer worry in this sample. Interventions aimed at assessing radon knowledge and increasing radon risk perception among rural populations are warranted.
In addition, the sample’s mean score for synergistic risk perception fell between the perception of equal risk and more risk. As those who are exposed to tobacco smoke and radon have a 10-fold greater risk of developing lung cancer than those exposed to radon alone, the relatively low mean synergistic risk score is concerning, as participants did not perceive the combination of tobacco and radon to be much more risky to one’s health. Numerous studies from around the world have demonstrated the combined effects of tobacco and radon exposure on lung cancer, with more radon-induced lung cancers occurring among smokers.33–43 Perceiving the synergistic risk associated with the combined effects of tobacco and radon as anything but “much more risky” indicates a lack of public awareness about the increased risk for lung cancer when exposed to both tobacco smoke and radon. Health care practitioners in rural Appalachia are well suited to bring radon awareness to the public by discussing primary lung cancer prevention strategies with patients including home radon testing, mitigation, and creating smoke-free homes and vehicles. Educating tobacco users and those who are exposed to SHS about the combined risks of radon and tobacco exposure may further serve as a cue to action for radon testing.
Strengths and Limitations
The findings from this study provide preliminary evidence of the need for public education about radon and its harmful effects on one’s health, particularly when combined with tobacco exposure, in rural Appalachia. In addition, evidence from this study supports the provision of free radon test kits in primary care clinics to promote home radon testing. Despite the small sample size, this is the first study to explore home radon testing in rural Appalachia. Previous research which examined radon risk perception and testing in rural populations10,16 did so in non-Appalachian regions of the US. In addition, 1 of the aforementioned studies10 reported findings from an even smaller sample, highlighting the fact that home radon testing in rural Appalachia is under-researched.
In this exploratory study, because of a limited number of radon test kits available, we did not conduct an a priori power analysis to estimate the minimum sample size it would take to detect a specific effect; this is a limitation. Another related limitation is the small sample size, which restricted the number of predictor variables that could be included in the logistic regression model. Furthermore, the convenience sample may have resulted in self-selection bias as participants may have been more motivated to take health actions given they were recruited at a primary care office. Given the sample characteristics, participants were also not representative of the low socioeconomic population in the region, as the majority of the sample were homeowners who were non-smokers and lived in smoke-free homes, were employed, and had at least some post-secondary education. In addition, we did not measure participants’ knowledge of radon nor their health-related self-concept, limiting our understanding of their influence on radon testing. Lastly, participants were not asked if their health care provider counseled them on home radon testing. As a doctor’s recommendation has been found to be significantly associated with home radon testing,11 this limited the internal validity of our findings. Future radon testing studies would benefit from using quota sampling with a larger number of participants, so they would be more inclusive of tobacco smokers and/or those exposed to tobacco smoke to account for synergistic risk. The larger sample would also provide for more robust group comparisons.
While the limited sample size does not allow for generalization of the findings, there are areas of concern highlighted in the study findings that have implications for clinical and public health practice in rural Appalachian communities. Due to the synergism between tobacco and radon, it is important for all health care providers and public health professionals to screen for tobacco exposure and encourage all patients to test their homes for radon, especially those who smoke or report smoking in the home. In this study, providing free, in-person home radon test kits in the primary care office served as a cue to action and may be a promising way to increase radon testing in rural Appalachia. Lung cancer rates in the region and evidence from this study necessitate further exploration of the variables associated with radon testing in rural Appalachia. Future studies that explore radon testing in rural Appalachia need to include a larger, more diverse sample with varying demographics and measurement of radon knowledge and health-related self-concept. Additionally, further exploration of home radon testing among rural Appalachia residents guided by other health behavior theories or models such as the Health Belief Model,44,45 Social Cognitive Theory,46 and the Theory of Planned Behavior47 may be considered to guide the development of evidence-based tailored interventions that prompt individuals to take action to reduce radon exposure in the home.
Conclusions
This exploratory correlational study was an effort to understand variables associated with home radon testing in a rural Appalachian population. While the small sample size may limit the generalizability of findings, results from this study reveal that the provision of free, in-person home radon test kits as a cue to action in the primary care setting shows promise in increasing radon testing in rural Appalachia. Given that younger participants were less likely than older ones to complete home radon testing, the cumulative effects of radon exposure on the development of lung cancer are concerning. Home radon testing is a primary strategy for the prevention of lung cancer and is an essential step to reducing the burden of the disease in rural Appalachia. Because there is no safe level of radon exposure, it is important for all health care providers in rural communities to include radon assessment as part of their patient education and encourage all patients to test their homes, especially those who smoke or report smoking in the home.
Acknowledgments:
The authors would like to thank St. Claire HealthCare and the Northeast Area Health Education Center for partnering on this project.
Funding: This publication was supported, in part, by UK-CARES through Grant P30 ES026529. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Environmental Health Sciences.
References
- 1.American Cancer Society. Cancer facts & figures 2020. Atlanta, GA: American Cancer Society; 2020. Available at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf. Accessed January 6, 2020. [Google Scholar]
- 2.Wilson RJ, Ryerson AB, Singh SD, et al. Cancer incidence in Appalachia, 2004–2011. Cancer Epidemiol Biomarkers Prev. 2016;25(2): 250–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Environmental Protection Agency. Health risks from radon. United States Environmental Protection Agency. https://www.epa.gov/radon/health-risk-radon. Updated July 24, 2019. Accessed November 18, 2019. [Google Scholar]
- 4.Environmental Protection Agency. A citizen’s guide to radon. The guide to protecting yourself and your family from radon. https://www.epa.gov/sites/production/files/2016-12/documents/2016_a_citizens_guide_to_radon.pdf. Updated December, 2016. Accessed November 18, 2019.
- 5.Environmental Protection Agency. Consumer’s guide to radon reduction. How to fix your home. https://www.epa.gov/sites/production/files/2016-12/documents/2016_consumers_guide_to_radon_reduction.pdf. Updated December, 2016. Accessed November 18, 2019.
- 6.United States Department of Health and Human Services, Office of the Surgeon General. Surgeon General releases national health advisory on radon. http://www.adph.org/radon/assets/surgeon_general_radon.pdf. Published January 13, 2005. Accessed November 19, 2019.
- 7.Eheman C, Ford E, Staehling N, et al. Knowledge about indoor radon in the United States: 1990 national health interview survey. Arch Environ Health. 1996;51(3):245–247. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Ju C, Stark AD, et al. Radon awareness, testing, and remediation survey among New York State residents. Health Phys. 2000;78(6):641–647. [DOI] [PubMed] [Google Scholar]
- 9.Halpern MT, Warner KE. Radon risk perception and testing: Sociodemographic correlates. J Environ Health. 1994;56(7):31–35. [Google Scholar]
- 10.Hill WG, Butterfield P, Larsson LS. Rural parent’s perceptions of risks associated with their children’s exposure to radon. Public Health Nurs. 2006;23(5);392–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nissen MJ, Leach JW, Nissen JA, et al. Radon testing and mitigation: An intervention in a primary care setting. J Cancer Educ. 2012;27:566–572. [DOI] [PubMed] [Google Scholar]
- 12.Zahn WE, Mueller-Luckey GS, Ratnapradipa K, et al. Predictors and spatial variation of radon testing in Illinois, 2005–2012. J Public Health Manag Pract. 2017;00(00): 1–9. [DOI] [PubMed] [Google Scholar]
- 13.Butler KM, Huntington-Moskos L, Rayens MK, et al. (2018). Access to free home test kits for radon and secondhand smoke to reduce environmental risks for lung cancer. J Environ Health. 2018;81(3):E1–E6. [Google Scholar]
- 14.DiPofi JA, LaTour MS, Henthorne TL. The new social marketing challenge to promote radon testing. Health Mark Q. 2001;19(1):79–90. [DOI] [PubMed] [Google Scholar]
- 15.Rinker GH, Hahn EJ, Rayens MK. Residential radon testing intentions, perceived radon severity, and tobacco use. J Environ Health. 2014;76(6):42–47. [PubMed] [Google Scholar]
- 16.Duckworth LT, Frank-Stromborg M, Oleckno WA, et al. Relationship of perception of radon as a health risk and willingness to engage in radon testing and mitigation. Onc Nurs Forum. 2002;29(7):1099–1107. [DOI] [PubMed] [Google Scholar]
- 17.Weinstein ND, Sandman PM, Roberts NE. Perceived susceptibility and self-protective behavior: A field experiment to encourage home radon testing. Health Psychol. 1991;10(1):25–33. [DOI] [PubMed] [Google Scholar]
- 18.Neri A, McNaughton C, Momi B, et al. Measuring public knowledge, attitudes, and behaviors related to radon to inform cancer control activities and practices. Indoor Air. 2018;28:604–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marshall JL, Thomas L, Lane NM, et al. Creating a culture of health in Appalachia: Disparities and bright spots. Appalachian Regional Commission. https://www.arc.gov/assets/research_reports/Health_Disparities_in_Appalachia_August_2017.pdf. Published August, 2017. Accessed April 29, 2020. [Google Scholar]
- 20.Environmental Protection Agency. EPA map of radon zones. https://www.epa.gov/radon/find-information-about-local-radon-zones-and-state-contact-information#radonmap. Updated April 23, 2020. Accessed April 29, 2020.
- 21.Pollard K, Jacobsen LA. The Appalachian Region: A data overview from the 2010–2014 American Community Survey. Appalachian Regional Commission. https://www.arc.gov/assets/research_reports/DataOverviewfrom2010to2014ACS.pdf. Published April, 2016. Accessed April 29, 2020. [Google Scholar]
- 22.Radon Policy Division. Kentucky residential radon registry, 1986–2014. BREATHE, University of Kentucky College of Nursing and Kentucky Geologic Survey; (unpublished data). [Google Scholar]
- 23.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–170. [DOI] [PubMed] [Google Scholar]
- 24.University of Kentucky College of Nursing Radon Policy Research Program. Healthcare Providers & Radon Prevention [Pamphlet]. Lexington, KY: University of Kentucky; 2011. https://www.uky.edu/breathe/sites/breathe.uky.edu/files/Radon_Physician_Brochure_FINAL.pdf [Google Scholar]
- 25.Butler KM, Rayens MK, Wiggins AT, et al. Association of smoking in the home with lung cancer worry, perceived risk, and Synergistic risk. Onc Nurs Forum. 2017;44(2):E55–E63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lerman C, Trock B, Rimer B, et al. Psychological side effects of breast cancer screening. Health Psychol. 1991;10:259–267. [DOI] [PubMed] [Google Scholar]
- 27.Hahn EJ, Rayens MK, Kercsmar SE, et al. Dual home screening and tailored environmental feedback to reduce radon and secondhand smoke: An exploratory study. J Environ Health. 2013; 76(6):156–161. [PubMed] [Google Scholar]
- 28.Hahn EJ, Wiggins AT, Rademacher K, et al. FRESH: Long-term outcomes of a randomized trial to reduce radon and tobacco smoke in the home. Prev Chronic Dis. 2019: 16(E127): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radon Safety Services Inc. RSSI’s Alpha-track radon detector. https://www.rssi.us/radon-alpha-track-radon-detector.htm. Updated 2019. Accessed May 11, 2020.
- 30.Babyak MA. What you see may not be what you get: A brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66(3):411–421. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Preventive Services Task Force (n.d) Recommendations: Cancer. Retrieved October 23, 2020, from https://www.uspreventiveservicestaskforce.org/uspstf/topic_search_results?topic_status=P&category%5B%5D=15&searchterm=
- 32.Lau J, Adams S, Boscardin W, et al. Young adults’ health care utilization and expenditures prior to the affordable care act. J Adolesc Health. 2014;54:663–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ajrouche R, Roudie C, Clero E, et al. Quantitative health impact of indoor radon in France. Radiat Environ Biophys. 2018;57:205–214. [DOI] [PubMed] [Google Scholar]
- 34.Bochicchio F, Antignani S, Venoso G, et al. Quantitative evaluation of the lung cancer deaths attributable to residential radon: A simple method and results for all the 21 Italian regions. Radiat Meas. 2013;50:121–126. [Google Scholar]
- 35.Chen J, Moir D, Whyte J. Canadian population risk of radon induced lung cancer: A re-assessment based on the recent cross-Canada radon survey. Radiat Prot Dosimetry. 2012;152(1–3):9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Darby S, Hill D, Auvinen A, et al. Radon in homes and risk of lung cancer: collaborative analysis of individual data from 13 European case-control studies. BMJ. 2005;330:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grundy A, Brand K, Khandwala F, et al. Lung cancer incidence attributable to residential radon exposure in Alberta in 2012. CMAJ Open. 2017;5(2):E529–E534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee HA, Lee WK, Lim D, et al. Risks of lung cancer due to radon exposure among the regions of Korea. J Korean Med Sci 2015;30:542–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Menzler S, Piller G, Gruson M, et al. Population attributable fraction for lung cancer due to residential radon in Switzerland and Germany. Health Phys. 2008;95(2):179–189. [DOI] [PubMed] [Google Scholar]
- 40.National Research Council Committee on Health Risks of Exposure to Radon. Health effects of exposure to radon: BEIR VI. Washington, DC: National Academy Press; 1999. [Google Scholar]
- 41.Peterson E, Aker A, Kim J, et al. Lung cancer risk from radon in Ontario, Canada: how many lung cancers can we prevent? Cancer Causes Control. 2013;24:2013–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Truta-Popa LA, Dinu A, Dicu T, et al. Preliminary lung cancer risk assessment of exposure to radon progeny for Transylvania, Romania. Health Phys. 2010;99(3):301–307. [DOI] [PubMed] [Google Scholar]
- 43.Veloso B, Nogueira JR, Cardoso MF. Lung cancer and indoor radon exposure in the north of Portugal - an ecological study. Cancer Epidemiol. 2012;36:e26–e32. [DOI] [PubMed] [Google Scholar]
- 44.Hochbaum GM. Public Participation in Medical Screening Program: A Socio-Psychological Study. Washington, DC: U.S. Department of Health, Education and Welfare; 1958. [Google Scholar]
- 45.Rosenstock IM. What research in motivation suggests for public health. American Journal of Public Health and the Nation’s Health. 1960;50:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bandura A Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 47.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]