Abstract
Objective
Heart Rate Variability (HRV) is a marker of autonomic nervous system function associated with both physical and mental health. Many studies have suggested that mindfulness and meditation-based interventions (MBIs) are associated with improvements in HRV, but findings are mixed and to date no comprehensive meta-analysis has synthesized results.
Methods
Systematic literature searches were conducted using PsycINFO, Embase, Medline, CINAHL, ERIC and Scopus to identify randomized controlled trials (RCTs) investigating the effects of predominantly seated MBIs on resting-state vagally-mediated HRV. Risk of bias was judged using the Cochrane Risk of Bias tool.
Results
Nineteen RCTs met criteria for inclusion in the meta-analysis. Random-effects meta-analysis found that MBIs were not efficacious in increasing vagally-mediated resting-state HRV relative to control conditions (Hedges’ g = 0.38, 95% CI = − 0.014 to 0.77). When removing an outlier (g = 3.22), the effect size was reduced, confidence interval narrowed, and findings remained non-significant (g = 0.19, 95% CI = −0.02 to 0.39). High heterogeneity in results (I2 = 89.12%) could not be explained by a priori determined moderators including intervention duration, study setting and control type.
Conclusion
There is currently insufficient evidence to indicate that MBIs lead to improvements in vagally-mediated HRV over control conditions. Future large, well-designed RCTs with low risk of methodological bias could help add to the current evidence to elucidate any role MBIs might play in impacting HRV.
Keywords: Mindfulness, meditation, heart rate variability, vagal tone, respiratory sinus arrhythmia, mechanisms, meta-analysis
INTRODUCTION
Mindfulness and meditation-based interventions (MBIs) have become increasingly popular (1), given their potential to facilitate adaptive physical and psychological change (2). MBIs are a class of psychological intervention that focus on developing the skill of non-judgmental awareness of the present moment (i.e. mindfulness) and attentional training (3).The mechanisms underlying potential benefits of MBIs remains unclear and are the focus of increasing attention (4, 5). While there has been much focus on self-reported mechanisms, potential changes to physiological functioning are of particular interest (6, 7) and could provide more robust evidence of the utility of MBIs.
One such physiological marker, attracting rapidly growing attention, is heart rate variability (HRV). HRV, defined as beat-to-beat variations in heart rate, reflects the interplay between parasympathetic and sympathetic influences on heart rate. Vagally-mediated HRV indices that specifically reflect parasympathetic modulation of heart rate include time-domain measures (e.g. the root-mean-square of successive R-R-interval differences; RMSSD), high-frequency (HF) HRV and respiratory sinus arrhythmia (RSA) (8). Indices of vagally-mediated cardiac activity and reactivity are of particular clinical interest because vagal tone is indicative of the sensitivity of the nervous system to everchanging physical and emotional demands in the environment (9). Longitudinal studies have found that high HRV is a powerful indicator of health outcomes such as morbidity and risk of mortality in both medical (10, 11) and community settings (12-14). Moreover, because the prefrontal cortical activity crucial to top-down regulation of emotions also produces inhibitory input to the sinoatrial node by way of the parasympathetic nervous system, vagally-mediated HRV can be considered a peripheral biomarker of emotion regulation (15), though viewpoints are mixed (16). Regardless of what process it reflects, HRV is correlated with indicators of mental health and well-being, including greater psychological flexibility, social approach behaviors, and reduced risk of mental illness (15, 17).
Self-reported mindfulness, as well as MBIs, are associated with enhanced emotion regulation and cognitive control (5, 18), however prior findings are largely reliant on self-reported measures of emotion regulation, which can have notable construct overlap with measures of mindfulness (19). Therefore, there is a need to ascertain the extent to which MBIs are associated with underlying changes in physiological indicators, such as vagally-mediated HRV. MBIs appear to enhance the regulation of emotion by facilitating reduction of evaluative processing, which is supported by structures along the cortical midline, in favor of recruitment of a nonconceptual sensory pathway, supported by a limbic pathway (20, 21). In other words, mindfulness may offer an alternative to effortful top-down cognitive control of negative emotions by instead promoting a more nonconceptual, body-based way of experiencing emotions (20, 21). Thus MBIs may result in improvements in cognitive control and emotion regulation that, by proxy, would be evidenced by increases in HRV (15, 20, 21).
There is some evidence that MBIs are associated with adaptive increases in HRV (22, 23), however findings are mixed (24, 25) and a comprehensive quantitative synthesis of findings is lacking. A scoping review was recently published (26) but did not include any quantitative assessment. To date just one meta-analysis has considered HRV changes associated with MBI participation (27). Synthesizing results from four studies, Radmark and colleagues (27) found no evidence of an association between MBI participation and changes in HRV. Unfortunately, the inclusion of only four studies limited the statistical power to detect a true effect and limited the generalizability of results. Additionally, the analysis was not limited to randomized controlled trials (RCTs), which can increase the risk of bias (28). Finally, results for four different – yet highly inter-correlated measures of HRV were reported, including the low-frequency/high-frequency ratio whose mechanism of action is not well understood (29). To reduce risk of type I statistical error and improve interpretability of results, we respond to these issues by limiting our reporting to vagally-mediated HRV, which has a clear mechanism of action (i.e. parasympathetic down regulation of the heart). We also conduct a comprehensive literature search of RCTs to help synthesize current evidence on the relationship between mindfulness-based-training and potential improvements in HRV.
Methods
Search strategy and selection criteria
The review followed The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (30), and was pre-registered on the PROSPERO database for systematic reviews (# CRD42018108456). Systematic literature searches were conducted using five electronic databases: PsycINFO (Ovid), Embase (Ovid), Medline (Ovid), CINAHL, ERIC and Scopus, covering the period up until December 4th 2019. Broadly, the search aimed to identify studies that simultaneously related to both mindfulness/meditation and HRV.
Search terms relating to mindfulness and meditation were based on those used in an earlier meta-analysis on meditation (31) and included “mindful*”, “meditat*”, “Vipassana”, “Zen”, “Sahaj yoga”, “Dhyan yoga”. We added the terms “body scan”, “breath awareness”, “focused attention”, (“open-monitoring” or “open monitoring”) and “choiceless awareness”, given that these terms are used widely in the meditation literature. Meditation terms were paired with HRV related terms including: “heart rate variability”, “HRV”, “vagal” and “respiratory sinus arrhythmia”. Only peer reviewed journal articles published in English were considered in this review. A sample search strategy can be found in the Appendix A, Supplemental Digital Content. After removing duplicates, search results were then screened manually by two of three reviewers (authors LB, AR and KE) to identify relevant studies that met our inclusion criteria.
Studies were considered eligible for inclusion if they were RCTs of an MBI that delivered instruction for predominantly formal and seated practice in adults (aged 18+) and included outcome data on at least one index of vagally-mediated HRV. Movement-based contemplative practices such as tai chi and yoga were excluded to reduce heterogeneity, and to limit the confounding factor of physical exercise, which is a known predictor of HRV (32). To delineate our findings from brief interventions and induction studies, eligible interventions were required to have a minimum total duration of four hours and include face-to-face contact with an instructor. To reduce the risk of inflating study findings through the inclusion of very small samples (33), studies were required to have a minimum of at least 10 participants allocated to each arm of the study. A comprehensive list of inclusion and exclusion criteria can be found in Appendix B, Supplemental Digital Content.
HRV Measurement
Time domain measures are the simplest measure of vagally-mediated HRV, and of these RMSSD has been recommended for use because it is more independent of respiratory influences on heart rate than other vagally-mediated measures such as RSA (34, 35). For this reason, RMSSD was selected as the preferred HRV metric to include in our analyses where available, or alternatively another time-domain measure such as the standard deviation of NN intervals (SDNN) was used. If a time-domain measure was unavailable, HF-HRV or RSA was used. These vagally-mediated HRV measures are highly correlated and have been directly compared in previous meta-analyses (36-38).
Data extraction
Data on the year and place of publication, population, sample size, HRV outcome measure and intervention characteristics (name, duration, total contact hours, prescription of homework, mode of delivery, instructor qualifications, control type, number of study arms) were extracted by two independent authors (LB and AR) with excellent inter-rater reliability ( κ = .90) and discussed until consensus was achieved.
Risk of Bias
The Cochrane Collaboration Risk of Bias Tool (39) was utilized to identify potential sources of bias in included studies on four domains. These include 1) method of randomization and allocation concealment (the domain of selection bias); 2) blinding of outcome assessment (the domain of detection bias); 3) quantity and management of missing data (the domain of attrition bias); and 4) selective outcome reporting (the domain of reporting bias). Risk of bias was assessed by two independent judges with good inter-rater agreement (κ = .95), and summary scores were visualised using the robvis tool (40).
Statistical analyses
Random effects meta-analyses were conducted using the Metafor package in R, version 3.5.0. A random effects approach was chosen as a conservative alternative to fixed effects modelling. Random effects modelling is appropriate when there is some between-study variation, such as study population (41). Hedges’ g was used as the effect size measure, which is similar to Cohen’s d but has the advantage in correcting for upwards bias. Hedges’ g was computed based on between-group post-intervention differences in HRV, as baseline data was only available for a subgroup (k = 13) of studies on the primary outcome. To test the robustness of the primary result, differences in change scores were also considered. Where studies included two control conditions (e.g. both an active and waitlist control), we used active control data as this represents a more rigorous control. Post-intervention resting state vagally-mediated HRV was the primary outcome measure. Since statistically non-significant effects can be caused by inadequate statistical power to detect a real effect (e.g. type II error), it is important to consider effect size estimates alongside tests of statistical significance (e.g. if the confidence interval captures the null hypothesised value) (42). Thus, in addition to statistical significance determined by the confidence interval, we also consider the effect size of estimates when interpreting results. Hedges’ g values of 0.25, 0.5 and 0.9 were determined to indicate evidence of small, medium and large effects, as recommended for use in HRV research (43).
Between-study heterogeneity was tested using the Q and I2 statistics, and influential cases were determined based on the criteria of Cooks distance being greater than one. Any significant variance was modelled using the a priori determined moderators including intervention-related factors (gold standard versus other interventions and dose), study setting, and control type (active versus passive). Publication bias was examined based on visual examination of funnel plots, as well as significance of the Egger regression and Kendall rank correlation tests.
Results
Our search generated a total of 1045 unique studies. After screening against inclusion criteria, 19 RCTs (combined n analysed = 1465 including 606 allocated to the mindfulness treatment arm) met criteria for inclusion in this review (see figure 1 for a flowchart of included studies).
Figure 1.
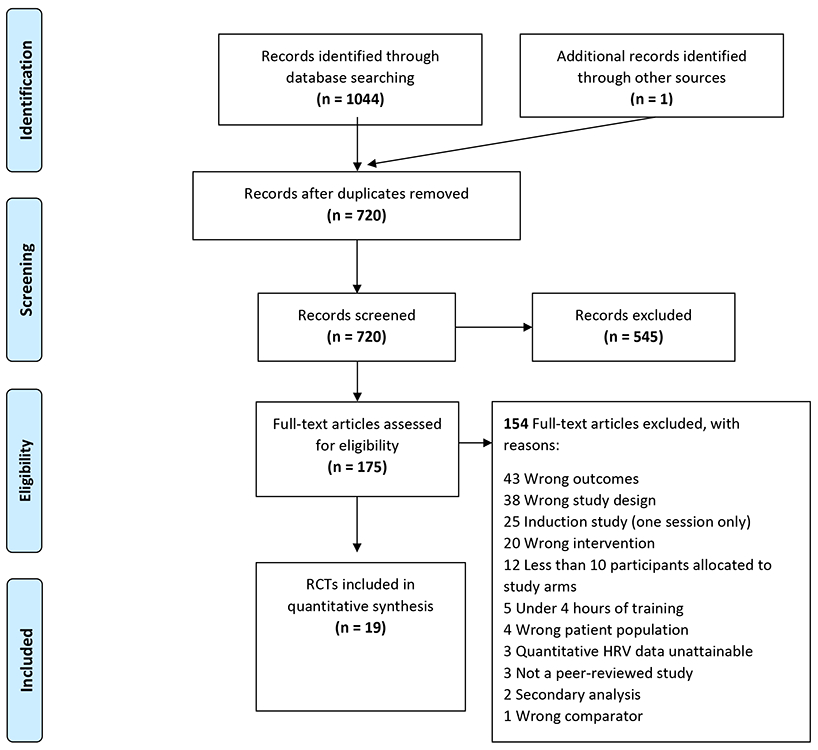
Flow chart of included studies in this meta-analysis
Study Characteristics
Characteristics of included studies are found in Table 1. Five of the included studies employed mindfulness based stress reduction (MBSR), which is a gold standard mindfulness-based intervention (1), and the remaining 14 studies used other meditation-based interventions. Seventeen studies compared the MBI to a control condition (k = 13 passive; k = 4 active). Three studies made comparisons to an active treatment, cognitive behaviour therapy(44-46). Three studies measured HRV using 24-hour Holter recordings (24, 47, 48), and the remaining studies used short-term recordings ranging from 2 – 30 minutes (mean = 7.8 minutes).
Table 1.
Study Characteristics of Randomized Controlled Trials
| Reference | Country | N | Mean Age |
% female |
Population | Intervention | Mode of Delivery |
Total contact hours |
Homework | Instructor Qualifications |
Control type |
Study arms |
HRV measure |
Duration of measurement (mins) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Carroll & Lustyk, 2018) | USA | 34 | 43.4 | 27 | Substance use disorder | MBRP | Group | 16 | Not reported | Experienced health professional | Passive | 3 | RMSDD | 15 |
| (Crosswell et al., 2017) | USA | 71 | 47 | 100 | Breast cancer survivors | MAP | Group | 12 | 17.5 | Mindfulness teacher with >20 years experience | Passive | 2 | RMSSD | 10 |
| (Delgado et al., 2010) | Spain | 36 | Range 18-24 | 100 | College students high in worry | Mindfulness practices | Group | 10 | Encouraged | Health professional with > 10 years experience | Treatment: CBT techniques | 2 | HF-HRV | 5 |
| (Delgado-Pastor et al., 2015) | Spain | 45 | 21.5 | 100 | College students high in worry | Mindfulness interoceptive training | Group | 6 | Encouraged | Not reported | Passive | 3 | RMSSD | 5 |
| (Dunne et al., 2019) | Ireland | 42 | 41 | 74 | Emergency department personnel | ABT | Group | 16 | 32.5 | Not reported | Passive | 2 | RMSSD | 24 hours |
| (Faucher, Koszycki, Bradwejn, Merali, & Bielajew, 2016) | Canada | 38 | 38 | 38.5 | Social anxiety disorder | MBSR | Group | 27.5 | Prescribed | MBSR instructor with > 20 years experience | Treatment: CBT | 2 | HF-HRV | 30 |
| (Grossman et al., 2017) | Switzerland | 168 | 52.5 | 100 | Fibromyalgia | MBSR | Group | 27 | 42 | MBSR instructors with > 7 years experience | Active and Passive | 3 | RSA | 24 hours |
| (Hunt, Al-Braiki, Dailey, Russell, & Simon, 2018) | USA | 119 | 19.3 | 74 | College students | MBI | Group | 4 | Encouraged | Not reported | Active and Passive | 5 | SDNN | 5 |
| (Kok et al, 2013) | USA | 71 | 37.5 (median) | 66 | University staff | LKM | Group | 6 | Encouraged | Experienced health professional | Passive | 2 | HF-HRV | 2 |
| (Krick & Felfe, 2019) | Germany | 267 | 26.0 | 21.3 | Police officers | MBI | Group | 12 | Prescribed | Experienced instructor | Passive | 2 | RMSSD | 5 |
| (Muthukrishnan, Jain, Kohli, & Batra, 2016) | India | 74 | 22 | 100 | Pregnant women | MBI | Unclear | 10 | 17.5 | Not reported | Passive | 2 | Unclear | unclear |
| (Nyklicek et al., 2013) | Netherlands | 88 | 46.1 | 71 | Stressed community sample | MBSR | Group | 20 | 42 | MBSR instructor with 1 year experience | Passive | 2 | RMSSD | 5 |
| (Oken et al., 2017) | USA | 128 | 59.8 | 80 | Stressed adults age 50+ | MBI | Individual | 7.5 | Encouraged | Experienced instructor | Passive | 2 | SDRR | 5 |
| (Owens et al., 2016) | USA | 19 | 49.4 | 89 | Those with benign heart palpitations | MBSR | Group | 27 | 42 | Not reported | Passive | 2 | RMSSD | 24 hours |
| (Price et al., 2019) | USA | 217 | 35 | 100 | Substance use disorder | MABT | Individual | 12 | Encouraged | Not reported | Active and Passive | 3 | RSA | 5 |
| (Sekar et al., 2019) | India | 30 | 28.5 | 100 | Nurses with perceived stress | Mahamantra Chanting | Individual | 15 | Not clear | Research assistant | Passive | 2 | SDNN | 5 |
| (Wahbeh, Goodrich, Goy, & Oken, 2016) | USA | 114 | 52.1 | 6 | Combat Veterans | Mindful body-scan | Individual | 2 | 14 | Trained research assistant | Passive | 4 | Unclear | 5 |
| (Wolever et al., 2012) | USA | 239 | 42.9 | 77 | Insurance employees | Mindfulness at Work | Group* | 14 | Encouraged | Experienced instructor | Passive | 3 | RR Intervals | 10 |
| (Zimmermann-Schlegel et al., 2018) | Germany | 110 | 58.8 | 22.1 | Type 2 Diabetes Patients | MBSR - modified | Group | 20 | Encouraged | Health professionals | Passive | 2 | RMSSD | 5 |
ABT: Attention Based Training. CEB: Cultivating Emotional Balance. H: High. HRV: Heart Rate Variability. L: Low. LKM: Loving Kindness Meditation. M: Medium. MABT: Mindful Awareness in Body Oriented Therapy. MAP: Mindful Awareness Practices. MBRP: Mindfulness Based Relapse Prevention. MBSR: Mindfulness Based Stress Reduction. MORE: Mindfulness Oriented Recovery Enhancement. MRBWT. Mindfulness and Resource Based Worksite Training. TM Transcendental Meditation.
Group was delivered in either a conventional classroom or virtual classroom allowing for real-time bi-directional communication with no significant differences in effect sizes across modalities. Note. N represents the total study sample size of those randomized to a condition. Mean age and proportion female are calculated based on the total sample size.
The total duration of interventions ranged from 4 to 28 hours, with a mean of 14 hours. Additionally, seventeen of the nineteen studies encouraged or assigned home mindfulness practice between sessions. About half of the included studies (k = 9) were conducted in the United States. Study samples were diverse including medical (k = 5) mental health (k = 4) and community (k = 10) settings.
Resting State HRV
Sixteen RCTs compared MBI treatment to a control condition and used resting state HRV as an outcome measure. Twelve of these studies used passive control conditions and the remaining four used an active control. There was a non-significant difference in resting state HRV between meditation and control groups, g = 0.38, 95% confidence interval (CI) = −0.014 to 0.77, p = .059 (see figure 2 for the forest plot). This small to medium sized non-significant effect favored the MBI condition. This result was close to significance. Thus, to test the robustness of this result, we also considered meta-analyses using i) group differences in pre-post change scores and ii) pre-post difference in HRV in the treatment group alone. For the group differences in pre-post change analysis, a subgroup of studies (k = 13) were included that had both pre and post intervention data on resting-state HRV. Echoing findings from our primary analysis, this effect was non-significant with evidence of a small to medium effect size, g = 0.29, 95% CI = −0.19 to 0.76. For the less-rigorous analysis of pre-post change in the intervention arm alone (excluding data from the control condition), there was evidence of a significant small-medium increase in HRV post MBI intervention relative to baseline, g = 0.33, 95% CI = 0.11 to 0.55.
Figure 2.
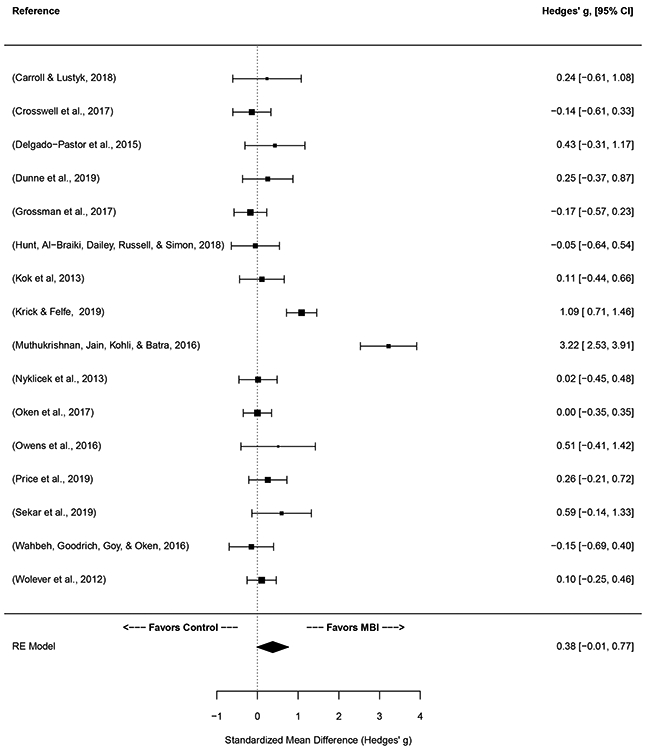
Forest plot of post-intervention group differences in resting-state HRV between intervention and control conditions.
There was a high degree of inter-study heterogeneity in results of the primary analysis Q (15) = 105.39, p < 0.001, with I2 indicating that 89.12% of observed variance being attributable to study heterogeneity. While all Cook’s d values were less than 1 indicating no influential cases, the study by Muthukrishnan and colleagues (2016) had a standardized difference of beta value of 1.91, indicating that the pooled effect shifts by 1.91 standard deviation units when the study is removed from the model. When the effect associated with this study was removed, the pooled main effect was smaller and remained non-significant (g = 0.19, 95% CI = −0.02 to 0.39). Heterogeneity was attenuated but remained significant (Q (14) = 33.63, p = 0.002, I2 = 56.15%).
Four studies reported on resting HRV at follow-up (mean follow-up = 23.5 weeks). There was no difference in HRV between treatment and control groups at follow-up (g = − 0.18, 95% CI = − 0.62 to 0.26; see forest plot, Figure S1, Supplemental Digital Content.
Mindfulness versus cognitive behavior therapy (CBT)
Three studies compared MBIs to CBT. In this subset of studies, no post-intervention group differences in resting-state HRV were observed, g = 0.44, 95% CI = −0.23 to 1.10. The non-significant difference favored MBI treatment, indicating a potential small to medium effect favoring MBIs over CBT. There was no evidence of heterogeneity in results Q (2) = 4.46, p = 0.11, I2 = 55.32%.
Do results vary as a function of intervention related factors?
We considered whether results from studies of the gold standard MBSR intervention (k = 5) differed from studies of non-gold-standard interventions on the primary outcome. Overall, intervention type (MBSR versus other) was not a significant moderator of results QM (2) = 3.93, p = 0.14. In a subgroup analysis, non-gold standard interventions were associated with significantly higher resting-state HRV post-intervention g = .44, 95% CI = .003 to .88. In contrast, the effect was not significant for MBSR interventions, g = 0.09, 95% CI = −0.084 to 1.01.
We also considered if dose was associated with between-study heterogeneity in results. We found that intervention duration was not a significant moderator of results, QM (1) = 0.041, p = 0.84. Longer interventions did not lead to greater improvements in HRV relative to shorter interventions.
Do results vary across study settings?
Study setting (medical, mental health, community) was also a non-significant moderator of results, QM (df = 3) = 4.93, p = 0.18. The non-significant trend favored studies conducted in a medical setting. These studies exhibited a large but non-significant pooled effect, g = 0.81, 95% CI = −0.005 to 1.62. It should be noted that the effect within medical settings included the outlier study by Muthukrishnan and colleagues, that individually reported a very large effect of the intervention on resting state HRV of g = 3.22 (49). When removed, the non-significant effect within medical setting studies was no longer present g = − 0.037, 95% CI = −0.49 to 0.42.
Do results vary between studies with active versus passive control conditions?
Control type (active versus passive) was not a significant moderator of results, QM (2) = 5.16, p = 0.076. The non-significant trend favored studies with a passive control condition. In a subgroup analysis, our primary outcome reached significance among studies with a passive control condition g = 0.52, 95% CI = .07 to .96. There was no effect among studies with an active control g = − 0.03, 95% CI = −.78 to .73.
Risk of bias
Seven studies were assessed as having low risk of bias, scoring low risk on at least four of six domains of study bias (24, 48, 50-54). Six studies were assessed as having high risk of bias, with at least one domain rated at high risk (44, 46, 47, 55-57). Most studies were rated high risk due to having high levels of missing data (more than 20% missing or between 5-20% missing but with no clear indication of appropriate handling of missing data). The remaining six studies were assessed as having unclear risk of bias, with fewer than four domains being rated as low risk, and the remaining domains rated as unclear (22, 45, 49, 58-60). A traffic light plot of assessments is found in Figure S2, Supplemental Digital Content.
A moderator analysis comparing studies at low risk of bias to those of unclear or high risk of bias was significant QM (2) = 6.41, p = 0.041. Studies rated low risk of bias reported no significant post-intervention group differences in resting state HRV g = 0.044, 95% CI = −0.51 to 0.60. The effect was significant, however, for studies rated unclear or high risk of bias, with evidence of a medium to large effect g = 0.64, 95% CI 0.14 to 1.14.
While considering the potential role of duration of HRV measurement was not an a priori determined moderator, we also considered if the primary result varied as a function of HRV duration given that recording duration is a relevant variable that can influence HRV measures (35). Three studies used 24 hour Holter monitor recordings (24, 47, 48) and the remaining studies used short-term recordings with a mean recording duration of 7.8 minutes.., This effect was not significant QM (2) = 3.63 p = 0.16.
Publication bias
The funnel plot (see figure 3) shows asymmetrical bias, as there was an absence of studies to the middle right of the funnel. Bias was also indicated by a significant rank correlation test τ = 0.43, p = .02, but not by an eggers regression which was non-significant, Z = 1.12, p = .26. The trim and fill test estimated zero studies missing on the left side of the funnel and six studies missing on the right side (favoring MBIs). Thus, there is no evidence of publication bias in the expected direction (i.e. non-publication of non-significant findings) (61). A Funnel plot for the follow-up timepoint is found in Figure S3, Supplemental Digital Content.
Figure 3.
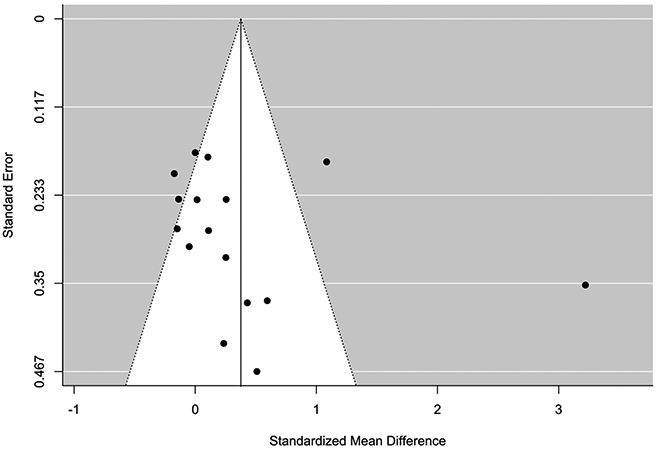
Funnel plot for meta-analysis of post-intervention group differences in the primary outcome, resting-state HRV.
Discussion
This is the first comprehensive meta-analysis to examine the effects of mindfulness-based training on HRV relative to a control or active treatment comparison. Our primary analysis found that MBI training was not significantly related to higher resting-state vagally-mediated HRV relative to control conditions at either post-intervention or follow-up. Our primary analysis was robust to meta-analytic method, as it was replicated when considering group differences in change scores, an approach which is more likely to detect a significant effect (62). However, despite the absence of a statistically significant overall result, results were nearing significance and we found evidence of small-medium sized non-significant effects in resting-state HRV which is noteworthy (42). The effect is, however, diminished considerably when a single study that shows evidence of effect size inflation is removed. Taken together, these results suggest a small, but potentially meaningful effect that warrants further investigation.
A recent scoping review has identified HRV as a potentially useful biomarker, capable of demonstrating MBI effects (26) but the authors failed to quantitatively synthesize study results and they included uncontrolled studies in their review which are lower quality and more prone to bias (28). Here, we address these limitations by examining objective evidence from RCTs linking MBI training with changes in HRV. Overall, we found little evidence of improved resting-state vagally-mediated HRV following mindfulness training.
Our primary outcome of group differences in resting-state HRV was approaching significance (p = .059), and was associated with small-medium effect favoring the intervention group (g = 0.38) so it is important to consider the robustness of this result. Firstly, we found evidence of high levels of between-study heterogeneity (I2 = 89.12%). Thus, it is plausible that differences in study design could explain why a subgroup of included studies might exert salutary effects on HRV whereas others might not (1). If there was a real effect of mindfulness on HRV, we might expect to see evidence that more rigorous interventions – such as the gold standard MBSR program – were more efficacious in increasing HRV than shorter and less regulated interventions. However, intervention type (MBSR versus other) was a non-significant moderator of the resting-state HRV. Moreover, when investigating the subgroups separately, other interventions (g = .44) but not MBSR (g = .09) were associated with significantly higher HRV post-intervention. Similarly, there was no evidence of a dose response, meaning that longer interventions were no more likely to lead to improvements in HRV than shorter interventions. Taken together, our findings show that gold standard and more intensive MBIs are no more likely to lead to improvements in HRV than shorter and less intensive interventions. This evidence points to the fact that our non-significant main finding cannot be explained by the inclusion of brief or non-gold standard interventions. On the contrary, the gold standard MBSR program was associated with a trivial effect size, as well as a non-significant result.
A second way to investigate the robustness of our finding is to consider alternate methods of conducting the meta-analysis. Thirteen studies had data on pre- and post-intervention resting state HRV, enabling us to conduct a meta-analysis of change scores in this subgroup. Change score meta-analyses may be more likely to detect significant effects than analyses based on study arm group differences alone (62). However, our analysis of change scores echoed our main result; there was no difference in pre-post resting HRV change scores in MBI versus control conditions, although the small to medium effect size (albeit non-significant) was replicated (g = 0.29). It is important to note that when we removed control data and considered pre-post change in the intervention group alone, there was evidence of a significant effect (g = .33). This finding agrees with prior systematic reviews investigating associations between meditation and HRV which have reported on evidence of significant effects (26, 63). Both of these review papers included one-arm trials in their descriptive summaries, and no quantitative synthesis was conducted. This indicates that any improvement in HRV observed in one-arm trials of MBIs may be due to common factors that are not specific to meditation (64). Non-randomized studies cannot add to our current knowledge of the efficacy of MBIs in improving HRV, and only large well-designed RCTs will be helpful in adding to the evidence at this stage (1, 65).
A third consideration of the robustness of our results is to look at the pooled effect when outliers and/or influential cases are removed from the model. As visualized in the forest plot (figure 2), we found evidence that the effect reported by Muthukrishnan and colleagues (49) was significant and substantially higher than other studies (g = 3.22). It is unclear why this intervention differed from the others and exerted a very large effect on resting HRV. When this study was removed from analysis, the pooled effect was attenuated (g = .19) and remained non-significant.
We cannot definitively determine if our non-significant result is primarily due to limited data, methodological differences between studies, or a combination of the two. However, we recommend interpreting the non-significant overall effect size (g = 0.38) with caution because this effect was not observed in studies using the gold-standard MBSR intervention (g = 0.11), and it was not observed in studies rated as having a low risk of bias, assessed using the Cochrane collaboration tool (g = 0.044). Additionally, studies with a higher risk of bias tended to report larger effect sizes (g = 0.64). Nonetheless, it is important to acknowledge that group differences did (non-significantly) favor the MBI intervention over control conditions post-intervention, but not at follow-up. Therefore, it is possible that MBIs might contribute to short-term improvements in HRV in some instances, but more research would be needed to understand this issue, and specifically when and for whom MBIs might exert salutatory benefits on HRV.
While we limited our analyses to vagally-mediated metrics of HRV including RMSSD, other time-domain measures, as well as HF-HRV and RSA, it is important to note that these measures, while highly inter-correlated, are not synonymous with vagal tone. Numerous factors can confound the association between these measures and underlying vagal tone, including interindividual differences, physical activity and, importantly, respiration (16). A key caveat in the methodological design of the included studies that only three of the 19 studies (>16%) controlled for respiration rate (24, 44, 55). While we mitigated this issue through adopting RMSSD as the primary HRV metric used when available, which is less affected by respiration than other measures such as RSA, RMSSD is nonetheless influenced by respiration (35). This is problematic, as respiration rate changes can influence HRV metrics without affecting vagal tone (35). We excluded studies of paced or controlled breathing interventions for this reason, however it is possible that mindfulness-based practices with natural breathing may nonetheless lead to changes in respiration rate that could subsequently influence HRV, independent of any underlying changes in vagal tone and associated influence of the parasympathetic nervous system. Thus, we recommend that future studies control for respiration rate, in accordance with current recommendations (66). The predictive value of HRV may be improved when controlling for respiration, so it is possible that this methodological consideration could help identify any true effect of MBIs on HRV (67).
While we found no evidence of a dose-response, it should be noted that this review of RCTs does not include coverage of expert or longer-term meditators, a group wherein physiological changes associated with mindfulness might be more pronounced. It is difficult to conduct RCTs investigating very high doses of mindfulness, due to time and resource limitations, and non-randomized studies of expert meditators run the risk of confounding factors influencing results (68). Nonetheless, group comparison studies (controlling for differences in demographics and other factors known to influence HRV) of HRV indices in expert versus novice meditators could be helpful to shed light on this question, and help ascertain the extent to which mindfulness might influence HRV at very high doses, and thus help determine if a true effect of mindfulness on HRV exists, while acknowledging that there are some lifestyle factors that may be incredibly difficult to control (68).
The American Heart Association has recently recommended meditation as an adjunct treatment to reduce cardiovascular risk (69). HRV is an index of cardiac health, so it is important to consider the extent to which it might specifically be improved through meditation training. The results of this meta-analysis show that there is currently insufficient evidence to indicate that meditation improves HRV, and further research is needed. In contrast, there is stronger evidence that physical interventions such as exercise (32) and mindful movement-based practices such as tai chi and yoga (70) lead to salutary HRV changes. Therefore, physical activity-based interventions may offer a more plausible pathway to improved HRV than seated meditation practice.
To our knowledge, only one prior study has conducted a meta-analysis of MBIs and HRV, and it included data from only four studies (27). In this small earlier synthesis, authors found no evidence that MBIs were associated with improvements in resting state HRV relative to control conditions. We expand on this finding to include a larger sample of studies . In agreement with Radmark and colleagues (27), we also found insufficient evidence that meditation training is associated with higher resting-state HRV relative to control conditions. HRV may not be a key mechanism that helps explain the wide-ranging health benefits of meditation practice, and so future small trials of MBIs should not prioritize including HRV as an outcome measure. Only large, well-designed RCTs of high quality MBIs (e.g. gold standard or other rigorously developed interventions) designed with low risk of methodological bias could help add to the current evidence to elucidate any role MBIs might play in improving HRV.
Supplementary Material
Acknowledgments
Conflicts of Interest and Source of Funding: This study was supported by La Trobe University and Healthscope Hospitals, with grants awarded to Prof. Morris. Time for analysis and article preparation was also funded by the National Heart, Lung, and Blood Institute through grant R01HL113272 (to Dr. Huffman) and K23HL123607 (to Dr. Celano). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health. Dr. Celano has received honoraria for talks to Sunovion Pharmaceuticals on topics unrelated to this research. The authors report no other conflicts of interest.
The authors thank Xi Wang (University of Melbourne) for her role as an assessor of risk of bias in included studies.
Glossary
- HRV
heart rate variability
- HF-HRV
high-frequency heart rate variability
- MBI
mindfulness based intervention
- RSA
respiratory sinus arrhythmia
Footnotes
Statement of Ethics: The authors have no ethical conflicts to disclose
References
- 1.Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, Meissner T, Lazar SW, Kerr CE, Gorchov J. Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on psychological science. 2018;13:36–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Creswell J Biological pathways linking mindfulness with health. 2015. [Google Scholar]
- 3.Vago DR, David SA. Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in human neuroscience. 2012;6:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wielgosz J, Goldberg SB, Kral TR, Dunne JD, Davidson RJ. Mindfulness meditation and psychopathology. Annual review of clinical psychology. 2019;15:285–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindsay EK, Creswell JD. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review. 2017;51:48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: Systematic review and meta-analysis. Journal of psychiatric research. 2017;95:156–78. [DOI] [PubMed] [Google Scholar]
- 7.Rubia K The neurobiology of meditation and its clinical effectiveness in psychiatric disorders. Biological psychology. 2009;82:1–11. [DOI] [PubMed] [Google Scholar]
- 8.Goedhart AD, Van der Sluis S, Houtveen JH, Willemsen G, De Geus EJ. Comparison of time and frequency domain measures of RSA in ambulatory recordings. Psychophysiology. 2007;44:203–15. [DOI] [PubMed] [Google Scholar]
- 9.Appelhans BM, Luecken LJ. Heart rate variability as an index of regulated emotional responding. Review of general psychology. 2006;10:229. [Google Scholar]
- 10.Huikuri HV, Raatikainen MP, Moerch-Joergensen R, Hartikainen J, Virtanen V, Boland J, Anttonen O, Hoest N, Boersma LV, Platou ES. Prediction of fatal or near-fatal cardiac arrhythmia events in patients with depressed left ventricular function after an acute myocardial infarction. European heart journal. 2009;30:689–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liao D, Carnethon M, Evans GW, Cascio WE, Heiss G. Lower heart rate variability is associated with the development of coronary heart disease in individuals with diabetes: the atherosclerosis risk in communities (ARIC) study. Diabetes. 2002;51:3524–31. [DOI] [PubMed] [Google Scholar]
- 12.Tsuji H, Larson MG, Venditti FJ, Manders ES, Evans JC, Feldman CL, Levy D. Impact of reduced heart rate variability on risk for cardiac events: the Framingham Heart Study. Circulation. 1996;94:2850–5. [DOI] [PubMed] [Google Scholar]
- 13.Tsuji H, Venditti FJ, Manders ES, Evans JC, Larson MG, Feldman CL, Levy D. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation. 1994;90:878–83. [DOI] [PubMed] [Google Scholar]
- 14.Frewen J, Finucane C, Savva GM, Boyle G, Coen RF, Kenny RA. Cognitive function is associated with impaired heart rate variability in ageing adults: the Irish longitudinal study on ageing wave one results. Clinical Autonomic Research. 2013;23:313–23. [DOI] [PubMed] [Google Scholar]
- 15.Beauchaine TP, Thayer JF. Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology. 2015;98:338–50. [DOI] [PubMed] [Google Scholar]
- 16.Grossman P, Taylor EW. Toward understanding respiratory sinus arrhythmia: relations to cardiac vagal tone, evolution and biobehavioral functions. Biological psychology. 2007;74:263–85. [DOI] [PubMed] [Google Scholar]
- 17.Kemp AH, Quintana DS. The relationship between mental and physical health: insights from the study of heart rate variability. International Journal of Psychophysiology. 2013;89:288–96. [DOI] [PubMed] [Google Scholar]
- 18.Eberth J, Sedlmeier P. The effects of mindfulness meditation: a meta-analysis. Mindfulness. 2012;3:174–89. [Google Scholar]
- 19.Roemer L, Williston SK, Rollins LG. Mindfulness and emotion regulation. Current Opinion in Psychology. 2015;3:52–7. [Google Scholar]
- 20.Farb NA, Anderson AK, Segal ZV. The mindful brain and emotion regulation in mood disorders. The Canadian Journal of Psychiatry. 2012;57:70–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farb NA, Anderson AK, Mayberg H, Bean J, McKeon D, Segal ZV. Minding one’s emotions: mindfulness training alters the neural expression of sadness. Emotion. 2010;10:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kok BE, Coffey KA, Cohn MA, Catalino LI, Vacharkulksemsuk T, Algoe SB, Brantley M, Fredrickson BL. How positive emotions build physical health: Perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychological science. 2013;24:1123–32. [DOI] [PubMed] [Google Scholar]
- 23.Nijjar PS, Puppala VK, Dickinson O, Duval S, Duprez D, Kreitzer MJ, Benditt DG. Modulation of the autonomic nervous system assessed through heart rate variability by a mindfulness based stress reduction program. International journal of cardiology. 2014;177:557–9. [DOI] [PubMed] [Google Scholar]
- 24.Grossman P, Deuring G, Walach H, Schwarzer B, Schmidt S. Mindfulness-Based Intervention Does Not Influence Cardiac Autonomic Control or the Pattern of Physical Activity in Fibromyalgia During Daily Life. The Clinical journal of pain. 2017;33:385–94. [DOI] [PubMed] [Google Scholar]
- 25.Lumma A-L, Kok BE, Singer T. Is meditation always relaxing? Investigating heart rate, heart rate variability, experienced effort and likeability during training of three types of meditation. International Journal of Psychophysiology. 2015;97:38–45. [DOI] [PubMed] [Google Scholar]
- 26.Christodoulou G, Salami N, Black DS. The Utility of Heart Rate Variability in Mindfulness Research. Mindfulness. In Press:1–17. [Google Scholar]
- 27.Rådmark L, Sidorchuk A, Osika W, Niemi M. A Systematic Review and Meta-Analysis of the Impact of Mindfulness Based Interventions on Heart Rate Variability and Inflammatory Markers. Journal of clinical medicine. 2019;8:1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reeves BC, Deeks JJ, Higgins J. 13 Including non-randomized studies. Cochrane handbook for systematic reviews of interventions. 2008;1:391. [Google Scholar]
- 29.Quintana D, Alvares GA, Heathers J. Guidelines for Reporting Articles on Psychiatry and Heart rate variability (GRAPH): recommendations to advance research communication. Translational psychiatry. 2016;6:e803–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151:264–9. [DOI] [PubMed] [Google Scholar]
- 31.Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z, Sleicher D, Maron DD, Shihab HM. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA internal medicine. 2014;174:357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sandercock G, Bromley PD, Brodie DA. Effects of exercise on heart rate variability: inferences from meta-analysis. 2005. [DOI] [PubMed] [Google Scholar]
- 33.Button KS, Ioannidis JP, Mokrysz C, Nosek BA, Flint J, Robinson ES, Munafò MR. Power failure: why small sample size undermines the reliability of neuroscience. Nature Reviews Neuroscience. 2013;14:365. [DOI] [PubMed] [Google Scholar]
- 34.Kleiger RE, Stein PK, Bigger JT Jr. Heart rate variability: measurement and clinical utility. Annals of Noninvasive Electrocardiology. 2005;10:88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shaffer F, Ginsberg J. An overview of heart rate variability metrics and norms. Frontiers in public health. 2017;5:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown L, Karmakar C, Gray R, Jindal R, Lim T, Bryant C. Heart rate variability alterations in late life depression: a meta-analysis. Journal of affective disorders. 2018;235:456–66. [DOI] [PubMed] [Google Scholar]
- 37.Shahrestani S, Stewart EM, Quintana DS, Hickie IB, Guastella AJ. Heart rate variability during adolescent and adult social interactions: A meta-analysis. Biological Psychology. 2015;105:43–50. [DOI] [PubMed] [Google Scholar]
- 38.Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Frontiers in psychiatry. 2014;5:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McGuinness LA. robvis: An R package and web application for visualising risk-of-bias assessments. 2019. [DOI] [PubMed] [Google Scholar]
- 41.Hedges LV, Vevea JL. Fixed-and random-effects models in meta-analysis. Psychological methods. 1998;3:486. [Google Scholar]
- 42.Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature Publishing Group; 2019. [DOI] [PubMed] [Google Scholar]
- 43.Quintana D Statistical considerations for reporting and planning heart rate variability case-control studies. Psychophysiology. 2017;54:344–9. [DOI] [PubMed] [Google Scholar]
- 44.Carroll H, Lustyk MKB. Mindfulness-based relapse prevention for substance use disorders: effects on cardiac vagal control and craving under stress. Mindfulness. 2018;9:488–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Delgado LC, Guerra P, Perakakis P, Vera MN, del Paso GR, Vila J. Treating chronic worry: Psychological and physiological effects of a training programme based on mindfulness. Behaviour research and therapy. 2010;48:873–82. [DOI] [PubMed] [Google Scholar]
- 46.Faucher J, Koszycki D, Bradwejn J, Merali Z, Bielajew C. Effects of CBT versus MBSR treatment on social stress reactions in social anxiety disorder. Mindfulness. 2016;7:514–26. [Google Scholar]
- 47.Dunne PJ, Lynch J, Prihodova L, O'Leary C, Ghoreyshi A, Basdeo SA, Cox DJ, Breen R, Sheikhi A, Carroll Á. Burnout in the emergency department: randomized controlled trial of an attention-based training program. Journal of integrative medicine. 2019;17:173–80. [DOI] [PubMed] [Google Scholar]
- 48.Owens JE, Schorling J, Plews-Ogan M, Goodman M, Moorman R, Zaklin R, Dent J. A randomized controlled trial evaluating Mindfulness-Based Stress Reduction (MBSR) for the treatment of palpitations: A pilot study. International journal of cardiology. 2016;223:25–7. [DOI] [PubMed] [Google Scholar]
- 49.Muthukrishnan S, Jain R, Kohli S, Batra S. Effect of mindfulness meditation on perceived stress scores and autonomic function tests of pregnant Indian women. Journal of clinical and diagnostic research: JCDR. 2016;10:CC05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crosswell AD, Moreno PI, Raposa EB, Motivala SJ, Stanton AL, Ganz PA, Bower JE. Effects of mindfulness training on emotional and physiologic recovery from induced negative affect. Psychoneuroendocrinology. 2017;86:78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hunt M, Al-Braiki F, Dailey S, Russell R, Simon K. Mindfulness training, yoga, or both? Dismantling the active components of a mindfulness-based stress reduction intervention. Mindfulness. 2018;9:512–20. [Google Scholar]
- 52.Nyklíček I, Mommersteeg P, Van Beugen S, Ramakers C, Van Boxtel GJ. Mindfulness-based stress reduction and physiological activity during acute stress: A randomized controlled trial. Health Psychology. 2013;32:1110. [DOI] [PubMed] [Google Scholar]
- 53.Oken BS, Wahbeh H, Goodrich E, Klee D, Memmott T, Miller M, Fu R. Meditation in stressed older adults: improvements in self-rated mental health not paralleled by improvements in cognitive function or physiological measures. Mindfulness. 2017;8:627–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Price CJ, Thompson EA, Crowell S, Pike K. Longitudinal effects of interoceptive awareness training through mindful awareness in body-oriented therapy (MABT) as an adjunct to women’s substance use disorder treatment: A randomized controlled trial. Drug and alcohol dependence. 2019;198:140–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zimmermann-Schlegel V, Wild B, Nawroth P, Kopf S, Herzog W, Hartmann M. Impact of depression and psychosocial treatment on heart rate variability in patients with type 2 diabetes mellitus: an exploratory analysis based on the HEIDIS trial. Experimental and Clinical Endocrinology & Diabetes. 2019;127:367–76. [DOI] [PubMed] [Google Scholar]
- 56.Krick A, Felfe J. Who benefits from mindfulness? The moderating role of personality and social norms for the effectiveness on psychological and physiological outcomes among police officers. Journal of occupational health psychology. 2019. [DOI] [PubMed] [Google Scholar]
- 57.Sekar L, Niva W, Maheshkumar K, Thangavel G, Manikandan A, Silambanan S, Shriraam V, Ramaswamy P. Effect of Mahamantra Chanting on Autonomic and Cognitive Functions-An Interventional Study. Journal of Clinical & Diagnostic Research. 2019;13. [Google Scholar]
- 58.Delgado-Pastor LC, Ciria LF, Blanca B, Mata JL, Vera MN, Vila J. Dissociation between the cognitive and interoceptive components of mindfulness in the treatment of chronic worry. Journal of behavior therapy and experimental psychiatry. 2015;48:192–9. [DOI] [PubMed] [Google Scholar]
- 59.Wahbeh H, Goodrich E, Goy E, Oken BS. Mechanistic pathways of mindfulness meditation in combat veterans with posttraumatic stress disorder. Journal of clinical psychology. 2016;72:365–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA, Baime M. Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. Journal of occupational health psychology. 2012;17:246. [DOI] [PubMed] [Google Scholar]
- 61.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, Harbord RM, Schmid CH. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. Bmj. 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
- 62.Fu R, Holmer HK. Change score or followup score? An empirical evaluation of the impact of choice of mean difference estimates. 2015. [PubMed] [Google Scholar]
- 63.Tung Y-H, Hsieh J-C. The Impacts of Mindfulness on Heart Rate Variability: A Brief Review. 2019. [Google Scholar]
- 64.Wampold BE, Imel ZE. The great psychotherapy debate: The evidence for what makes psychotherapy work: Routledge; 2015. [Google Scholar]
- 65.Dimidjian S, Segal ZV. Prospects for a clinical science of mindfulness-based intervention. American Psychologist. 2015;70:593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research–recommendations for experiment planning, data analysis, and data reporting. Frontiers in psychology. 2017;8:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wilhelm FH, Grossman P, Coyle MA. Improving estimation of cardiac vagal tone during spontaneous breathing using a paced breathing calibration. Biomedical Sciences Instrumentation. 2004;40:317–24. [PubMed] [Google Scholar]
- 68.Davidson RJ, Kaszniak AW. Conceptual and methodological issues in research on mindfulness and meditation. American Psychologist. 2015;70:581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Levine GN, Lange RA, Bairey-Merz CN, Davidson RJ, Jamerson K, Mehta PK, Michos ED, Norris K, Ray IB, Saban KL. Meditation and cardiovascular risk reduction: a scientific statement from the American Heart Association. Journal of the American Heart Association. 2017;6:e002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zou L, Sasaki JE, Wei G-X, Huang T, Yeung AS, Neto OB, Chen KW, Hui SS-c. Effects of mind–body exercises (Tai Chi/Yoga) on heart rate variability parameters and perceived stress: A systematic review with meta-analysis of randomized controlled trials. Journal of clinical medicine. 2018;7:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


