Abstract
Purpose:
Despite the known benefits of cardiac rehabilitation (CR), it remains underutilized particularly among women. The aim of this review was to provide an overview regarding women in CR, addressing barriers which may affect enrollment and attendance as well as to discuss the training response and methods to optimize exercise-related benefits of CR.
Review Methods:
The review examines original studies and meta-analyses regarding women in CR.
Summary:
Women are less likely to engage in CR compared to men and this may be attributed to lack of referral or psychosocial barriers on the part of the patient. Furthermore, despite having lower levels of fitness, women do not improve their fitness as much as men in CR. This review summarizes the current literature and provides recommendations for providers regarding participation and adherence as well as optimal methods for exercise training for women in CR.
Keywords: Cardiac Rehabilitation, Secondary prevention
Condensed Abstract:
This review summarizes the current literature pertaining to women in cardiac rehabilitation (CR) with particular attention to participation rates and exercise training response. Specific interventions can help with enrollment and adherence. Additionally, the exercise prescription for women in CR can be designed to optimize the benefits of CR.
Cardiovascular disease (CVD) is the leading cause of death in the United States for women, killing roughly 300,000 women a year.1 While medical advances have improved overall survival rates in patients with CVD, a sex-related gap exists regarding recovery from an acute cardiac event. Independent of age, within 5 yr of experiencing a myocardial infarction (MI), women are more likely to die, have congestive heart failure or suffer a stroke compared to men.2
Phase 2 cardiac rehabilitation (CR) plays a key role in prevention for cardiac patients and has also been shown to reduce mortality and morbidity and improve quality of life, exercise capacity, and physical function.3–6 Although the benefits of CR have been clearly established, it is remarkably underutilized, particularly among women.7,8 The purpose of this review is to provide an overview regarding women in CR, addressing barriers which may impact enrollment and adherence as well as to discuss the exercise training response compared with men and methods to optimize the beneficial effects of CR.
CARDIOVASCULAR DISEASE IN WOMEN
Although traditional CVD risk factors are the same for both men and women, there are differences regarding the prevalence of these risk factors.9 Hypertension is higher in women >65 yr of age compared to men.10 Similarly, type 2 diabetes mellitus and elevated cholesterol are more prevalent in adult women than men, particularly among non-Hispanic black and Mexican American women.11,12 Additionally, new studies have identified female-specific CVD risk factors, including history of preterm delivery, gestational diabetes or hypertension, surgical or early menopause, autoimmune disease and cancer treatment (such as breast cancer) 13 (Figure 1).
Figure 1:
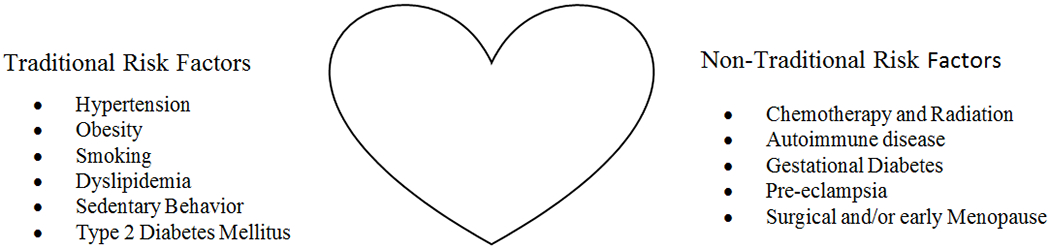
Cardiovascular risk factors in Women
While women develop ischemic heart disease at a later age compared to men, rates of ischemic heart disease have been escalating among younger women.14 One in five women will die from heart disease yet only 56% of women recognize that CVD is the number one cause of death in women. 1 Furthermore, women are less likely than men to receive preventive treatment or guidance.13,15
CR REFERRAL, ENROLLMENT AND ADHERENCE IN WOMEN
CR is a cost effective class 1A recommendation of the American Heart Association and American College of Cardiology for risk reduction, yet women are less likely to enroll and complete CR compared to men.16,17 National surveys of Medicare enrollees have shown that following an MI, women participated at a rate of 14.3% compared to 22.1% in men.7 Additionally, women have lower CR referral rates which impacts CR participation.8 This lower referral rate may be due, in part, to physician bias since, on average, women are older and have more medical and psychological co-morbidities than men following a cardiac event. 18 Paradoxically, however, it is these challenges that make participation in CR all the more necessary and potentially beneficial.
In a meta-analysis of 297,719 individuals with a CR eligible diagnosis, a 36% lower enrollment rate was observed in women compared to men.19 Previous studies have identified low educational attainment, social isolation, lack of insurance, transportation issues and mental health as potential determinants of CR participation.8,20–22 A recent study by Khadanga et al examined the medical, psychosocial, and behavioral factors which influence CR participation among both sexes based upon interviews while patients were hospitalized.23 Use of electronic referral to CR upon hospital discharge, strong physician recommendation of CR and surgical diagnosis were predictors of CR attendance in women. Additionally, the authors examined how combinations of various characteristics can drastically change the likelihood of CR attendance for a given individual. For women, in particular, the likelihood of attending CR varied in large part as to whether women had high levels of social support (77% CR attendance) or low levels of support (33%). Similarly, women ≥61 yr with lower self reported physical function were less likely to participate compared with women reporting normal to high levels of physical function.23 This would suggest that low functional capacity may be a barrier to attending an outpatient CR program. Additional factors such as lack of awareness, unemployment, older age, and fear of exercise have also been associated with lower CR participation in women.8,24,25
While CR enrollment and attendance is low in women, this is particularly prominent for minority females.26 Among 366,103 Medicare patients eligible for CR, overall 18.9% women participated. Non-Hispanic black, Hispanic and Asian women had particularly low rates, averaging between 10-12%.27 Mochari et al examined ethnic differences in CR referral among 304 women (48% white, 34% black, 15% Hispanic) and found that minorities were less likely to receive instruction to attend CR and more likely to report financial barriers compared to whites.28 Specific attention should be focused to increase participation among racial and ethnic minority women.
Sex differences also persist regarding CR adherence. Compared to men, women are less likely to adhere or complete CR.29 Interestingly, Marzolini et al examined reasons for withdrawal from a 12 mo CR program and found that sex itself was not the necessarily the main reason for withdrawal but rather it was due to particular characteristics (single status, lower physical function, family issues) which tend to affect women more than men.30 Additionally, women who are active smokers, <55 yr, obese or lack coronary disease (ex. valve patients) are much less likely to complete CR.8,30,31 Table 1 summarizes the differences between men and women regarding CR participation, adherence, completion and fitness.
Table 1:
Differences Between Men and Women in Cardiac Rehabilitation
| Women | Men | |
|---|---|---|
| CR referral rates | 311 | 421 |
| CR participation rates | 19-392 | 29-452 |
| CR completion rates | 26-501,3 | 28-641,3 |
| Improvement in peak VO2 | 11-134,5 | 17-194,5 |
Abbreviations: CR, cardiac rehabilitation; peak VO2, peak aerobic capacity
Data represented as range (%)
Data adapted from studies with more than 1,000 subjects:
Colbert JD, et al. Eur J Prev Cardiol. 2015;22(8):979-986.
Samayoa L,et al. Can J Cardiol. 2014;30(7):793-800.
Ritchey MD, et al. Circ Cardiovasc Qual Outcomes. 2020;13(1):e005902.
Ades PA, et al. Circulation. 2006;113(23):2706-2712.
Rengo JL,et al. J Cardiopulm Rehabil Prev. 2020;40(5):319-324. Please see references for further information.
DEMOGRAPHICS OF FEMALE CR PARTICIPANTS
A recent study examined the evolving clinical and demographic characteristics of CR participants (n=5396) between 1996-2015 and significant sex differences were observed.32 Compared to men, women at CR entry were noted to be older with lower levels of fitness (all P <.001). While rates of diabetes and current smoking did not differ by sex, hypertension was more common in females (11% higher, P<.001) and women had higher co-morbidity scores (P <.02). Additionally, index diagnosis differed by sex. Patients with a diagnosis of MI or heart valve procedure were more likely to be female whereas patients with coronary artery bypass graft surgery were more likely to be male.32
CR BEHAVIORAL, CLINICIAL AND PSYCHOSOCIAL ISSUES in WOMEN
Many of the issues around engaging women in CR are tied to behavioral or psychosocial factors. Some of these barriers are present for both men and women, but are more prevalent in women or have a larger impact. For example, one of the strongest predictors of attending CR is the strength of the physician recommendation.23,33 However, compared to men, women are more likely to report not having CR strongly recommended, or not receiving support in enrolling in CR.34 Women are also more likely to rate lack of awareness of CR as a barrier to attending.25
Transportation problems are an often-cited barrier to participation, and specifically the ability to drive is strongly associated with attending CR.35 As mentioned earlier, women tend to enter CR at older ages, with more comorbidities, and thus are also less likely to be independent, including driving themselves. Indeed, transportation is more likely to be mentioned by women than men as a barrier to CR attendance.25,30
Smoking is another serious concern within the CR population and receiving a CR-eligible diagnosis, such as MI, may not be enough for a person to successfully quit smoking.36 In the majority of studies examining smoking and CR, women are often underrepresented, making it difficult to discern if there is an underlying sex difference.36,37 Current smoking, in addition to being highly associated with further negative health outcomes, is a strong independent predictor of dropout in CR.37 It is highly likely, therefore, for a female current smoker to not participate or drop out from CR compared to a female non-smoker. Current smoking should be a particular focus for CR in regards to women; the association of negative health effects with smoking appears to be stronger in women than in men, and women may have more difficulty quitting smoking than men.38,39
With >80% of CR participants being overweight, there has been a dramatic increase in insulin resistance and type 2 diabetes mellitus in CR.40 In one study, women had a higher prevalence of insulin resistance than men (73 vs. 64%) and a greater percentage with an elevated waist circumference (71% vs 60%).41 While those with type 2 diabetes mellitus are less likely to complete CR than non-diabetics, the difference is greater in women (72 vs 82%) than in men (83 vs 86%).42 Interventions specifically directed towards female diabetics may improve CR adherence rates.
Psychiatric symptoms such as depression and anxiety are associated with lower levels of CR attendance and adherence.43 In the U.S., women have about twice the rate of depression as men and studies suggest, among older adults, women are at least twice as likely to suffer from anxiety disorders.44,45 Accordingly, women are more likely to have elevated anxiety and depressive symptoms coming into CR which are likely to impact the participation and attendance. 46
Other behavioral barriers to CR participation are more specific to women. For example, social relationships play an important role for women. Women are more likely to take on caregiving roles, and those who should attend CR may be caring for children, partners, or parents. Social obligations can interfere with management of their own medical condition, decreasing the likelihood of attending CR. Indeed, women are much more likely than men to report family responsibilities as a barrier to attending CR.25,30 A lack of social support may also impact CR attendance among women suggesting that a combination of high social obligations with low social support could be extremely challenging for women.23,43
Women also appear to differ in how they experience the exercise portion of CR. Enjoyment of exercise is an important predictor of CR adherence. People who exercised regularly before their event are more likely to participate in and men are more likely to have higher levels of physical activity coming into CR.47,48 Contrast this with women, who are older with more comorbidities which could make exercise more painful or difficult. Indeed, women are more likely than men to report exercise as being tiring/painful, or issues with musculoskeletal conditions, as being barriers for CR adherence.25,30 Behavioral factors play a major role in the lower CR participation rates in women and there is an opportunity for CR liaisons to address these issues for women in order to improve CR participation.
INTERVENTIONS TO IMPROVE CR UTILIZATION IN WOMEN
Although there is limited research specifically examining ways to improve CR participation and adherence in women, certain interventions have proven to be beneficial (Figure 2). The use of automatic electronic referral for hospitalized patients has been shown to increase participation as well as overcome a potential bias on the part of the provider as to whether or not a patient is suitable for CR; this is particularly pertinent for women given that they tend to be under-referred. 8,49 A systemic referral process can improve CR referral by a factor of 2-7 times.49 Interestingly, in subsequent research, use of electronic referral was noted to be an independent predictor for CR participation in women.23,50
Figure 2:
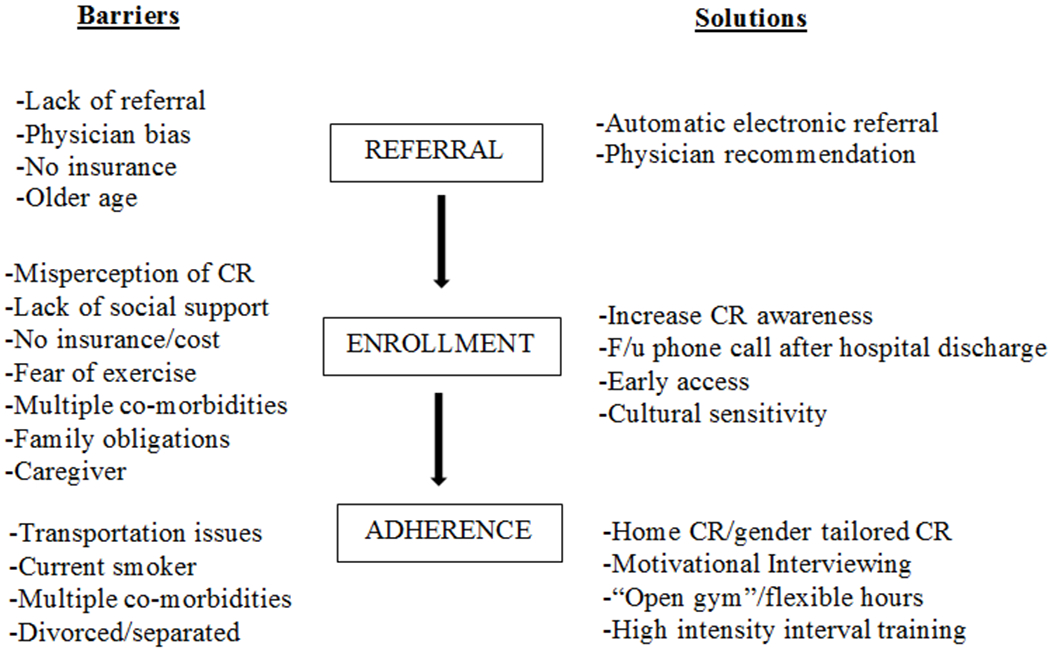
Utilization of Cardiac Rehabilitation in Women: Specific Barriers and Solutions
Sanderson et al found that women who did not attend CR often stated “my doctor doesn’t think I really need it.”24 Thus, interventions aimed at increasing CR awareness among patients and health care providers have been found to improve referral and enrollment rates. 51,52 Recent findings that women who received a strong recommendation from their provider while in the hospital are much more likely to attend CR support this idea.23
Due to family obligations, many women have difficulty attending CR often due to the scheduled set times.20,25 If women lack appropriate support at home, they may be unwilling or unable to take time away from their responsibilities. Providing more flexible times or an “open gym” concept may help with this.53
Some women perceive CR as a “men’s club” and that CR may not fit with their needs.53 Several studies have examined the effect of different models of CR on participation among women with mixed results. Beckie et al performed a randomized controlled trial in which women were randomized to standard CR or a gender-tailored, stage of change matched CR program using motivational interviewing.54 Compared to traditional CR, the gender-tailored intervention increased attendance by four sessions. This motivational interviewing included in the intervention can perhaps help overcome the hesitancy or ambivalence towards healthy behavioral change. This, however, differs from Grace et al who compared program adherence between women referred to standard CR, supervised women-only CR or home based CR and found no difference in adherence among the alternative program models. 55
To help delineate this further, another trial assessed women’s preferences for different CR program models; patients were assigned to mixed-sex, women-only or home based CR. 56 Women were highly satisfied irrespective of the CR model, however the majority preferred supervised programs as opposed to home-based. Additional research, therefore, is needed to assess the utility of gender-tailored CR programs.
CARDIORESPIRATORY FITNESS: WOMEN vs MEN
Women entering CR programs are older with more co-morbidities and have lower cardiopulmonary fitness (CRF) and strength at baseline than men.57–59 Even after adjusting for age, women will have lower CRF, measured as peak oxygen uptake (VO2peak) than that of men upon entry to CR. Furthermore, in most studies, women do not improve VO2peak as much as men in CR despite having lower fitness at baseline.60–63
Among a diverse population consisting of 2,896 patients entering CR, women improved to a lesser degree in VO2peak than men, 11 vs 19% respectively.61 A more recent analysis of the same database in 2020 demonstrated similar findings with women improving only 13 vs 17% in men. 62 Additionally, a higher percentage of women failed to demonstrate any improvement in VO2peak whatsoever, compared to men (24 vs 16%, P <.001). This is of clinical significance given that VO2peak is the best predictor of mortality and survival benefits of CR. 64
Strength and Physical Function
Reduced muscular strength has been associated with increased cardiovascular disease and mortality for men and women and women have significant higher rates of physical disability than men of the same age.57,65,66 Women self report lower levels of physical function and have lower measured handgrip strength compared to men in the CR setting.52,57,62
One of the major goals in CR is to improve CRF and overall strength, yet it appears that women may not experience the same benefits of CR participation, perhaps, adjustments should be made regarding the exercise prescription for women in CR.
EXERCISE TRAINING REGIMENS SPECIFIC TO WOMEN
Currently, most CR programs do not alter the exercise prescription for women compared with men other than tailoring exercise intensity to the current CRF status of the participant. Studies at our institution and elsewhere have demonstrated that the exercise prescription for women in CR should differ versus what is utilized for men.
Resistance Training
Given that women entering CR tend to be older and have lower muscle mass and strength, additional focus should be placed on resistance training (RT). It is notable that RT alone improves leg strength and walking endurance among older individuals.63,67,68 The value of RT on measures of physical performance were carefully assessed in a randomized controlled trial in 42 disabled female coronary patients >65 yr.68 Subjects were randomized to higher intensity RT or a control group that performed light yoga and breathing exercises. Weight training for 7 different exercises began at 50% of 1-repetition maximum gradually increasing to 80% of 1-repetition maximum, as tolerated. Also, intensity was guided by perceived exertion scores with patients increasing the resistance when perceived exertion scores drop below a threshold value (14 on the Borg scale of 6-20). The resistance-training program was performed with universal weights and dumbbells. The 7 exercises focused on leg, arm, and shoulder strength. Measurable improvements were seen in a wide range of physical activities such as stair climb, grocery carry, and 6 minute walk test as well as tasks involving flexibility and coordination such as pouring a gallon of milk or vacuuming.68 This study demonstrated that participation in high intensity RT can be done safely and improves performance of a wide range of daily activities in older women with heart disease; thus, a strong emphasis should be placed on strength training for women undergoing CR.
Higher Intensity Aerobic Interval Training
High intensity interval training (HIIT) is more effective in increasing VO2peak compared to traditional moderate intensity continuous training in patients with heart disease.69,70 However, the majority of HIIT studies consisted primarily of men with heart disease; thus, the true benefits for female cardiac patients alone remains poorly defined.69–71
In one study of 1787 patients who completed CR, response to exercise training differed by sex.62 In this particular study, only 11% of women performed interval training while for men, it was 22% and for most, this was moderate rather than HIIT. The discrepancy of HIIT between women and men can perhaps, at least in part, explain the lower response in VO2peak.
Since RT alone improves both leg strength and walking endurance in older adults, Khadanga et al set out to optimize exercise training response in women by combining intensive strength training with HIIT.59,72 In this study, 56 women were randomized to either a control status of standard aerobic exercise training (70-85% of peak heart rate) with moderate intensive RT vs. HIIT (90-95% of peak heart rate) along with higher intensive lower extremity RT 3 sessions/wk for 12wk. The mean age of women in this study was 65±11 with a range of 43-98 yr. VO2peak increased to a greater degree in the HIIT group (+23%) than in the control group (+7%) (0.3±0.07 vs 0.1±0.01 L/min, P<.03). Similarly, the change in leg extension strength was greater in the HIIT-RT group compared to the control group (15.3±0.3 vs 6.4±1.1 kg, P <.001).59 The exercise prescription for women in CR should consist of intensive RT and HIIT within the range of women’s fitness to help address differences in fitness outcomes compared to men.
CR FOR SPECIAL POPULATIONS of WOMEN
Spontaneous coronary artery dissection (SCAD) is a non-traumatic tear in the coronary vessel and is an important cause of MI in younger women, accounting for 10-30% of MIs in women <50 yr.73 Current guidelines recommend CR for all patients with recent MI caused by SCAD due to the mounting supporting evidence that participation in CR improves not only physical and social well being but also lower symptom frequency.73,74 Often, these women do not have the traditional CVD risk factors therefore, therapy in CR should be tailored to focus on patient centered goals and psychosocial behavior to help subside the fear of exercise many patients experience following their SCAD event.74,75
Given the suggestion of an association between SCAD and extreme physical exertion, these women are often advised against prolonged high-intensity activities or participation in competitive sports.73 While all are encouraged to engage in moderate intensity exercise, there is some evidence to support the use of HIIT in female patients with SCAD.76 In this small retrospective study, female patients participated in moderate intensity exercise training and when able to exercise 20 continuous minutes at prescribed intensity (usually after session 4-6), HIIT was incorporated. Improvements in depression symptomology and VO2peak were seen and no adverse events were reported. Unfortunately, there are no clear guidelines regarding exercise prescription for aerobic training or strength training in the SCAD population and additional research is needed.73
Stress induced cardiomyopathy (SICM) also known as Takasubo’s cardiomyopathy is characterized by a transient decrease of systolic function of the left ventricle without evidence of obstructive coronary disease. It is often due to intense emotional or physical stress and the clinical presentation is similar to acute coronary syndrome and often includes an elevation of cardiac enzymes. SICM occurs more frequently in postmenopausal women, accounting for ~90% of reported cases.77 In a retrospective study performed at Mayo Clinic Rochester, 380 unique patients were identified with SICM from 2008-2015.78 Of those, only 18 patients (5%) were referred to CR all of whom were female. Further, only 10 of the 18 (55%) completed CR. Following CR completion, significant improvements were seen in exercise duration and weight reduction. Future research is needed to identify barriers for enrollment as well as reasons for poor CR adherence in patient with SICM.
FUTURE DIRECTIONS: MOVING FORWARD
The underutilization of CR has led to national level efforts to increase CR participation such as the Million Hearts initiative which aims to achieve 70% participation rate by 2022.79 To help overcome the disparity seen between men and women in CR, additional research specifically tailored to women is needed. Strong physician recommendation, increased awareness and automatic referral can increase female CR participation.23,25,49 To increase CR attendance, alternative models of CR delivery such as hybrid home based CR or smartphone based CR may provide the flexibility needed for some women but further research is warranted to assess the impact of these newer programs.8 Given the lack of social support and high rates of anxiety and depression in women, perhaps assigning a case manager can provide the necessary assistance and support needed to increase CR participation.
Use of motivational interviewing can help overcome the hesitancy women have towards healthy behavioral change and promote CR adherence.54 Other modalities of exercise such as Zumba classes or group walking activities are more appealing to women and perhaps can be incorporated into CR programs.53 Additionally, more research is warranted in minority women and those of lower socioeconomic status given that they are the most vulnerable population and least likely to use CR.25,80
CONCLUSIONS
Cardiovascular disease affects women in alarming numbers and despite the benefits of CR for secondary prevention, it continues to be substantially underutilized. Specific interventions such as automatic electronic referral and a strong physician recommendation can help aid in CR participation, however, additional studies are needed to improve longer term adherence. Efforts should be made to help women overcome some of the behavioral and psychological barriers that can hinder CR attendance. While women entering CR tend to be older and have lower CRF at baseline, they fail to improve their fitness as much compared to men. This may be attributed to discrepancies in how the exercise training protocol is applied between men and women. The use of higher intensity aerobic and resistance training should be incorporated wherever possible, irrespective of age. Additionally, certain conditions such as SCAD and SICM are more prevalent in women and CR can serve a pivotal role in the treatment and management of these patients.
Sources of Funding:
This research was supported by National Institutes of Health Center of Biomedical Research Excellence award from the National Institute of General Medical Sciences: P20GM103644 and by the National Heart, Lung and Blood Institute: R33HL143305.
Footnotes
Conflicts of Interest: None
REFERENCES
- 1.https://www.cdc.gov/heartdisease/women.htm. Accessed December 2, 2020.
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015. Jan 27;131(4):e29–322. [DOI] [PubMed] [Google Scholar]
- 3.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124(29):2951–2960. [DOI] [PubMed] [Google Scholar]
- 4.Martin BJ, Hauer T, Arena R, et al. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation. 2012;126(6):677–687. [DOI] [PubMed] [Google Scholar]
- 5.Schofper DW, Forman DE. Cardiac rehabilitation in older adults. Can J Cardiol. 2016;32(9):1088–1096. [DOI] [PubMed] [Google Scholar]
- 6.Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. New England Journal of Medicine. 2001;345(12):892–902. [DOI] [PubMed] [Google Scholar]
- 7.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, and Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007; 116(15):1653–1662. [DOI] [PubMed] [Google Scholar]
- 8.Supervía M, Medina-Inojosa JR, Yeung C, et al. Cardiac rehabilitation for women: a systematic review of barriers and solutions. Mayo Clin Proc. 2017; S0025-6196(17)30026-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peters SAE, Muntner P, Woodward M. Sex differences in the prevalence of, and trends in, cardiovascular risk factors, treatment, and control in the United States, 2001 to 2016. Circulation. 2019;139(8):1025–1035. [DOI] [PubMed] [Google Scholar]
- 10.Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation 2018;137:e67–492. [DOI] [PubMed] [Google Scholar]
- 11.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the US population in 1988–1994 and 2005–2006. Diabetes Care. 2009; 32(2):287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia M, Mulvagh SL, Merz CN, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118(8):1273–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.EUGenMed Cardiovascular Clinical Study Group, Regitz-Zagrosek V, Oertelt-Prigione S, et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. 2016;37(1):24–34. [DOI] [PubMed] [Google Scholar]
- 15.Mehta LS, Beckie TM, DeVon HA, et al. American Heart Association Cardiovascular Disease in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, and Council on Quality of Care and Outcomes Research. Acute Myocardial Infarction in Women: A Scientific Statement From the American Heart Association. Circulation. 2016. Mar 1;133(9):916–47. [DOI] [PubMed] [Google Scholar]
- 16.Colbert JD, Martin BJ, Haykowsky MJ, et al. Cardiac rehabilitation referral, attendance and mortality in women. Eur J Prev Cardiol. 2015;22(8):979–986. [DOI] [PubMed] [Google Scholar]
- 17.Smith SJ Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124(22):2458–73. [DOI] [PubMed] [Google Scholar]
- 18.Cossette S, Maheu-Cadotte MA, Mailhot T, et al. Sex- and gender-related factors associated with cardiac rehabilitation enrollment: a secondary analysis among systematically referred patients. J Cardiopulm Rehabil Prev. 2019;39(4):259–265. [DOI] [PubMed] [Google Scholar]
- 19.Samayoa L, Grace SL, Gravely S, Scott LB, Marzolini S, Colella TJ. Sex differences in cardiac rehabilitation enrollment: a meta-analysis. Can J Cardiol. 2014;30(7):793–800. [DOI] [PubMed] [Google Scholar]
- 20.Grace SL, Abbey SE, Shnek ZM, Irvine J, Franche RL, Stewart DE. Cardiac rehabilitation II: referral and participation. Gen Hosp Psychiatry. 2002;24(3):127–34. [DOI] [PubMed] [Google Scholar]
- 21.Cooper AF, Jackson G, Weinman J, Horne R. Factors associated with cardiac rehabilitation attendance: a systematic review of the literature. Clin Rehabil. 2002;16(5):541–552. [DOI] [PubMed] [Google Scholar]
- 22.Lieberman L, Meana M, Stewart D. Cardiac rehabilitation: gender differences in factors influencing participation. J Womens Health. 1998;7(6):717–723. [DOI] [PubMed] [Google Scholar]
- 23.Khadanga S, Savage PD, Gaalema DE, Ades PA. Predictors of cardiac rehabilitation participation: opportunities to increase enrollment. J Cardiopulm Rehabil Prev. 2021. Jan 25. Epub ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanderson BK, Shewchuk RM, Bittner V. Cardiac rehabilitation and women: what keeps them away? J Cardiopulm Rehabil Prev. 2010;30(1):12–21 [DOI] [PubMed] [Google Scholar]
- 25.Grace SL, Gravely-Witte S, Kayaniyil S, Brual J, Suskin N, Stewart DE. A multi-site examination of sex differences in cardiac rehabilitation barriers by participation status. Journal of Women’s Health. 2009;18(2):209–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allen JK, Scott LB, Stewart KJ, Young DR. Disparities in women’s referral to and enrollment in outpatient cardiac rehabilitation. J Gen Intern Med. 2004;19(7):747–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ritchey MD, Maresh S, McNeely J, et al. Tracking cardiac rehabilitation participation and completion among medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes. 2020;13(1):e005902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mochari H, Lee JR, Kligfield P, Mosca L. Ethnic differences in barriers and referral to cardiac rehabilitation among women hospitalized with coronary heart disease. Prev Cardiol. 2006;9(1):8–13. [DOI] [PubMed] [Google Scholar]
- 29.Feola M, Garnero S, Daniele B, et al. Gender differences in the efficacy of cardiovascular rehabilitation in patients after cardiac surgery procedures. J Geriatr Cardiol. 2015;12(5):575–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marzolini S, Brooks D, Oh PI. Sex differences in completion of a 12-month cardiac rehabilitation programme: an analysis of 5922 women and men. Eur J Cardiovasc Prev Rehabil. 2008;15(6):698–703. [DOI] [PubMed] [Google Scholar]
- 31.Women Missik E. and cardiac rehabilitation: accessibility issues and policy recommendations. Rehabil Nurs. 2001;26(4):141–147. [DOI] [PubMed] [Google Scholar]
- 32.Gaalema DE, Savage PD, Leadholm K, et al. Clinical and demographic trends in cardiac rehabilitation: 1996-2015. J Cardiopulm Rehabil Prev. 2019;39(4):266–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghisi GL, Polyzotis P, Oh P, Pakosh M, Grace SL. Physician factors affecting cardiac rehabilitation referral and patient enrollment: a systematic review. Clinical Cardiology. 2013;36(6):323–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benz Scott LA, Ben-Or K, Allen JK. Why are women missing from outpatient cardiac rehabilitation programs? A review of multilevel factors affecting referral, enrollment, and completion. Journal of Women’s Health. 2002;11(9):773–91. [DOI] [PubMed] [Google Scholar]
- 35.Ruano-Ravina A, Pena-Gil C, Abu-Assi E, et al. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int J of Cardiol. 2016; 223:436–443. [DOI] [PubMed] [Google Scholar]
- 36.Gaalema DE, Pericot-Valverde I, Bunn JY, et al.Tobacco use in cardiac patients: perceptions, use, and changes after a recent myocardial infarction among US adults in the PATH study (2013–2015). Prev Med. 2018;117:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gaalema DE, Cutler AY, Higgins ST, Ades PA. Smoking and cardiac rehabilitation participation: associations with referral, attendance and adherence. Prev Med. 2015. 80:67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378(9799):1297–305. [DOI] [PubMed] [Google Scholar]
- 39.Smith PH, Bessette AJ, Weinberger AH, Sheffer CE, McKee SA. Sex/gender differences in smoking cessation: a review. Prev Med. 2016;92:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ades PA, Savage PD, Toth MJ, et al. High-calorie-expenditure exercise. A new approach to cardiac rehabilitation for overweight coronary patients. Circulation. 2009;119(20):2671–2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khadanga S, Savage PD, Ades PA. Insulin Resistance and Diabetes Mellitus in Contemporary Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2016;36(5):331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Armstrong MJ, Martin BJ, Arena R, et al. Patients with diabetes in cardiac rehabilitation: attendance and exercise capacity. Med Sci Sports Exerc. 2014;46(5):845–850. [DOI] [PubMed] [Google Scholar]
- 43.Resurrección DM, Moreno-Peral P, Gómez-Herranz M, et al. Factors associated with non-participation in and dropout from cardiac rehabilitation programmes: a systematic review of prospective cohort studies. Euro J of Cardiovasc Nurs. 2019;18(1):38–47. [DOI] [PubMed] [Google Scholar]
- 44.Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013-2016. NCHS Data Brief, no 303. Hyattsville, MD: National Center for Health Statistics. 2018. [PubMed] [Google Scholar]
- 45.Canuto A, Weber K, Baertschi M, et al. Anxiety disorders in old age: psychiatric comorbidities, quality of life, and prevalence according to age, gender, and country. Am J Geriatr Psychiatry. 2018;26(2):174–185. [DOI] [PubMed] [Google Scholar]
- 46.Caulin-Glaser T, Maciejewski PK, Snow R, LaLonde M, Mazure C. Depressive symptoms and sex affect completion rates and clinical outcomes in cardiac rehabilitation. Prev Cardiol. 2007;10(1):15–21. [DOI] [PubMed] [Google Scholar]
- 47.Lane D, Carroll D, Ring C, Beevers DG, Lip GY. Predictors of attendance at cardiac rehabilitation after myocardial infarction. Journal of psychosomatic research. 2001;51(3):497–501. [DOI] [PubMed] [Google Scholar]
- 48.O’Farrell P, Murray J, Huston P, LeGrand C, Adamo K. Sex differences in cardiac rehabilitation. Can J Cardiol. 2000;16(3):319–325. [PubMed] [Google Scholar]
- 49.Grace SL, Russell KL, Reid RD, et al. Effect of cardiac rehabilitation referral strategies on utilization rates: a prospective, controlled study. Arch Intern Med. 2011;171(3):235–241. [DOI] [PubMed] [Google Scholar]
- 50.Mueller E, Savage PD, Schneider DJ, et al. Effect of a computerized referral at hospital discharge on cardiac rehabilitation participation rates. J Cardiopulm Rehabil Prev. 2009;29(6):365–369. [DOI] [PubMed] [Google Scholar]
- 51.Dankner R, Drory Y, Geulayov G, et al. A controlled intervention to increase participation in cardiac rehabilitation. Eur J Prev Cardiol. 2015;22(9):1121–1128. [DOI] [PubMed] [Google Scholar]
- 52.Ades PA, Waldman ML, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol. 1992;69(17):1422–1425. [DOI] [PubMed] [Google Scholar]
- 53.Vidal-Almela S, Czajkowski B, Prince SA, et al. Lessons learned from community- and home-based physical activity programs: A narrative review of factors influencing women’s participation in cardiac rehabilitation. Eur J Prev Cardiol. 2020;2047487320907748. [DOI] [PubMed] [Google Scholar]
- 54.Beckie TM, Beckstead JW. Predicting cardiac rehabilitation attendance in a gender-tailored randomized clinical trial. J Cardiopulm Rehabil Prev. 2010;30(3):147–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grace SL, Midence L, Oh P, et al. Cardiac rehabilitation program adherence and functional capacity among women: a randomized controlled trial. Mayo Clin Proc. 2016;91(2):140–148 [DOI] [PubMed] [Google Scholar]
- 56.Andraos C, Arthur HM, Oh P, Chessex C, Brister S, Grace SL. Women’s preferences for cardiac rehabilitation program model: a randomized controlled trial. Eur J Prev Cardiol. 2015;22(12):1513–1522. [DOI] [PubMed] [Google Scholar]
- 57.Ades PA, Maloney A, Savage PD, Carhart RL. Determinants of physical functioning in coronary patients: response to cardiac rehabilitation. Arch Intern Med. 1999;159(19):2357–2360. [DOI] [PubMed] [Google Scholar]
- 58.Mroszczyk-McDonald A, Savage PD, Ades PA. Handgrip strength in cardiac rehabilitation: normative values, interaction with physical function, and response to training. J Cardiopulm Rehabil Prev. 2007;27(5):298–302. [DOI] [PubMed] [Google Scholar]
- 59.Khadanga S, Savage PA, Pecha A, Rengo J, Ades PA. Optimizing Training Response for Women in Cardiac Rehabilitation: A Randomized Controlled Trial. Manuscript in Review [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stone JA, Arena R, Hauer T, Matin BJ, et al. Long-term retention of aerobic fitness improvements following participation in cardiac rehabilitation. Int J Cardiol. 2011;150(3):355–356. [DOI] [PubMed] [Google Scholar]
- 61.Ades PA, Savage PD, Brawner CA, et al. Aerobic capacity in patients entering cardiac rehabilitation. Circulation. 2006;113(23):2706–2712. [DOI] [PubMed] [Google Scholar]
- 62.Rengo JL, Khadanga S, Savage PD, Ades PA. Response to exercise training during cardiac rehabilitation differs by sex. J Cardiopulm Rehabil Prev. 2020;40(5):319–324. [DOI] [PubMed] [Google Scholar]
- 63.Savage PD, Antkowiak M, Ades PA. Failure to improve cardiopulmonary fitness in cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2009;29(5):284–91 [DOI] [PubMed] [Google Scholar]
- 64.Kavanagh T, Mertens DJ, Hamm LF, Beyene J, Kennedy J, Corey P Prediction of long-term prognosis in 12169 men referred for cardiac rehabilitation. Circulation 2002; 106:666–671. [DOI] [PubMed] [Google Scholar]
- 65.Carbone S, Kirkman DL, Garten RS, et al. Muscular Strength and Cardiovascular Disease: AN UPDATED STATE-OF-THE-ART NARRATIVE REVIEW. J Cardiopulm Rehabil Prev. 2020;40(5):302–309. [DOI] [PubMed] [Google Scholar]
- 66.Artero EG, Lee DC, Lavie CJ, et al. Effects of muscular strength on cardiovascular risk factors and prognosis. J Cardiopulm Rehabil Prev. 2012;32(6):351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fiatarone MA, Marks EC, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA.1990;263(22):3029–34 [PubMed] [Google Scholar]
- 68.Ades PA, Savage P, Cress ME, Brochu M, Lee NM, Poehlman ET. Resistance training on physical performance in disabled older female cardiac patients. Med Sci Sports Exerc. 2003;35:1265–70. [DOI] [PubMed] [Google Scholar]
- 69.Rognmo O, Hetland E, Helgerud J, Hoff J, et al. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2004;11(3):216–22. [DOI] [PubMed] [Google Scholar]
- 70.Wisløff U, Støylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007. 115(24):3086–94. [DOI] [PubMed] [Google Scholar]
- 71.Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227–1234. [DOI] [PubMed] [Google Scholar]
- 72.Ades PA, Ballor DL, Ashikaga T, Utton JL, Nair KS. Weight training improves walking endurance in healthy elderly persons. Ann Intern Med. 1996;124:568–72. [DOI] [PubMed] [Google Scholar]
- 73.Hayes SN, Tweet MS, Adlam D, Kim ESH, Gulati R, Price JE, Rose CH. Spontaneous coronary artery dissection: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76(8):961–984. [DOI] [PubMed] [Google Scholar]
- 74.Tweet MS, Hayes SN, Pitta SR, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126(5):579–588 [DOI] [PubMed] [Google Scholar]
- 75.Krittanwong C, Tweet MS, Hayes SN et al. Usefulness of cardiac rehabilitation after spontaneous coronary artery dissection. Am J Cardiol. 2016;117(110):1604–1609. [DOI] [PubMed] [Google Scholar]
- 76.Siber TC, Tweet MS, Bowman MD et al. Cardiac rehabilitation after spontaneous coronary artery dissection. J Cardiopul Rehab Prev. 2014;34(2):138–142. [DOI] [PubMed] [Google Scholar]
- 77.Medina de Chazal H, Del Buono MG, Keyser-Marcus L, et al. Stress cardiomyopathy diagnosis and treatment: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018;72(16):1955–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wu CM, McKeon J, Abbott JD, Jiang L, Wu WC. Referral to cardiac rehabilitation and outcomes for patients with takotsubo cardiomyopathy. J Cardiopulm Rehabil Prev. 2019;39(3):E8–E11. [DOI] [PubMed] [Google Scholar]
- 79.Wall HK, Stolp H, Wright JS, et al. The Million Hearts Initiative: Catalyzing utilization of cardiac rehabilitation and accelerating implementation of new care models.. J Cardiopulm Rehabil Prev. 2020;40(5):290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mead H, Ramos C, Grantham SC. Drivers of racial and ethnic disparities in cardiac rehabilitation use: patient and provider perspectives. Med Care Res Rev. 2016;73(3):251–282. [DOI] [PubMed] [Google Scholar]


