Abstract
Introduction
In older U.S. nursing home residents, there is limited research on the prevalence of physical frailty, its potential dynamic changes, and its association with cognitive impairment in older adults’ first six months of nursing home stay.
Methods
Minimum Data Set (MDS) 3.0 is the national database on residents in U.S. Medicare-/Medicaid-certified nursing homes. MDS 3.0 was used to identify older adults aged ≥65 years, newly-admitted to NHs during 2014/01/01 and 2016/06/30, with life expectancy ≥6 months at admission and NH length of stay ≥6 months (n=571,139). MDS 3.0 assessments at admission, 3 months and 6 months were used. In each assessment, physical frailty was measured by FRAIL-NH (robust; pre-frail; frail) and cognitive impairment by Brief Interview for Mental Status and Cognitive Performance Scale (none/mild; moderate; severe). Demographic characteristics and diagnosed conditions were measured at admission, while presence of pain and receipt of psychotropic medications were at each assessment. Distribution of physical frailty and its change over time by cognitive impairment were described. Non-proportional odds model was fitted with generalized estimation equation to longitudinally examine the association between physical frailty and cognitive impairment, adjusting for demographic and clinical characteristics.
Results
Around 60% of older residents were physically frail in the first 6 months. Improvement and worsening across physical frailty levels were observed. Particularly, in those who were pre-frail at admission, 23% improved to robust by 3 months. At admission, 3 months and 6 months, over 37% of older residents had severe cognitive impairment, and about 70% of those with cognitive impairment were physically frail. At admission, older residents with moderate cognitive impairment were 35% more likely [adjusted odds ratio (aOR): 1.35, 95% confidence interval (CI): 1.33-1.37] and those with severe impairment 74% more likely (aOR: 1.74, 95%CI: 1.72-1.77) to be frail than pre-frail/robust, compared to those with none/mild impairment. The association between the two conditions remained positive and consistently increased over time.
Discussion/Conclusion
Physical frailty was prevalent in NHs with potential to improve and was strongly associated with cognitive impairment. Physical frailty could be a modifiable target and interventions may include efforts to address cognitive impairment.
Keywords: Physical frailty, Cognitive Impairment, Nursing home, longitudinal study
Introduction
Physical frailty is characterized by decreased physiologic reserve and increased vulnerability to exogenous stressors[1] and affects 15% of community-dwelling older adults in the U.S.[2] Older adults with physical frailty are at elevated risks for falls, functional dependency, lowered quality of life, decreased life expectancy and mortality.[3–5] Physical frailty also predicts older adults’ admission to nursing homes (NHs).[6] U.S. NHs provide care to over 1.2 million older adults.[7] However, there is limited national-level research examining the burden of physical frailty and its associated characteristics after older adults entered NHs.
The early period of NH stay is not only a critical window for older residents to adjust to the changes in clinical care and living environment, but also a time when functional impairment could impact those adjustments and their long-term health outcomes.[8,9] Physical frailty is a dynamic condition and older adults may improve or decline across its spectrum.[10–12] Understanding the “natural history” of physical frailty over the early course of NH stay is important, as it may be a promising, potentially modifiable, target for intervention.[13]
Nearly two-thirds of older NH residents experience moderate to severe cognitive impairment.[7] Yet, little is known about the extent to which cognitive impairment impacts physical frailty in older NH residents during their stay. Given the strong correlation between physical frailty and cognitive impairment in community-dwelling older adults,[14–16] it is likely that older NH residents with more severe cognitive impairment would experience greater physical frailty. However, no studies have quantified this association in older NH residents.
To address these gaps, we conducted this longitudinal study using national NH data, the Minimum Data Set (MDS) 3.0. The objectives were to (1) estimate the prevalence of physical frailty at admission, 3 months and 6 months, (2) describe the changes in the prevalence of physical frailty over time; and (3) examine the association between physical frailty and cognitive impairment during older residents’ first six months of NH stay.
Materials and Methods
The University Institutional Review Board approved this study.
Data
MDS 3.0 is federally mandated for all residents in Medicaid-/Medicare-certified NHs at NH admission, quarterly, annually and when significant changes in residents’ health occurs, assessing residents’ demographics, cognitive functioning, mood, functional status, bladder and bowel conditions, nutritional status, diagnoses and medications.[17]
Sample
We included NH residents who were (1) newly-admitted between 01/01/2014 and 06/30/2016, (2) aged ≥65 years with life expectancy ≥6 months at admission, (3) stayed in the NH for ≥6 months, and (4) had MDS 3.0 assessments at admission, 3 months and 6 months of NH stay. See Method Supplement and Supplementary Figure S1 for details.
Measures
Physical frailty
FRAIL-NH was developed to measure physical frailty in NHs using MDS 3.0 items on Fatigue, Resistance, Ambulation, Incontinence, Loss of weight, Nutritional approach and Help with dressing.[18,19] (Supplementary Table S1; total score: 0-13) FRAIL-NH has comparable performance in identifying residents with physical frailty with other well-established metrics across NH settings; physical frailty as assessed by FRAIL-NH was consistently predictive of adverse health outcomes.[19–25] Using MDS 3.0 assessments at admission, 3 months and 6 months, we scored each item and obtained the total FRAIL-NH score, which was categorized using previously validated thresholds: robust (0-5), prefrail (6-7), and frail (≥8).[21]
Cognitive impairment
Brief Interview for Mental Status (BIMS; total score: 0-15)[26] and Cognitive Performance Scale (CPS; total score: 0-6)[27] were used. Both were feasible for the NH population and highly correlated with standard cognitive function examination, including the Mini-Mental Status Examination.[26,27] Cognitive impairment was categorized as none/mild impairment (BIMS 13-15/CPS 0-2), moderate impairment (BIMS 8-12/CPS 3-4), and severe impairment (BIMS 0-7/CPS 5-6) [7] and measured at admission, 3-month and 6-month as a time-varying variable. (See Method Supplement)
Demographic and clinical characteristics
Demographics were assessed at admission: age groups, sex, race/ethnicity, NH location (urban; rural), admission sources (community; acute hospital; other). (See Method Supplement)
For clinical characteristics, we examined at admission if older residents were diagnosed with: arthritis, diabetes mellitus, hypertension, cancer, cerebrovascular accident/transient ischemic attack (TIA)/stroke, heart failure, asthma/chronic obstructive pulmonary disease (COPD)/chronic lung disease, dementia, Alzheimer’s disease, Parkinson’s disease, anxiety disorder, depression, hip fracture, other fracture, osteoporosis, multiple sclerosis, seizure disorder/epilepsy. We measured presence of pain and receipt of psychotropic medications (antipsychotics; antianxiety medications; antidepressants; hypnotics) at admission, 3 months and 6 months to capture the potential time-varying experience of pain and receipt of medications.
Analysis
Distributions of sample demographic and clinical characteristics at admission calculated. Prevalence of physical frailty at admission, 3 months and 6 months were shown, followed by its changes over time. As a trivial difference would be statistically significant with the large sample size, a 5% difference was considered noteworthy.
To examine the longitudinal association between physical frailty and cognitive impairment, a non-proportional odds model (NPOM) was fitted. Physical frailty was operationalized as an ordinal variable with three levels (robust/pre-frail/frail) measured repeatedly at admission, 3 months and 6 months. Independent variables included assessment times (3-month; 6-month), cognitive impairment and its interaction with assessment times, and demographic and clinical variables and their respective interactions with the assessment times. The associations between the independent variables and physical frailty may not be necessarily uniform across different levels of physical frailty. NPOM was thus used to capture this variation, because it does not assume proportional odds and estimates separate sets of log odds for frail versus prefrail/robust and for frail/pre-frail versus robust with respect to every independent variable.[28] Additionally, to capture the potential different correlations between repeated measures, NPOM was fitted with generalized estimation equation with the unstructured working covariance matrix. Results were presented in adjusted odds ratios (aOR) with 95% confidence intervals (CI) to show the concurrent associations between different levels of physical frailty and cognitive impairment at admission, 3 months and 6 months, adjusting for all other independent variables.
All analyses were conducted in SAS 9.4 with GEEORD macro for NPOM.[28] Figure was created in R with ggplot2.[29]
Results
Sample characteristics at admission
Nearly half of the older residents (n = 571,139) were ≥85 years, two-thirds were female, over 80% were non-Hispanic White, and one-fourth resided in a rural NH. The majority entered NH from acute hospitals, while 20.4% were admitted from the community. The top five diagnoses were hypertension (76.0%), dementia (41.8%), depression (37.2%), diabetes (30.2%), and arthritis (26.7%). About 39% of older adults reported presence of pain. One in five older residents received antipsychotics, and almost 45% received antidepressants. (Table 1)
Table 1.
Demographic and clinical characteristics at nursing home admission (n = 571,139)
| All (n = 571,139) |
|
|---|---|
| (column percent) | |
| Age (years) | |
| 65 - <75 | 20.3 |
| 75 - <85 | 34.2 |
| ≥ 85 | 45.5 |
| Sex | |
| Male | 33.1 |
| Female | 66.9 |
| Race/Ethnicity | |
| Non-Hispanic White | 81.9 |
| Racial/ethnic minority 1 | 18.1 |
| Nursing home location | |
| Urban | 75.6 |
| Rural | 24.4 |
| Admission source | |
| Community | 20.4 |
| Acute hospital | 59.6 |
| Other sources 2 | 20.1 |
| Diagnosed conditions | |
| Arthritis | 26.7 |
| Diabetes mellitus | 30.2 |
| Hypertension | 76.0 |
| Cancer | 5.9 |
| Cerebrovascular accident/TIA/stroke | 13.8 |
| Heart failure | 17.6 |
| Asthma/COPD/chronic lung disease | 18.5 |
| Dementia | 41.8 |
| Alzheimer’s disease | 13.2 |
| Parkinson’s disease | 6.0 |
| Anxiety disorder | 22.1 |
| Depression | 37.2 |
| Hip fracture | 5.0 |
| Other fracture | 7.4 |
| Osteoporosis | 12.2 |
| Multiple sclerosis | 0.5 |
| Seizure disorder/Epilepsy | 5.8 |
| Any presence of pain | 38.7 |
| Receipt of psychotropic medications | |
| Antipsychotics | 20.0 |
| Antianxiety medications | 18.4 |
| Antidepressants | 44.8 |
| Hypnotics | 4.0 |
Note. Abbreviation: TIA = transient ischemic attack; COPD = chronic obstructive pulmonary disease
Racial/ethnic minority includes American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian/Other Pacific Islander, multi-racial, and Hispanic or Latino of any race.
Other admission sources include another nursing home/swing bed, psychiatric hospital, inpatient rehabilitation facility, facility for the mentally retarded or developmentally disabled (MR/DD facility), hospice, long-term care hospital, and other unspecified sources.
Prevalence of physical frailty over time
The prevalence of physical frailty was 63.6% at admission, and similar at 3 months and 6 months around 60%. Improvement and decline across the levels of physical frailty were observed, especially in older adults who were pre-frail and during the first 3 months. Specially, 22.8% of older residents who were pre-frail at admission became robust by 3 months; later, 15.3% of those who were pre-frail at 3-month stay became robust by 6 months. About 30.5% of those who were pre-frail at admission were frail by 3 months, and 31.2% of those who were pre-frail at 3 months transitioned to frail at 6 months. (Table 2)
Table 2.
Prevalence and changes of physical frailty over older adults’ first six months of nursing home stay (n = 571,139)
| Physical frailty |
||||
|---|---|---|---|---|
| Robust | Pre-frail | Frail | ||
| (row percent) | ||||
| Prevalence at each time | ||||
| Admission | 11.0 | 25.4 | 63.6 | |
| 3 months | 17.0 | 23.5 | 59.5 | |
| 6 months | 17.5 | 21.9 | 60.5 | |
| Changes in physical frailty over time | ||||
| 3 months | ||||
| Admission | Robust | 75.9 | 17.1 | 7.0 |
| Pre-frail | 22.8 | 46.8 | 30.5 | |
| Frail | 4.7 | 15 .7 | 79 .7 | |
| 6 months | ||||
| 3 months | Robust | 75.7 | 17.2 | 7.1 |
| Pre-frail | 15.3 | 53.5 | 31.2 | |
| Frail | 1.8 | 11.0 | 87.2 | |
Prevalence of physical frailty over time by cognitive impairment
At admission, 30.5% of older adults had moderate cognitive impairment and 37.2% severe impairment, and similarly at 3 and 6 months. At all assessment times, physical frailty was less prevalent in older adults with none/mild cognitive impairment, and more prevalent in those with severe impairment. The prevalence of physical frailty appeared to decrease by almost 10% in those with none/mild impairment over time, with most decrease occurred in the first 3 months. The prevalence did not show considerable decrease among those with moderate or severe cognitive impairment. (Table 3)
Table 3.
Levels of physical frailty at admission, 3 months, and 6 months of older residents’ nursing home stay by cognitive impairment at each respective time (n = 571,139)
| All | Physical frailty 1 |
|||
|---|---|---|---|---|
| Robust | Pre-frail | Frail | ||
| (column percent) | (row percent) | |||
| Admission | ||||
| Cognitive impairment 2 | ||||
| None/Mild impairment | 32.3 | 12.6 | 30.5 | 56.9 |
| Moderate impairment | 30.5 | 11.1 | 25.1 | 63.8 |
| Severe impairment | 37.2 | 9.5 | 21.1 | 69.3 |
| 3-month | ||||
| Cognitive impairment 2 | ||||
| None/Mild impairment | 32.0 | 22.8 | 28.6 | 48.7 |
| Moderate impairment | 30.1 | 17.0 | 23.6 | 59.4 |
| Severe impairment | 37.9 | 12.1 | 19.2 | 68.7 |
| 6-month | ||||
| Cognitive impairment 2 | ||||
| None/Mild impairment | 31.3 | 25.2 | 27.5 | 47.3 |
| Moderate impairment | 29.4 | 17.5 | 22.3 | 60.2 |
| Severe impairment | 39.3 | 11.4 | 17.3 | 71.3 |
Note.
Physical frailty was measured at admission, 3-month, and 6-month.
Cognitive impairment was measured concurrently with physical frailty at admission, 3-month, and 6-month.
Association between physical frailty and cognitive impairment
Cognitive impairment was shown to be associated with physical frailty (Fig. 1; Supplementary Table S4). At admission, those with moderate impairment were 35% more likely to be frail (aOR: 1.35, 95% CI: 1.33-1.37) and those with severe impairment were 74% more likely to be frail (aOR: 1.74, 95% CI: 1.72-1.77) than pre-frail or robust. Moreover, these associations remained consistent and appeared to increase over time: at 3 months, older residents with moderate cognitive impairment were 42% more likely (aOR: 1.42, 95% CI: 1.40-1.43) and those with severe impairment were almost twice as likely (aOR: 1.96, 95% CI: 1.94-1.99) to be frail than pre-frail or robust; at 6 months, those with moderate impairment were 50% more likely (aOR: 1.50, 95% CI: 1.48-1.51) and those with severe impairment were over twice as likely (aOR: 2.24, 95% CI: 2.21-2.27) to be frail than pre-frail or robust. The set of odds of being frail/pre-frail vs. robust were slightly lower, but followed a similar increasing trend over time.
Fig. 1.
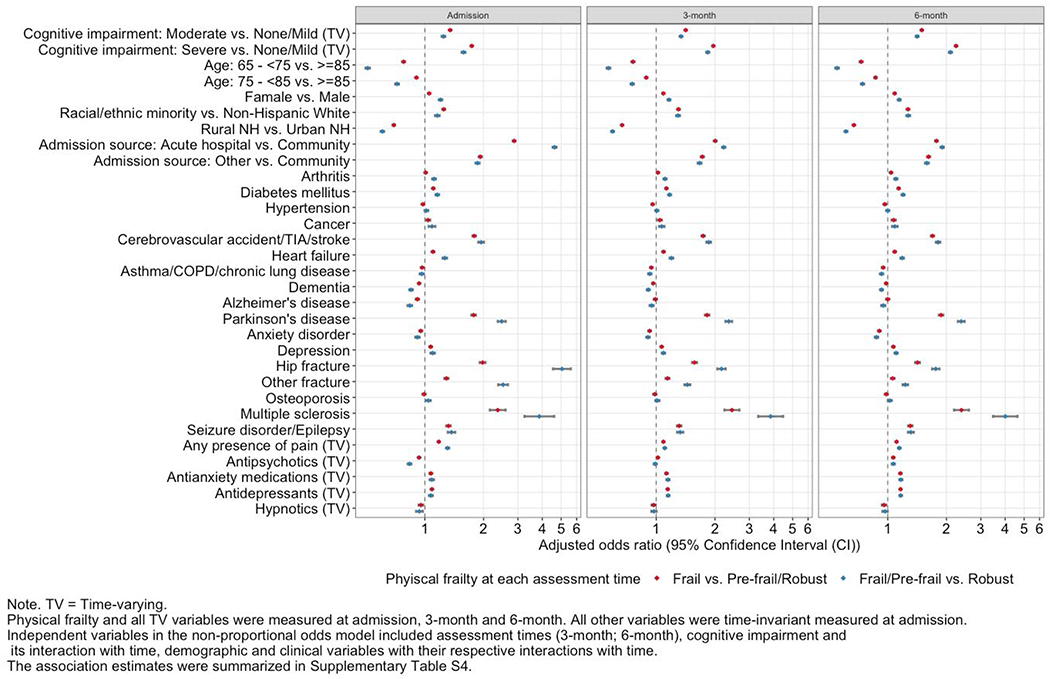
Concurrent associations between physical frailty and cognitive impairment, demographic and clinical characteristics over older residents’ first six months of nursing home stay
For demographic and clinical characteristics, younger age and residing in a rural NH were associated with lower odds to be frail vs. pre-frail/robust as well as frail/pre-frail vs. robust, while being female, racial/ethnic minority, and admitted from acute hospital or other sources were associated with higher odds. These associations remained consistent over time, with the only exception being admission from acute hospitals. At admission, older residents who entered NHs from acute hospitals were almost 3 times as likely to be frail than pre-frail/robust (aOR: 2.87, 95% CI: 2.83-2.91), and about 4.6 times as likely to be frail/pre-frail than robust (aOR: 4.62, 95% CI: 4.52-4.73), compared to those from the community. These associations remained positive but decreased over time.
At-admission diagnoses consistently associated with higher odds of physical frailty included arthritis, diabetes mellitus, cancer, cerebrovascular accident/TIA/stroke, heart failure, Parkinson’s disease, depression, hip fracture, other fracture, multiple sclerosis, and seizure disorder/epilepsy. Residents with presence of pain at admission, 3 months, or 6 months were at greater odds to be physically frail vs. pre-frail/robust at respective times. Those who received antianxiety medications or antidepressants consistently had greater odds of being frail vs. prefrail/robust as well as frail/prefrail vs. robust, while those who received hypnotics consistently had lower odds. In contrast, residents who received antipsychotics at admission were less likely to be physically frail vs. pre-frail/robust, but those who received antipsychotics at 3 months and 6 months were more likely to be physically frail.
Discussion/Conclusion
To the best of our knowledge, this is the first national-level study to longitudinally estimate the prevalence of physical frailty and its association with cognitive impairment over older adults’ first six months of stay in U.S. NHs. We found that nearly two in every three older NH residents were physically frail at admission, 3 months and 6 months. Improvement and decline in physical frailty were observed in substantial proportions of residents who were pre-frail and during the first 3 months. Greater levels of cognitive impairment were associated with higher levels of physical frailty at all assessment times, and this association consistently increased over time.
Clinical trials of interventions to improve physical frailty in older NH residents are rarely conducted and none in the U.S. In Spain, a 12-week multicomponent exercise intervention in NH residents aged ≥85 years with frailty was found effective in improving physical functioning, but change in frailty was not one of the outcomes.[30] Whether the physical, cognitive, nutritional or multi-pronged interventions that effectively improved physical frailty and other health outcomes in community-dwelling older adults [31,32] could be implemented in older NH residents remains unclear. The NH setting poses additional barriers. Staff’s priority might be given to essential tasks to maintain basic living,[33] leaving limited time and efforts to implement interventions that involve various physical activities. Nonetheless, interventions to address physical frailty are necessary, given that physical frailty is associated with numerous adverse health outcomes and that it is possible to reverse its progression. Cognitive impairment, plus several demographic and clinical characteristics, were found to be consistently associated with physical frailty over time, which could be informative in identifying older residents with greater odds of experiencing physical frailty. More importantly, this study found improvement in the physical frailty status were more often observed in older adults who were pre-frail and during the first 3 months of stay, which may represent a population and optimal window that have greater potential to benefit from intervention.
Findings provided evidence on the positive association between physical frailty and cognitive impairment in older NH residents, which was expected given the close interrelationship between these conditions [16,34–36] but missing in previous research mainly focusing on community-dwelling older adults. This study focused on the concurrent association between the two conditions at each assessment time, so findings cannot not attest to the potential bi-directional relationship between physical frailty and cognitive impairment in longitudinal studies of community older adults.[37–44] However, the strong and increasing association between the two conditions found in this study indicated the necessity to consider intervention methods to improve physical frailty involving cognitive component, such as cognitive training.[32] Future investigation is needed on if physical frailty could predict later changes in cognitive impairment and vice versa in older NH residents, in order to develop more effective intervention efforts.
We note a few limitations. We focused on older adults’ first six months of NH stay. As such, only those who had length of stay greater than six months were included. Yet, older residents with more severe physical frailty and/or cognitive impairment may be less likely to remain in the NH for over 6 months. Although we limited the sample to older residents with life expectancy greater than 6 months at admission, selection bias is still possible, if length of stay was differential with regards to physical frailty and cognitive impairment, and other demographic and characteristics. MDS 3.0 allowed us to conduct this national-level analysis, but we were limited by the availability of validated instruments and other clinical measures in it. FRAIL-NH is a relatively new instrument; therefore, more studies are needed to confirm our findings. The combined BIMS/CPS metric captures broad cognitive impairment levels. Further research on the association between specific cognitive domains and physical frailty in older NH residents may offer additional insight on their interrelationship. We were not able to examine if non-pharmacotherapy would influence physical frailty over time. While MDS 3.0 documents broad categories including occupational therapy, physical therapy and psychotherapy, the content of and residents’ participation in these therapies may largely vary across NHs. Due to the complexity of multilevel NPOM in a large sample, we could not address the impact of NH facility-level factors such as staffing and quality of care, warranting future work.
In conclusion, physical frailty was highly prevalent in older U.S. NH residents at admission and during the first six months of stay, with improvement more frequently occurred in those with pre-frail status and in the first three months. Cognitive impairment was shown to be strongly associated with physical frailty over time. Describing the dynamic nature of physical frailty over time in older NH residents is an essential first step towards the development of intervention to reverse physical frailty. By longitudinally addressing the association between physical frailty and cognitive impairment, findings have implications for future work on the mechanisms underlying the interrelationship between two conditions and physical frailty intervention to include efforts to address cognitive impairment.
Supplementary Material
Acknowledgments
FUNDING SOURCES
This work was supported by the National Institute on Aging (grant number: 1F99AG068591; PI: Yiyang Yuan) and the National Institute of Mental Health (grant number: 5R01MH117586; PI: Christine Ulbricht).
Footnotes
STATEMENT OF ETHICS
The University of Massachusetts Medical School Institutional Review Board has approved this study. The study was considered exempt because it was a secondary data analysis using data (the Minimum Data Set Version 3.0) under a strict data use agreement with the Centers for Medicare and Medicaid Services.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci [Internet]. 2001. March [cited 2019 Feb 19];56(3):M146–56. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11253156 [DOI] [PubMed] [Google Scholar]
- 2.Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, et al. Frailty in Older Adults: A Nationally Representative Profile in the United States. J Gerontol A Biol Sci Med Sci [Internet]. 2015. November [cited 2019 Mar 19];70(11):1427–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26297656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang SF, Lin PL. Frail phenotype and mortality prediction: A systematic review and meta-analysis of prospective cohort studies [Internet]. Vol. 52, International Journal of Nursing Studies. Pergamon; 2015. [cited 2019 Feb 23]. p. 1362–74. Available from: https://www.sciencedirect.com/science/article/pii/S0020748915001066 [DOI] [PubMed] [Google Scholar]
- 4.Kojima G, Taniguchi Y, Iliffe S, Walters K. Frailty as a Predictor of Alzheimer Disease, Vascular Dementia, and All Dementia Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc [Internet]. 2016. October 1 [cited 2019 Mar 13];17(10):881–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27324809 [DOI] [PubMed] [Google Scholar]
- 5.Vermeiren S, Vella-Azzopardi R, Beckwee D, Habbig A-K, Scafoglieri A, Jansen B, et al. Frailty and the Prediction of Negative Health Outcomes: A Meta-Analysis. J Am Med Dir Assoc [Internet]. 2016. December 1 [cited 2019 Feb 23];17(12):1163.e1–1163.e17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27886869 [DOI] [PubMed] [Google Scholar]
- 6.Kojima G Frailty as a Predictor of Nursing Home Placement Among Community-Dwelling Older Adults. J Geriatr Phys Ther [Internet]. 2018. [cited 2019 Feb 18];41(1):42–8. Available from: http://insights.ovid.com/crossref?an=00139143-201801000-00006 [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services. Nursing Home Data Compendium 2015. 2015.
- 8.Banaszak-Holl J, Liang J, Quiñones A, Cigolle C, Lee I-C, Verbrugge LM. Trajectories of Functional Change Among Long Stayers in Nursing Homes. J Aging Health [Internet]. 2011. August 24 [cited 2019 May 6];23(5):862–82. Available from: http://journals.sagepub.com/doi/10.1177/0898264311399759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee DT, Woo J, Mackenzie AE. The Cultural Context of Adjusting to Nursing Home Life: Chinese Elders’ Perspectives. Gerontologist [Internet]. 2002;42(5):667–75. Available from: https://pubmed.ncbi.nlm.nih.gov/12351802/ [DOI] [PubMed] [Google Scholar]
- 10.Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med [Internet]. 2006. February 27 [cited 2019 Mar 13];166(4):418–23. Available from: http://archinte.jamanetwork.com/article.aspx?doi=10.1001/archinte.166.4.418 [DOI] [PubMed] [Google Scholar]
- 11.Lee JSW, Auyeung T-W, Leung J, Kwok T, Woo J. Transitions in Frailty States Among Community-Living Older Adults and Their Associated Factors. J Am Med Dir Assoc [Internet]. 2014. April 1 [cited 2019 Feb 23];15(4):281–6. Available from: https://www.sciencedirect.com/science/article/pii/S1525861013006713?via%3Dihub [DOI] [PubMed] [Google Scholar]
- 12.Lorenzo-López L, López-López R, Maseda A, Buján A, Rodríguez-Villamil JL, Millán-Calenti JC. Changes in frailty status in a community-dwelling cohort of older adults: The VERISAÚDE study. Maturitas [Internet]. 2019. January 1 [cited 2019 Feb 23];119:54–60. Available from: https://www.sciencedirect.com/science/article/pii/S037851221830478X [DOI] [PubMed] [Google Scholar]
- 13.von Haehling S, Bernabei R, Anker SD, Morley JE, Vandewoude MF, Rockwood K, et al. Frailty Consensus: A Call to Action. J Am Med Dir Assoc [Internet]. 2013. June [cited 2019 Mar 18];14(6):392–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23764209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosado-Artalejo C, Carnicero JA, Losa-Reyna J, Guadalupe-Grau A, Castillo-Gallego C, Gutierrez-Avila G, et al. Cognitive Performance across 3 Frailty Phenotypes: Toledo Study for Healthy Aging. J Am Med Dir Assoc [Internet]. 2017. September 1 [cited 2019 Feb 23];18(9):785–90. Available from: https://www.sciencedirect.com/science/article/pii/S1525861017302232 [DOI] [PubMed] [Google Scholar]
- 15.Ávila-Funes JA, Amieva H, Barberger-Gateau P, Le Goff M, Raoux N, Ritchie K, et al. Cognitive impairment improves the predictive validity of the phenotype of frailty for adverse health outcomes: The three-city study. J Am Geriatr Soc [Internet]. 2009. March 1 [cited 2019 Mar 19];57(3):453–61. Available from: http://doi.wiley.com/10.1111/j.1532-5415.2008.02136.x [DOI] [PubMed] [Google Scholar]
- 16.Robertson DA, Savva GM, Kenny RA. Frailty and cognitive impairment—A review of the evidence and causal mechanisms. Ageing Res Rev [Internet]. 2013. September [cited 2019 Feb 19];12(4):840–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23831959 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. Long-Term Care Facility Resident Assessment Instrument 3.0 User’s Manual, Version 1.14. 2016.
- 18.Kaehr E, Visvanathan R, Malmstrom TK, Morley JE. Frailty in nursing homes: The FRAIL-NH scale. Journal of the American Medical Directors Association [Internet]. 2015. February 1 [cited 2019 Feb 24];16(2):87–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25556303 [DOI] [PubMed] [Google Scholar]
- 19.Theou O, Sluggett JK, Bell JS, Lalic S, Cooper T, Robson L, et al. Frailty, Hospitalization, and Mortality in Residential Aged Care. Journals Gerontol Ser A [Internet]. 2018. July 9 [cited 2019 Mar 13];73(8):1090–6. Available from: https://academic.oup.com/biomedgerontology/article/73/8/1090/4372242 [DOI] [PubMed] [Google Scholar]
- 20.Luo H, Lum TYS, Wong GHY, Kwan JSK, Tang JYM, Chi I. Predicting Adverse Health Outcomes in Nursing Homes: A 9-Year Longitudinal Study and Development of the FRAIL-Minimum Data Set (MDS) Quick Screening Tool. J Am Med Dir Assoc [Internet]. 2015. December 1 [cited 2019 Mar 16];16(12):1042–7. Available from: https://www.sciencedirect.com/science/article/pii/S1525861015006064?via%3Dihub [DOI] [PubMed] [Google Scholar]
- 21.Kaehr EW, Pape LC, Malmstrom TK, Morley JE. FRAIL-NH predicts outcomes in long term care. J Nutr Health Aging [Internet]. 2016. February 11 [cited 2019 Feb 20];20(2):192–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26812516 [DOI] [PubMed] [Google Scholar]
- 22.Theou O, Tan ECK, Bell JS, Emery T, Robson L, Morley JE, et al. Frailty Levels in Residential Aged Care Facilities Measured Using the Frailty Index and FRAIL-NH Scale. J Am Geriatr Soc [Internet]. 2016. November [cited 2019 Feb 19];64(11):e207–12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27783396 [DOI] [PubMed] [Google Scholar]
- 23.De Silva TR, Theou O, Vellas B, Cesari M, Visvanathan R. Frailty Screening (FRAIL-NH) and Mortality in French Nursing Homes: Results From the Incidence of Pneumonia and Related Consequences in Nursing Home Residents Study. J Am Med Dir Assoc [Internet]. 2018. May 1 [cited 2019 Mar 16];19(5):411–4. Available from: https://www.sciencedirect.com/science/article/pii/S1525861017307879?via%3Dihub [DOI] [PubMed] [Google Scholar]
- 24.Yang M, Zhuo Y, Hu X, Xie L. Predictive validity of two frailty tools for mortality in Chinese nursing home residents: frailty index based on common laboratory tests (FI-Lab) versus FRAIL-NH. Aging Clin Exp Res [Internet]. 2018. December 26 [cited 2019 Mar 16];30(12):1445–52. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30259498 [DOI] [PubMed] [Google Scholar]
- 25.Buckinx F, Croisier J-L, Reginster J-Y, Lenaerts C, Brunois T, Rygaert X, et al. Prediction of the Incidence of Falls and Deaths Among Elderly Nursing Home Residents: The SENIOR Study. J Am Med Dir Assoc [Internet]. 2018. January 1 [cited 2019 Mar 16];19(1):18–24. Available from: https://www.sciencedirect.com/science/article/pii/S1525861017303572?via%3Dihub [DOI] [PubMed] [Google Scholar]
- 26.Saliba D, Buchanan J, Edelen MO, Streim J, Ouslander J, Berlowitz D, et al. MDS 3.0: Brief Interview for Mental Status. J Am Med Dir Assoc [Internet]. 2012. September [cited 2019 Apr 6]; 13(7):611–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22796362 [DOI] [PubMed] [Google Scholar]
- 27.Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, et al. MDS Cognitive Performance Scale. J Gerontol [Internet]. 1994. July [cited 2019 Apr 6];49(4):M174–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8014392 [DOI] [PubMed] [Google Scholar]
- 28.Gao X, Schwartz TA, Preisser JS, Perin J. GEEORD: A SAS macro for analyzing ordinal response variables with repeated measures through proportional odds, partial proportional odds, or non-proportional odds models. Comput Methods Programs Biomed. 2017. October 1;150:23–30. [DOI] [PubMed] [Google Scholar]
- 29.Wickham H ggplot2: Elegant Graphics for Data Analysis. New York, NY: Springer-Verlag; 2016. [Google Scholar]
- 30.Cadore EL, Casas-Herrero A, Zambom-Ferraresi F, Idoate F, Millor N, Gomez M, et al. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age (Dordr) [Internet]. 2014. April [cited 2019 Mar 18];36(2):773–85. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24030238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee PH, Lee YS, Chan DC. Interventions targeting geriatric frailty: A systemic review [Internet]. Vol. 3, Journal of Clinical Gerontology and Geriatrics. No longer published by Elsevier; 2012. [cited 2019 Feb 24]. p. 47–52. Available from: https://www.sciencedirect.com/science/article/pii/S2210833512000238 [Google Scholar]
- 32.Apóstolo J, Cooke R, Bobrowicz-Campos E, Santana S, Marcucci M, Cano A, et al. Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults: a systematic review. JBI database Syst Rev Implement reports [Internet]. 2018. January [cited 2019 Feb 18];16(1):140–232. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29324562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laf fon de Mazieres C, Morley JE, Levy C, Agenes F, Barbagallo M, Cesari M, et al. Prevention of Functional Decline by Reframing the Role of Nursing Homes? J Am Med Dir Assoc. 2017. February 1;18(2):105–10. [DOI] [PubMed] [Google Scholar]
- 34.Panza F, Lozupone M, Solfrizzi V, Sardone R, Dibello V, Di Lena L, et al. Different Cognitive Frailty Models and Health- and Cognitive-related Outcomes in Older Age: From Epidemiology to Prevention. Perry G, Avila J, Tabaton M, Zhu X, editors. J Alzheimer’s Dis [Internet]. 2018. March 13 [cited 2019 Mar 13];62(3):993–1012. Available from: http://www.medra.org/servlet/aliasResolver?alias=iospress&doi=10.3233/JAD-170963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buchman AS, Yu L, Wilson RS, Boyle PA, Schneider JA, Bennett DA. Brain pathology contributes to simultaneous change in physical frailty and cognition in old age. J Gerontol A Biol Sci Med Sci [Internet]. 2014. December [cited 2019 Mar 19];69(12):1536–44. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25136002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kelaiditi E, Cesari M, Canevelli M, Abellan van Kan G, Ousset P-J, Gillette-Guyonnet S, et al. Cognitive frailty: Rational and definition from an (I.A.N.A./I.A.G.G.) International Consensus Group. J Nutr Health Aging [Internet]. 2013. November 14 [cited 2019 Apr 2];17(9):726–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24154642 [DOI] [PubMed] [Google Scholar]
- 37.Del Brutto OH, Mera RM, Zambrano M, Sedler MJ. Influence of Frailty on Cognitive Decline: A Population-Based Cohort Study in Rural Ecuador. J Am Med Dir Assoc [Internet]. 2019. February 1 [cited 2019 Feb 23];20(2):213–6. Available from: https://www.sciencedirect.com/science/article/pii/S1525861018305346 [DOI] [PubMed] [Google Scholar]
- 38.Mitnitski A, Fallah N, Rockwood K. A Multistate Model of Cognitive Dynamics in Relation to Frailty in Older Adults. Ann Epidemiol [Internet]. 2011. July 1 [cited 2019 Feb 24];21(7):507–16. Available from: https://www.sciencedirect.com/science/article/pii/S1047279711000275 [DOI] [PubMed] [Google Scholar]
- 39.Samper-Ternent R, Al Snih S, Raji MA, Markides KS, Ottenbacher KJ. Relationship Between Frailty and Cognitive Decline in Older Mexican Americans. J Am Geriatr Soc [Internet]. 2008. October 1 [cited 2019 Feb 24];56(10):1845–52. Available from: http://doi.wiley.com/10.1111/j.1532-5415.2008.01947.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Auyeung TW, Lee JSW, Kwok T, Woo J. Physical frailty predicts future cognitive decline — A four-year prospective study in 2737 cognitively normal older adults. J Nutr Health Aging [Internet]. 2011. October 10 [cited 2019 Feb 24];15(8):690–4. Available from: http://link.springer.com/10.1007/s12603-011-0110-9 [DOI] [PubMed] [Google Scholar]
- 41.Doba N, Tokuda Y, Goldstein NE, Kushiro T, Hinohara S. A pilot trial to predict frailty syndrome: The Japanese Health Research Volunteer Study. Exp Gerontol [Internet]. 2012. August 1 [cited 2019 Feb 19];47(8):638–43. Available from: https://www.sciencedirect.com/science/article/pii/S0531556512001416 [DOI] [PubMed] [Google Scholar]
- 42.Raji MA, Al Snih S, Ostir G V., Markides KS, Ottenbacher KJ. Cognitive Status and Future Risk of Frailty in Older Mexican Americans. Journals Gerontol Ser A Biol Sci Med Sci [Internet]. 2010. November 1 [cited 2019 Feb 19];65A(11):1228–34. Available from: https://academic.oup.com/biomedgerontology/article-lookup/doi/10.1093/gerona/glq121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aranda MP, Ray LA, Snih S Al, Ottenbacher KJ, Markides KS. The Protective Effect of Neighborhood Composition on Increasing Frailty Among Older Mexican Americans. Whitfield K, Angel JL, Wong R, editors. J Aging Health [Internet]. 2011. October 23 [cited 2019 Feb 19];23(7):1189–217. Available from: http://journals.sagepub.com/doi/10.1177/0898264311421961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gross AL, Xue QL, Bandeen-Roche K, Fried LP, Varadhan R, McAdams-DeMarco MA, et al. Declines and impairment in executive function predict onset of physical frailty. Journals Gerontol - Ser A Biol Sci Med Sci [Internet]. 2016. [cited 2019 Mar 19];71(12):1624–30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27084314 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


