Abstract
Background:
Despite evidence of benefit after injury, helicopter emergency medical services (HEMS) overtriage (OT) remains high. Scene and transfer OT are distinct processes. Our objectives were to identify geographic variation in overtriage, patient-level predictors, and determine if overtriage impacts population-level outcomes.
Methods:
Patients ≥16 undergoing scene or interfacility HEMS in the Pennsylvania Trauma Outcomes Study were included. Overtriage was defined as discharge within 24hr of arrival. Patients were mapped to zip code and rates of OT were calculated. Hot spot analysis identified regions of high and low OT. Mixed effects logistic regression determined patient predictors of OT. High and low OT regions were compared for population-level injury fatality rates. Analyses were performed for scene and transfer patients separately.
Results:
85,572 patients were included (37.4% transfers). OT was 5.5% among scene and 11.8% among transfer HEMS (p<0.01). Hot spot analysis demonstrated geographic variation in high and low OT for scene and transfer patients. For scene patients, OT was associated with distance (OR 1.03; 95%CI 1.01–1.06 per 10mi, p=0.04), neck injury (OR 1.27; 95%CI 1.01–1.60, p=0.04), and single-system injury (OR 1.37; 95%CI 1.15–1.64, p<0.01). For transfer patients, OT was associated with rurality (OR 1.64; 95%CI 1.22–2.21, p<0.01), facial injury (OR 1.22; 95%CI 1.03–1.44, p=0.02), and single-system injury (OR 1.35; 95%CI 1.18–2.19, p<0.01). For scene patients, high OT was associated with higher injury fatality rate (coeff 1.72; 95%CI 1.68, 1.76, p<0.01); low OT was associated with lower injury fatality rate (coeff −0.73; 95%CI −0.78, −0.68, p<0.01). For transfer patients, high OT was not associated with injury fatality rate (p=0.53); low OT was associated with lower injury fatality rate (coeff −2.87; 95%CI −4.59, −1.16, p<0.01).
Conclusions
Geographic OT rates vary significantly for scene and transfer HEMS and are associated with population-level outcomes. These findings can help guide targeted performance improvement initiatives to reduce HEMS overtriage.
Level of Evidence:
Epidemiological, Level IV
Keywords: Helicopter, Triage, Prehospital, Geographic, Emergency medical services
BACKGROUND
Helicopter emergency medical services (HEMS) are an integral part of trauma systems and associated with improved survival after injury when compared to ground transport.1–4 Although guidelines and a predictive HEMS triage score have been developed to assist prehospital providers in determining the need for helicopter transport5–9, widespread adoption of these tools is limited which contributes to significant practice variation.
While severely injured patients may require the resources of a trauma center, not all severely injured patients require the use of HEMS transport. Misallocation results in unnecessary helicopter transport for many patients, driving up HEMS overtriage. Several definitions of HEMS overtriage exist in the literature; one of the most telling is that up to 25% of HEMS patients are discharged within 24 hours of their helicopter ride.1, 10–12 HEMS is expensive to healthcare systems and individual patients when balance billing is practiced, and it carries a higher crash risk than ground transport.13–17 Despite the fact that there are currently over 1,100 medical transport helicopters in the United States,18 they are a scare resource as each helicopter must cover a defined geographic catchment area. Coupled with the fact that up to 27% of the US population is dependent on HEMS transport to access a trauma center within one hour of injury,19 high HEMS overtriage may preclude air transport availability to patients that truly need it. Thus, we must be cognizant of the implications of HEMS overtriage for trauma systems and patient outcomes.
HEMS transport is used for direct scene response as well as interfacility transfer after injury. In efforts to evaluate helicopter resource utilization and issues of overtriage, it is imperative to consider these scenarios independently. Direct scene transport reflects EMS decision-making but interfacility transfer reflects physician decision-making after evaluation in a hospital. Ultimately, strategies to mitigate scene and interfacility HEMS overtriage require different approaches given this distinction. Additionally, multiple local factors such as trauma center, ground ambulance, and helicopter resource accessibility, rurality, and traffic congestion will lead to geographic variation in scene and interfacility HEMS overtriage.19, 20 Identifying regions with higher overtriage rates can guide targeted quality improvement initiatives directed at specific scene or interfacility HEMS overtriage, as some have shown performance improvement programs reduce HEMS overtriage at a regional level.12
Our objectives were first, to identify geographic variation in HEMS overtriage for scene and interfacility transfer patients, and second, to identify patient-level factors associated with HEMS overtriage. We also sought to establish the clinical importance of HEMS overtriage by evaluating whether geographic variation in HEMS overtriage correlates with population-level injury mortality. We hypothesized that HEMS overtriage has significant geographic variation and differs by scene versus interfacility transfer; and that high HEMS overtriage is associated with increased population level injury fatality.
METHODS
Study Design & Population
We conducted a retrospective analysis of all patients 16 years and older from the Pennsylvania Trauma Outcomes Study (PTOS) registry inclusive of years 2000–2017. Patients were included if transported by HEMS from the scene of injury or as an interfacility transfer. Patients who sustained burn injury or were dead on arrival were excluded from analysis. Demographics, injury severity, prehospital and admission vital signs, International Classification of Diseases (ICD) 9th revision diagnoses codes, patient disposition and outcomes were abstracted for each patient.
Outcomes
The primary outcome measure was HEMS overtriage. This was defined for patients that were transported by helicopter, either direct from the scene of injury or from a referring hospital, to the trauma center and were subsequently discharged from the ED or within 24 hours of admission. Our secondary outcome was population level injury fatality rate. Age-adjusted injury fatality rates from 2008–2014 were obtained from the Centers for Disease Control (CDC) Web-based Injury Statistics Query and Reporting System for each county in Pennsylvania.21
Geospatial Analysis
The location of each patient in the PTOS dataset was assigned to the zip code of residence in geographic information system mapping software. We then calculated the HEMS overtriage rate as the number of patients overtriaged per 100 HEMS patients in every zip code for Pennsylvania. A hotspot analysis was performed separately for scene and interfacility transfer HEMS overtriage rates. Hot spot analysis identifies areas of spatially clustered high and low outcome values. This technique calculated the Getis-Ord Gi* statistic for each HEMS patient in the dataset. The Gi* statistic is a z-score that evaluates the outcome values for each feature within the context of the outcome values of neighboring features.22 The outcome values in a local area must be significantly higher (hot spot) or lower (cold spot) than would be expected if the outcome was randomly distributed geographically. Based on the Gi* statistic, p-values are calculated, with hot and cold spots identified at the 99%, 95%, and 90% confidence levels. This technique allows identification of spatially clustered areas of high or low HEMS overtriage rates compared to non-outlier areas.
Because we utilized data over a long time period, we also performed hot spot analysis for three time periods (2000–2006, 2007–2014, 2015–2017) to evaluate for potential temporal changes in HEMS overtriage for interfacility or scene transports.
To assess population injury fatality rates, which were available from the CDC at the county level, we then spatially joined hot and cold spot zip codes of counties to create contiguous county regions of Pennsylvania representing non-outliers, hot spots, and cold spots for HEMS overtriage. This, again, was performed separately for scene and interfacility HEMS transports. Geospatial analysis was performed using ArcGIS v10.8 (ESRI; Redlands, CA).
Statistical Analysis
Multivariable logistic regression modeling was used to test the association of patient and system level factors with HEMS overtriage. Analyses were performed separately for direct scene and interfacility transfer patients. Models adjusted for confounding factors including age, rurality, prehospital time and distance, injury time of day to account for traffic congestion (rush hour [defined as weekdays 6a-10a & 3p-7p]23 versus non-rush hour), prehospital hemodynamics, mechanism of injury, and measures of injured body region by abbreviated injury scales (AIS). Models for interfacility transfer were also adjusted for hemodynamics at the referring facility and time spent at the referring facility. Robust variance sandwich estimators were used to account for clustering at the center level.
Multivariable linear regression was used to test the association of hot and cold spot regions with county level injury fatality rates. Models were adjusted for rurality, mean county ISS, mean county prehospital systolic blood pressure, proportion of HEMS transport in the county, and trauma system resource density (trauma center, ground ambulance, and HEMS base densities per 100 square miles and per 100,000 population within the county).
Continuous and categorical data are reported as median (interquartile range) and frequency (percentage), respectively. For univariate comparisons, Mann-Whitney U tests were used for nonparametric continuous variables and Chi-square tests were used for categorical variables. Logistic regression models are reported as adjusted odds ratio (aOR) and 95% confidence intervals (95% CI). Linear regression models are reported as adjusted coefficients and 95% CI. Reported p-values were 2-tailed, and a p-value <0.05 was considered statistically significant. All analyses were performed using Stata version 15MP (StataCorps LP, College Station, TX).
RESULTS
We analyzed 85,752 patients transported by HEMS; of which 53,541 (62.6%) were direct scene transports and 32,031 (37.4%) were transferred from a referring hospital. Patients that underwent direct scene HEMS transport were younger, more frequently had multisystem trauma (Table 1). Interfacility transfer patients were more commonly injured in a rural setting and had greater transport distance and prehospital time. More than 50% of scene HEMS patients and nearly 60% of interfacility HEMS patients had an ISS ≤15. In the overall cohort, interfacility transfer patients experienced more than a doubling in HEMS patients discharged within 24 hours (11.8% vs 5.5%, p<0.001) but no difference in unadjusted mortality. For scene HEMS patients, between 25–31% of patients met National Field Triage Guidelines (NFTG) step 1 (physiologic) or step 2 (anatomic) criteria indicating the need for transport to the highest-level trauma center, but only 26% of these patients scored ≥2 on the validated air medical prehospital triage (AMPT) score indicating a potential survival benefit for HEMS transport (Table 2).
Table 1.
Patient Demographics, Injury Characteristics and Outcomes: Direct Scene vs. Interfacility Transfer HEMS
| Scene HEMS (n=53,541) | Interfacility HEMS (n=32,031) | p-value | |
|---|---|---|---|
| Age | 41 (25, 57) | 50 (31, 71) | <0.001 |
| Sex (male) | 37433 (69.9%) | 21563 (67.3%) | <0.001 |
| ISS | 14 (9, 24) | 13 (8, 21) | <0.001 |
| ISS ≤15 | 28401 (53.4%) | 18102 (57.0%) | <0.001 |
| AIS ≥3 (any system) | 38025 (71.0%) | 22210 (69.3%) | <0.001 |
| Multisystem trauma* | 4907 (9.2%) | 1370 (4.3%) | <0.001 |
| Rural injury | 26578 (54.7%) | 15709 (65.5%) | <0.001 |
| Distance (miles) | 25.7 (17.3, 36.7) | 40.8 (25.2, 64.6) | <0.001 |
| Prehospital time (mins) | 52 (42, 63) | 214 (150, 292) | <0.001 |
| HEMS overtriage | 2962 (5.5%) | 3795 (11.8%) | <0.001 |
| Mortality | 4692 (8.8%) | 2745 (8.6%) | 0.330 |
Continuous variables presented as median (IQR)
Categorical variables presented as n (%)
ISS, injury severity score; AIS, abbreviated injury score; HEMS, helicopter emergency medical services.
Three or more anatomic body regions injured
Table 2.
National Field Triage Guidelines Physiologic & Anatomic Criteria for Scene HEMS Transport
| Scene HEMS (n=53,541) | |
|---|---|
| GCS | 15 (12, 15) |
| SBP | 134 (118, 150) |
| RR | 18 (16, 20) |
| Penetrating injury | 2985 (5.6%) |
| Flail chest | 918 (1.7%) |
| Open skull fracture | 1304 (2.4%) |
| ≥2 Long bone fractures | 1898 (3.5%) |
| Pelvic fracture | 6832 (12.8%) |
| Crush injury | 246 (0.5%) |
| Amputation | 350 (0.7%) |
| Paralysis | 632 (1.2%) |
| Any step 1 PHY criteria | 16340 (30.5%) |
| Any step 2 ANA criteria | 13454 (25.1%) |
| AMPT Score ≥2 | 11351 (25.7%) |
Continuous variables presented as median (IQR)
Categorical variables presented as n (%)
HEMS, helicopter emergency medical services; GCS, Glasgow coma scale; SBP, systolic blood pressure; RR, respiratory rate; PHY, physiologic; ANA, anatomic; AMPT, air medical prehospital triage Score: GCS <14: 1 point, RR <10/>29: 1 point, Flail chest: 1 point, Suspected hemothorax/pneumothorax: 1 point, Paralysis: 1 point, Multisystem trauma: 1 point, Any one physiologic NFTG criterion plus any one anatomic criterion: 2 points (Consider helicopter transport if AMPT ≥2)
The most frequent mechanism of injury for direct scene transports was MVC (43.6%), and for interfacility transfer, MVC and fall from height were most common (25.1% and 25.8%, respectively). For HEMS patients discharged within 24 hours of admission (overtriage), again MVC was the most common mechanism. For interfacility HEMS transfers, the proportion of penetrating injuries that resulted in overtriage was 20.2%.
Geographic Variation of HEMS Overtriage
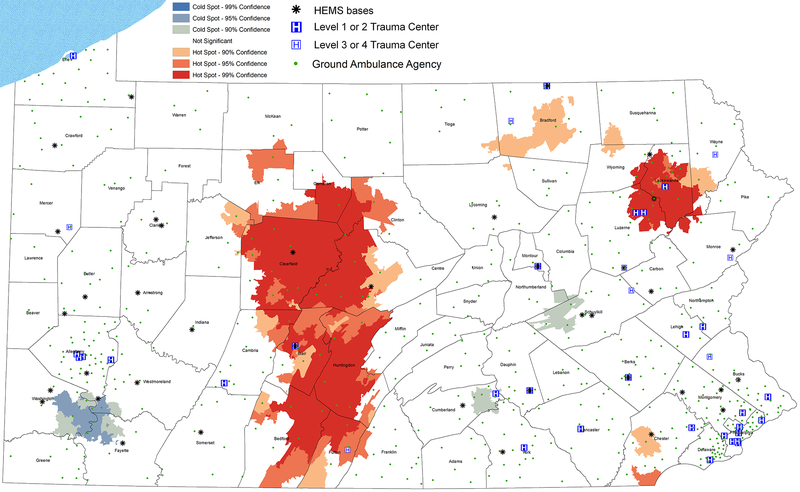
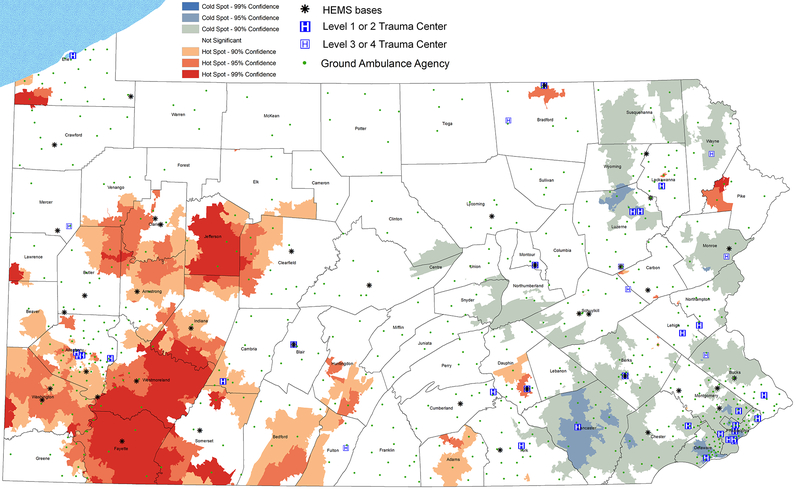
For direct scene transports, hot-spot analysis identified geospatial clusters of high HEMS overtriage rates (hot spots) in central and northeast Pennsylvania, and a cluster of low HEMS overtriage rates (cold spots) in southwest Pennsylvania (Figure 1). With review of time-lapse mapping (Supplemental Digital Content, eFigures 1–3), we discovered some variation with the northeast hot spot, but a predominance of the central region high overtriage persisted, which notably reflects a rural region of the state. A cold spot persisted in the southwestern region of the state. In contrast, for interfacility transfer HEMS, there was a predominant hot spot in the southwest region of the state (Figure 2), with minimal variation observed over the study period (Supplemental Digital Content, eFigures 4–6). Interestingly, this interfacility HEMS overtriage hot spot geographically overlaps with the major scene HEMS overtriage cold spot. An interfacility HEMS transfer cold spot along the eastern portion of the state predominated.
Figure 1: Geospatial Hot Spot Analysis—Scene Transport.
Hot spot analysis identifies areas of spatially clustered high and low HEMS overtriage values with hot and cold spots identified at the 99%, 95%, and 90% confidence levels as compared to non-outlier areas
Figure 2: Geospatial Hot Spot Analysis—Interfacility Transfers.
Hot spot analysis identifies areas of spatially clustered high and low HEMS overtriage values with hot and cold spots identified at the 99%, 95%, and 90% confidence levels as compared to non-outlier areas
Patient-level Factors
Intuitively, for scene transports, overtriage was associated with increased distance from a trauma center with a 3% per 10-mile increase in the odds of overtriage (aOR 1.03; 95%CI 1.01–1.06 per 10mi, p=0.04). Other independent predictors of overtriage included isolated neck injury with 27% increased odds of overtriage, (aOR 1.27; 95%CI 1.01–1.60, p=0.04), and single system injury with 37% increased odds (aOR 1.37; 95%CI 1.15–1.64, p<0.01).
For interfacility transfer, patients injured in a rural setting experienced 64% increased odds of overtriage (aOR 1.64; 95%CI 1.22–2.21, p<0.01). Patients with isolated facial injury had a 21% increase in odds of overtriage (aOR 1.21; 95%CI 1.03–1.43, p=0.02). Similar to scene transport patients, those with single system injuries experienced 35% increased odds of overtriage (aOR 1.35; 95%CI 1.18–1.54, p<0.01).
Population-level Mortality
The population mortality rate for non-outlier regions of Pennsylvania (non-hot or cold spots) was 11.6 deaths per 100,000 population. For scene transports, counties designated as HEMS overtriage hot spots were associated with 2 deaths higher per 100,000 persons compared to non-outlier regions (coefficient 1.72; 95%CI 1.68, 1.76, p<0.01). Counties designated as HEMS overtriage cold spots were associated with nearly 1 death fewer per 100,000 persons lower compared to non-outlier regions (coefficient −0.73; 95%CI −0.78, −0.68, p<0.01).
For interfacility transfers, counties designated as HEMS overtriage hot spots were not associated with injury fatality rate (coefficient −0.75; 95%CI −3.12, 1.62, p=0.53). Counties designated as HEMS overtriage cold spots were associated with nearly 3 deaths fewer per 100,000 persons compared to non-outlier regions (coefficient −2.87; 95%CI −4.59, −1.16, p<0.01).
DISCUSSION
We found significant geographic variation in HEMS overtriage across Pennsylvania for both scene and interfacility transports in disparate regions. Overall, HEMS overtriage was greater for interfacility transfer than scene transports. For scene transports, HEMS overtriage was greatest in central, rural regions of the state whereas interfacility HEMS overtriage was greatest in southwestern Pennsylvania, notably in regions of closer proximity to multiple trauma centers. Unique patient level factors were associated with HEMS overtriage for scene and interfacility transfers. These included isolated neck injuries for scene transports and isolated facial injuries for interfacility transfers. Single body system injuries were associated with HEMS overtriage for both means of transport. Regions of high scene HEMS overtriage experienced a significant increase in adjusted population injury fatality, while regions of low scene HEMS overtriage experienced a decrease in population mortality. Regions of low interfacility HEMS overtriage experienced a decrease in adjusted population injury fatality.
HEMS transport improves survival for injured patients, however distinguishing which patients require this mode of transport to provide for this benefit remains a challenge and the incidence of HEMS use for nonlife-threatening injuries is high.10 The mortality benefit is likely driven by multiple potential mechanisms and varies by patient. Thus, understanding why a patient may benefit from HEMS will facilitate better triage for HEMS and assist in establishing benchmarks for over- and undertriage rates for HEMS transport. The American College of Surgeons Committee on Trauma (ACS-COT) has established benchmarks for trauma center overtriage of 25–35% to maintain undertriage of 1–5%; however, no such benchmarks exist for HEMS transport.24 These are fundamentally different questions as many patients requiring trauma center evaluation and care do not need to fly there. Applying these geospatial techniques on a regional level can help trauma systems establish local HEMS over- and undertriage benchmarks, as well as targets for HEMS performance improvement, which the ACS-COT does call for.
For some with time-sensitive injuries, HEMS provides the quickest route to definitive care. For others, the mortality benefit is likely due to the advanced capabilities and experience provided by HEMS crews.25 The NFTG indicate trauma center need, but do not provide direction for who requires HEMS. Guidelines for HEMS have previously been published but are supported by limited evidence and extrapolate existing triage criteria for HEMS triage. This lack of specificity to patients who truly need HEMS contributes to the ongoing high overtriage rates.8, 9 The American College of Surgeons Committee on Trauma previously put out a call to investigate, improve and standardize HEMS utilization nationwide.7
Overtriage is common in HEMS for trauma across multiple definitions. Prior work shows between 15% and 25% of HEMS patients are discharged from the emergency room or within 24 hours of admission.1, 10–12 In the present study, we found lower overtriage rates overall, but when assessing regional variability, some areas had even higher rates than this. When looking at injury severity, 36% to 60% of HEMS patients have minor injuries defined by an ISS <15 or AIS <3, similar to our findings of more than half of HEMS transports with an ISS<15.1, 10, 16, 26 This means that up to one in four patients are discharged home the same day they arrived by helicopter, and even more have minor injuries that do not require or benefit from HEMS.
In a retrospective analysis, Madiraju et al11 reported on overtriage rates during a five-year study period. Twenty-eight percent of patients were transported by HEMS with 18% of those patients discharged from the ED. When the authors included medical admission with no significant injuries or observation status admissions, overtriage exceeded 50%. The authors estimated this HEMS overtriage to cost $1.3 million in their system. Another study utilizing the National Trauma Databank to look at HEMS overtriage nationally, defining overtriage as transport of minor injuries (AIS <3). They found a 36% HEMS overtriage rate, with uninsured status and penetrating injuries associated with HEMS overtriage. They also demonstrated variation in overtriage by US census region and annual trauma volume patterns.26
Although the rationale for HEMS use in these scenarios may seem reasonable for some, it is unlikely that the providers recognize the consequences of this decision when patients do not truly require this resource. The impact of overtriage regarding risk of transport, cost, and of resource utilization is felt by the patient, the medical team, and severely injured patients in need of this resource. First, HEMS transport carries significant risk. Accidents are increasing with 120 deaths and 146 serious injuries in 139 helicopter crashes in the last decade.27 This is twice the fatality rate per mile traveled when compared to ground ambulances.15 Transport is the only medical intervention that risks the providers’ lives and HEMS is the riskiest form of patient transport. Survivors of HEMS crashes frequently have lasting physical, psychologic, and financial burdens.28 Second, HEMS is a costly resource, at a median of $10,199 per flight.29 Beyond this, there is an alarming trend of shifting costs to individual patients. Up to 73% of HEMS agencies are out-of-network which leads to balance billing of patients to an average of $21,698; putting them at risk for bankruptcy.30 Finally, despite the number of helicopters across the United States, each covers a distinct geographic area. When the helicopter is on a mission, particularly one that does not benefit a patient, a second helicopter may not be available for patients that would actually benefit from them. This has been shown to increase mortality, morbidity, and time delays to definitive care.31–33
Given these consequences and the adverse impact on injury outcomes it is critical we address the overutilization of HEMS. There have been some efforts to reduce HEMS overtriage taken from multiple perspectives. Brown et al5, 6 developed the air medical prehospital transport (AMPT) score as a triage tool to identify patients at the scene of injury that would derive a mortality benefit with HEMS versus ground transport. Importantly, they utilized the existing NFTG criteria to ensure that this would pragmatically fit within the prehospital workflow. This tool was externally validated but wide-spread implementation is limited. Our data shows only 26% of scene patients met AMPT score criteria yet were transported by HEMS. Incorporation of HEMS triage criteria such as the AMPT score into transport guidelines may help standardize HEMS use and reduce overtriage.
Wormer et al 12 demonstrated the implementation of a Trauma Advisory Committee as part of a performance improvement agenda successfully reduced HEMS overtriage regionally. In this study, quarterly meetings were held with EMS agencies to review specific HEMS overtriage cases over a five-year period. A continual reduction in HEMS overtriage was observed over the entire study period as compared to surrounding, non-participating EMS agencies, demonstrating the efficacy of education and performance improvement initiatives to mitigate HEMS overtriage. Thus, it is possible to address this overtriage on a system level.
Our findings also highlight the importance of distinguishing scene and interfacility overtriage. Overall, interfacility transfers have higher overtriage in Pennsylvania than scene transports. The initiatives to improve overtriage in these settings will be different. The evidence noted above is targeted towards scene overtriage which is a function of EMS and first responder decision making, largely dependent on system protocols and limited diagnostic and patient information. Conversely, interfacility transfer overtriage initiatives will need to target physician decision making and behavior in a setting with much greater diagnostic capabilities and resources.
Unique patient-level factors were associated with HEMS overtriage from the scene and interfacility transfers. Similarly, these likely represent differences in the HEMS triage process in scene and interfacility transfer. Intuitively, for scene transports, increased distance from a trauma center was associated with overtriage. Isolated neck and single body system injuries were also associated with scene HEMS overtriage. Prior literature suggests that the EMS transport decision is often based on dispatch information, initial gestalt of scene severity and with the greatest emphasis on proximity to the trauma center.34, 35 Neck injuries can rapidly result in a life threatening situation given the relative proximity of vascular and airway structures, likely leading ground EMS providers to employ HEMS for neck injuries. Despite limited anatomic injuries as indicated by the single-body system association with overtriage, it is apparent in our study that distance from the nearest trauma center also dictates the decision to utilize HEMS.
Rurality, isolated facial injury, and single system injuries were associated with interfacility HEMS overtriage. Given that these patients were discharged within 24 hours (overtriage), we speculate that they likely represent those that have isolated injuries evident after a thorough hospital diagnostic workup, but that require a specialist evaluation that is unavailable at the presenting hospital. Clinically, these might represent the patients with, for example, stable isolated long bone fractures, low grade solid organ injuries, or facial fractures. It is evident that these patients may require evaluation at a trauma center but are unlikely to be so severely injured that they require the expedience and advanced care of HEMS over ground transport. Counter to the relationship we observed with scene EMS, it appears as if physicians were more likely to elect to fly patients for interfacility transfer despite the presence of trauma centers accessible by ground.
Notably, for scene and interfacility transfer, distance from the trauma center and rurality were associated with increased overtriage. From a logistical standpoint it is important to recognize an important factor in transport decisions for rural hospitals and those far from a trauma center may be limited ground ambulance resources independent of patient injury severity. Prolonged transport of a patient to a distant trauma center would render the catchment area for that ground transport system vulnerable to not only other injuries but any emergency call that may come in while the ambulance is unavailable transporting a patient to the trauma center. Thus, despite the absence of severe time-sensitive injuries, some patients with trauma center need but not necessarily helicopter need will be flown for logistical reasons to ensure resource availability for the region. Under these circumstances, this would not necessarily be an inappropriate use of HEMS resources even if the patient were discharged within 24 hours given system resource constraints. This actually highlights the utility of our geospatial approach to identify outlier overtriage areas, allowing a more tailored approach to potential underlying reasons. Thus, trauma system leaders can parse out areas with higher HEMS over-triage due to poor ground ambulance coverage and evaluate potential system-level solutions, while also identifying HEMS transports of low utility despite adequate system resources that could improve with educational initiatives. Given the limitation of not knowing the rationale for transport decision, we did adjust for availability of ground and air ambulances per area and population to account for system EMS resource availability.
Our data also highlights the importance of measuring regional variation. There were disparate regions of high overtriage when considering scene versus interfacility transfer. In fact, southwestern Pennsylvania had lower than average scene overtriage but higher than average interfacility overtriage. This is critical to allow targeting the appropriate EMS agencies and referring hospitals with the right type of approach to maximize impact. If trying to implement performance improvement initiatives to reduce HEMS overtriage in areas of already lower than average overtriage, one may erroneously conclude the initiative is ineffective and a waste of valuable resources. This is particularly highlighted by the low overall scene HEMS triage rate in the state while some regions are well in excess of previously published overtriage rates. Performance improvement initiatives should be tailored by geographic region and differentiated on EMS (scene) versus physician (interfacility) overtriage disparities. A similar approach could be generalized nationally to reduce HEMS overtriage.
Importantly, we were able to quantify the impact of high overtriage rates on population outcomes in the corresponding regions. Scene HEMS overtriage hot spots were associated with increased injury fatality rates which may represent the strain on a limited HEMS resource and resultant unavailable or delayed care for severely injured patients. For interfacility transfers, HEMS hot spots were not associated with increased injury fatality. This is possibly explained by the fact that injured hospital inpatients were protected by hospital management but injured scene patients in this region were actually in a scene HEMS cold spot allowing for increased field availability and response by helicopter. In contrast, HEMS interfacility transfer cold spots regions did experience an association with decreased injury fatality perhaps indicating increased HEMS availability for other patients. Certainly, the above or below average HEMS overtriage rates do not solely explain the variation in population injury fatality rates but may yet be important markers of variation in care that impacts population outcomes after injury and warrants ongoing investigation.
Our study has important limitations to acknowledge. This is a retrospective study with pre-determined variables available for analysis and not initially intended to address our clinical question. Specifically, the reason for EMS or physician transport decision was not available to us. This knowledge would elucidate clinical judgement (e.g. transporting minor injuries by helicopter) from logistical reasons for transport (e.g. unavailability of ground ambulance). Additionally, referring hospital and trauma centers are de-identified within the database and therefore prevent evaluation of potential hospital network influences upon transport decision making. Understanding this decision-making process in the field and at referring hospitals is central to designing improvement initiatives and would help direct educational efforts. Our observed scene HEMS overtriage rate was lower than other published data. This is likely due to the marked geographic disparities in overtriage rates, with hotspot regions demonstrating overtriage rates exceeding that of prior works, and thus emphasizing the need for assessment of regional variation prior to the implementation of mitigation efforts. Our definition of overtriage is also more extreme, with discharge from the ED or within 24 hours. There are certainly more patients than those that met our definition that did not ultimately benefit from HEMS transport, even if not discharged within 24 hours. If we utilized ISS <15 as our definition, greater than 50% of patients would have been classified as HEMS overtriage. Additionally, there were changes in local HEMS policies over the course of this study, however, time-lapse analyses were completed to evaluate for any major difference in transport patterns and did not show significant temporal differences. Lastly, for our population injury fatality analyses, we cannot claim causality as these are population level data and not specific to the patient data collected in PTOS, however, we believe that the associations that we observed are informative, hypothesis generating, and warrant ongoing investigation to see if initiatives to reduce HEMS overtriage may also impact population outcomes after injury.
Conclusion
Significant geographic variation exists for HEMS overtriage. Unique patient profiles contribute to transport decisions and overtriage and may be a target for performance improvement. Scene and interfacility transfer HEMS utilization are independent processes with disparate overtriage patterns and require different approaches to address. HEMS overtriage is expensive and with significant risk to the patient, crew, and other injured patients within the HEMS catchment area. HEMS overtriage rates also appear to correlate with population injury fatality rates in Pennsylvania. Taken together, this data should be used to develop a tailored approach to mitigate HEMS overtriage with an emphasis on standardized HEMS triage protocols and performance improvement educational initiatives for both EMS agencies and referring physicians with consideration of regional patterns of HEMS overtriage.
Supplementary Material
Figures 1–3: Geospatial Hot Spot Analysis—Scene Transport, Time-Lapse Over Study Period
Figures 4–6: Geospatial Hot Spot Analysis—Interfacility Transfers, Time-Lapse Over Study Period
Acknowledgments
These data were provided by the Pennsylvania Trauma Systems Foundation, Mechanicsburg, PA. The Foundation specifically disclaims responsibility for any analyses, interpretations, or conclusions.
Support: National Institutes of Health [Grant: 2T32GM008516-26, 2020]
Footnotes
Disclosures
There are no conflicts of interest for the current study
References
- 1.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69:1030–1034; discussion 1034–1036. [DOI] [PubMed] [Google Scholar]
- 2.Galvagno SM Jr., Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ Jr., Baker SP, Bowman SM, Pronovost PJ, Haider AH. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA. 2012;307:1602–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galvagno SM Jr., Sikorski R, Hirshon JM, Floccare D, Stephens C, Beecher D, Thomas S. Helicopter emergency medical services for adults with major trauma. Cochrane Database Syst Rev. 2015:CD009228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivent EE, Faul M, Wald MM. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehosp Emerg Care. 2011;15:295–302. [DOI] [PubMed] [Google Scholar]
- 5.Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Development and Validation of the Air Medical Prehospital Triage Score for Helicopter Transport of Trauma Patients. Ann Surg. 2016;264:378–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. External validation of the Air Medical Prehospital Triage score for identifying trauma patients likely to benefit from scene helicopter transport. J Trauma Acute Care Surg. 2017;82:270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doucet J, Bulger E, Sanddal N, Fallat M, Bromberg W, Gestring M, Emergency Medical System Subcommittee CoTACoS. Appropriate use of helicopter emergency medical services for transport of trauma patients: guidelines from the Emergency Medical System Subcommittee, Committee on Trauma, American College of Surgeons. J Trauma Acute Care Surg. 2013;75:734–741. [DOI] [PubMed] [Google Scholar]
- 8.Thomas SH, Brown KM, Oliver ZJ, Spaite DW, Lawner BJ, Sahni R, Weik TS, Falck-Ytter Y, Wright JL, Lang ES. An Evidence-based Guideline for the air medical transportation of prehospital trauma patients. Prehosp Emerg Care. 2014;18 Suppl 1:35–44. [DOI] [PubMed] [Google Scholar]
- 9.Thomson DP, Thomas SH, Physicians AMSCotNAoE. Guidelines for air medical dispatch. Prehosp Emerg Care. 2003;7:265–271. [DOI] [PubMed] [Google Scholar]
- 10.Bledsoe BE, Wesley AK, Eckstein M, Dunn TM, O’Keefe MF. Helicopter scene transport of trauma patients with nonlife-threatening injuries: a meta-analysis. J Trauma. 2006;60:1257–1265; discussion 1265–1256. [DOI] [PubMed] [Google Scholar]
- 11.Madiraju SK, Catino J, Kokaram C, Genuit T, Bukur M. In by helicopter out by cab: the financial cost of aeromedical overtriage of trauma patients. J Surg Res. 2017;218:261–270. [DOI] [PubMed] [Google Scholar]
- 12.Wormer BA, Fleming GP, Christmas AB, Sing RF, Thomason MH, Huynh T. Improving overtriage of aeromedical transport in trauma: a regional process improvement initiative. J Trauma Acute Care Surg. 2013;75:92–96; discussion 96. [DOI] [PubMed] [Google Scholar]
- 13.Bledsoe BE. Air medical helicopter accidents in the United States: a five-year review. Prehosp Emerg Care. 2003;7:94–98. [DOI] [PubMed] [Google Scholar]
- 14.Bledsoe BE, Smith MG. Medical helicopter accidents in the United States: a 10-year review. J Trauma. 2004;56:1325–1328; discussion 1328–1329. [DOI] [PubMed] [Google Scholar]
- 15.Brown JB, Smith KJ, Gestring ML, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL, Weissman JS. Comparing the Air Medical Prehospital Triage Score With Current Practice for Triage of Injured Patients to Helicopter Emergency Medical Services: A Cost-effectiveness Analysis. JAMA Surg. 2018;153:261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delgado MK, Staudenmayer KL, Wang NE, Spain DA, Weir S, Owens DK, Goldhaber-Fiebert JD. Cost-effectiveness of helicopter versus ground emergency medical services for trauma scene transport in the United States. Ann Emerg Med. 2013;62:351–364 e319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rhee KJ, Holmes EM 3rd, Moecke HP, Thomas FO. A comparison of emergency medical helicopter accident rates in the United States and the Federal Republic of Germany. Aviat Space Environ Med. 1990;61:750–752. [PubMed] [Google Scholar]
- 18.Atlas & Database of Air Medical Services (ADAMS; ). In. vol. 17th, 2019. [Google Scholar]
- 19.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to trauma centers in the United States. JAMA. 2005;293:2626–2633. [DOI] [PubMed] [Google Scholar]
- 20.Chen X, Gestring ML, Rosengart MR, Peitzman AB, Billiar TR, Sperry JL, Brown JB. Logistics of air medical transport: When and where does helicopter transport reduce prehospital time for trauma? J Trauma Acute Care Surg. 2018;85:174–181. [DOI] [PubMed] [Google Scholar]
- 21.Center for Disease Control and Prevention. Injury Prevention and Control: Data and Statistics (WISQARS): Fatal Injury Data. Available at: http://www.cdc.gov/injury/wisqars/fatal.html. Accessed: May 15, 2018.
- 22.Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geographical Analysis. 1992;24:189–206. [Google Scholar]
- 23.Schrank D, Eisele B, Lomax T, Bak J. 2015 Urban Mobility Score Card. In. College Station, Tx: Texas A&M Transportation Institute, 2015. [Google Scholar]
- 24.American College of Surgeons Committee on Trauma. Prehospital Trauma Care. In: Rotondo MF, Cribari C, Smith RS, eds. Resources for the optimal care of the injured patient. Chicago, IL: American College of Surgeons, 2014:23–29. [Google Scholar]
- 25.Chen X, Gestring ML, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL, Brown JB. Speed is not everything: Identifying patients who may benefit from helicopter transport despite faster ground transport. J Trauma Acute Care Surg. 2018;84:549–557. [DOI] [PubMed] [Google Scholar]
- 26.Cheung BH, Delgado MK, Staudenmayer KL. Patient and Trauma Center Characteristics Associated With Helicopter Emergency Medical Services Transport for Patients With Minor Injuries in the United States. Acad Emerg Med. 2014;21:1232–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Habib FA, Shatz D, Habib AI, Bukur M, Puente I, Catino J, Farrington R. Probable cause in helicopter emergency medical services crashes: What role does ownership play? J Trauma Acute Care Surg. 2014;77:989–993. [DOI] [PubMed] [Google Scholar]
- 28.Jaynes CL, Valdez A, Hamilton M, Haugen K, Henry C, Jones P, Werman HA, White LJ. Survivors Perceptions of Recovery following Air Medical Transport Accidents. Prehosp Emerg Care. 2015;19:44–52. [DOI] [PubMed] [Google Scholar]
- 29.Kugel M, Chen H, Forys A. Air Medical Services Cost Study Report. In. Palm Harbor, FL: Association of Air Medical Services, 2017:1–18. [Google Scholar]
- 30.Chhabra KR, McGuire K, Sheetz KH, Scott JW, Nuliyalu U, Ryan AM. Most Patients Undergoing Ground And Air Ambulance Transportation Receive Sizable Out-Of-Network Bills. Health Aff (Millwood). 2020:101377hlthaff201901484. [DOI] [PubMed] [Google Scholar]
- 31.McVey J, Petrie DA, Tallon JM. Air versus ground transport of the major trauma patient: a natural experiment. Prehosp Emerg Care. 2010;14:45–50. [DOI] [PubMed] [Google Scholar]
- 32.Zakariassen E, Osteras O, Nystoyl DS, Breidablik HJ, Solheim E, Brattebo G, Ellensen VS, Hoff JM, Hordnes K, Aksnes A, et al. Loss of life years due to unavailable helicopter emergency medical service: a single base study from a rural area of Norway. Scand J Prim Health Care. 2019;37:233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borst GM, Davies SW, Waibel BH, Leonard KL, Rinehart SM, Newell MA, Goettler CE, Bard MR, Poulin NR, Toschlog EA. When birds can’t fly: an analysis of interfacility ground transport using advanced life support when helicopter emergency medical service is unavailable. J Trauma Acute Care Surg. 2014;77:331–336; discussion 336–337. [DOI] [PubMed] [Google Scholar]
- 34.Deeb AP, Phelos HM, Peitzman AB, Billiar TR, Sperry JL, Brown JB. Disparities in rural versus urban field triage: Risk and mitigating factors for undertriage. J Trauma Acute Care Surg. 2020;89:246–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones CM, Cushman JT, Lerner EB, Fisher SG, Seplaki CL, Veazie PJ, Wasserman EB, Dozier A, Shah MN. Prehospital Trauma Triage Decision-making: A Model of What Happens between the 9–1-1 Call and the Hospital. Prehosp Emerg Care. 2016;20:6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figures 1–3: Geospatial Hot Spot Analysis—Scene Transport, Time-Lapse Over Study Period
Figures 4–6: Geospatial Hot Spot Analysis—Interfacility Transfers, Time-Lapse Over Study Period