Abstract
Objective
Cancer patients are increasingly involved in decision‐making for cancer treatment. General practitioners' (GPs) support in this process is advocated. Therefore, GPs need to be aware of patients' treatment decision‐making process and their potential role. We aim to understand the treatment decision‐making process and to explore the added value of GP involvement, from the perspective of cancer patients treated with curative intent.
Methods
An explorative qualitative study was performed. Semi‐structured interviews were conducted with 20 purposively sampled Dutch cancer patients treated with curative intent.
Results
Patients' treatment decision‐making process was dominated by a focus on ‘safeguarding survival’. Patients generally followed the treatment plan as proposed by their physician and did not always experience having a treatment choice. The majority of patients expressed added value for GP involvement, mainly to provide psychological support, but also for providing shared decision‐making (SDM) support.
Conclusion
The treatment decision‐making process of cancer patients treated with curative intent is dominated by the urge to ‘safeguard survival’. GPs should be aware of their added value in providing psychological support and their potential role to support SDM following a cancer diagnosis.
Keywords: decision‐making, general practice, general practitioners, medical oncology, neoplasms, patient preference
1. INTRODUCTION
Following a cancer diagnosis, patients are usually faced with various treatment options. The recent increase in treatment options added complexity to the decision‐making process, but simultaneously increased the possibilities for personalised decision‐making (NHG, 2014). In order to make an individual informed choice, patient involvement is key. Patient involvement is facilitated by shared decision‐making (SDM). Recent studies, however, suggest that SDM is insufficiently facilitated in the current cancer care pathway (Brom et al., 2017; Jansen et al., 2006; Weeks et al., 2012). Cancer patients are often not aware of different treatment options (Brom et al., 2017; Jansen et al., 2006), and the time and support required for deliberation seem lacking (Brom et al., 2017). Current treatment guidelines are generally focussed on an optimal gain in survival. Also, the option to refrain from treatment is often underexposed (KNMG, 2015). Consequently, an overview of options to choose from is often incomplete, and opportunities for reviewing and incorporating patients' priorities and preferences in the decision‐making process are insufficiently facilitated.
The SDM process and personalised decision‐making for cancer treatment may be improved by the involvement of the general practitioner (GP) (NHG, 2014). In general, the GP has a long‐term relationship with the patient, resulting in optimal knowledge of the patient's psychosocial and cultural situation and medical history (Lawrence et al., 2016). Because of the position of ‘trusted professional’, GPs are well‐equipped to support patients in the SDM process by elucidating patient's priorities in life and empowering the patient to include these priorities in their decision‐making process. Therefore, patients and GPs envision a role for the GP in treatment decision‐making (Halkett et al., 2015; Klabunde et al., 2009), and both advocate more GP involvement to improve the SDM process after a cancer diagnosis (Noteboom et al., 2020).
To be able to support their recently diagnosed cancer patients in the SDM process, GPs need to understand the patients' perspective on treatment decision‐making. Some aspects, such as the factors that influence the acceptance or decline of a proposed treatment, including treatment success rate, fear of side effects or the recommendation of the physician, are known (Puts et al., 2015). To truly support a patient in the SDM process, understanding of the weighing of considerations (which and how) for treatment decision‐making is vital. Currently, detailed information about the SDM process from patients' perspective and the added value of the GP in this process is lacking. Therefore, we aim to understand the decision‐making process for cancer treatment and to explore the perceived added value of the GP from the perspective of cancer patients treated with a curative intent.
2. METHODS
2.1. Study design
An explorative qualitative study was performed. The GRIP study and Time Out study were approved by the Medical Ethics Research Committee of the University Medical Centre Utrecht (GRIP METC protocol number 16‐232/C, Time Out METC protocol number 16‐654/C) and considered non‐eligible for full ethical review according to Dutch law.
2.2. Sample and setting
Patients who were recently diagnosed with cancer and experienced the process of making a decision for cancer treatment with curative intent were eligible. Since we aimed to explore the support of the GP in this process at a distinct moment in time in their care path, we only included patients who consulted their GP shortly after the cancer diagnosis. Patients were purposefully selected from two ongoing projects on SDM in cancer, the GRIP (Perfors et al., 2018) and the Time Out study. In both studies, patients had a consultation with their GP soon after they were diagnosed with cancer (Time Out Consultation—TOC), which was aimed to facilitate GP support in SDM and to discuss the proposed treatment options (Perfors et al., 2018). This TOC was intended to be planned before the moment of the final treatment decision with the treating physician in secondary care.
Patients in the GRIP study were invited by the coordinating researcher to participate in this follow‐up interview study. Patients in the Time Out study were invited by their treating physician or nurse in the hospital. If willing and eligible, patients provided verbal and written consent for participation in the interviews.
2.3. Data collection
Semi‐structured in‐depth face‐to‐face interviews were conducted between May 2016 and January 2018 by one researcher (EN) (Kolb, 2012). An interview guide was used, with predetermined questions based on the main topics: patient's experiences with 1) the treatment decision‐making process, and 2) the added value of GP's involvement shortly after the cancer diagnosis (Table 1 presents the full topic list). The topics were based on the research aim and the clinical experience of the research team. This team includes a GP, a medical oncologist and researchers in the field of oncology and primary care. The decision‐making process was defined as the process of the weighing of considerations (which and how) in the period from the presentation of the treatment plan by the treating physician to the patient and the decision for treatment.
TABLE 1.
Semi‐structured interview topic list
| Topics treatment decision‐making process |
|---|
| 1. Impact of diagnosis |
| 2. Content of treatment decision |
| 3. Involvement of patient him/herself in their treatment decision |
| 4. Influencers, such as: |
| Social context |
| Life goals |
| Impact of treatment |
| Prognosis |
| 5. Role of significant others in treatment decision |
| Added value of GP |
| 6. General experiences with Time Out Consultation |
| 7. Topics discussed during Time Out Consultation |
| 8. Added value of the GP shortly after diagnosis, such as for: |
| Shared decision‐making |
| Final decision |
Interviews had the character of an open conversation, with prompt questions to gain deeper insight into the experiences of the patient. The interview guide was adapted during the study based on the insights gathered during the analysis, by rephrasing or adding questions. Patients in the GRIP study were interviewed after GRIP study participation. Patients in the Time Out study were interviewed shortly after the treatment decision and were interviewed on average of six months (range 1–12) after diagnosis. Interviews took place at a location of patient's preference. Most patients were interviewed at home, and two patients were interviewed at their hospital. During one interview the daughter and in four interviews the partner of the patient was present. The interviews were audio recorded. The duration of the interviews was on average 43 minutes (range 21–93 minutes). Directly after each interview, memos were written addressing observations and reflections on initial thoughts related to the emerging themes and alterations of the interview guide. Demographic characteristics were available from the GRIP and Time Out study files and included sex, age, type of cancer, social situation and education. Data collection continued until data saturation occurred, that is no new themes emerged from the data (Saunders et al., 2018).
2.4. Data analysis
All interviews were transcribed verbatim. To increase the credibility of the results and if desired by patients (n = 11), a summary of the interview was sent to the patient and used as member check. One patient contacted the interviewing researcher for a minor revision afterwards. Data analysis was performed by two researchers (EN & SV) according to the principles of the grounded theory (Glaser et al., 1967). The constant comparative method was used; data collection and analysis were alternated, and identified themes were continuously compared for differences and similarities within and between interviews (Glaser et al., 1967). In addition, memos were created during the analysis regarding the creation of themes and how these relate, which supported the analysis process (de Casterle et al., 2012).
First, the interview texts were read out in full to get an overall picture and were reread to grasp the details. Secondly, the interview texts were open coded. Data were segmented, and initial codes were identified and linked to the text fragments. After performing open coding of four interviews, axial coding was started. During axial coding, initial codes were collated. These related codes were integrated and brought under broader categories, which were labelled with meaningful themes. In this phase, the first coding tree was established and adapted during the analyses. Themes were further defined and reviewed based on the interview texts. Finally, during selective coding, we confirmed the core theme of the treatment decision‐making process and defined how other themes related to and influenced the core theme. Discrepancies in coding between the two researchers were discussed until consensus was reached. The data and the analysis were discussed regularly in joint meetings within the research team (EW, CH, AM, NW, EN) (Guba, 1981). NVivo 12.0 software (QSR International Pty Ltd, version 12, 2015) was used to support the analysis.
3. RESULTS
In total, 68 patients were selected from both studies, of which 22 patients agreed to participate. The main reason for non‐participation was that ‘participation was considered as too much of a burden’. Two patients were excluded after interviewing, as in both interviews patients were unable to provide in‐depth answers for robust analysis; one due to cognitive problems and the other needed to be performed by telephone, which did not provide data of high enough quality (Figure 1). The majority of the patients was female (70%), diagnosed with breast cancer (45%) and on average 69 years old. The majority of the patients received high education (58%) and was married (63%) (Table 2).
FIGURE 1.
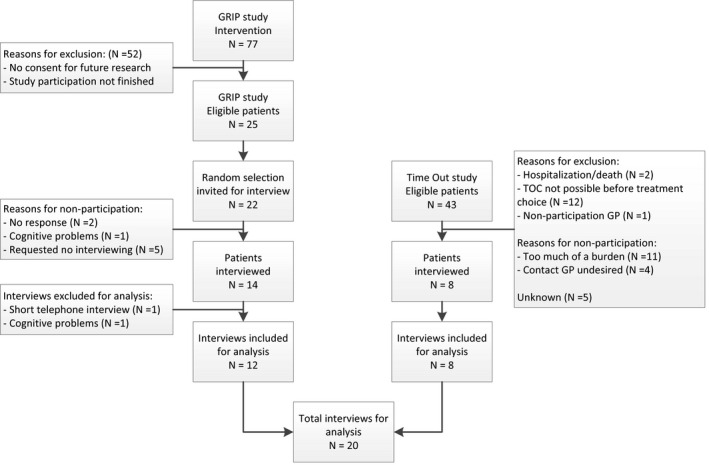
Overview of number of eligible patients, patients invited and patients interviewed in the GRIP and Time Out study
TABLE 2.
Characteristics of the participants
| Pt | Study | Sex | Age (yrs) | Cancer type | Education | Social situation | Experienced treatment plan | |
|---|---|---|---|---|---|---|---|---|
| 01 | GRIP | F | 66 | Melanoma | Low | Single | 1 option | O |
| 02 | GRIP | F | 68 | Breast | Low | Married | Sequential steps | O→CT→RT |
| 03 | GRIP | M | 65 | Colon | High | Married | Sequential steps | RT→CT→O |
| 04 | GRIP | F | 66 | Breast | High | Married | Sequential steps | O→CT |
| 05 | GRIP | F | 69 | Melanoma | Low | Married | 1 option | O |
| 06 | GRIP | F | 76 | Breast | High | Married | Sequential steps | CT→O→RT→HT |
| 07 | GRIP | F | 72 | Breast | High | Widow | Sequential steps | O→HT |
| 08 | GRIP | F | 72 | Breast | High | Married | Sequential steps | O→RT |
| 09 | GRIP | F | 55 | Breast | Low | Married | Sequential steps | O→RT |
| 10 | GRIP | M | 55 | Colon | High | Widow | Sequential steps | RT→CT→O |
| 11 | GRIP | F | 54 | Breast | High | Married | Sequential steps | O→CT→RT→HT |
| 12 | GRIP | F | 59 | Breast | High | Divorced | Sequential steps | CT→O→RT→HT |
| 13 | TO | F | 69 | Breast | Middle | Married | Sequential steps | RT→O→CT |
| 14 | TO | M | 74 | Prostate | Low | Married | >1 option | RT or CT or O |
| 15 | TO | F | 82 | Lung | Low | Widow | >1 option | Doing nothing or O or RT |
| 16 | TO | M | 77 | Prostate | High | Married | >1 option | RT or CT or O |
| 17 | TO | F | 81 | Gynaecologic | High | Single | Sequential steps | O→ RT |
| 18 | TO | F | 75 | Gynaecologic | Middle | Single | Sequential steps | O→ RT |
| 19 | TO | M | 74 | Prostate | Middle | Married | 1 option | RT |
| 20 | TO | M | 73 | Prostate | Middle | Married | >1 option | RT or O |
Abbreviations: ‘→’, treatment plan with sequential steps; CT, chemotherapy; F, female; HT, hormonal therapy; M, male; O, operation; Pt, patient; RT, radiotherapy; TO, Time Out.
Treatment options in bold were accepted and non‐bold treatment options were rejected by the patient.
3.1. The treatment decision‐making process
All patients described that their treating physician offered a treatment plan. Patients described the time in which the treatment plan was presented as a chaotic period in their life, and they used words like a ‘circus’, ‘surrealistic world’, ‘rollercoaster’, ‘automatic process’ and ‘windmill’. Three types of treatment plans could be distinguished: a treatment plan with 1) one treatment option, 2) multiple treatment options or 3) sequential treatment steps (Table 2). The extent to which patients perceived having a treatment choice differed per type of treatment plan. All patients who expressed that they were presented with one treatment option (type 1) perceived to have no choice. Patients with multiple treatment options (type 2) described that they felt they were offered with options to choose from. For patients presented with sequential treatment steps (type 3), the extent to which having a choice was perceived differed. Those who did feel they had a choice described their options as: acceptance of their treatment plan or not, acceptance of receiving adjuvant treatment or not, or choosing the type of surgery/radiotherapy. Patients who did not perceive having a choice expressed that following the proposed treatment plan was the only option. One patient suggested that, even though a choice was offered, the rollercoaster after diagnosis did not allow participation in treatment decision‐making.
Figure 2 presents the model for cancer patients' treatment decision‐making process for patients who did experience having a choice and those who did not. The core concept in patients' treatment decision‐making process was ‘safeguarding survival’. This dominant theme determined all patients' treatment decision‐making processes, including the prioritisation of the considerations involved. A theme which was strongly related to ‘safeguarding survival’ was ‘trust in the physician’, which was often expressed as a reason to follow the physician's proposed treatment plan. Based on patients' considerations of safeguarding survival, strengthened by trust in the physician, patients accepted, at least partially, the treatment plan as proposed by the physician. They viewed this as the best way to safeguard survival. For patients who perceived having a choice and expressed that they actively made a treatment decision, the following themes were additionally important: ‘burden of treatment’, ‘feeling safe that the cancer is removed’, ‘treatment option as plan B’ and ‘previous experiences’. The themes determining the decision‐making process are explained in detail below.
FIGURE 2.
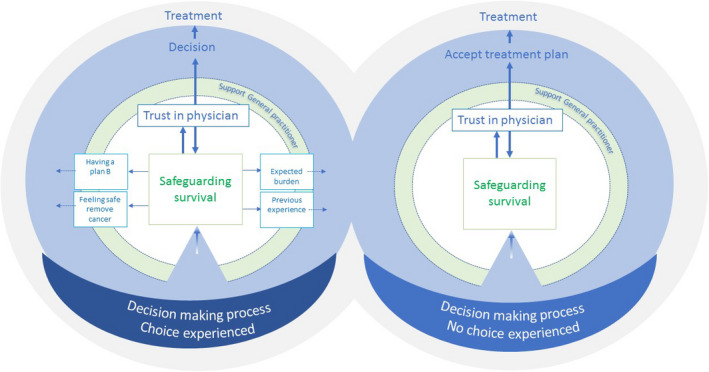
Cancer patients' treatment decision‐making process for those patients who experienced a choice and those who did not
3.1.1. Theme: Safeguarding survival
For all patients, the decision‐making process was strongly determined by the ‘urge to survive’. Consequently, pursuing optimal survival to safeguard survival dominated their decision‐making process. Patients' desire to survive was expressed as the result of a deep‐felt wish to live, to support children or to realise plans for the future. This aim to safeguard survival led to a firm belief that abstaining from treatment was not a realistic option. Patients reasoned that leaving cancer untreated would lead to worsening of complaints and ultimately premature death. Patients also reasoned that, since their cancer was diagnosed in a relatively early and curable stage, aiming for survival was possible, which for them logically led to the acceptance of treatment. Moreover, patients mentioned that by accepting the proposed treatment plan, they would avoid regrets later in life in case of recurrence of cancer. Refusing treatment was felt to jeopardise their chance of survival, resulting in a clear wish to be treated.
‘Then I thought again, yes, but I once started this treatment thinking, well…, please stay away (cancer) as long as possible. So, let's accept everything then’. (PT13).
Patients, who did not perceive having a choice, expressed that they thought that the proposed treatment plan was the only and best approach for attaining survival ‘this is what needs to be done’. Some patients said that the physician had stressed that this was the only option.
Some patients were faced with the decision to accept or decline adjuvant treatment. Again safeguarding survival was the main motivation to guide their decision. Two patients expressed that they felt their survival was already guaranteed by the primary treatment and therefore rejected adjuvant treatment. This was strengthened by the wish to prevent the potential side effects of treatment.
3.1.2. Theme: Trust in the physician
Patients expressed trust in the physician's expertise of what should be done to treat their cancer and safeguard survival. They considered the treating physician as having the required expertise to choose the best option to safeguard survival. They belief that the physician in particular has the necessary knowledge and experience for this. Consequently, most patients felt an urge to follow the initially proposed treatment plan, without reconsideration. A patient, who had been offered multiple options, expressed disappointment since the physician did not propose ‘the single best treatment option’. A few patients felt incapable to make a choice since they did not experience having the required expertise themselves.
‘Even if he (treating physician) had offered me a choice, I would have said to him, doctor: “What do you think is the best option?” Because I don't know. If I should make a choice, I would start guessing, but I can't judge what's best. I do not have the expertise and to go back to school is not an option either. So I trust on the doctor's profession’. (PT03).
3.1.3. Theme: Burden of treatment
Even though safeguarding survival was dominant in the decision‐making process, patients who actively made a treatment decision did weigh the expected burden of the treatment against the potential gain in survival. Burden was described by patients as the potential side effects of treatment (e.g. muscle damage or flushes). Patients also considered the duration of treatment, its impact on daily life (e.g. impact of erectile dysfunction on sexual behaviour) and the impact on physical status (e.g. influence of narcosis on cognition or adjuvant hormonal therapy on polyarthritis) as potential burden. Patients also considered practical issues, such as transportation to the hospital or hospital stay (overnight) as potential burden. However, the latter issues were not mentioned as decisive. As part of the considerations concerning burden, patients expressed that this was inevitable and they reasoned that treatment could always be discontinued if the burden would become untenable. Therefore, patients accepted treatment.
‘So, I let him (treating physician) calculate exactly what that meant for me in terms of survival, 5% I found….well significant. But I thought yes, 5 years of feeling bad…look I’ve been feeling bad from the chemotherapy, operation and radiotherapy let's say three quarters of a year. Okay, that's what I’m willing to do. Five years is too long for me. So, I thought I’d get started, but if it's too much of a burden, then I’ll stop’. (PT13).
Burden only became decisive if different treatment options were considered to have the same effect on survival. Then, patients generally choose the treatment with the least expected burden. As an exception, for one patient who considered accepting adjuvant treatment, the potential gain in survival was overruled by the potential burden of treatment (i.e. side effects). The burden was considered unacceptable, which resulted in abstaining from treatment.
3.1.4. Theme: Feeling safe because cancer will be removed
Some patients who actively made a treatment choice expressed that they desired a treatment that should give them a feeling of safety. Removing cancer physically was felt to be the safest option. Patients favoured physical removal of cancer with surgery over radiotherapy or ablation over breast conserving treatment for a higher feeling of safety.
‘In the end I chose for ablation, as it felt safer. That wasn't supported by evidence, but I thought, I really don't want anything to ever happen in the remaining breast or to be afraid that anything could happen’. (PT12).
3.1.5. Theme: Treatment option as plan B
For some patients, the fact that they had a ‘plan B’ influenced decision‐making. Patients described a ‘plan B’ as a treatment that would function as a safety net to ensure survival if needed, in case primary treatment fails. One patient reasoned that if surgery was unsuccessful, radiotherapy could be an option. As surgery was not a consecutive option if radiotherapy was unsuccessful, this patient preferred to have surgery first.
‘I understood that in my case, if the cancer is not completely removed by surgery, radiation would still be possible. […] Yes, a plan B. I don’t know if it provides me with a 100% guarantee, but it is a sort of lifesaver. (PT16)’
Another patient explained that she was told that the adjuvant therapy would remain available in case of a recurrence. She therefore refused adjuvant treatment initially and considered this treatment as plan B for the future.
3.1.6. Theme: Expectations from previous experiences with treatment
Previous experiences of the patient or others with treatment and side effects, such as previous operations, radiotherapy for previous disease or flushes caused by menopause, influenced the expectations of treatment. They could either increase the expectations of the burden of treatment or provide trust that it was going to be all right as patients already knew they could handle the side effects. These previous experiences were part of the considerations, but were not decisive in treatment decision.
‘Well okay, but I also talked to a friend who is a couple of years younger and she said: “I took it (hormonal treatment) for a couple of months and I've had flushes. I was really in the bathroom at night with my wrists under cold water and thinking, ah I feel so miserable.” But yes, well I thought I've had the menopause and the related issues, but well that's over and well if it comes back, than it will never be as bad as it was then. No.’ (PT08).
3.2. The added value of the GP shortly after diagnosis
All patients experienced contact with the GP shortly after diagnosis as pleasant. Patients described their GP as ‘easily accessible’, ‘independent’, ‘a trusted person’, ‘familiar to the patient’ and ‘has time for the patient’. The themes concerning the added value of the GP during the decision‐making process were ‘the GP is up to date with my situation’, ‘experienced support to cope with diagnosis’ and ‘experienced support for decision‐making’.
3.2.1. Theme: The GP is up to date about my situation
The majority of the patients mentioned that it is important that the GP was aware of their diagnosis. They explained that in case of future health problems for which they expect to visit their GP, it is important for the GP to be fully up to date with their health status. In addition, patients expressed a feeling of trust, knowing that the GP was up to date.
3.2.2. Theme: Experienced support to cope with diagnosis
The majority of the patients experienced support from their GP in discussing the impact of the diagnosis, discussing their feelings and for reflecting on what was about to happen.
‘Then they say yes you should be able to discuss it with your family, but there are certain things that you think would burden your partner too much and I would like to discuss these with my GP. Look, one day you can handle it very well, but the other day you feel a sort of sad and you think who should I talk to, so that are moments I think my GP should take care of that’. (PT02).
Patients expressed ‘being heard’ by the GP. Knowing that the GP was willing to involve other healthcare professionals for additional support if necessary, strengthened this feeling. Most patients considered the psychological support of the GP as of added value in the process of coping with the diagnosis.
‘Well, it does make you feel like they're fighting for you. That you're important. I had that feeling, and I still do, that they are not letting you go’. (PT13).
Some patients, however, did not express a need for reflection on the diagnosis with the GP, as they reasoned that they had sufficient support in the hospital and therefore felt well prepared, or because they experienced enough support from their significant others.
‘We have a very large social safety net, so in that respect, we do not need to knock on the door of the GP, so to speak. (PT10)’
3.2.3. Theme: Experienced support for decision‐making
When reflecting on their TOC with the GP, a minority of the patients experienced GP support in their actual treatment decision‐making process. If SDM support was present, patients mentioned that the GP helped them to understand the information as given by the treating physician. Patients also indicated that their GP answered the remaining questions or provided questions which the patient could ask during the next consultation with the treating physician. Finally, patients said that the GP created awareness of having a choice or confirmed patient's choice for treatment, if it had already been made by the patient.
‘She (GP) remarked to ask (to the treating physician), “If I do nothing, no radiotherapy, what would be the consequences?” That was a useful suggestion and made it clear to me that I was not offered by my treating gynaecologist with the choice to accept radiotherapy or not. While that was very important to be able to make an informed choice and not to wait and see what I was told to do’. (PT18).
Some patients did not experience added value of the GP for decision‐making. For them, the information provided in the hospital was enough to make a decision since they had trust in the expertise of the treating physician. They explained that in their view, the GP does not have sufficient knowledge about treatment options. They also wanted to prevent confusion if the GP would suggest a different treatment.
‘If I’m going to discuss this with my GP…well he does not know the ins and outs of the treatment or the disease itself well enough. (PT11)’
4. DISCUSSION
This qualitative study aimed to understand the treatment decision‐making process for cancer patients treated with a curative intent and to describe the patients' experienced added value of the GP in this process. In this curative setting, the core concept in the process of decision‐making was ‘a focus on safeguarding survival’. This focus dominated and determined all patients' decision‐making processes. This resulted in accepting (at least part of) the proposed treatment plan. To ensure survival, patients relied on the physician's expertise to guide the treatment decision. Part of the patients did not perceive having a choice in the treatment decision. Only when treatment options had a comparable influence on survival or when adjuvant treatment was discussed, other considerations could become decisive. The GP was generally experienced as of added value for providing psychosocial support, particularly for coping with the diagnosis. In addition, patients appreciated being able to discuss the impact of the diagnosis with a trusted professional who is up to date with their context. Added value of the GP in the decision‐making process was confirmed by some, mainly because of the opportunity for reflection and awareness of choice, but opposed by others.
4.1. Strengths and limitations
A strength of this study is data saturation we reached for the main themes. In addition, the chance of interpretation bias was reduced by verbatim transcription of the interviews, coding by two researchers, followed by peer review. The main limitation is the potential recall bias in the interviews since some patients were interviewed after substantial time after the diagnosis. Also, we did not check patients' treatment plan in their electronic health record. Therefore, we do not know whether the treatment option(s), as perceived by the patients, corresponds with those as proposed by the treating physician. In addition, we had difficulties with reaching maximum variation in our sample as patients with breast cancer were over‐represented in the GRIP study. This might have limited diversity in our data and therefore potentially limits transferability of the outcomes. Finally, potential selective participation may have occurred, since reasons for non‐participation included ‘too much of a burden’ and since our population was of a relatively high education level. This may lead to a group of participants which is relatively fit and well‐equipped for a more active approach to cancer treatment decision‐making. However, since the strong urge for survival was present in all patients, it seems highly plausible that this is the decisive factor among patients with all cancer types treated with curative intent.
4.2. Comparison with existing literature
The literature describes that, as the number of treatment options increases, treatment decisions become more complex. Additionally, professionally dominated decision‐making processes seem to primarily focus on gaining survival, leaving little room for personal preferences (Amalraj et al., 2009; Brom et al., 2017; Greene & Adelman, 2003; KNMG, 2015; Puts et al., 2015; Rodrigues & Sanatani, 2012; Walko & McLeod, 2014; de Wit, 2017). Our study shows that from the perspective of cancer patients, the decision‐making process is dominated by a strong focus on survival. It also shows that this focus on survival in a turbulent phase impedes the perception of choice and leads to a tendency to follow the physician's advice without consideration. This paternalistic approach is the opposite of what is advocated for in recent literature, since it may reduce the room for involving personal preference in decision‐making.
The perception of not having a choice could be due to inadequate communication (initially proposed treatment plan is not presented as an option), a lack of awareness of having a choice (options presented, but not perceived as options) or a lack of awareness to be involved in a critical decision in the short and turbulent time between diagnosis and treatment decision. This confirms earlier reports. Brom et al. (2017) reported that patients' unawareness of having a treatment choice might be the result of insufficient awareness creation by physicians (Brom et al., 2017). Jansen et al. (2006) found that one predictor for not experiencing a treatment choice was the patients' preference for a passive role in decision‐making (Jansen et al., 2006). The effect of patients' perceived involvement and the perception of having a choice on patient reported outcomes are relevant, but studies assessing these effects show contradictory results (Hack et al., 2006; Jansen et al., 2004; Orom et al., 2016).
A review by Puts et al. (2015) concluded that, although the reasons of older adults to accept or decline cancer treatment varied considerably between studies, the physician's recommendation is the most consistent decisive factor (Puts et al., 2015). Our results confirm that most patients follow the physician's recommendation, with the underlying explanation that patients want to safeguard their survival and that they trust their physician's expertise to achieve this aim. Both our results and the review report that the potential burden of treatment is mentioned as a potential reason to decline treatment (Puts et al., 2015).
Regarding the role of the GP, Wallner et al. (2016) concluded that increased GP support in decision‐making was associated with higher decision satisfaction (Wallner et al., 2016). In 2019, we showed that palliative cancer patients and their healthcare providers appreciated increased GP involvement in SDM, such as for reflection on and preparation for treatment decision (Noteboom et al., 2020). Our more recent study showed that patients often perceive psychosocial support after a cancer diagnosis, but that the need to be supported by the GP in SDM remains generally unanswered (accepted for publication in British Journal of General Practice Open, June 2020). In this current study, among those treated with curative intent, we found that the added value for GP involvement was mostly ascribed to psychological support and only modestly for supporting the treatment decision. Therefore, the added value of psychological GP support seems universally confirmed, but the experienced added value for SDM support may be more subject to preference and disease and treatment characteristics.
4.3. Implications for practice
The results guide GPs on how to support their patients after a cancer diagnosis. The key added value of the GP is in offering psychological support, to help patients to deal with the impact of the cancer diagnosis. In a joint effort between primary and secondary care, GPs and treating physicians in the hospital should actively explore patients' preferences for GP involvement in the decision‐making process. Also, they should be aware that patients do not always perceive having a choice, are focussed on survival and are inclined to follow the treating physicians' advice. Patients should be actively made aware of their share in decision‐making, as well as the potential role of the GP in the decision‐making process.
5. CONCLUSION
The treatment decision‐making process of cancer patients treated with curative intent is dominated by the urge to ‘safeguard survival’. As a result, there is a strong tendency to accept the treatment plan as offered by the physician. GPs should be aware of their added value in providing psychological support and their potential role to support SDM following a cancer diagnosis.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interests.
ACKNOWLEDGEMENTS
The authors are grateful to the participants of the study and the participating hospital staff and GPs. In addition, we are grateful to Nicole Plum, who, as patient representative, supported the design of the interviews and the GRIP study. Financial support was provided by the Dutch Cancer Society (KWF) and the unrestricted Danone Ecosystem Fund.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- Amalraj, S. , Starkweather, C. , Nguyen, C. , Naeim, A. (2009). Health literacy, communication, and treatment decision‐making in older cancer patients. Ethics, 23(4), 369–375. [PubMed] [Google Scholar]
- Brom, L. , De Snoo‐Trimp, J. C. , Onwuteaka‐Philipsen, B. D. , Widdershoven, G. A. M. , Stiggelbout, A. M. , & Pasman, H. R. W. (2017). Challenges in shared decision making in advanced cancer care: a qualitative longitudinal observational and interview study. Health Expectations, 20(1), 69–84. 10.1111/hex.12434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Casterle, B. D. , Gastmans, C. , Bryon, E. , & Denier, Y. (2012). QUAGOL: A guide for qualitative data analysis. International Journal of Nursing Studies, 49(3), 360–371. 10.1016/j.ijnurstu.2011.09.012 [DOI] [PubMed] [Google Scholar]
- de Wit, N. J. (2017). A "time out consultation" in primary care for elderly patients with cancer: Better treatment decisions by structural involvement of the general practitioner. European Journal of Cancer Care, 26(3), e12711. 10.1111/ecc.12711 [DOI] [PubMed] [Google Scholar]
- Glaser, B. G. , Strauss, A. L. , & Strutzel, E. (1967). The discovery of grounded theory; strategies for qualitative research. Nursing Research, 17(4), 364. [Google Scholar]
- Greene, M. G. , & Adelman, R. D. (2003). Physician‐older patient communication about cancer. Patient Education and Counseling, 50(1), 55–60. 10.1016/S0738-3991(03)00081-8 [DOI] [PubMed] [Google Scholar]
- Guba, E. G. (1981). Criteria for assessing the trustworthiness of naturalistic inquiries. Ectj, 29(2), 75. [Google Scholar]
- Hack, T. F. , Degner, L. F. , Watson, P. , & Sinha, L. (2006). Do patients benefit from participating in medical decision making? Longitudinal follow‐up of women with breast cancer. Psycho‐Oncology, 15(1), 9–19. 10.1002/pon.907 [DOI] [PubMed] [Google Scholar]
- Halkett, G. K. , Jiwa, M. , & Lobb, E. A. (2015). Patients' perspectives on the role of their general practitioner after receiving an advanced cancer diagnosis. European Journal of Cancer Care, 24(5), 662–672. 10.1111/ecc.12224 [DOI] [PubMed] [Google Scholar]
- Jansen, S. J. T. , Otten, W. , & Stiggelbout, A. M. (2006). Factors affecting patients' perceptions of choice regarding adjuvant chemotherapy for breast cancer. Breast Cancer Research and Treatment, 99(1), 35–45. 10.1007/s10549-006-9178-z [DOI] [PubMed] [Google Scholar]
- Jansen, S. J. T. , Otten, W. , van de Velde, C. J. H. , Nortier, J. W. R. , & Stiggelbout, A. M. (2004). The impact of the perception of treatment choice on satisfaction with treatment, experienced chemotherapy burden and current quality of life. British Journal of Cancer, 91(1), 56–61. 10.1038/sj.bjc.6601903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klabunde, C. N. , Ambs, A. , Keating, N. L. , He, Y. , Doucette, W. R. , Tisnado, D. , Clauser, S. , & Kahn, K. L. (2009). The role of primary care physicians in cancer care. Journal of General Internal Medicine, 24(9), 1029–1036. 10.1007/s11606-009-1058-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- KNMG . (2015). Niet alles wat kan, hoeft. Retrieved from Utrecht: www.knmg.nl/passendezorg [Google Scholar]
- Kolb, S. M. (2012). Grounded theory and the constant comparative method: Valid research strategies for educators. Journal of Emerging Trends in Educational Research and Policy Studies, 3(1), 83. [Google Scholar]
- Lawrence, R. A. , McLoone, J. K. , Wakefield, C. E. , Cohn, & R. J. (2016). Primary care physicians' perspectives of their role in cancer care: A systematic review. Journal of General Internal Medicine, 31(10), 1222–1236. 10.1007/s11606-016-3746-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHG . (2014). NHG‐Standpunt Oncologische zorg in de huisartsenpraktijk. Retrieved from https://www.nhg.org/sites/default/files/content/nhg_org/uploads/nhg‐standpunt_oncologische_zorg.pdf [Google Scholar]
- Noteboom, E. A. , de Wit, N. J. , van Asseldonk, I. , Janssen, M. C. A. M. , Lam‐Wong, W. Y. , Linssen, R. H. P. J. , Pepels, M. J. A. E. , Schrama, N. A. W. P. , Trompper, M. E. H. , Maaike Veldhuizen, L. , Wijtvliet, A. P. , Zeldenrust, E. G. F , Hendrikx, A. M. , van de Boomen, W. A. , Elbersen, D. M. , Jacobs, E. M. G. , van der Wall, E. , & Helsper, C. W. (2020). Off to a good start after a cancer diagnosis: implementation of a time out consultation in primary care before cancer treatment decision. Journal of Cancer Survivorship, 14(1), 9–13. 10.1007/s11764-019-00814-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orom, H. , Biddle, C. , Underwood, W. III , Nelson, C. J. , & Lynn Homish, D. (2016). What is a “good” treatment decision? Decisional control, knowledge, treatment decision making, and quality of life in men with clinically localized prostate cancer. Medical Decision Making, 36(6), 714–725. 10.1177/0272989X16635633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perfors, I. A. A. , Helsper, C. W. , Noteboom, E. A. , de Wit, N. J. , & May, A. M. (2018). Randomised controlled trial protocol (GRIP study): examining the effect of involvement of a general practitioner and home care oncology nurse after a cancer diagnosis on patient reported outcomes and healthcare utilization. BMC Cancer, 18(1), 132. 10.1186/s12885-018-4005-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puts, M. T. , Tapscott, B. , Fitch, M. , Howell, D. , Monette, J. , Wan‐Chow‐Wah, D. , Krzyzanowska, M. , Leighl, N. B. , Springall, E. , & Alibhai, S. M. (2015). A systematic review of factors influencing older adults' decision to accept or decline cancer treatment. Cancer Treatment Reviews, 41(2), 197–215. 10.1016/j.ctrv.2014.12.010 [DOI] [PubMed] [Google Scholar]
- Rodrigues, G. , & Sanatani, M. (2012). Age and comorbidity considerations related to radiotherapy and chemotherapy administration. Seminars in Radiation Oncology, 22(4), 277–283. 10.1016/j.semradonc.2012.05.004 [DOI] [PubMed] [Google Scholar]
- Saunders, B. , Sim, J. , Kingstone, T. , Baker, S. , Waterfield, J. , Bartlam, B. , Burroughs, H. , & Jinks, C. (2018). Saturation in qualitative research: exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walko, C. M. , & McLeod, H. L. (2014). Personalizing medicine in geriatric oncology. Journal of Clinical Oncology, 32(24), 2581–2586. 10.1200/jco.2014.55.9047 [DOI] [PubMed] [Google Scholar]
- Wallner, L. P. , Abrahamse, P. , Uppal, J. K. , Friese, C. R. , Hamilton, A. S. , Ward, K. C. , Katz, S. J. , & Hawley, S. T. (2016). Involvement of primary care physicians in the decision making and care of patients with breast cancer. Journal of Clinical Oncology, 34(33), 3969–3975. 10.1200/jco.2016.67.8896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks, J. C. , Catalano, P. J. , Cronin, A. , Finkelman, M. D. , Mack, J. W. , Keating, N. L. , & Schrag, D. (2012). Patients' expectations about effects of chemotherapy for advanced cancer. New England Journal of Medicine, 367(17), 1616–1625. 10.1056/NEJMoa1204410 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


