Abstract
Background
Cardiopulmonary resuscitation (CPR) in adults following non-traumatic out of hospital cardiac arrest (OHCA) can cause thoracic complications including rib fractures, sternal fractures, and pneumothorax. Post-CPR complication rates are poorly studied and the optimum imaging modality to detect these complications post-resuscitation has not been established.
Methods
We performed a retrospective review of adult patients transported to a single, urban, academic hospital following atraumatic OHCA between September 2015 and January 2020. Patients who achieved sustained return of spontaneous circulation (ROSC) and who underwent computed tomography (CT) imaging of the chest following radiographic chest x-ray were included in the analyses. Patient demographics and prehospital data were collected. Descriptive statistics and multivariate logistic regression analysis were performed. Sensitivity and specificity of chest x-ray for the detection of thoracic injury in this population were estimated.
Results
786 non-traumatic OHCA patients were transported to the ED, 417 of whom obtained sustained ROSC and were admitted to the hospital (53%). 137 (32.9%) admitted patients underwent CT imaging of the chest in the ED. Of these imaged patients median age was 62 years old (IQR 53–70) with 54.0% female and 38.0% of patients having received bystander CPR. 40/137 (29.2%) patients had skeletal fractures noted on CT imaging and 12/137 (8.8%) had pneumothorax present on CT imaging. X-ray yielded a sensitivity of 7.5% for rib fracture and 50% for pneumothorax with a specificity of 100% for both. Logistic regression analysis revealed no significant association between age, sex, bystander CPR, or resuscitation length with thoracic fractures or pneumothorax.
Conclusions
Complications from OHCA CPR were high with 29.2% of CT imaged patients having rib fractures and 8.8% having pneumothoraces. X-ray had poor sensitivity for these post-resuscitation complications. Post-CPR CT imaging of the chest should be considered for detecting post-CPR complications.
Keywords: Out of hospital CPR, Chest compression, Return of spontaneous circulation, Pneumothorax
Introduction
Since its inception, the mainstay of cardiopulmonary resuscitation (CPR) continues to be external chest compression.1, 2, 3, 4 The process of external chest compression has been known to cause thoracic chest trauma with complications such as rib and sternal fractures commonly found in cardiac arrest patients.5, 6, 7, 8, 9 Forensic autopsy and post mortem imaging data have aided in the evaluation of thoracic injuries, particularly in examining fracture patterns, but the incidence of thoracic injury in post-resuscitation patients of cardiac arrest is not well known.10, 11, 12 Furthermore, the optimum modality to evaluate these thoracic injuries has not been well described.
Chest film radiography is a routine component of post-cardiac arrest care.13,14 X-ray alone, however, may not be an adequate tool to identify potential complications of CPR in patients with initial return of spontaneous circulation (ROSC).15 Post-cardiac arrest patients are prone to a number of traumatic compilations that can affect their long term outcomes.14,16 Early identification of these injuries may play an important role in the management of these patients in the acute care setting. With the increasing number of post-ROSC therapies and interventions being accrued and as bystander CPR becomes more routine, the accurate evaluation of post-CPR complications becomes increasingly important.
In this study we examined post-ROSC computerized tomography (CT) findings of traumatic thoracic complications in adult out of hospital cardiac arrest patients at our institution and compared them against initial findings on plain radiography. Our objective was to evaluate the rate of complications and the sensitivity of x-ray in detecting those injuries. Our secondary aim was to investigate if any resuscitation variables were more highly associated with thoracic complications in post-ROSC patients.
Methods
This study was a retrospective review of adult patients who obtained CT imaging of the thorax after suffering out of hospital cardiac arrest (OHCA) and presenting to a single, urban, academic emergency department (ED) in the United States. This study was approved by the hospital’s institutional review board. Inclusion criteria included adult (18 years of age or greater), nontraumatic, cardiac arrest patients who presented to the ED from September 2015 to January 2020 who also achieved sustained (i.e. greater than 20 min) ROSC and underwent both plain film chest radiography and CT imaging of the chest in that encounter prior to the conclusion of that hospitalization. All patients received manual compressions in the prehospital and Emergency Department settings as no mechanical CPR devices were employed in these settings for this patient cohort. Cases were excluded if they were in-hospital, less than 18 years of age, traumatic in nature, did not achieve sustained ROSC, or did not obtain CT imaging of the chest in addition to plain film radiography of the chest in that hospital encounter. Chest CT was performed using a GE Revolution 256 slice CT scanner with axial, coronal, and sagittal images obtained (70–140 kV; GE Healthcare, Waukesha WI, USA). Chest plain film radiography was conducted using a Shimadzu MobileArt Evolution MX7 mobile x-ray system (40–125 kV; Shimadzu Corp, Kyoto, Japan). The initial chest x-ray post arrest after sustained ROSC was used for comparison with initial chest CT imaging in the same encounter. The clinical indication reported on chest CT orders within the electronic medical record was also examined and categorized. All radiology interpretations of CT and plain film radiography were performed by board certified radiologists who were unaware of the study.
Incidence of skeletal fractures, pneumothorax, hemothorax, and other traumatic injuries as reported by the interpreting radiologists were collected in addition to demographic information and factors surrounding the arrests (e.g. ROSC rates, bystander CPR). Bystander CPR was defined as CPR performed by a layperson prior to EMS arrival or if the cardiac arrest was witnessed by first responders and initiated by them in the out of hospital setting. Descriptive statistics and a logistic regression analysis was used for analysis using SPSS version 24.0 for Windows (IBM Corp, Armonk NY, USA, Released 2016). A p-value of <0.05 was considered statistically significant.
Results
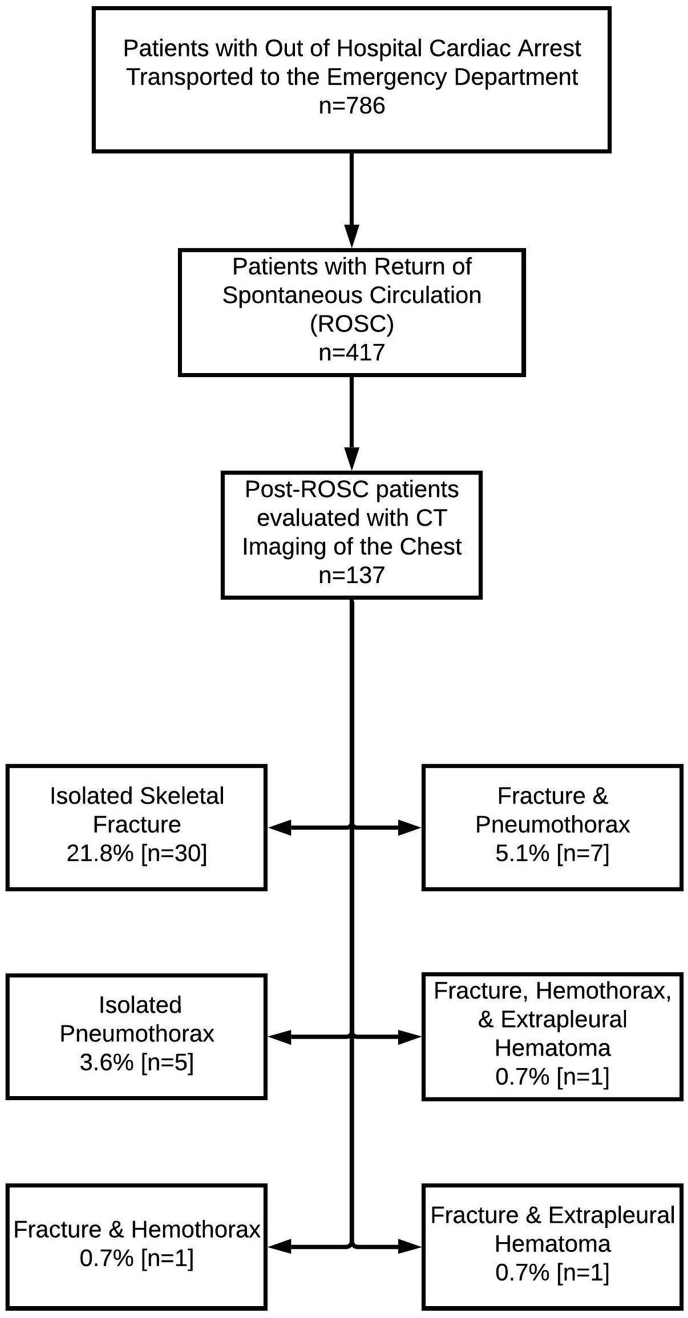
During the study period, 786 adult patients suffered OHCA and were transported to the emergency department with 417 (53.5%) patients achieving sustained ROSC. 137 (32.9%) of the patients with sustained ROSC underwent CT imaging of the chest. Median age for this group was 62 years old (IQR 53–70) with 54.0% female. Overall survival to discharge was 28.5% in this cohort. The majority of patients in this cohort were African American (84.7%) and bystander CPR was reported in 38.0% of the overall patients (Table 1). The indication for CT imaging was reported as evaluation for pulmonary embolism in 75.2% of cases while 11.1% of cases listed “Cardiac Arrest” as the clinical indication. An additional 7.3% reported pulmonary embolism along with a secondary diagnosis (aortic dissection and pneumothorax most commonly) as the reason for CT investigation. A minority (5.1%) reported other indications such as pulmonary infection or drowning; 1.5% of cases did not report an indication for CT chest imaging. Acute pulmonary embolism was found in 28 of the 137 (20.4%) of the CT scans performed. In total, 45 (32.8%) patients were found to have traumatic thoracic injuries (Fig. 1). Rib or sternal fractures were noted in 40 patients (29.2%) while a pneumothorax was seen in 12 patients (8.8%). Extrapleural hematomas (1.5%) and hemothorax (1.5%) were also noted in lower incidence (Table 2).
Table 1.
Characteristics of patients with and without traumatic thoracic complications presenting following OHCA with ROSC and CT imaging of the chest.
| Characteristic | Total patients (n = 137) | Without CT Identified Complications (n = 92) | With CT Identified Complications (n = 45) |
|---|---|---|---|
| Age – Median Years (IQR) | 62 (53–70) | 61 (52–68) | 65 (54–74) |
| Female sex – % | 54.0% | 47.8% | 66.7% |
| Race – % | |||
| African American | 84.7% | 87.0% | 80.0% |
| Caucasian | 5.1% | 4.3% | 6.7% |
| Hispanic | 4.3% | 5.4% | 2.2% |
| Other/Unknown | 5.1% | 3.3% | 8.9% |
| Asian | 0.7% | 0% | 2.2% |
| Bystander CPR | 38.0% | 42.4% | 28.9% |
| Acute Pulmonary Embolism |
20.4% | 22.8% | 15.6% |
Fig. 1.
Traumatic thoracic complications in out of hospital cardiopulmonary resuscitation at a single urban academic center following sustained ROSC and CT imaging of the chest.
Table 2.
Thoracic injuries in patients presenting following OHCA with ROSC on CT imaging of the chest.
| Complication | No. of Patients (Total = 137) |
|---|---|
| Isolated Thoracic Skeletal Fractures | 30 |
| Isolated Pneumothorax | 5 |
| Thoracic Skeletal Fracture and Pneumothorax | 7 |
| Thoracic Skeletal Fracture and Extrapleural Hematoma | 1 |
| Thoracic Skeletal Fracture, Extrapleural hematoma, and hemothorax | 1 |
| Thoracic Skeletal Fracture and Hemothorax | 1 |
| Total Number of Patients with Complications | 45 |
A logistic regression analysis was applied to the factors surrounding the resuscitation including age, sex, bystander CPR, and resuscitation length. No single factor in univariate analysis was found to be significantly associated with the presence of fractures or pneumothorax (Table 3). Additionally, the absence of fractures or pneumothorax was not found to be significantly associated with survival to discharge in this group of patients (p > 0.05).
Table 3.
Logistic regression analysis of factors surrounding thoracic injuries in patients presenting following OHCA with ROSC and CT imaging of the chest.
| Characteristic | Fracture | 95% CI | Pneumothorax | 95% CI |
|---|---|---|---|---|
| Age | p = 0.06 | (0.99–1.05) | p = 0.43 | (0.98–1.06) |
| Sex | ||||
| Female | p = 0.10 | (0.25–1.13) | p = 0.14 | (0.09–1.40) |
| Male | p = 0.10 | (0.89–4.06) | p = 0.14 | (0.09–1.40) |
| Bystander CPR | p = 0.20 | (0.76–3.67) | p = 0.80 | (0.26–2.85) |
| Resus Length | p = 0.30 | (0.09–1.61) | p = 0.90 | (0.13–4.14) |
Rates of traumatic complications related to CPR were also examined as detected on portable chest x-ray. Of the 40 patients found to have fractures noted on the CT of chest, only 3 were noted on portable chest x-ray yielding a sensitivity of 7.5% and a specificity of 100%. For pneumothorax, of the 12 identified on CT, 6 were identified on portable chest x-ray resulting in a sensitivity of 50% and a specificity of 100%.
Of the 14 patients with pneumothorax or hemothorax detected on imaging, 5 patients received chest tube thoracostomy interventions with two of these were performed prior to CT imaging. 5 patients were made comfort care or had care withdrawn with no interventions performed after CT findings. The remaining 4 patients were watched conservatively with 2 surviving to hospital discharge, one in a vegetative state and another with moderate cerebral disability at the time of discharge. One of the five patients receiving chest tubes survived to hospital discharge to a rehabilitation facility with moderate cerebral disability.
Discussion
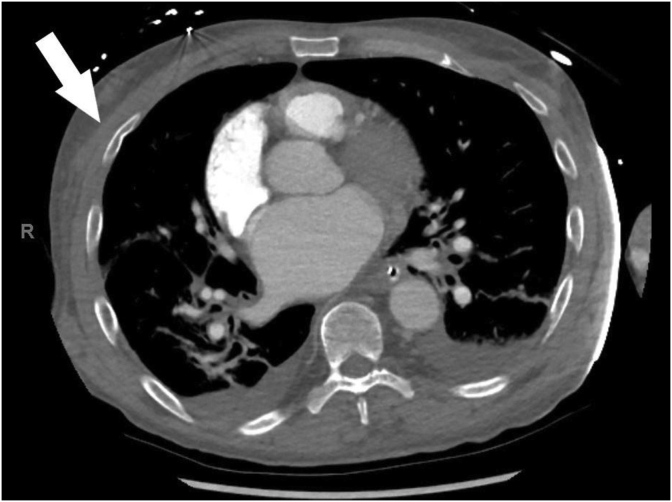
A wide range of incidence of complications related to CPR has been reported in the literature. Skeletal fractures have been the most common reported complication of resuscitation with literature reports ranging from 13 to 97% while lung injuries such as pneumothorax range from 0 to 26%.6,7,17, 18, 19, 20 A greater incidence of rib and sternal fractures have also been associated with lower rates of ROSC.21 The most robust data comes from large prospective autopsy studies that focus on identifying complications related to resuscitation in non-survivors of cardiac arrest.6,10 These investigations have helped clarify that sternal and rib fractures are likely more common that originally conceived in cardiac arrest patients. Their detection is also reported to be underestimated by chest x-ray.22,23 This may be attributed to anterior compression forces during CPR causing incomplete or buckle fractures along the inner cortex that are more accurately detected on CT scans as exemplified in Fig. 2.24 Additionally, a higher incidence of thoracic organ injury such as pneumothorax and hemothorax has also been found in victims of cardiac arrest than originally suspected. Within post-cardiac arrest patients who achieve sustained ROSC, recent studies have begun to evaluate the diagnostic utility of whole body post-ROSC CT protocols to help identify pathology such as pneumothorax earlier.19,25,26 These studies have shown feasibility and value in post-ROSC CT to aid in early detection of pathology such as CPR complications, thoracic organ injury, and acute neurological emergencies. This study has helped to add to the body of literature with evidence that routine thoracic CT in survivors of cardiac arrest can help aid in early identification of complications related to resuscitation that are not appreciated by portable chest radiography.
Fig. 2.
Characteristic bent or angulated appearance of a buckle fracture in a patient who underwent CPR and achieved return of spontaneous circulation. The patient was found to have a incomplete fracture of the mediastinum as well as bilateral anterolateral rib buckling with several displaced rib fractures not detected on chest x-ray imaging.
In this investigation we discovered almost a third of patients (32.8%) having traumatic thoracic injuries detected on post-ROSC CT imaged patients. The incidence of skeletal fracture was nearly 30% while the incidence of pneumothorax was approximately 9% of imaged patients. The incidence of these complications is within the expected range reported in literature and aligns with the most common reports of complication rates.6,7,17, 18, 19, 20 The majority of these injuries were not discovered on portable plain film radiography with sensitivity of x-ray at 7.5% and 50% of these two complications, respectively. Our investigation did not find any significant association between age, sex, bystander CPR or length of resuscitation with the incidence of skeletal fractures or pneumothorax. The incidence of pulmonary embolism in our study population was notably high with a detection rate of over 20% in patients having undergone CT imaging compared to relevant literature citing 2–13% in OHCA.19,27, 28, 29, 30, 31, 32 Our detection rate, however, is within a sample in which clinicians may have had significant clinical suspicion for pulmonary embolism and directed imaging to help investigate its presence compared to all cardiac arrest survivors.
Little is known about the relationship between complications of resuscitation and meaningful outcomes. Guidelines or real time CPR feedback devices that emphasize stronger or deeper compressions may affect the thoracic trauma seen post resuscitation patients. Additionally, the number of peri-arrest and post-ROSC therapies continues to expand.14 With the increased use of extracorporeal membrane oxygenation, targeted temperature management, and low tidal volume ventilation strategies, the early detection of complications such as hemothorax or pneumothorax may become increasingly important given the effects of delayed or missed diagnosis.33, 34, 35 While ultrasound has become a mainstay of pneumothorax detection at the bedside, mediastinal injuries, abdominal injuries, and esophageal injuries which have been noted with cardiac arrest resuscitation would not be detected.6,25,36, 37, 38 In the potential cases of misidentification of cardiac arrest and initiation of bystander CPR, the literature in addition to this study would support the use of thoracic chest CT to help evaluate for complications of CPR in the otherwise non-traumatic arrest patient to help detect injuries portable x-ray would fail to detect. With our study showing the limited utility of plain film radiography, we advocate for increased investigation into the addition of routine thoracic CT in survivors of atraumatic cardiac arrest to help aid in early identification of iatrogenic or bystander thoracic trauma in addition to its already established diagnostic utility for the detection of vascular and thrombotic causes of cardiac arrest.
Limitations
This study has several key limitations. First, this is a single center retrospective study in a primarily urban African American population and our findings may not be generalizable to other populations. Secondly, the analysis was only conducted on patients with sustained ROSC in whom emergency medicine providers felt a CT scan of the thorax was indicated without protocolized post-ROSC treatment. Non-survivors, those who were deemed too unstable for CT imaging, those taken for intervention immediately post-ROSC (e.g. cardiac catheterization), or those that were not imaged were not included in this study. Third, this study does not examine the clinical consequences of the complications found, an important component for future study. Future studies should be directed at identifying meaningful clinical complications such as difficulty with mechanical ventilation, pneumonia, acute respiratory distress syndrome, or clinically significant pneumothorax under positive pressure ventilation.
Conclusion
Complications from OHCA CPR are common with 29.5% of CT imaged patients having rib fractures and 8.6% having pneumothoraces. These findings are significantly under-reported on portable radiographic imaging CT imaging of the chest detects post cardiac arrest complications of CPR in addition to detection of pulmonary embolism. Further study is needed to determine whether routine chest CT imaging in post-OHCA patients results in improved clinical outcomes.
Prior presentations
Poster Presentation at the National Association of EMS Physicians, January 2020, San Diego CA.
Funding sources
For Author Willard Sharp MD, PhD: NIH RO1HL133675.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
References
- 1.Baringer J.R., Salzman E.W., Jones W.A. External cardiac massage. N Engl J Med. 1961;265(2):62–65. doi: 10.1056/NEJM196107132650203. July 13. [DOI] [PubMed] [Google Scholar]
- 2.Kouwenhoven W.B., Jude J.R., Knickerbocker G.G. CLOSED-CHEST cardiac massage. J Am Med Assoc. 1960;173(10):1064–1067. doi: 10.1001/jama.1960.03020280004002. July 9. [DOI] [PubMed] [Google Scholar]
- 3.Kleinman Monica E., Brennan Erin E., Goldberger Zachary D. Part 5: adult basic life support and cardiopulmonary resuscitation quality. Circulation. 2015;132(18_suppl_2):S414–S435. doi: 10.1161/CIR.0000000000000259. November 3. [DOI] [PubMed] [Google Scholar]
- 4.Kleinman M.E., Goldberger Z.D., Rea T. American heart association focused update on adult basic life support and cardiopulmonary resuscitation quality: an update to the American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2017;(1):137. doi: 10.1161/CIR.0000000000000539. 2018;January 2. [DOI] [PubMed] [Google Scholar]
- 5.Tsitlik J.E., Weisfeldt M.L., Chandra N. Elastic properties of the human chest during cardiopulmonary resuscitation. Crit Care Med. 1983;11(9):685–692. doi: 10.1097/00003246-198309000-00003. September. [DOI] [PubMed] [Google Scholar]
- 6.Krischer J.P., Fine E.G., Davis J.H. Complications of cardiac resuscitation. Chest. 1987;92(2):287–291. doi: 10.1378/chest.92.2.287. August 1. [DOI] [PubMed] [Google Scholar]
- 7.Hoke R.S., Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation. 2004;63(3):327–338. doi: 10.1016/j.resuscitation.2004.05.019. December. [DOI] [PubMed] [Google Scholar]
- 8.Black C.J., Busuttil A., Robertson C. Chest wall injuries following cardiopulmonary resuscitation. Resuscitation. 2004;63(3):339–343. doi: 10.1016/j.resuscitation.2004.07.005. December. [DOI] [PubMed] [Google Scholar]
- 9.Wininger K.L. Chest compressions: biomechanics and injury. Radiol Technol. 2007;78(4):269–274. April. [PubMed] [Google Scholar]
- 10.Kralj E., Podbregar M., Kejžar N. Frequency and number of resuscitation related rib and sternum fractures are higher than generally considered. Resuscitation. 2015;93:136–141. doi: 10.1016/j.resuscitation.2015.02.034. August 1. [DOI] [PubMed] [Google Scholar]
- 11.Schulze C., Hoppe H., Schweitzer W. Rib fractures at postmortem computed tomography (PMCT) validated against the autopsy. Forensic Sci Int. 2013;233(1):90–98. doi: 10.1016/j.forsciint.2013.08.025. December 10. [DOI] [PubMed] [Google Scholar]
- 12.Smekal D., Hansen T., Sandler H. Comparison of computed tomography and autopsy in detection of injuries after unsuccessful cardiopulmonary resuscitation. Resuscitation. 2013;84(3):357–360. doi: 10.1016/j.resuscitation.2012.06.023. March. [DOI] [PubMed] [Google Scholar]
- 13.Peberdy Mary Ann, Callaway Clifton W., Neumar Robert W. Part 9: post–cardiac arrest care. Circulation. 2010;122(18_suppl_3):S768–S786. doi: 10.1161/CIRCULATIONAHA.110.971002. November 2. [DOI] [PubMed] [Google Scholar]
- 14.Callaway Clifton W., Donnino Michael W., Fink Ericka L. Part 8: post–cardiac arrest care. Circulation. 2015;132(18_suppl_2):S465–S482. doi: 10.1161/CIR.0000000000000262. November 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oschatz E., Wunderbaldinger P., Sterz F. Cardiopulmonary resuscitation performed by bystanders does not increase adverse effects as assessed by chest radiography. Anesth Analg. 2001;93(1):128–133. doi: 10.1097/00000539-200107000-00027. July. [DOI] [PubMed] [Google Scholar]
- 16.Neumar Robert W., Nolan Jerry P., Christophe Adrie. Post–cardiac arrest syndrome. Circulation. 2008;118(23):2452–2483. doi: 10.1161/CIRCULATIONAHA.108.190652. December 2. [DOI] [PubMed] [Google Scholar]
- 17.Kim E.Y., Yang H.J., Sung Y.M. Multidetector CT findings of skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation. 2011;82(10):1285–1288. doi: 10.1016/j.resuscitation.2011.05.023. October. [DOI] [PubMed] [Google Scholar]
- 18.Kim M.J., Park Y.S., Kim S.W. Chest injury following cardiopulmonary resuscitation: a prospective computed tomography evaluation. Resuscitation. 2013;84(3):361–364. doi: 10.1016/j.resuscitation.2012.07.011. March. [DOI] [PubMed] [Google Scholar]
- 19.Viniol S, Thomas RP, König AM, et al.: Early whole-body CT for treatment guidance in patients with return of spontaneous circulation after cardiac arrest. Emerg Radiol. doi: 10.1007/s10140-019-01723-x (Epub ahead of print). [DOI] [PubMed]
- 20.Yamaguchi R., Makino Y., Chiba F. Frequency and influencing factors of cardiopulmonary resuscitation-related injuries during implementation of the American Heart Association 2010 Guidelines: a retrospective study based on autopsy and postmortem computed tomography. Int J Leg Med. 2017;131(6):1655–1663. doi: 10.1007/s00414-017-1673-8. November. [DOI] [PubMed] [Google Scholar]
- 21.Kashiwagi Y., Sasakawa T., Tampo A. Computed tomography findings of complications resulting from cardiopulmonary resuscitation. Resuscitation. 2015;88:86–91. doi: 10.1016/j.resuscitation.2014.12.022. March 1. [DOI] [PubMed] [Google Scholar]
- 22.Chapman B.C., Overbey D.M., Tesfalidet F. Clinical utility of chest computed tomography in patients with rib fractures CT chest and rib fractures. Arch Trauma Res. 2016;5(4) doi: 10.5812/atr.37070. December. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lederer W., Mair D., Rabl W. Frequency of rib and sternum fractures associated with out-of-hospital cardiopulmonary resuscitation is underestimated by conventional chest X-ray. Resuscitation. 2004;60(2):157–162. doi: 10.1016/j.resuscitation.2003.10.003. February. [DOI] [PubMed] [Google Scholar]
- 24.Yang K.-M., Lynch M., O’Donnell C. “Buckle” rib fracture: an artifact following cardio-pulmonary resuscitation detected on postmortem CT. Leg Med. 2011;13(5):233–239. doi: 10.1016/j.legalmed.2011.05.004. September. [DOI] [PubMed] [Google Scholar]
- 25.Dunham G.M., Perez-Girbes A., Bolster F. Use of whole body CT to detect patterns of CPR-related injuries after sudden cardiac arrest. Eur Radiol. 2018;28(10):4122–4127. doi: 10.1007/s00330-017-5117-0. October. [DOI] [PubMed] [Google Scholar]
- 26.Betz S., Sassen M., Beutel B. Pneumothorax in out-of-hospital resuscitation: the need for early diagnostics in a cardiac arrest center. Resuscitation. 2018;130:e3. September 1. [Google Scholar]
- 27.Kürkciyan I., Meron G., Sterz F. Pulmonary embolism as a cause of cardiac arrest: presentation and outcome. Arch Intern Med. 2000;160(10):1529–1535. doi: 10.1001/archinte.160.10.1529. May 22. [DOI] [PubMed] [Google Scholar]
- 28.Stein P.D., Henry J.W. Prevalence of acute pulmonary embolism among patients in a general hospital and at autopsy. Chest. 1995;108(4):978–981. doi: 10.1378/chest.108.4.978. October. [DOI] [PubMed] [Google Scholar]
- 29.Böttiger B.W., Arntz H.-R., Chamberlain D.A. Thrombolysis during resuscitation for out-of-hospital cardiac arrest. N Engl J Med. 2008;359(25):2651–2662. doi: 10.1056/NEJMoa070570. December 18. [DOI] [PubMed] [Google Scholar]
- 30.Javaudin F., Lascarrou J.-B., Bastard Q.L. Thrombolysis during resuscitation for out-of-hospital cardiac arrest caused by pulmonary embolism increases 30-day survival: findings from the French national cardiac arrest registry. Chest. 2019;156(6):1167–1175. doi: 10.1016/j.chest.2019.07.015. December 1. [DOI] [PubMed] [Google Scholar]
- 31.Bougouin W., Marijon E., Planquette B. Pulmonary embolism related sudden cardiac arrest admitted alive at hospital: management and outcomes. Resuscitation. 2017;115:135–140. doi: 10.1016/j.resuscitation.2017.04.019. June 1. [DOI] [PubMed] [Google Scholar]
- 32.Hess E.P., Campbell R.L., White R.D. Epidemiology, trends, and outcome of out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation. 2007;72(2):200–206. doi: 10.1016/j.resuscitation.2006.06.040. February 1. [DOI] [PubMed] [Google Scholar]
- 33.Bitto T., Mannion J.D., Stephenson L.W. Pneumothorax during positive-pressure mechanical ventilation. J Thorac Cardiovasc Surg. 1985;89(4):585–591. April. [PubMed] [Google Scholar]
- 34.Tocino I.M., Miller M.H., Fairfax W.R. Distribution of pneumothorax in the supine and semirecumbent critically ill adult. AJR Am J Roentgenol. 1985;144(5):901–905. doi: 10.2214/ajr.144.5.901. May. [DOI] [PubMed] [Google Scholar]
- 35.Steier M., Ching N., Roberts E.B. Pneumothorax complicating continuous ventilatory support. J Thorac Cardiovasc Surg. 1974;67(1):17–23. January. [PubMed] [Google Scholar]
- 36.Chan S.S.W. Emergency bedside ultrasound to detect pneumothorax. Acad Emerg Med. 2003;10(1):91–94. doi: 10.1111/j.1553-2712.2003.tb01984.x. [DOI] [PubMed] [Google Scholar]
- 37.Röthlin M.A., Näf R., Amgwerd M. Ultrasound in blunt abdominal and thoracic trauma. J Trauma. 1993;34(4):488–495. doi: 10.1097/00005373-199304000-00003. April. [DOI] [PubMed] [Google Scholar]
- 38.Stengel D., Leisterer J., Ferrada P. Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev. 2018;12 doi: 10.1002/14651858.CD012669.pub2. 12:CD012669. [DOI] [PMC free article] [PubMed] [Google Scholar]