Abstract
Objective
To assess knowledge of female and male fertility among students enrolled in a Master of Business Administration (MBA) program.
Design
Web-based cross-sectional survey.
Setting
Academic setting.
Patient(s)
Not applicable.
Intervention(s)
None.
Main Outcome Measure(s)
Knowledge of how female and male age impacts reproduction, fecundability, and success rates with in vitro fertilization (IVF).
Result(s)
A total of 133 female and male MBA students completed the survey. Nearly 10% of participants were not aware that women are born with a fixed number of oocytes and that oocyte quantity and quality decline with age. More than 30% of participants overestimated fecundability in women aged ≥35 years, and >50% overestimated IVF success rates in women older than 40 years. Fifteen percent of participants did not know that men have stem cells in the testes, and >25% were not aware that men experience a decrease in sperm concentration and quality with age. Nearly 30% believed that a man’s age never impacts reproductive outcomes. Less than 30% of participants correctly estimated fecundability and IVF success rates based on male age.
Conclusion(s)
These data highlight important knowledge gaps in a highly educated group of MBA students, most whom desire future childbearing. Specifically, there is a lack of understanding of both male and female reproductive aging and an overestimation of treatment success. As delayed childbearing continues, particularly among those with high educational attainment, attention should be focused on introducing broad fertility education at a younger age to improve future reproductive success.
Key Words: Fertility knowledge, female fertility, male fertility, reproductive aging, delayed childbearing
Discuss: You can discuss this article with its authors and other readers at https://www.fertstertdialog.com/posts/xfre-d-20-00084
Attention to fertility has increased significantly in recent years, largely fueled by the trend toward delayed childbearing (1). The ability to pursue planned oocyte cryopreservation has factored into the growing interest and has promoted increasing media attention (2, 3). This growing interest does not ensure that all individuals possess an accurate understanding of reproductive aging, and misinformation is common (1, 4, 5). Data suggest that some individuals do have reasonable knowledge regarding the relationship between female age and fertility. However, other studies (2, 5, 6, 7, 8) have demonstrated that there is a limited understanding of this correlation, and that the success rate of fertility treatment is often overestimated. Much focus has been on female age and fertility, with few studies (9, 10, 11) examining knowledge of male fertility. The data that do exist demonstrate that there is also a limited understanding of how male factors impact reproductive success, and studies (12, 13, 14) specifically examining the relationship between male age and fertility are scarce.
Parental age is increasing and an accurate understanding of how age impacts female and male fertility is critical. From 2007 to 2017, the mean female age at first birth in large metropolitan counties in the United States increased from 25.9 to 27.7 years old (15). Similarly, the rate of men having children in their thirties declined, and birth rates among men in their forties increased nearly 30% (16). In parallel with this increase in parental age, the proportion of women who are using in vitro fertilization (IVF) continues to be highest in women of advanced maternal age. In 2017, >70,000 women aged ≥35 years underwent IVF using their own eggs (approximately 60% of the total IVF population) and nearly 21,000 of these women were >40 years old (17).
It is anticipated that the trend toward delayed childbearing, increased infertility, and possible consequential need to use assisted reproductive technology (ART) will continue (1). This seems especially likely in individuals pursuing higher education and career advancement, as these individuals may elect to hold on starting a family until they complete their studies and settle into their careers (3, 5, 7, 18, 19). Examining fertility knowledge and identifying knowledge gaps in those individuals pursuing higher education is essential. The aim of the present study was to assess knowledge of female and male fertility among highly educated graduate students outside of the medical field who may delay childbearing due to educational and career pursuits.
Materials and methods
Survey
A web-based survey was developed using Research Electronic Data Capture (REDCap) by a research team, which included two board certified reproductive and infertility physicians. The survey was administered using REDCap and was completed online. Participants were asked about demographic information as well as pregnancy history and childbearing goals. The questions included 18 items related to female fertility and 14 items related to male fertility. The 32 fertility knowledge questions can be found in the Supplemental Appendix (available online). These questions asked participants to assess the likelihood of pregnancy per month with properly timed intercourse, as well as the likelihood of success in a single cycle of IVF treatment. The questions assessed fecundability and IVF success rates when female age varied yet male age remained constant at <35 years, as well as when male age varied yet female age remained constant at <35 years. The proportion of participants answering correctly for each of the fertility knowledge questions was calculated. The proportion of participants who answered incorrectly was grouped based on whether fecundability and IVF success rates were underestimated or overestimated.
Participants
This study was deemed exempt by the Institutional Review Board at Northwestern University. Participants included students enrolled in the Master of Business Administration (MBA) program at the Kellogg School of Management at Northwestern University. Kellogg has a Health Club where the students select areas of interest and opportunity and they invite speakers to the graduate school to give lectures. The students invited faculty from the division of Reproductive Endocrinology and Infertility and in advance of the meeting, this anonymous survey was distributed by e-mail to all students enrolled in the MBA program.
Statistical Analyses
Survey results were collected in REDCap. Descriptive statistics were compiled and analyzed. Proportions are presented for categorical variables. Means with standard deviations are presented for continuous variables. The results related to fecundability and IVF success rates were converted into groups, as follows: correct, underestimation, and overestimation. The χ2 tests were performed to compare proportion of participants who provided correct answers or underestimated or overestimated fecundability and IVF success rates. A P value of <.05 was deemed statistically significant. Statistical analyses were performed with SPSS (PASW version 21).
Results
Demographics
The survey was completed by 133 MBA students (103 women, 30 men) with a mean age of 29.5 years. The response rate was 11.1%. As shown in Table 1, most participants were white United States citizens who spoke English as their primary language. Approximately three quarters were married or in a committed relationship and >95% were heterosexual. Less than 5% reported having children, but 83% of those with children had a history of infertility and used medical assistance to achieve a pregnancy. Over 95% of childless individuals reported a desire to have children in the future.
Table 1.
Demographics (N=133)
| Sex at birth | % |
| Female | 77.4% |
| Male | 22.6% |
| Age, mean (SD) | 28.9 (2.22) |
| Racial background | |
| White | 66.9% |
| Black | 5.4% |
| Asian | 20.8% |
| Mixed race | 5.4% |
| Other | 1.5% |
| Primary language | |
| English | 85.3% |
| Other | 14.7% |
| Citizenship | |
| US | 81.9% |
| Other | 18.1% |
| Sexual orientation | |
| Heterosexual | 96.2% |
| Homosexual | 3.0% |
| Bisexual | 0.8% |
| Relationship status | |
| Married | 35.4% |
| Committed relationship | 40.0% |
| Single | 24.6% |
| Current child status | |
| Have children | 4.5% |
| Used medical assistance to achieve a pregnancy | 3.8% |
| Desire children in future | 96.0% |
Relationship Between Age and Fertility
When queried about the age at which female fertility dramatically declines, almost 75% of participants answered age 35 years. Nearly 75% of participants reported that the oldest age a woman has conceived using her own eggs was ≥50 years, with a range of answers from age 40–73 years. When the impact of age on oocyte quantity and quality was assessed, 8.3% of participants believed that women continue to make oocytes as they age and that oocyte quality does not decrease with age. Just >10% believed that women have stem cells in the ovaries that allow for repletion of oocytes.
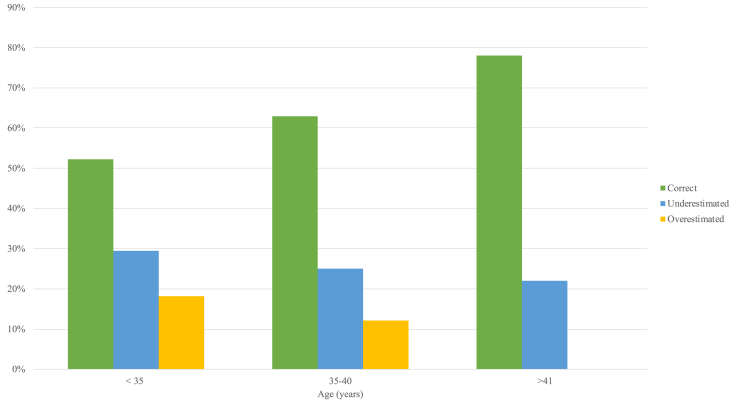
As shown in Figure 1, >50% of participants accurately estimated miscarriage rates. The proportion that accurately estimated miscarriage rates increased as women got older. When participants were incorrect, miscarriage rates were more commonly underestimated than overestimated. Nearly a third of participants stated that the miscarriage rate is 5% in women <35 years.
Figure 1.
Proportion of participants that correctly, overestimated, or underestimated miscarriage rates by female age.
When the impact of age on sperm quantity and quality was assessed, approximately 15% of participants did not believe that men have stem cells in the testes and just >25% of participants reported that men do not experience a decrease in sperm concentration or quality as they age. Nearly 30% stated that a man’s age never impacts reproductive outcomes, although approximately 10% of all participants believed that men stopped producing sperm somewhere between 55 and 75 years of age. More than 55% of participants reported that miscarriage rates did not increase as men age if their partner is <35 years old.
Estimated Fecundability by Age
One third of participants correctly estimated that 80% of couples aged <35 years would conceive after 1 year of attempting conception. The remainder of participants underestimated success with nearly 40% of participants reporting a 50% chance of pregnancy after 1 year of conception attempts.
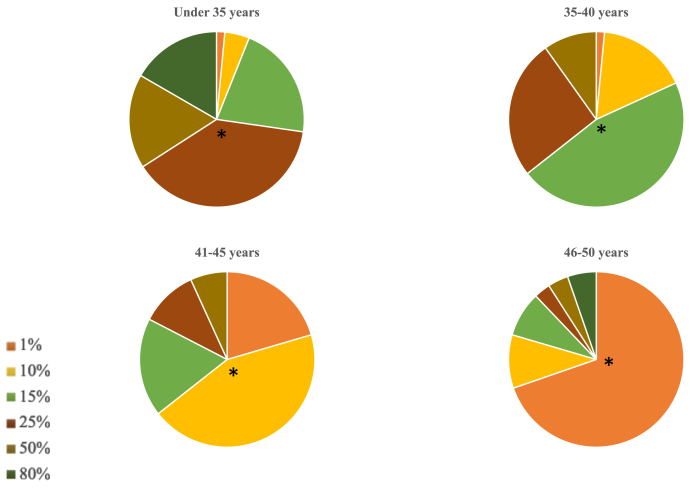
Participants estimated fecundability based on female age assuming a male age <35 years (Fig. 2) and based on male age assuming a female age <35 years (Supplemental Fig. 1, available online). Participants more accurately estimated fecundability as female age increased (Table 2). Alternatively, predicted fecundability by male age was estimated to be higher in the 35- to 40-year-old men compared with the 41- to 50-year-old men. When the percentage of participants who correctly estimated fecundability based on female and male ages were compared, in every age group more participants accurately estimated fecundability based on female age compared with fecundability based on male age.
Figure 2.
Proportion of participants that estimated fecundability rates of 1%, 10%, 15%, 25%, 50%, and 80% based on female age when male age was <35 years. ∗Correct response.
Table 2.
Estimated fecundability based on female and male age.
| Age (years) | Correctly estimated fecundability for females (male age <35 years) | Correctly estimated fecundability for males (female age <35 years) | P-value | Under-estimated fecundability for females (male age <35 years) | Under-estimated fecundability for males (female age <35 years) | P -value | Over-estimated fecundability for females (male age <35 years) | Over-estimated fecundability for males (female age <35 years) | P -value |
|---|---|---|---|---|---|---|---|---|---|
| 35-40 | 46.2%a | 28.5%d | <.05 | 18.2% | 32.4% | <.05 | 35.6% | 39.2% | .54 |
| 41-45 | 43.9%b | 20.8%d | <.05 | 20.5% | 47.7% | <.05 | 35.6% | 31.5% | .49 |
| 46-50 | 69.7%c | 23.1%d | <.05 | -- | 56.1% | -- | 30.3% | 20.8% | .08 |
Correct response 15%.
Correct response 10%.
Correct response 1%.
Correct response 25%.
The proportion of participants that underestimated fecundability was also assessed (Table 2). A slightly higher proportion of participants underestimated fecundability in women aged 41–45 years compared with 35- to 40-year olds. There were no participants who underestimated fecundability in the 46- to 50-year olds as the fecundability in this group is only 1%. As male age increased, the proportion of participants who underestimated fecundability increased with >55% of participants underestimating fecundability in males aged 46–50 years. When the proportion of participants who underestimated fecundability based on female and male age were compared, in both age groups there were significantly more participants who underestimated fecundability based on male age compared with fecundability based on female age.
The proportion of participants that overestimated fecundability was also assessed (Table 2). Participants (>30%) overestimated fecundability in all female age groups with more participants overestimating fecundability than underestimating it. Nearly 10% of participants estimated fecundability of >50% in women aged 46–50 years. As male age increased, the proportion of participants who overestimated fecundability decreased. When comparing the proportion of participants who overestimated fecundability based on female and male age, there were no significant differences.
Estimated IVF Success Rates by Age
Almost 30% of participants correctly estimated that 40% of couples <35 years of age will conceive after one IVF cycle. Participants (>45%) underestimated IVF success rates in this age group, whereas approximately 25% overestimated success rates.
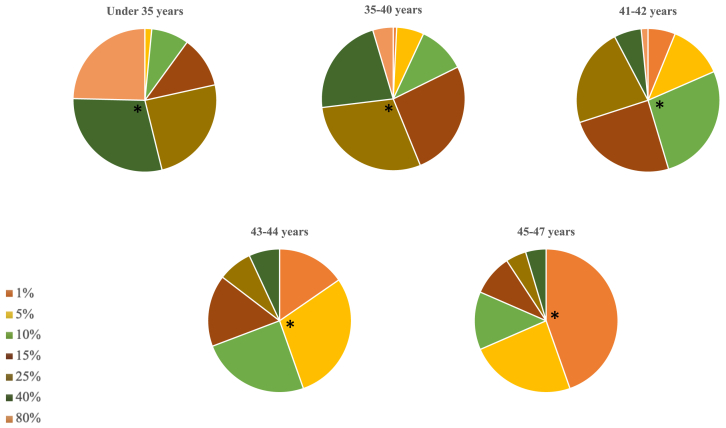
Participants (>25%) provided a correct response when they estimated IVF success rates by female age assuming a male age <35 years (Fig. 3). The highest proportion of participants that responded correctly occurred in estimation of success in women in the oldest age group (aged 45–47 years), although even in this group the proportion of participants that responded correctly was <50%. When estimating IVF success rates as male age increased, the percentage of participants that correctly responded decreased (Supplemental Fig. 2, available online). When the proportion of participants who correctly estimated IVF success rates based on female and male age were compared, the only age group where significantly more participants accurately estimated IVF success rates based on female age were women in the 45-47-year-old group (Table 3).
Figure 3.
Proportion of participants that estimated in vitro fertilization success rates of 1%, 5%, 10%, 15%, 25%, 40%, and 80% based on female age when male age was <35 years. ∗Correct response.
Table 3.
Estimated IVF success rates based on female and male age.
| Age (years) | Correctly estimated IVF success rates for females (male age <35 years) | Correctly estimated IVF success rates for males (female age <35 years) | P -value | Under-estimated IVF success rates for females (male age <35 years) | Under-estimated IVF success rates for males (female age <35 years) | P -value | Over-estimated IVF success rates for females (male age <35 years) | Over-estimated IVF success rates for males (female age <35 years) | P -value |
|---|---|---|---|---|---|---|---|---|---|
| 35-40 | 29.2%a | 29.2%e | 1.00 | 43.9% | 39.2% | .45 | 26.9% | 31.6% | .41 |
| 41-42 | 26.9%b | 25.4%e | .78 | 18.5% | 56.9% | <.05 | 54.6% | 17.7% | <.05 |
| 43-44 | 29.2%c | 20.8%e | .12 | 15.4% | 63.8% | <.05 | 55.4% | 15.4% | <.05 |
| 45-47 | 44.6%d | 13.1%e | <.05 | -- | 71.5% | -- | 55.4% | 15.4% | <.05 |
Correct response 25%.
Correct response 10%.
Correct response 5%.
Correct response 1%.
Correct response 40%.
As demonstrated in Table 3, the proportion of participants that underestimated IVF success rates was also assessed. As male age increased, the proportion of participants who underestimated IVF success rates increased. Participants (>70%) underestimated IVF success rates in males aged 45–47 years. A reverse trend occurred when female age increased, as fewer participants underestimated IVF success rates in the oldest female group. When the proportion of participants who underestimated IVF success rates based on female and male age were compared, there were significantly higher rates of underestimation based on male age of ≥41 years.
The proportion of participants that overestimated IVF success rates was also assessed (Table 3). As female age increased, the proportion of participants who overestimated IVF success rates increased with >50% of participants overestimating IVF success rates in women aged ≥41 years. Conversely, as male age increased, the proportion of participants who overestimated IVF success rates decreased. When the proportion of participants who overestimated IVF success rates based on female and male age were compared, there were significantly higher rates of overestimation based on women aged ≥41 years.
Discussion
It is imperative that those who delay childbearing understand how age impacts reproductive success. Previous studies (2, 5, 7, 18, 20) have examined fertility and fecundity knowledge in those pursuing educational advancement, specifically undergraduates, medical students and residents. However, there are few studies (18, 21) investigating baseline knowledge surrounding fertility in other groups of students outside of the medical field who are likely to delay childbearing, such as those pursuing graduate degrees. Limited data in graduate student populations suggest that fertility knowledge is average but that only a relatively small proportion feel well informed about fertility (18, 21). The MBA students are ideal to study given that they are a highly educated group who may be likely to delay childbearing due to career pursuits. These students are also unlikely to have received formal fertility education, thus making them more representative of the general population than those in the medical field.
The findings of our study highlight the important need for increased education about female and male reproductive aging and the likelihood of success with treatment. These data were captured from a population of graduate students in a highly competitive business school. The respondents demonstrated significant knowledge gaps.
Respondents did not understand several key concepts. Most notably they did not know that women are born with a fixed number of oocytes and the quantity and quality of oocytes decreases over time. Respondents (>10%) believed that women have stem cells in the ovaries, which allows for repletion of oocytes. When the impact of age on oocyte quantity and quality was assessed, 8.3% of participants believed that women continue to make oocytes as they age and that oocyte quality does not decrease with age. They also grossly overestimated a woman’s ability to have a child after the age of 45 years. Almost 75% of participants reported that a woman can still conceived using her own eggs at 50 years, with a range of answers up to age 73 years. The likelihood of conception was overestimated in all age groups, but especially in those >40 years. Surprisingly, nearly 10% of participants estimated fecundability of >50% in women aged 46–50 years. This false sense of reproductive security is likely one of several issues that contributes to delayed childbearing.
The second major gap identified was the overestimation of treatment success. Previous studies (6, 9, 22, 23) have demonstrated that there is a commonly held belief that IVF can overcome the age-related decline in fertility. Our results are concordant with published data. In our study 70% of respondents incorrectly estimated IVF success for women aged 35–40 years with 40% underestimating success and 30% overestimating success. More notable, however, was the perceived success rate in those >40 years with >50% overestimating treatment success in these age groups. The lack of transparency regarding the use of donor oocytes, especially in public domain, likely contributes to this pervasive knowledge gap.
The third major knowledge gap was how reproductive aging impacts men. One of the key reproductive differences between men and women is the presence of stem cells. Men have spermatogonial stem cells that allow for continuous production of sperm from puberty to death. Furthermore, during the past decade an association with age, environmental exposures, like tobacco, alcohol, and marijuana, and comorbidities of male obesity, diabetes, and hypertension, have emerged as risk factors for poor sperm quality (24). There also appears to be an association between sperm DNA fragmentation, recurrent pregnancy loss, and IVF failure (24). Paternal age has been shown to be a predictor of sperm morphology and motility, embryo development, and reproductive outcomes, as well as a marker overall male health (25, 26). Fifteen percent of participations did not believe that men have stem cells in the testes, and 26% of participants reported that men do not experience a decrease in sperm concentration or quality as they age. Nearly 30% stated that a man’s age never impacts reproductive outcomes, whereas 10% of participants believed that men stopped producing sperm somewhere between age 55 and 75 years. Less than 30% of participants correctly estimated fecundability and IVF success rates based on male age.
Although other studies (2, 5, 6, 18, 20, 21) have examined fertility knowledge in various groups of individuals, one of the strengths of this study is that female and male students’ knowledge about fertility in both sexes was assessed. Given that there has been a 20-fold increase in the number of women who obtain professional degrees during the past 40 years (18), it seems likely that women will continue to delay childbearing. This makes it critical that women, particularly those pursuing advanced degrees, understand reproductive aging and their own fertility. However, attention must also be paid to men given that they have a desire to parent as much as women do, but may also delay childbearing (9, 27, 28). Previous studies (10, 30) have demonstrated that men’s knowledge of their own fertility and ART is limited. Despite limited knowledge, men are interested in obtaining information about male fertility and reproductive health (10, 29). Fortunately attention to men’s health has increased in recent years, but it has not been established if this includes reproductive health (11) and universal guidelines regarding men’s preconception health are lacking (30). Our study highlights the importance of discussing and understanding male reproductive aging and health.
Another strength of this study is that we examined fertility knowledge in graduate students enrolled in a highly competitive MBA program. This is a unique population to evaluate given their aspirational educational and career goals. The mean age of the participants was 29.5 years, which is already older than the mean age of American women are at first birth, suggesting that this group of individuals may be more likely to delay childbearing. Other studies (18, 21) have examined fertility knowledge in those pursuing higher education, but to our knowledge, this is the first study to specifically examine female and male MBA students. Two previous studies (18, 21) of female graduate students also found significant knowledge deficits. Only about half of one of the well-educated cohorts knew when peak fertility occurs and when fertility begins to decline. Most participants believed that women retain their fertility at age 45 years (18). In the other study (21) of graduate students fertility knowledge was average, but >30% of those participants believed that a woman in her forties has a similar chance of pregnancy as a woman in her thirties. Three studies (2, 7, 31) examining residents in obstetrics and gynecology, another group of individuals likely to delay childbearing due to career pursuits, also found gaps in fertility knowledge. In one study (7) of >200 residents, almost 50% overestimated the age at which female fertility markedly declines and >75% overestimated success with ART. Another study (2) of female medical trainees also demonstrated that chances of success for natural and assisted conception were overestimated. Even third year residents had some knowledge gaps, and overestimated IVF success rates. A slightly smaller study (31) also found that nearly half of residents overestimated not only the age when fertility markedly declines, but also success with one IVF cycle. Our data add to the literature on fertility knowledge in well-educated individuals by demonstrating that female and male MBA students also have significant gaps in fertility knowledge.
One limitation of this study was the number of students included. Ideally, data would have been gathered from more individuals. However, it is possible that the students who elected to complete the survey may be most interested and invested in future fertility. If that holds true, those who participated may potentially have more knowledge than the average student, therefore if more students were included even larger knowledge gaps may be identified. Another limitation was that the survey was administered through the web, making it possible that students may have used outside resources to answer the questions, although they were asked not to do so. This would make accurate responses more likely, suggesting that actual knowledge may be even more limited. Finally, the demographics of the cohort were fairly homogenous, with most participants reporting they were white heterosexual women. Therefore, the results may not be applicable to MBA students universally.
The goal with disseminating these data is to understand the knowledge gaps related to female and male fertility in individuals who are at risk of delaying childbearing so that education can be tailored and reproductive success can be increased. Fortunately, data have demonstrated that education does increase fertility knowledge (32, 33) and that fertility awareness may also modify future reproductive outcomes (34). In one study (11) examining fertility awareness in men, there was a significant improvement after reproductive life plan-based counseling. More than 75% of the men who participated reported a positive experience. Furthermore, 95% believed that it was fairly or very important to educate young men about fertility and factors that can affect a healthy pregnancy. Another study (35) of childless men and women demonstrated that fertility and ART knowledge scores increased after online education. In that study it would have been informative to assess fertility knowledge after the lecture to determine whether this method of education improves short-term understanding of fertility. Unfortunately, these data are unavailable given that the students did not complete a survey after the lecture. Through previous studies (2, 5, 6, 18, 20, 21) and our work, it seems clear that targeted fertility education is necessary and, although additional insight is required to determine exactly how to best inform individuals, it does appear education is effective in improving fertility knowledge. It is unclear when the optimal time to introduce fertility education is, but providing middle school, high school, and possibly even college students with fertility education in tandem with sexual health education may be a strategy to consider. By educating female and male students in their earlier reproductive years, and potentially at multiple time points, it may be possible to better capture individuals before they have reached peak fertility, thus allowing for more time to make well informed reproductive decisions.
In conclusion, these data highlight important knowledge gaps in a highly educated group of MBA students at one of the nation’s most competitive business schools. Our data demonstrate a pervasive lack of understanding of male and female reproductive aging and an overestimation of treatment success. Broad education in the arena of fertility should be introduced at a younger age so that decision making regarding family building can be made proactively and based on biology.
Footnotes
L.A.B. has nothing to disclose. M.L. has nothing to disclose. M.A.K. has nothing to disclose. E.C.F. has nothing to disclose.
Supplementary data
Proportion of participants that estimated fecundability rates of 1%, 5%, 10%, 15%, 25%, 40% and 80% based on male age when female age <35 years
Proportion of participants that estimated IVF success rates of 1%, 5%, 10%, 15%, 25%, 40% and 80% based on male age when female age <35 years
References
- 1.Wyndham N., Marin Figueira P.G., Patrizio P. A persistent misperception: assisted reproductive technology can reverse the “aged biological clock.”. Fertil Steril. 2012;97:1044–1047. doi: 10.1016/j.fertnstert.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 2.Kudesia R., Chernyak E., McAvey B. Low fertility awareness in United States reproductive-aged women and medical trainees: creation and validation of the Fertility & Infertility Treatment Knowledge Score (FIT-KS) Fertil Steril. 2017;108:711–717. doi: 10.1016/j.fertnstert.2017.07.1158. [DOI] [PubMed] [Google Scholar]
- 3.Pedro J., Brandão T., Schmidt L., Costa M.E., Martins M.V. What do people know about fertility? A systematic review on fertility awareness and its associated factors. Ups J Med Sci. 2018;123:71–81. doi: 10.1080/03009734.2018.1480186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shao Y.H., Tulandi T., Abenhaim H.A. evaluating the quality and reliability of online information on social fertility preservation. J Obstet Gynaecol Can. 2020;42:561–567. doi: 10.1016/j.jogc.2019.10.029. [DOI] [PubMed] [Google Scholar]
- 5.Lampic C., Svanberg A.S., Karlström P., Tydén T. Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Hum Reprod. 2006;21:558–564. doi: 10.1093/humrep/dei367. [DOI] [PubMed] [Google Scholar]
- 6.Peterson B.D., Pirritano M., Tucker L., Lampic C. Fertility awareness and parenting attitudes among American male and female undergraduate university students. Hum Reprod. 2012;27:1375–1382. doi: 10.1093/humrep/des011. [DOI] [PubMed] [Google Scholar]
- 7.Yu L., Peterson B., Inhorn M.C., Boehm J.K., Patrizio P. Knowledge, attitudes, and intentions toward fertility awareness and oocyte cryopreservation among obstetrics and gynecology resident physicians. Hum Reprod. 2016;31:403–411. doi: 10.1093/humrep/dev308. [DOI] [PubMed] [Google Scholar]
- 8.García D., Brazal S., Rodríguez A., Prat A., Vassena R. Knowledge of age-related fertility decline in women: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2018;230:109–118. doi: 10.1016/j.ejogrb.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 9.Hammarberg K., Collins V., Holden C., Young K., McLachlan R. Men's knowledge, attitudes and behaviours relating to fertility. Hum Reprod Update. 2017;23:458–480. doi: 10.1093/humupd/dmx005. [DOI] [PubMed] [Google Scholar]
- 10.Daumler D., Chan P., Lo K.C., Takefman J., Zelkowitz P. Men's knowledge of their own fertility: a population-based survey examining the awareness of factors that are associated with male infertility. Hum Reprod. 2016;31:2781–2790. doi: 10.1093/humrep/dew265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodin M., Tydén T., Käll L., Larsson M. Can reproductive life plan-based counselling increase men's fertility awareness? Ups J Med Sci. 2018;123:255–263. doi: 10.1080/03009734.2018.1541948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunson D.B., Baird D.D., Colombo B. Increased infertility with age in men and women. Obstet Gynecol. 2004;103:51–56. doi: 10.1097/01.AOG.0000100153.24061.45. [DOI] [PubMed] [Google Scholar]
- 13.Baird D.T., Collins J., Egozcue J., Evers L.H., Gianaroli L., Leridon H. Fertility and ageing. Hum Reprod Update. 2005;11:261–276. doi: 10.1093/humupd/dmi006. [DOI] [PubMed] [Google Scholar]
- 14.Mazur D.J., Lipshultz L.I. Infertility in the aging male. Curr Urol Rep. 2018;19:54. doi: 10.1007/s11934-018-0802-3. [DOI] [PubMed] [Google Scholar]
- 15.Ely D.M.H.B. National Center for Health Statistics; Hyattsville, MD: 2018. Trends in fertility and mother’s age at first birth among rural and metropolitan counties: United States, 2007–2017. NCHS Data Brief, no 323.https://www.cdc.gov/nchs/products/databriefs/db323.htm#Suggested_citation Available at: [PubMed] [Google Scholar]
- 16.Harris I.D., Fronczak C., Roth L., Meacham R.B. Fertility and the aging male. Rev Urol. 2011;13:e184–e190. [PMC free article] [PubMed] [Google Scholar]
- 17.National Summary Report: All SART Member Clinics. Society for Assisted Reproductive Technology 2017. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?reportingYear=2017 Available at:
- 18.Hickman L.C., Fortin C., Goodman L., Liu X., Flyckt R. Fertility and fertility preservation: knowledge, awareness and attitudes of female graduate students. Eur J Contracept Reprod Health Care. 2018;23:130–138. doi: 10.1080/13625187.2018.1455085. [DOI] [PubMed] [Google Scholar]
- 19.Lundsberg L.S., Pal L., Gariepy A.M., Xu X., Chu M.C., Illuzzi J.L. Knowledge, attitudes, and practices regarding conception and fertility: a population-based survey among reproductive-age United States women. Fertil Steril. 2014;101:767–774. doi: 10.1016/j.fertnstert.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Hashiloni-Dolev Y., Kaplan A., Shkedi-Rafid S. The fertility myth: Israeli students' knowledge regarding age-related fertility decline and late pregnancies in an era of assisted reproduction technology. Hum Reprod. 2011;26:3045–3053. doi: 10.1093/humrep/der304. [DOI] [PubMed] [Google Scholar]
- 21.Stevenson E.L., Gispanski L., Fields K., Cappadora M., Hurt M. Knowledge and decision making about future fertility and oocyte cryopreservation among young women. Hum Fertil. 2019:1–10. doi: 10.1080/14647273.2018.1546411. [DOI] [PubMed] [Google Scholar]
- 22.Maheshwari A., Porter M., Shetty A., Bhattacharya S. Women's awareness and perceptions of delay in childbearing. Fertil Steril. 2008;90:1036–1042. doi: 10.1016/j.fertnstert.2007.07.1338. [DOI] [PubMed] [Google Scholar]
- 23.Daniluk J.C., Koert E., Cheung A. Childless women's knowledge of fertility and assisted human reproduction: identifying the gaps. Fertil Steril. 2012;97:420–426. doi: 10.1016/j.fertnstert.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 24.Halpern J.A., Brannigan R.E. Paternal health and perinatal morbidity: increasing evidence for the influence of paternity on fertility outcomes. Fertil Steril. 2020;113:925–926. doi: 10.1016/j.fertnstert.2020.01.032. [DOI] [PubMed] [Google Scholar]
- 25.Choy J.T., Eisenberg M.L. Male infertility as a window to health. Fertil Steril. 2018;110:810–814. doi: 10.1016/j.fertnstert.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 26.Kaarouch I., Bouamoud N., Madkour A., Louanjli N., Saadani B., Assou S. Paternal age: negative impact on sperm genome decays and IVF outcomes after 40 years. Mol Reprod Dev. 2018;85:271–280. doi: 10.1002/mrd.22963. [DOI] [PubMed] [Google Scholar]
- 27.Thompson R., Lee C. Sooner or later? Young Australian men's perspectives on timing of parenthood. J Health Psychol. 2011;16:807–818. doi: 10.1177/1359105310392091. [DOI] [PubMed] [Google Scholar]
- 28.Roberts E., Metcalfe A., Jack M., Tough S.C. Factors that influence the childbearing intentions of Canadian men. Hum Reprod. 2011;26:1202–1208. doi: 10.1093/humrep/der007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daniluk J.C., Koert E. The other side of the fertility coin: a comparison of childless men's and women's knowledge of fertility and assisted reproductive technology. Fertil Steril. 2013;99:839–846. doi: 10.1016/j.fertnstert.2012.10.033. [DOI] [PubMed] [Google Scholar]
- 30.Shawe J., Delbaere I., Ekstrand M., Hegaard H.K., Larsson M., Mastroiacovo P. Preconception care policy, guidelines, recommendations and services across six European countries: Belgium (Flanders), Denmark, Italy, the Netherlands, Sweden and the United Kingdom. Eur J Contracept Reprod Health Care. 2015;20:77–87. doi: 10.3109/13625187.2014.990088. [DOI] [PubMed] [Google Scholar]
- 31.Kemal Harzif A., Maidarti M., Silvia M., Mariana A., Dewi Mutia H., Wiweko B. Knowledge, attitude, intention, and religion aspect toward fertility preservation among obstetrics and gynecology residents in Indonesia: a cross-sectional study. Int J Reprod Biomed (Yazd) 2019;18:47–56. doi: 10.18502/ijrm.v18i1.6199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wojcieszek A.M., Thompson R. Conceiving of change: a brief intervention increases young adults' knowledge of fertility and the effectiveness of in vitro fertilization. Fertil Steril. 2013;100:523–529. doi: 10.1016/j.fertnstert.2013.03.050. [DOI] [PubMed] [Google Scholar]
- 33.Garcia D., Vassena R., Prat A., Vernaeve V. Increasing fertility knowledge and awareness by tailored education: a randomized controlled trial. Reprod Biomed Online. 2016;32:113–120. doi: 10.1016/j.rbmo.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 34.Maeda E., Boivin J., Toyokawa S., Murata K., Saito H. Two-year follow-up of a randomized controlled trial: knowledge and reproductive outcome after online fertility education. Hum Reprod. 2018;33:2035–2042. doi: 10.1093/humrep/dey293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daniluk J.C., Koert E. Fertility awareness online: the efficacy of a fertility education website in increasing knowledge and changing fertility beliefs. Hum Reprod. 2015;30:353–363. doi: 10.1093/humrep/deu328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Proportion of participants that estimated fecundability rates of 1%, 5%, 10%, 15%, 25%, 40% and 80% based on male age when female age <35 years
Proportion of participants that estimated IVF success rates of 1%, 5%, 10%, 15%, 25%, 40% and 80% based on male age when female age <35 years