Abstract
Objective
To examine current levels, correlates of, and changes in contraceptive use among reproductive-age women in the United States between 2014 and 2016.
Design
We conducted simple and multivariable logistic regression analyses to identify associations between user characteristics and contraceptive use, with specific attention to methods requiring a visit to a health care provider.
Setting
Not applicable.
Patient(s)
All self-identified female respondents to the surveys. Secondary analysis of two rounds of the National Survey of Family Growth, an in-home, nationally representative survey of people ages 15–44 years (2013–2015) and 15–49 years (2015–2017).
Intervention(s)
None.
Main Outcome Measure(s)
Current use of a contraceptive method, including use of individual methods and grouped method use in 2016, and change in use from 2014.
Result(s)
Contraceptive use remained steady between 2014 and 2016 among sexually active females not seeking pregnancy (88%). Among users, use of long-acting reversible contraceptive (LARC) methods increased from 14% to 18%, as use of short-acting reversible contraceptive (SARC) methods fell from 32% to 28%. Implant use among 15- to 19-year-olds rose from 6% to 16% and represents one of the largest increases observed. Access to sexual and reproductive health care was strongly associated with use of all LARC and SARC methods except for the implant (adjusted odds ratios ranged from 3.21 to 13.53).
Conclusion(s)
Contraceptive users are shifting primarily among the most and moderately effective method groups, and not from contraceptive nonuse to use. Reductions in access to sexual and reproductive health care could have implications for individuals’ ability to use their preferred contraceptive methods.
Key Words: Contraception, family planning, United States, demography
Highlights
-
•
Contraceptive use in the United States remained steady between 2014 and 2016.
-
•
Increases in use of long-acting reversible contraceptive methods paralleled a decrease in use of short-acting reversible contraceptive methods.
-
•
Contraceptive users are shifting primarily among the most and moderately effective method groups and not from contraceptive nonuse to use.
-
•
Access to sexual and reproductive health care is strongly associated with use of most long- and short-acting reversible contraception.
Introduction
Discuss: You can discuss this article with its authors and other readers at https://www.fertstertdialog.com/users/16110-fertility-and-sterility/posts/xfre-d-20-00063
In the United States, the average desired family size includes two children; to achieve this goal, individuals and their partners must spend approximately three decades trying to prevent pregnancy (1). During the reproductive years, overall contraceptive method use is ubiquitous among sexually active American women (2), and shifts in use between different methods within the overall method mix can have implications for several population-level reproductive health outcomes such as pregnancies, abortions, and births. Using contraception can help individuals to achieve some desired reproductive health outcomes, and population-level measures reflecting methods being used represent one metric, among many, that helps shed light on individuals’ ability to realize full reproductive autonomy.
Surveillance at the state and national level helps to illustrate whether state and federal policies may be facilitating or impeding access to contraception, a necessary prerequisite to contraceptive use for most methods. And identifying differences in specific method use among population groups can help determine whether additional programmatic or policy attention needs to be directed toward ensuring access to the full range of methods available for everyone. Patterns of contraceptive use vary considerably at the state level, likely related to varying contexts across states with regards to population demographics and differential support for contraceptive access (3). Two examples of federal initiatives that have helped individuals to access contraceptive methods for free or low out-of-pocket costs include the Affordable Care Act (ACA) and the Title X family planning program, a federally funded initiative since 1970 that prioritizes providing free or low-cost family planning care to low-income and young individuals (4, 5, 6).
Between 2008 and 2014, large shifts in the percentage of users of permanent contraception and long-acting reversible contraceptive (LARC) methods at the national level were documented, with an inverse relationship documented between rising use of LARC methods coinciding with falling rates of permanent contraception (7). More recent national-level data are now available that represent 2015–17, and new analyses of these data are needed to consider whether the contraceptive method mix in the population is relatively stable and, if not, whether any recent changes observed may be continuing longer-term trends that were previously documented (7). In addition, given recent federal efforts to undermine broad contraceptive access with regards to both the ACA and the Title X program (8, 9), these latest contraceptive use data can provide a baseline from which future shifts in use—overall and among methods—can be tracked.
This study examines overall contraceptive use and use of individual methods, focusing on the most recent national data from 2015 to 2017 and highlighting change between the periods of 2013 to 2015 and 2015 to 2017. Additionally, this study considers associations between demographic, sexual, and reproductive health characteristics of users and method use in 2015 to 2017 and examines changes in specific method use by these user characteristics between the past two rounds of data, from 2013 to 2015 to 2015 to 2017. Given the national attention on access to sexual and reproductive health care during the time period studied, this analysis helps to shed light on the relationship between this access and specific contraceptive method use across population groups.
Materials and Methods
This study uses publicly available cross-sectional data from the 2013 to 2015 and 2015 to 2017 female respondent files of the National Survey of Family Growth (NSFG). All NSFG respondents self-report their current gender at the time of interview, which determines the questionnaire they are routed into. The NSFG conducts in-home, face-to-face interviews of a nationally representative sample of people of reproductive age, including those living in college dormitories, fraternities, or sororities, oversampling black and Hispanic teenagers ages 15 to 19 years-old. As such, the NSFG provides the most comprehensive, deidentified data on contraceptive use in the United States. The data and more detailed information on survey methodology, sample design, response rates, fieldwork procedures, and variance estimation are available on the NSFG website (10). Given the deidentified nature of the public-use data in the data set, our organization’s institutional review board (Department of Health and Human Services identifier IRB00002197) determined that this analysis was exempt from institutional review board approval.
The NSFG data were weighted to reflect the U.S. reproductive-age female civilian population for each of the 2-year time spans, that is, September 2013 to September 2015 and September 2015 to September 2017. Analyses are presented at the midpoint of each time period (2014 and 2016) as a reference year. The sample consists of 5,699 and 4,886 female respondents ages 15 to 44, from the 2013 to 2015 and 2015 to 2017 surveys, respectively. The 2015 to 2017 NSFG included an additional 668 female respondents ages 45 to 49 at the time of screening; these individuals were included only in analyses of 2015 to 2017 method use and not in any analyses of change between the two time periods.
The analysis considered current use and nonuse of contraception in 2014 and 2016, as well as changes in use and nonuse between 2014 and 2016, among three populations: all reproductive-age women, sexually active reproductive-age women not seeking pregnancy, and sexually active reproductive-age women who reported current contraceptive use. Among the last population of contraceptive users, we examined use of specific contraceptive methods and groups of methods in 2014 and 2016, as well as changes in method use between 2014 and 2016. In previous analyses (7), we identified the population of sexually active reproductive-age women not seeking pregnancy as those who were “at risk for unintended pregnancy.” The population described in this current analysis is identified using the same criteria as in past analyses (women who were sexually active in the 3 months before interview who were not pregnant or trying to conceive and who were not sterile for noncontraceptive reasons), but we have updated our terminology to more accurately reflect the text used in the survey. Given no change over time in either the proportion of sexually active reproductive-age women not seeking pregnancy or contraceptive use among this population, we focus our analyses, examining use of specific methods and groups and change in use of these between the time periods on the narrower population of sexually active reproductive-age women who reported current contraceptive use.
Current contraceptive use is defined as the most effective method respondents reported using during the month of the interview, as represented by the CONSTAT1 recode in the NSFG data set. Of note, due to this prioritization of a method based on effectiveness (11), use of more than one method is not reflected in these analyses. Methods represented in this analysis include female permanent contraception (tubal ligation, Essure [Bayer], etc.), male permanent contraception (vasectomy), intrauterine device (IUD), implant, pill, patch, ring, injectable, condom, withdrawal, natural family planning, and other coitus-dependent methods (diaphragm, foam, sponge, suppositories, and jellies). The natural family planning category includes periodic abstinence, cervical mucus test or temperature rhythm, and calendar rhythm. Due to small numbers of respondents reporting patch, ring, or injectable use, we grouped these together as nonpill short-acting reversible contraceptive (SARC) methods. We also created additional method groups: permanent methods (female and male), LARC methods (IUDs and implants), and SARC methods (pills, patch, ring, and injectables). Respondents who indicated that they were sterile by noncontraceptive surgical or nonsurgical means were not included in this analysis.
Method use was considered across demographic, sexual, and reproductive health characteristics that may be associated with contraceptive use. Such characteristics include age at the time of interview (for consistency with past analyses of contraceptive use), race and ethnicity, income as a percentage of the federal poverty level, nativity, education, relationship status, health insurance coverage, parity, and future births expected. Due to low response rates on items asking about sexual orientation and sexual attraction, we included respondents’ lifetime experience of same-sex behavior (ever having given or received oral sex from, or having ever had any sexual contact with, a female). We considered respondents’ source of reproductive health care in the past 12 months, which included having received any of the following services in the past 12 months: a birth control checkup, a Pap test, or a pelvic exam. For individuals who reported more than one source of reproductive health care, we prioritized first the receipt of care at Title X clinics, then care at any other public clinic, followed by care from any private provider. We also considered individuals’ current insurance coverage, prioritizing first private sources of coverage including Medi-Gap, then Medicaid, Children’s Health Insurance Program and state-sponsored health plans, then other public coverage including Medicare and military health care in cases where respondents indicated more than one type of coverage. Coverage through a single service plan or only Indian Health Service was grouped with no coverage, according to the NSFG recode documents. Finally, we created a variable that represented any access to reproductive health care, conceptualized as a combination of actual receipt of care and a means of covering the cost for care. Individuals who reported neither receiving any form of reproductive health care in the past year nor having any type of current health insurance coverage were considered as those without access. Those who either received any type of reproductive health care in the past year or had any type of current health insurance coverage were considered to have access to reproductive health care.
We tabulated three sets of statistics for 2014 and for 2016: the percentage of all women who used and did not use any method, the percentage of sexually active women not seeking pregnancy who used and did not use any method, and the percentage of method users by method type and demographic, sexual, and reproductive health characteristics. To examine changes in contraceptive use between the two time points, we conducted simple logistic regression analyses to test for significant differences between 2014 and 2016 in the percentages of use overall and within method groups and specific methods. Differences in method use between 2014 and 2016 that were significant at P < .05 are shown in the tables, but, for changes in method use by characteristics between the time points, we prioritize differences significant at P ≤ .01 and those for which there is strong literature to support interpretation of the findings. Supplemental Table 1 (available online) presents findings for use by demographic and reproductive characteristics for method groups for which there was no overall significant change between the two time periods examined, including permanent methods and coitus-dependent methods.
For individual and grouped methods for which there was significant change between 2014 and 2016, we used multivariable logistic regression to estimate adjusted odds ratios for the relationship among demographic, sexual, and reproductive health characteristics and each of these contraceptive methods or method groups in 2016. We began building each model with all independent variables, then conducted a backward stepwise elimination process using Wald tests for each independent variable at P > .1 in the full model to determine whether its exclusion affected the model. Variables were omitted from the model if the Wald test was not significant at P < .05; all models include age, race and ethnicity, and poverty status regardless of significance due to their theoretical relevance to the outcomes. Age was collapsed into four categories for the multivariable models due to small cell sizes. Associations in the final multivariable models were considered significant at the P < .05 level. All analyses were conducted using the “svy” command prefix within Stata 15.1 to account for the NSFG's use of a multistage probability sample.
Results
In 2016, female permanent contraception and oral contraceptive pills were the most commonly used methods among women in the United States, each at about 22% of all users, with condoms (15%) and IUDs (14%) representing the next most popular methods. Between 2014 and 2016, the overall prevalence of contraceptive use remained fairly stable, with just over 60% of all women and almost 90% of sexually active women not seeking pregnancy reporting use of a contraceptive method (Table 1). There were, however, some significant changes in the type of methods employed by contraceptive users. The percentage of contraceptive users relying on a LARC method increased from 14.3% in 2014 to 17.8% in 2016 (P < .05), while the increase in implants rose from 2.6% to 4.3% (P < .05), playing a dominant role in the overall increase in LARC methods. In contrast, the percentage of contraceptive users relying on any SARC method decreased from 31.8% in 2014 to 27.7% in 2016 (P < .05). There was a significant decrease in use of other coital methods, such as diaphragm, foam, sponge, suppositories, jellies, and creams during this time frame; however, given the small sample sizes for users of these methods, results from this particular significance test may be unstable and should be interpreted with caution.
Table 1.
Changes in contraceptive use and method mix between 2014 and 2016 among all women ages 15 to 44, sexually active women ages 15 to 44 not seeking pregnancy, and women ages 15 to 44 using contraception.
| Variable | 2014 (n = 5,699; weighted N = 61,491,766) | 2016 (n = 4,886; weighted N = 61,799,158) |
|---|---|---|
| Among all women | ||
| Not using contraception | 38.6 | 36.5 |
| Using contraception | 61.4 | 63.5 |
| Among sexually active women not seeking pregnancya | ||
| Not using contraception | 11.5 | 12.0 |
| Using contraception | 88.5 | 88.0 |
| Among contraceptive users | ||
| Any permanent method | 28.2 | 29.7 |
| Female permanent contraception | 21.8 | 22.4 |
| Vasectomy | 6.5 | 7.3 |
| LARC method | 14.3 | 17.8∗ |
| IUD | 11.8 | 13.5 |
| Implant | 2.6 | 4.3∗ |
| SARC method | 31.8 | 27.7∗ |
| Pill | 25.3 | 21.9 |
| Nonpill SARC methodb | 6.5 | 5.8 |
| Any coitus-dependent method | 25.1 | 24.5 |
| Condom | 14.5 | 15.2 |
| Withdrawal | 8.1 | 6.9 |
| Natural family planning | 2.2 | 2.4 |
| Other coitus-dependent methodsc | 0.6 | 0.1∗ |
Note: Data presented as percentages. Survey years in column headings represent the midpoint of data collection years for each of the two National Survey of Family Growth (NSFG) surveys. Population includes all female respondents ages 15 to 44 years, weighted to reflect the U.S. female civilian population. LARC = long-acting reversible contraception; IUD = intrauterine device; SARC = short-acting reversible contraception.
Sexually active women not seeking pregnancy includes female respondents who had had sexual intercourse in the 3 months before interview, who were not pregnant or trying to conceive, and who were not sterile for noncontraceptive reasons.
Other nonpill SARC methods include the contraceptive patch, the vaginal ring, and the medroxyprogesterone injectable.
Other coitus-dependent methods include the diaphragm, foam, sponge, suppositories, jelly/cream, and “other methods” as indicated by the CONSTAT1 variable (contraceptive status recode prioritizing most effective method reported having been used during the month of the interview) in the NSFG documentation.
Indicates significant difference between the years at P < .05.
Mirroring the pattern of no significant change in overall contraceptive method use among all sexually active women not seeking pregnancy as shown in Table 1, there were few significant changes in overall contraceptive method use by demographic, sexual, and reproductive health characteristics among this population (Table 2). One exception was a significant decrease in overall contraceptive use among sexually active young adults ages 20–24 not seeking pregnancy, from 90% to 83% (P < .05).
Table 2.
Changes in contraceptive use among sexually active women ages 15-44 not seeking pregnancy and changes in selected method use among women ages 15-44 using contraception, by demographic, sexual and reproductive health characteristics, between 2014 and 2016.
| Among Those at Risk for Pregnancya (N 2014=3,325, N2016=2,895) |
Among All Contraceptive Users (N 2014=3,307, N 2016=2,888) |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any Method Use |
LARC Methods |
IUD |
Implant |
SARC Methods |
Pill |
Non-pill SARC methodsb |
|||||||||||||||
| 2014 | 2016 | 2014 | 2016 | 2014 | 2016 | 2014 | 2016 | 2014 | 2016 | 2014 | 2016 | 2014 | 2016 | ||||||||
| Overall Use | 88.5 | 88.0 | 14.3 | 17.8∗ | 11.8 | 13.5 | 2.6 | 4.3∗ | 31.8 | 27.7∗ | 25.3 | 21.9 | 6.5 | 5.8 | |||||||
| Use by Demographic | |||||||||||||||||||||
| Age | |||||||||||||||||||||
| 15-19 | 80.8 | 83.4 | 9.8 | 22.2∗ | 3.5 | 5.7 | 6.3 | 16.4∗ | 66.7 | 58.5 | 49.0 | 44.7 | 17.7 | 13.8 | |||||||
| 20-24 | 90.0 | 82.7∗ | 18.6 | 17.9 | 12.7 | 9.6 | 5.9 | 8.2 | 51.7 | 45.0 | 42.4 | 38.3 | 9.3 | 6.6 | |||||||
| 25-29 | 88.6 | 90.5 | 18.7 | 24.0 | 14.5 | 19.1 | 4.2 | 4.9 | 36.2 | 32.5 | 30.0 | 25.7 | 6.2 | 6.8 | |||||||
| 30-34 | 88.1 | 91.4 | 15.8 | 15.3 | 15.3 | 13.7 | 0.5 | 1.6 | 25.6 | 24.4 | 20.2 | 19.3 | 5.5 | 5.1 | |||||||
| 35-39 | 90.3 | 88.9 | 14.1 | 17.1 | 13.7 | 15.5 | 0.4 | 1.6∗ | 18.2 | 16.2 | 13.0 | 11.0 | 5.1 | 5.2 | |||||||
| 40-44 | 88.2 | 87.3 | 6.9 | 12.9∗ | 6.6 | 12.7∗ | 0.3 | 0.2 | 11.9 | 9.3 | 10.4 | 7.5 | 1.5 | 1.7 | |||||||
| 45-49 | NA | 87.1 | NA | 5.6 | NA | 5.5 | NA | 0.2 | NA | 7.8 | NA | 6.5 | NA | 1.3 | |||||||
| Poverty status, % | |||||||||||||||||||||
| <100 federal poverty level | 85.8 | 85.5 | 15.9 | 19.6 | 12.1 | 11.3 | 3.8 | 8.3† | 26.0 | 25.4 | 17.8 | 18.5 | 8.2 | 6.9 | |||||||
| 100-199 | 87.8 | 83.2 | 15.2 | 17.0 | 13.2 | 12.7 | 2.0 | 4.3 | 31.4 | 22.6∗ | 21.5 | 15.0 | 9.9 | 7.6 | |||||||
| 200-299 | 90.6 | 91.4 | 15.7 | 17.8 | 12.6 | 12.4 | 3.1 | 5.4 | 32.1 | 27.6 | 28.1 | 21.2 | 4.0 | 6.3 | |||||||
| 300+ or higher | 89.7 | 90.8 | 12.1 | 17.2∗ | 10.4 | 15.6∗ | 1.7 | 1.6 | 36.1 | 31.9 | 31.4 | 27.8 | 4.7 | 4.0 | |||||||
| Race/ethnicity | |||||||||||||||||||||
| White, non-Hispanic | 90.2 | 89.0 | 13.2 | 18.1∗ | 11.0 | 14.2 | 2.2 | 3.9 | 34.8 | 29.6 | 29.6 | 25.2 | 5.2 | 4.4 | |||||||
| Black, non-Hispanic | 84.0 | 84.4 | 15.1 | 17.0 | 12.0 | 11.5 | 3.1 | 5.4 | 32.0 | 28.9 | 19.8 | 15.8 | 12.2 | 13.1 | |||||||
| Other or multiple races, non-Hispanic | 89.7 | 88.8 | 13.7 | 9.8 | 10.8 | 7.4 | 2.9 | 2.5 | 25.3 | 28.8 | 20.6 | 21.5 | 4.7 | 7.3 | |||||||
| Hispanic | 85.6 | 86.9 | 17.8 | 21.3 | 14.6 | 15.7 | 3.3 | 5.6 | 26.0 | 21.2 | 18.2 | 16.3 | 7.8 | 4.8 | |||||||
| Born outside the United States | |||||||||||||||||||||
| Born in the US | 88.6 | 88.2 | 14.7 | 18.1∗ | 12.0 | 13.7 | 2.6 | 4.4∗ | 33.7 | 29.9 | 27.3 | 23.4∗ | 6.4 | 6.5 | |||||||
| Foreign born | 87.7 | 86.8 | 12.7 | 16.2 | 10.6 | 12.4 | 2.1 | 3.8 | 22.5 | 15.5∗ | 15.5 | 13.6 | 7.0 | 1.9‡ | |||||||
| Relationship Status | |||||||||||||||||||||
| Married | 91.5 | 89.8 | 13.5 | 16.3 | 12.2 | 14.7 | 1.3 | 1.7 | 18.7 | 16.0 | 15.7 | 12.9 | 3.0 | 3.1 | |||||||
| Cohabitating | 90.3 | 93.0 | 18.1 | 20.7 | 15.0 | 15.4 | 3.1 | 5.3 | 31.6 | 27.7 | 25.7 | 20.6 | 6.0 | 7.1 | |||||||
| Not married or cohabitating | 83.1 | 82.8 | 13.6 | 18.2∗ | 9.8 | 11.3 | 3.8 | 6.9 | 47.5 | 41.4∗ | 36.6 | 32.9 | 10.9 | 8.5 | |||||||
| Education | |||||||||||||||||||||
| No high school diploma | 83.7 | 87.5 | 14.6 | 19.8 | 8.8 | 7.6 | 5.8 | 12.2 | 33.7 | 29.1 | 20.3 | 20.0 | 13.4 | 9.1 | |||||||
| High school or GED | 90.3 | 86.8 | 13.0 | 16.9 | 9.7 | 12.5 | 3.3 | 4.4 | 24.6 | 22.5 | 18.3 | 16.0 | 6.4 | 6.6 | |||||||
| Some College | 88.2 | 86.6 | 17.0 | 16.1 | 14.7 | 12.0 | 2.3 | 4.1 | 33.9 | 28.9 | 27.9 | 23.0 | 5.9 | 5.8 | |||||||
| College Graduate | 89.3 | 90.4 | 12.5 | 19.2† | 11.6 | 18.1† | 0.8 | 1.1 | 34.5 | 29.6 | 30.4 | 25.7 | 4.1 | 3.9 | |||||||
| Parity | |||||||||||||||||||||
| 0 | 85.4 | 84.7 | 8.6 | 15.1† | 5.7 | 9.5∗ | 2.9 | 5.6∗ | 58.3 | 49.0† | 49.3 | 41.4∗ | 9.0 | 7.7 | |||||||
| 1-2 | 84.3 | 86.7 | 26.7 | 24.3 | 22.7 | 17.3 | 3.9 | 7.1 | 29.2 | 26.2 | 20.2 | 19.5 | 9.0 | 6.7 | |||||||
| 3 or more | 92.1 | 90.9 | 14.7 | 17.6 | 12.8 | 15.3 | 1.8 | 2.3 | 12.7 | 11.7 | 8.9 | 7.6 | 3.8 | 4.1 | |||||||
| Number of future births expected | |||||||||||||||||||||
| 0 | 90.8 | 91.3 | 14.4 | 16.1 | 12.8 | 14.6 | 1.5 | 1.5 | 17.1 | 15.5 | 12.9 | 11.4 | 4.2 | 4.1 | |||||||
| 1-2 | 85.9 | 83.8 | 16.1 | 20.4 | 11.9 | 12.6 | 4.2 | 7.8∗ | 49.2 | 42.2∗ | 39.0 | 33.3 | 10.2 | 8.9 | |||||||
| 3 or more | 83.3 | 84.7 | 6.3 | 18.3‡ | 4.0 | 10.3∗ | 2.3 | 8.0† | 57.0 | 49.9 | 50.6 | 44.6 | 6.3 | 5.3 | |||||||
| Current insurance coverage | |||||||||||||||||||||
| None | 87.8 | 81.4 | 17.3 | 18.4 | 12.7 | 9.7 | 4.6 | 8.7 | 18.2 | 15.5 | 13.4 | 13.3 | 4.8 | 2.2∗ | |||||||
| Private | 89.8 | 90.0 | 12.6 | 16.4∗ | 11.4 | 15.0∗ | 1.2 | 1.4 | 36.4 | 31.5 | 30.9 | 27.0 | 5.5 | 4.5 | |||||||
| Medicaid | 85.6 | 86.9 | 18.2 | 20.8 | 13.1 | 10.5 | 5.1 | 10.3∗ | 27.1 | 24.9 | 15.6 | 12.5 | 11.6 | 12.4 | |||||||
| Other Public | 82.2 | 84.9 | 11.7 | 22.7∗ | 7.4 | 14.8 | 4.3 | 7.8 | 36.6 | 20.0∗ | 31.2 | 12.7† | 5.5 | 7.3 | |||||||
| Source of family planning or GYN care | |||||||||||||||||||||
| No Care | 84.1 | 84.0 | 12.7 | 15.5 | 10.6 | 10.3 | 2.1 | 5.2∗ | 12.6 | 17.5 | 9.9 | 15.2∗ | 2.7 | 2.3 | |||||||
| Private | 91.0 | 90.9 | 14.3 | 17.8 | 11.9 | 15.1 | 2.4 | 2.7 | 39.0 | 33.1∗ | 31.3 | 26.9 | 7.7 | 6.2 | |||||||
| Title X | 90.2 | 89.7 | 18.3 | 23.9 | 13.0 | 13.8 | 5.3 | 10.1 | 46.4 | 27.2† | 33.1 | 14.6† | 13.3 | 12.6 | |||||||
| Other Public | 87.0 | 82.4 | 17.0 | 24.1 | 14.1 | 15.1 | 2.9 | 9.0∗ | 37.9 | 27.3∗ | 31.8 | 17.2† | 6.2 | 10.1 | |||||||
| Access to carec | |||||||||||||||||||||
| No access to care | 84.8 | 76.9 | 12.7 | 11.5 | 10.0 | 4.1 | 2.7 | 7.3 | 5.5 | 5.2 | 3.1 | 4.6 | 2.3 | 0.6 | |||||||
| Access to care | 88.5 | 88.9 | 14.2 | 17.6∗ | 11.7 | 13.7 | 2.5 | 3.9 | 34.4 | 29.1† | 27.6 | 22.9∗ | 6.8 | 6.2 | |||||||
| Any same sex sexual contact | |||||||||||||||||||||
| Never had same sex sexual contact | 88.4 | 87.9 | 13.3 | 17.6† | 11.0 | 13.6 | 2.3 | 3.9∗ | 31.9 | 27.8 | 25.8 | 21.8∗ | 6.1 | 6.0 | |||||||
| Has had same sex sexual contact | 88.7 | 88.2 | 18.8 | 19.4 | 14.9 | 13.0 | 3.8 | 6.4 | 31.2 | 29.2 | 22.7 | 23.8 | 8.5 | 5.4 | |||||||
NA, not applicable; LARC, long-acting reversible contraception; IUD, intrauterine device; SARC, short-acting reversible contraception; GYN, gynecological.
Survey years in column headings represent the midpoint of data collection years for each of the two NSFG surveys.
Data are all %.
Population includes all sexually active female respondents ages 15-44 not seeking pregnancy and those who reported current contraceptive method use, weighted to reflect the U.S. female civilian population of the United States.
An additional 668 respondents are included among 45-49 year olds in 2016, as this was the first round of the NSFG in which this age group was surveyed.
Sexually active women not seeking pregnancy includes female respondents who had had sexual intercourse in the 3 months prior to interview, who were not pregnant or trying to conceive and who were not sterile for noncontraceptive reasons.
Non-pill SARC methods include the contraceptive patch, the vaginal ring, and injectable contraception.
Represents respondents who indicated either having received and of the following services in the past 12 months: a birth control check-up, a pap test, or a pelvic exam, OR having some form of insurance coverage.
Significant difference between years at p<0.05 based on simple logistic regression analyses.
Significant difference between years at p<0.01 based on simple logistic regression analyses.
Significant difference between years at p<0.001 based on simple logistic regression analyses.
Use of LARC methods among 15- to 19-year-old contraceptive users more than doubled from 9.8% in 2014 to 22.2% in 2016 (P < .05). Increases in LARC use also occurred among college graduates (12.5%-19.2%, P < .01), nulliparous women (8.6%-15.1%, P < .01), those expecting to have three or more (additional) births (6.3%-18.3%, P < .001), and those reporting never having had same-sex sexual contact (13.3%-17.6%, P < .01). With regard to specific LARC method use, between 2014 and 2016, IUD use significantly increased among those at the highest income levels (10.4%-15.6%, P < .05) and college graduates (11.6%-18.1%, P < .01); increases in implant use were seen among those in the lowest income level (3.8%-8.3%, P < .01) and those expecting three or more (additional) births (2.3%-8%, P < .01).
The use of SARC decreased significantly among those who had never given birth (58.3%-49.0%, P < .01), those who received their family planning or gynecological care at a Title X site in the past year (46.4%-27.2%, P < .01), and those with any access to reproductive health care (34.4%-29.1%, P < .01). Within SARC method use, pill use decreased among respondents with non-Medicaid public insurance (31.2%-12.7%, P < .01) and those who had received family planning or gynecological care at a Title X clinic (33.1%-14.6%, P < .01) or another public clinic in the past year (31.8%-17.2%, P < .01). There were large decreases in nonpill SARC use among those born outside of the United States (7.0%-1.9%, P < .001).
When controlling for users’ demographic, sexual, and reproductive health characteristics, having some level of access to reproductive health care is a key factor associated with higher levels of both LARC and SARC method use, grouped and individually (Table 3). Access to reproductive health care was associated with significantly higher levels of SARC method use especially; those with access had 13.5 times higher odds of using nonpill SARC methods than those without access (P < .01). Higher levels of LARC use were also associated with having given birth (P < .05), while lower levels were associated with being in the oldest age group of 45- to 49-year-olds (P < .001) and identifying as a race other than white, black, or Hispanic (P < .01). Similar patterns of associations among age, race, and parity as independent variables and the outcome of IUD use were observed at the multivariable level; being a college graduate was also associated with increased IUD use at the multivariable level (P < .05). Higher levels of implant use were associated with expecting one or more additional births (P < .01), while lower levels of implant use were associated with being older than 25 (P < .05), having at least a high school or GED education level (P < .01), and having an income at 300% of poverty or higher (P < .01).
Table 3.
Adjusted odds ratios from multivariable logistic regression analyses assessing the associations between selected demographic, sexual, and reproductive health characteristics and U.S. women’s use of selected contraceptive methods, among users of contraception ages 15 to 49 years, 2016 (N = 3,367).
| Variable | LARC methods | IUD | Implant | SARC methods | Pill | Nonpill SARC methodsa |
|---|---|---|---|---|---|---|
| Age (y) | ||||||
| 15–24 | Ref | Ref | Ref | Ref | Ref | Ref |
| 25–34 | 0.84 (0.57, 1.23) | 1.44 (0.90, 2.31) | 0.45 (0.23, 0.90)∗ | 0.77 (0.54, 1.12) | 0.77 (0.53, 1.11) | 0.95 (0.56, 1.59) |
| 35–44 | 0.57 (0.36, 0.91)∗ | 1.08 (0.61, 1.90) | 0.18 (0.07, 0.47)‡ | 0.52 (0.32, 0.84)† | 0.48 (0.28, 0.82)† | 0.77 (0.38, 1.56) |
| 45–49 | 0.18 (0.10, 0.34)‡ | 0.37 (0.21, 0.67)† | 0.04 (0.00, 0.31)† | 0.32 (0.14, 0.70)† | 0.34 (0.14, 0.82)∗ | 0.30 (0.08, 1.11) |
| Poverty status | ||||||
| <100% federal poverty level | Ref | Ref | Ref | Ref | Ref | Ref |
| 100%–199% | 0.92 (0.58, 1.45) | 1.01 (0.61, 1.68) | 0.62 (0.29, 1.31) | 0.78 (0.56, 1.10) | 0.68 (0.44, 1.04) | 1.26 (0.79, 2.02) |
| 200%–299% | 0.96 (0.60, 1.52) | 0.87 (0.54, 1.41) | 0.83 (0.36, 1.91) | 1.13 (0.74, 1.74) | 1.08 (0.70, 1.68) | 1.33 (0.70, 2.56) |
| ≥300% or higher | 1.18 (0.77, 1.80) | 1.22 (0.73, 2.04) | 0.34 (0.19, 0.64)† | 1.12 (0.77, 1.63) | 1.27 (0.85, 1.90) | 0.86 (0.49, 1.52) |
| Race/ethnicity | ||||||
| White, non-Hispanic | Ref | Ref | Ref | Ref | Ref | Ref |
| Black, non-Hispanic | 0.89 (0.61, 1.32) | 0.99 (0.65, 1.51) | 1.06 (0.62, 1.83) | 0.99 (0.66, 1.46) | 0.54 (0.32, 0.91)∗ | 3.01 (1.79, 5.06)‡ |
| Other or multiple races, non-Hispanic | 0.44 (0.27, 0.71)† | 0.45 (0.26, 0.79)† | 0.51 (0.17, 1.49) | 0.97 (0.57, 1.65) | 0.74 (0.41, 1.34) | 1.72 (0.69, 4.25) |
| Hispanic | 1.07 (0.75, 1.53) | 1.19 (0.78, 1.80) | 0.95 (0.51, 1.78) | 0.82 (0.56, 1.19) | 0.63 (0.42, 0.95)∗ | 1.48 (0.85, 2.56) |
| Born outside the United States | ||||||
| Born in the United States | Ref | Ref | ||||
| Foreign born | 0.64 (0.38, 1.07) | 0.35 (0.17, 0.71)† | ||||
| Relationship status | ||||||
| Married | Ref | Ref | Ref | |||
| Cohabitating | 1.25 (0.78, 2.01) | 1.09 (0.72, 1.65) | 0.94 (0.57, 1.55) | |||
| Not married or cohabitating | 1.42 (0.98, 2.06) | 1.66 (1.05, 2.64)∗ | 1.62 (0.96, 2.72) | |||
| Education | ||||||
| No high school diploma | Ref | Ref | Ref | |||
| High school or GED | 1.77 (0.86, 3.64) | 0.36 (0.19, 0.69)† | 0.62 (0.33, 1.14) | |||
| Some college | 1.58 (0.81, 3.06) | 0.35 (0.17, 0.70)† | 0.47 (0.23, 1.00)∗ | |||
| College graduate | 2.39 (1.23, 4.64)∗ | 0.19 (0.07, 0.47)‡ | 0.42 (0.20, 0.90)∗ | |||
| Parity | ||||||
| 0 | Ref | Ref | Ref | Ref | Ref | |
| 1–2 | 2.45 (1.56, 3.83)‡ | 2.02 (1.22, 3.36)† | 2.35 (1.03, 5.37)∗ | 0.57 (0.40, 0.82)† | 0.56 (0.37, 0.84)† | |
| ≥3 | 1.70 (1.07, 2.69)∗ | 1.65 (1.01, 2.71)∗ | 1.35 (0.64, 2.87) | 0.33 (0.22, 0.48)‡ | 0.30 (0.19, 0.45)‡ | |
| No. of future births expected | ||||||
| 0 | Ref | Ref | Ref | Ref | ||
| 1–2 | 3.04 (1.73. 5.33)‡ | 1.77 (1.22, 2.56)† | 1.59 (0.99, 2.56) | 2.12 (1.13, 3.96)∗ | ||
| ≥3 | 3.53 (1.40, 8.92)† | 1.53 (0.93, 2.53) | 1.64 (0.96, 2.79) | 1.25 (0.49, 3.21) | ||
| Access to careb | ||||||
| No access to care | Ref | Ref | Ref | Ref | Ref | |
| Access to care | 1.82 (0.92, 3.58) | 3.21 (1.31, 7.82)∗ | 7.20 (3.03, 17.14)‡ | 5.21 (2.05, 13.28)‡ | 13.53 (2.79, 65.74)† |
Note: Data presented as adjusted odds ratio (95% confidence interval). Population includes all female respondents ages 15 to 49 who reported current contraceptive method use, weighted to reflect the U.S. female civilian population. For some methods or method groups (implant, SARC methods, and nonpill SARC methods), the total N is slightly smaller than the full population of contraceptive users due to lower response rates on some demographic or reproductive characteristics among users of those particular methods. Adjusted odds ratios reflect final multivariable models after a backward stepwise elimination process in which independent variables were removed if Wald tests yielded P > .05. All multivariable models included age, race/ethnicity, and poverty status, regardless of significance due to their theoretical relevance to the models. Age categories were consolidated for the multivariable models due to insufficiently large cell sizes. IUD = intrauterine device; LARC = long-acting reversible contraception; SARC = short-acting reversible contraception.
Nonpill SARC methods include the contraceptive patch, the vaginal ring, and injectable contraception.
Respondents who indicated either having received any of the following services in the past 12 months—a birth control checkup, a Pap test, or a pelvic exam—OR having some form of insurance coverage.
Significant difference between user characteristics at P < .05 based on multivariable logistic regression analyses.
Significant difference between user characteristics at P < .01 based on multivariable logistic regression analyses.
Significant difference between user characteristics at P < .001 based on multivariable logistic regression analyses.
Higher levels of SARC use were also observed among contraceptive users who expected one to two future births (P < .01), while lower levels were observed among those 35 years and older (P < .01) and those who had given birth (P < .01). Lower levels of pill use were also associated with older ages 35–49 (P < .05) and parity (P < .05). Higher levels of nonpill SARC method use were associated with identifying as non-Hispanic black (P < .001), and lower levels were associated with individuals identifying as foreign born (P < .01).
Discussion
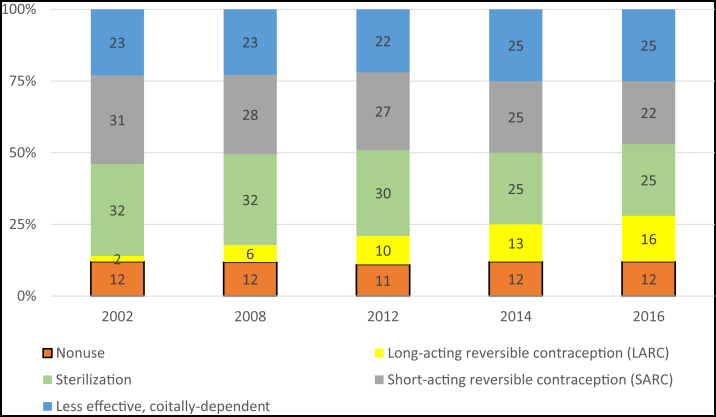
As would be expected for the short time frame examined, overall use of contraception, as well as use of contraception among sexually active women not seeking pregnancy, remained steady between 2014 and 2016. In fact, nonuse of contraception has remained steady for at least about 15 years at approximately 10% among sexually active women not seeking pregnancy, as has use of less effective, coitus-dependent methods (including the condom, withdrawal, and fertility awareness–based methods), which has remained around 20%–25% among this same population (7, 12). This reveals a notable pattern: most of the shifts observed in method use over this time period have been among the most and moderately effective method groups (permanent contraception, LARCs, and SARCs) and not from nonuse to use or from less effective, coitus-dependent method use to use of these more effective methods (Fig. 1). These shifts are occurring over the same time period that access to contraception through health insurance coverage has increased (13). Of note, these recent data indicate the start of a pattern demonstrating decreases in SARC methods paralleling LARC increases, representing some shifts toward more effective method use among these two groups.
Figure 1.
Recent contraceptive use by method groups among sexually active women ages 15 to 44 years not seeking pregnancy in the United States in 2014 and 2016, compared with shifts in contraceptive use among method groups in this population from 2002 to 2008, and 2008 to 2012 (7, 12).
Overall, however, these longer-term trends challenge a central assumption motivating some programmatic and policy initiatives aimed at reducing pregnancies among sexually active women not seeking them (14, 15, 16, 17); that is, increasing access to more effective methods of contraception will shift individuals who may have a need for contraception from nonuse to use or from less effective methods like withdrawal and condoms to some of the most effective ones like IUDs. Indeed, this exclusive focus on effectiveness prioritizes population-level reductions in pregnancies over individuals’ own preferences regarding reproduction and contraception, despite many studies having documented that individuals prioritize many factors when selecting a contraceptive method, with effectiveness representing just one of these factors (18, 19, 20, 21, 22, 23). Notably, sexually active young adults ages 20–24 not seeking pregnancy were the only age group to experience decreases in overall contraceptive use but no significant change in specific methods or method groups between 2014 and 2016, which may be related to recent shifts in their source of, and increases in use of insurance coverage for, sexual and reproductive health care (24).
The significant increases in use documented among LARC users, especially in the use of implants, is notable given both the short amount of time between the data points and that the increase continues a previously documented trend (7). Although female permanent contraception and oral contraception continue to be the two most popular contraceptive methods among users in the United States, these latest data are the first to document a significant decrease in use of shorter-acting hormonal methods, or those considered to be “moderately effective” (11), to parallel the increases in LARC use. If this pattern continues in subsequent years, most long-term increases in LARC use could be considered to be indicative of transitions in use from SARC and permanent contraception users. Use of shorter-acting methods, including the oral contraceptive pill, among women who had never given birth significantly decreased in recent years, corresponding to significant increases in the use of both LARC methods—the IUD and implant. These shifts may possibly be reflecting more widespread adoption of clinical guidance around IUDs being appropriate methods for all interested potential users, even those who have never been pregnant (25, 26). For all LARC and SARC methods except the implant, parity continues to be a predictor of use as in past years, with increasing parity associated with LARC method use and nulliparity associated with SARC method use (7).
Most LARC use continues to be IUD use; however, whereas increases in IUD use primarily drove past increases in LARC use between data years, these latest national data indicate that recent increases in LARC use can be attributed primarily to increases in the use of the implant. In addition, past increases in both IUD and implant use between 2008 and 2014 were documented across almost all reproductive-age women (7), whereas increases in both of these methods between 2014 and 2016 were concentrated among particular population groups. Use of an IUD increased between these time periods among those who fell into more advantaged categories with regards to income, education, and health insurance coverage. In contrast, implant use more than doubled among young contraceptive users ages 15 to 19 years from about 6% in 2014 to over 16% in 2016, and other characteristics associated with increases in implant use, such as having lower levels of education, falling into the lowest income category, and having Medicaid health insurance coverage, may also reflect a relationship of younger age, as well as disadvantage, to implant use. With multiple national organizations having recommended LARC methods as appropriate for adolescents starting in the early 2010s (25, 26), increased training focused on LARCs for this particular age group (27, 28), and evidence indicating that adolescents prefer implants over IUDs among LARC choices (29, 30), it may be that these latest data represent the first time point at which the impact of these many intersecting factors can be detected at the national level for the youngest age group.
Although receiving family planning care at a Title X site, a federally funded family planning program established explicitly to provide funding for contraceptive service delivery to young and low-income people, was not significantly associated with implant use in our analysis, a recent analysis of Family Planning Annual Report Data from the Office of Population Affairs (31) suggests that the Title X program may be playing a role in facilitating access to implant use among Title X patients. The significant decreases in use of SARC methods, especially the pill, among individuals obtaining care at Title X sites documented in our analysis during this period may support a story of longer-term transitions from SARC use to LARC use specifically among those getting care at Title X sites, which we may be able to document in future rounds of these data.
In 2016, access to reproductive health care, representing reduced cost burden for individuals through either health insurance coverage or having received care from a public or private provider, played a role in increased use of both LARC and SARC methods among contraceptive users, when controlling for other user characteristics. Given recent federal support for undermining both insurance protections under the federal contraceptive coverage guarantee of the ACA and the original intent behind the Title X federally funded family planning program (8, 32), monitoring the extent to which this type of access will continue to be associated with changes in these provider-controlled methods will be a critical undertaking. Reductions in access via health insurance coverage or reproductive health care could result in individuals having to change their method to a less-desired but more accessible one or to forego desired contraception all together.
Several limitations are inherent in the analysis of cross-sectional secondary data. Given the design of the NSFG, some population groups in the United States may be underrepresented or not represented at all, including those with English- and Spanish-language barriers, those who identify as transgender, and institutionalized individuals. Associations observed between respondent characteristics and contraceptive method use do not necessarily imply a causal relationship. Of note, contraceptive method use in our analysis represents the most effective method reported. As such, use of more than one method is not captured in this analysis, despite recent evidence indicating small increases in the use of multiple methods, and less effective methods that may be used in conjunction with more effective methods, such as condom and withdrawal, may be underrepresented (7). In addition, because permanent contraception is just that (permanent), findings related to use of these methods cannot be interpreted as incidence or “new” use of permanent contraception. Individuals who indicated that they had a single service health insurance coverage plan or coverage through the Indian Health Service were grouped with “no coverage” in the publicly available data, despite potentially having reproductive health care coverage through these sources.
Conclusions
Given the myriad positive outcomes for individuals’ health and socioeconomic well-being associated with using contraception, facilitating access to the full range of contraceptive methods available for people who wish to avoid pregnancy should continue to be high priority, especially in the current political climate. Perhaps even more importantly, to align with the core tenets of patient-centered care (33), people should be able to select contraceptive methods based on informed, voluntary, and full personal choice (34), not because a health care provider, public health professional, or legislator prioritizes a particular method over others (35, 36, 37). Health care providers have a key role to play in helping their patients make fully informed choices about contraceptive methods, as patients themselves indicate that they put a lot of stock in the opinions of their doctors (38). Accordingly, surveillance activities should move toward documenting both actual and preferred method use to reveal the extent to which a gap exists between these two metrics (39).
Acknowledgments
The authors thank Rachel Jones, Kathryn Kost, Adam Sonfield, and Rebecca Wind for reviewing and commenting on this manuscript.
Footnotes
M.L.K. has nothing to disclose. E.P. has nothing to disclose.
Supplementary data
References
- 1.Sonfield A., Hasstedt K., Gold R.B. Guttmacher Institute; New York: 2014. Moving forward: family planning in the era of health reform.https://www.guttmacher.org/report/moving-forward-family-planning-era-health-reform Available at: Accessed October 31, 2019. [Google Scholar]
- 2.Daniels K., Mosher W.D. Contraceptive methods women have ever used: United States, 1982–2010. Natl Health Stat Rep. 2013:1–15. [PubMed] [Google Scholar]
- 3.Kavanaugh M.L., Douglas-Hall A., Finn S.M. Health insurance coverage and contraceptive use at the state level: findings from the 2017 Behavioral Risk Factor Surveillance System. Contracept X. 2020;2 doi: 10.1016/j.conx.2019.100014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services About Title X grants. 2016. https://www.hhs.gov/opa/title-x-family-planning/about-title-x-grants/index.html Available at: Accessed October 31, 2019.
- 5.Frost JJ, Frohwirth LF, Blades N, Zolna MR, Douglas-Hall A, Bearak J. Publicly funded contraceptive services at U.S. clinics, 2015. New York: Guttmacher Institute. Available at: https://www.guttmacher.org/sites/default/files/report_pdf/publicly_funded_contraceptive_services_2015_3.pdf.
- 6.Health Resources and Service Administration Women’s preventive services guidelines. 2017. https://www.hrsa.gov/womens-guidelines-2016/index.html Available at: Accessed October 31, 2019.
- 7.Kavanaugh M.L., Jerman J. Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception. 2018;97:14–21. doi: 10.1016/j.contraception.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasstedt Kinsey. What the Trump administration’s final regulatory changes mean for Title X. Health Affairs Blog. 2017. https://www.healthaffairs.org/do/10.1377/hblog20190304.267855/full/ Available at: Accessed October 31, 2019.
- 9.Adam Sonfield. Health Affairs Blog; 2017. Despite leaving key questions unanswered, new contraceptive coverage exemptions will do clear harm.https://www.healthaffairs.org/do/10.1377/hblog20171018.607441/abs/ Available at: Accessed October 31, 2019. [Google Scholar]
- 10.Centers for Disease Control and Prevention . Homepage; 2019. National Survey of Family Growth.https://www.cdc.gov/nchs/nsfg/index.htm Available at: Accessed July 9, 2019. [Google Scholar]
- 11.Centers for Disease Control and Prevention Effectiveness of family planning methods. https://www.cdc.gov/reproductivehealth/UnintendedPregnancy/PDF/Family-Planning-Methods-2014.pdf Available at:
- 12.Mosher W.D., Martinez G.M., Chandra A., Abma J.C., Willson S.J. Use of contraception and use of family planning services in the United States: 1982–2002. Adv Data. 2004;350:1–36. [PubMed] [Google Scholar]
- 13.Sonfield A. What is at stake with the federal contraceptive coverage guarantee? Guttmacher Policy Rev. 2017;20:4. [Google Scholar]
- 14.Welti K., Manlove J. How increasing the use of effective contraception could reduce unintended pregnancy and public health care costs. Child Trends. 2017 https://www.childtrends.org/wp-content/uploads/2017/03/2017-03IncreasingEffectiveContraception.pdf Available at: [Google Scholar]
- 15.Okusanya B.O., Oduwole O., Effa E.E. Immediate postabortal insertion of intrauterine devices. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD001777.pub4. http://doi.wiley.com/10.1002/14651858.CD001777.pub4 Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Speidel J.J., Harper C.C., Shields W.C. The potential of long-acting reversible contraception to decrease unintended pregnancy. Contraception. 2008;78:197–200. doi: 10.1016/j.contraception.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Weese K. Washington Post; May 1, 2018. Almost half of pregnancies in the U.S. are unplanned. There’s a surprisingly easy way to change that.https://www.washingtonpost.com/news/posteverything/wp/2018/05/01/almost-half-of-pregnancies-in-the-u-s-are-unplanned-theres-a-surprisingly-easy-way-to-change-that/ Available at: [Google Scholar]
- 18.Samari G., Foster D.G., Ralph L.J., Rocca C.H. Pregnancy preferences and contraceptive use among US women. Contraception. 2020;101:79–85. doi: 10.1016/j.contraception.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lessard L.N., Karasek D., Ma S., Darney P., Deardorff J., Lahiff M. Contraceptive features preferred by women at high risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44:194–200. doi: 10.1363/4419412. [DOI] [PubMed] [Google Scholar]
- 20.Gomez A., Clark J. Method mismatch: discrepancies between young women’s contraceptive preferences and current method choice. Contraception. 2013;88:459–460. [Google Scholar]
- 21.Yee L., Simon M. The role of the social network in contraceptive decision-making among young, African American and Latina women. J Adolesc Health. 2010;47:374–380. doi: 10.1016/j.jadohealth.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gilliam M.L., Neustadt A., Whitaker A., Kozloski M. Familial, cultural and psychosocial influences of use of effective methods of contraception among Mexican-American adolescents and young adults. J Pediatr Adolesc Gynecol. 2011;24:79–84. doi: 10.1016/j.jpag.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kusunoki Y., Upchurch D.M. Contraceptive method choice among youth in the United States: the importance of relationship context. Demography. 2011;48:1451–1472. doi: 10.1007/s13524-011-0061-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frost J.J., Lindberg L.D. Trends in receipt of contraceptive services: young women in the U.S., 2002–2015. Am J Prev Med. 2019;56:343–351. doi: 10.1016/j.amepre.2018.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The American Collee of Obstetricians and Gynecologists Long-acting reversible contraception: implants and intrauterine devices. 2017. http://journals.lww.com/00006250-200311000-00047 Available at:
- 26.Committee on Adolescence Contraception for Adolescents. Pediatrics. 2014;134:e1244–e1256. doi: 10.1542/peds.2014-2299. [DOI] [PubMed] [Google Scholar]
- 27.Thompson K.M.J., Rocca C.H., Stern L., Morfesis J., Goodman S., Steinauer J. Training contraceptive providers to offer intrauterine devices and implants in contraceptive care: a cluster randomized trial. Am J Obstet Gynecol. 2018;218:597.e1–597.e7. doi: 10.1016/j.ajog.2018.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American College of Obstetricians and Gynecologists Adolescents and long-acting reversible contraception: implants and intrauterine devices. ACOG Comm Opin. 2018;131 https://www.acog.org/-/media/Committee-Opinions/Committee-on-Adolescent-Health-Care/co735.pdf?dmc=1&ts=20200225T1637438023 Available at: [Google Scholar]
- 29.Kavanaugh M.L., Frohwirth L., Jerman J., Popkin R., Ethier K. Long-acting reversible contraception for adolescents and young adults: patient and provider perspectives. J Pediatr Adolesc Gynecol. 2013;26:86–95. doi: 10.1016/j.jpag.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mestad R., Secura G., Allsworth J.E., Madden T., Zhao Q., Peipert J.F. Acceptance of long-acting reversible contraceptive methods by adolescent participants in the Contraceptive CHOICE Project. Contraception. 2011;84:493–498. doi: 10.1016/j.contraception.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fowler C., Gable J., Wang J., Lasater B., Wilson E. RTI International; Research Triangle Park, NC: 2019. Title X family planning annual report: 2018 national summary.https://www.hhs.gov/opa/sites/default/files/title-x-fpar-2018-national-summary.pdf Available at: [Google Scholar]
- 32.Center on Budget and Policy Priorities Sabotage watch: tracking efforts to undermine the ACA. 2017. https://www.cbpp.org/sabotage-watch-tracking-efforts-to-undermine-the-aca Available at: Accessed November 8, 2019.
- 33.Gilliam M.L. Beyond coercion: let us grapple with bias. Obstet Gynecol. 2015;126:915. doi: 10.1097/AOG.0000000000001116. [DOI] [PubMed] [Google Scholar]
- 34.Senderowicz L. “I was obligated to accept”: A qualitative exploration of contraceptive coercion. Soc Sci Med. 2019;239 doi: 10.1016/j.socscimed.2019.112531. [DOI] [PubMed] [Google Scholar]
- 35.Gomez A.M., Fuentes L., Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health. 2014;46:171–175. doi: 10.1363/46e1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins J.A., Kramer R.D., Ryder K.M. Provider bias in long-acting reversible contraception (LARC) promotion and removal: perceptions of young adult women. Am J Public Health. 2016;106:1932–1937. doi: 10.2105/AJPH.2016.303393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gomez A.M., Wapman M. Under (implicit) pressure: young black and Latina women’s perceptions of contraceptive care. Contraception. 2017;96:221–226. doi: 10.1016/j.contraception.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 38.Harper C.C., Brown B.A., Foster-Rosales A., Raine T.R. Hormonal contraceptive method choice among young, low-income women: How important is the provider? Patient Educ Couns. 2010;81:349–354. doi: 10.1016/j.pec.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marshall C., Guendelman S., Mauldon J., Nuru-Jeter A. Young women’s contraceptive decision making: do preferences for contraceptive attributes align with method choice? Perspect Sex Reprod Health. 2016;48:119–127. doi: 10.1363/48e10116. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.