Abstract
Objective
To study the racial and socioeconomic characteristics of women seeking fertility care in a state with mandated insurance coverage for fertility testing and treatment.
Design
Cross-sectional, self-administered survey.
Setting
Academic fertility center in Illinois.
Patient(s)
Of 5,000 consecutive fertility care patients, 1,460 completed the survey and were included in the study sample.
Intervention(s)
None.
Main Outcome Measure(s)
Details about demographic characteristics and health care access on the basis of patient race/ethnicity and socioeconomic status.
Result(s)
The mean age of participants was 36.1 years; 75.5% were White, 10.2% Asian, 7.3% Black, 5.7% Latinx, and 1.3% Other. Most women had a bachelor’s (35.5%) or master’s degree (40.5%) and an annual household income of >$100,000 (81.5%). Black and Hispanic women traveled twice as far (median 10 miles) as White and Asian women (median 5 miles for both) for treatment. Black women (14.7%) were more likely to report that their race was a barrier to getting fertility treatment compared with White (0.0%), Hispanic (5.1%), and Asian (5.4%) women. Black and Hispanic women were approximately twice as likely to report income level (26.5% and 20.3%, respectively) and weight (7.8% and 8.9%, respectively) as barriers compared with White and Asian respondents.
Conclusion(s)
Significant racial and socioeconomic disparities exist among fertility patients accessing care. Beyond providing all Americans with health insurance that covers fertility treatment, further research in the general population is needed to understand the complex social, cultural, racial, and economic factors that prohibit many individuals from accessing needed fertility care.
Key Words: Racial disparities, access to care, infertility, IVF, insurance coverage
Discuss: You can discuss this article with its authors and other readers at https://www.fertstertdialog.com/posts/xfre-d-20-00148
Infertility affects an estimated 6.7 million women in the United States (1). In the last two decades, increasing maternal age and expanded insurance coverage for fertility treatment have contributed to a rise in assisted reproductive technology use (1, 2, 3). However, comparative policy and economic analyses estimate that only 24% of assisted reproductive technology demand in the US is met (4). Previous data suggest that socioeconomic status is a key driver of patients’ decisions to pursue fertility treatment (5, 6). A 2015 US report estimated that the median cost of an in vitro fertilization (IVF) cycle, including medications, is $19,200 (7). With the median household income in the United States being $70,760 in 2018 (8), such fertility treatments can be financially inaccessible to many individuals in need.
Economics alone, however, does not seem to impact access to fertility care. A 2003 survey conducted of women presenting to a Massachusetts fertility center demonstrated that, even in a state with mandated insurance coverage for fertility treatment, disparities in access to infertility services persist (9). The majority of individuals accessing services were White, highly educated, and had income levels >$100,000. According to a 2004–2005 survey of fertility patients in Illinois, a state with a mandate to cover fertility treatment, racial and socioeconomic barriers hindered access to fertility treatments (5). For example, relative to their White peers, Black and Hispanic women attempted to conceive longer before seeking treatment and reported more difficulty getting appointments, taking time off work, and affording fertility treatment (5). Prior studies demonstrated that state-mandated insurance coverage for fertility treatment positively impacted access to fertility care (10, 11, 12). Otherwise, access to needed fertility treatment may be limited to more affluent patients.
A recent analysis of the National Health and Nutrition Examination Survey data from 2013–2016 of a nationally representative sample of women between 20 and 44 years old found no differences in infertility rates by race/ethnicity, education, income, US citizenship, insurance, or location of health care (10). However, despite equivalent infertility rates, the national analysis did not show equivalent access to fertility care. Women with college degrees and incomes >$100,000 accessed fertility care more than women without high school diplomas and women with incomes <$25,000. In addition, White women were approximately twice as likely to seek medical help to become pregnant relative to their Hispanic and Black peers (10).
Because of the existence of widely acknowledged racial and socioeconomic disparities, the American Society for Reproductive Medicine (ASRM) added “access to care” as a major focus of its 2014–2019 strategic plan. This included a greater focus on research and advocacy to identify and ameliorate such disparities (13). ASRM also held a 2-day national summit in September 2015 with over 75 experts and developed 25 action items to improve access to care (14).
To understand more clearly the current patterns of fertility care use and the racial, socioeconomic, and clinical factors that may influence patient access to fertility treatment, we systematically surveyed women presenting for fertility care at a major Midwestern fertility center in a state with mandated insurance coverage for fertility treatment. Despite the call to action by ASRM and others to improve access to care by rectifying disparities (13, 15, 16), we hypothesized that, because of persistent systemic inequities, we would observe significant racial and socioeconomic disparities.
Materials and methods
Data Collection
Institutional Review Board approval was obtained from Northwestern University Feinberg School of Medicine. A 32-question survey (Supplemental Fig. 2, available online) was adapted from previous work (5) and programmed into REDCap, a secure, Health Insurance Portability and Accountability Act-compliant, data collection platform. Modifications to the previous 24-question instrument were made to improve understanding of patient experiences with infertility and to account for recent technological advancements in fertility care. The questionnaire was piloted and reviewed by an infertility physician, a non-infertility physician, a licensed clinical psychologist specializing in women’s reproductive health, and five research study staff, including a survey methodologist and biostatistician. The survey instrument collected information regarding patient demographics, infertility history, treatments, and reported barriers in accessing care. Additionally, the survey examined cultural, racial, and economic factors that might contribute to disparities in the infertile population in the Midwestern United States.
The survey was offered electronically to 5,000 unique participants who presented to the Northwestern Center for Fertility and Reproductive Medicine for at least one visit between June 2018 and September 2019. Their e-mail addresses were obtained by the Northwestern Enterprise Data Warehouse. In September 2019, the electronic consent form and survey were e-mailed using REDCap, and responses were obtained for the next month. To encourage survey completion, up to two follow-up e-mails were sent to nonrespondents.
Northwestern Center for Fertility and Reproductive Medicine has three clinical sites throughout the greater Chicago area (downtown, northern suburb, and western suburb), which allows for potential patients with infertility better access to care (Supplemental Fig. 1, available online). Of the 5,000 e-mailed questionnaires, 377 were undeliverable because of incorrect e-mail addresses. From the remaining 4,623 questionnaires, 1,460 survey responses were obtained from participants containing their age, sex, and race/ethnicity (32% response rate). These baseline demographic data were also obtained from the 4,623 invited individuals via the Northwestern Enterprise Data Warehouse to compare the demographics between survey responders and nonresponders to evaluate potential nonresponse bias.
Statistical Analysis
Descriptive univariate means, 95% confidence intervals, frequencies, and percentages were calculated for all available continuous and categorical data to summarize participant demographics and other clinical characteristics, including infertility cause, treatment and referral type, barriers to access, and perceived hardships encountered while seeking infertility treatment. Some continuous variables were not normally distributed; median values and interquartile ranges were used in such cases to summarize their central tendency and dispersion. A choropleth map was created in R using the zip_choropleth function to visualize counts of survey respondents aggregated by Chicago area zip code.
Continuous patient characteristics were systematically compared across racial/ethnic, insurance coverage, and household income strata using one-way ANOVA or Kruskal-Wallis tests for comparison of raw values and by multiple linear and robust regression for comparison of covariate-adjusted values. For categorical outcomes, Pearson’s chi-squared tests were calculated to compare unadjusted quantities, while a series of multiple logistic regression models were fit to examine factors associated with each categorical patient-reported outcome. Adjusted models were used for the following: age (<35, 35–37, 38–40, 41–42, >42); parity (parous vs. nulliparous); race/ethnicity (White, Black, Latinx, Asian, multiple/other); income (<$100K, $100–200K, $200–400K, >$400K); religion (Catholic, Protestant, Jewish, nonreligious or spiritual, other Christian, Hindu, other); education (less than a bachelor’s, bachelor’s, master’s, or terminal professional degrees); insurance coverage for fertility treatment (none, <50%, 50%–75%, or >75% coverage); and an indicator of whether the respondent is currently seeking or undergoing fertility treatment or if they have completed fertility treatment in the past. Adjusted predicted probabilities and omnibus equivalence tests across all strata were calculated via the margins commands in Stata 15 (StataCorp LLC, College Station, TX). All reported P values are 2-sided omnibus tests.
Results
Demographics
As shown in Table 1, members of our analytic sample (N = 1,460) were between 18 and 58 years (mean, 36.2 years). This age distribution is comparable to that of the entire invited sample for whom age information was available (mean, 36.7 years). Most respondents were non-Hispanic White (72.2%), while 7.0% identified as non-Hispanic Black, 5.4% Hispanic/Latinx, 10.0% non-Hispanic Asian, and 5.4% multiple/other race/ethnicity. The racial/ethnic composition of our analytic sample also was comparable to that of the entire invited sample, which also was mostly White (71.9%), with 9.3% identified as Black, 8.0% Hispanic, and 11.4% Asian. Most respondents reported a bachelor’s (35.1%) or master’s degree (40.5%) and an annual household income >$100,000 (81.1%). The most prevalent religions were Catholicism (37.5%) followed by secular/agnostic/nonreligious (25.4%) and Protestant (15.0%).
Table 1.
Demographics of participants presenting at Northwestern fertility clinics.
| Demographic | No. (%) |
|---|---|
| Race or ethnicity (N = 1,460) | |
| Non-Hispanic White | 1,054 (72.2%) |
| Non-Hispanic Black or AA | 102 (7.0%) |
| Hispanic/Latinx | 79 (5.4%) |
| Non-Hispanic Asian | 146 (10.0%) |
| Other | 79 (5.4%) |
| Relationship status (N = 1,457) | |
| Single | 99 (6.8%) |
| Heterosexual relationship | 1,264 (86.8%) |
| Divorced or separated | 16 (1.1%) |
| Same-sex relationship | 74 (5.1%) |
| Other | 4 (0.3%) |
| Religion (N = 1,418) | |
| Catholic | 531 (38.3%) |
| Protestant | 212 (15.0%) |
| Other Christian | 102 (7.2%) |
| Judaism | 122 (8.6%) |
| Hinduism | 48 (3.4%) |
| Secular/agnostic/nonreligious | 360 (25.4%) |
| Other | 43 (3.0%) |
| Education (N = 1,458) | |
| Less than a bachelor’s degree | 76 (5.2%) |
| 4-year college (bachelor’s degree) | 512 (35.2%) |
| Master’s degree | 591 (40.5%) |
| Professional degree | 279 (19.1%) |
| Annual household income (N=1,440) | |
| <$50,000 | 41 (2.9%) |
| $50,001–$100,000 | 230 (16.0%) |
| $100,001–$200,000 | 589 (40.9%) |
| $200,001–$400,000 | 425 (29.5%) |
| >$400,000 | 155 (10.8%) |
| Insurance coverage for fertility treatment (N = 1,436) | |
| No coverage | 264 (18.4%) |
| <50% coverage | 83 (5.8%) |
| 50%–74% coverage | 300 (20.9%) |
| 75%–100% coverage | 789 (54.9%) |
Characteristics of Respondents Seen with Infertility
As shown in Table 2, Black respondents were older than the overall sample, with a mean age of 38.0 years (Padjusted <.001). Approximately half of the White respondents (52.6%) reported being nulliparous, which is significantly fewer than the Black respondents (74.0%), Hispanic respondents (58.1%), and Asian respondents (59.1%) (Padjusted < .01). Significant differences in nulliparity were also observed in insurance coverage (Padjusted <.001) and household income (Padjusted <.001), with respondents reporting no insurance coverage and those with an income of <$100,000 reporting the highest rates of nulliparity.
Table 2.
Characteristics of respondents presenting at Northwestern fertility clinics.
| Characteristic | Overall | No. of complete cases | White | Black | Hispanic | Asian | Multiple/other | Test statistic/unadjusted P value for omnibus test/ adjusted P value | No coverage | <50% coverage | 50%–74% coverage | 75%–100% coverage | Test statistic/unadjusted P value for omnibus test/adjusted P value | <$100,000 | $100,001– $200,000 | $200,001– $400,000 | >$400,000 | Test statistic/unadjusted P value for omnibus test/adjusted P value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age [mean (95% CI)] | 36.2 (35.9–36.4) | 1442 | 35.9 (35.7–36.2) | 38.0 (37.0–39.0) | 35.7 (34.6–36.8) | 36.4 (35.7–37.1) | 36.8 (35.8–37.8) | ANOVA F = 5.7; P<.001; P<.001 | 36.5 (36.0–37.0) | 36.6 (35.7–37.6) | 35.8 (35.3–36.3) | 36.2 (35.9–36.5) | ANOVA F = 1.4; P=.25P=.03 | 35.4 (34.8-35.9) | 36.2 (35.9-36.6) | 36.2 (35.8-36.6) | 37.1 (36.4-37.8) | ANOVA F Test=12.3; =0.001 P=.0008 |
| Duration attempting to conceive before seeking treatment, months [(median (IQR)] | 23.0 (47) | 1459 | 23 (40) | 28 (49) | 38 (45) | 28 (45) | 25 (37) | Kruskal-Wallis X2 = .38; df(4); P=.83P=.71 | 13 (47) | 23 (51) | 23 (40) | 28 (40) | Kruskal-Wallis X2 = 12.0;df(3); P=.007P=.11 | 23 (47) | 25 (40) | 28 (40) | 23 (40) | Kruskal-Wallis X2 = 9.8; df(3); P=.02P=.03 |
| Distance traveled to clinic, miles [(median (IQR)] | 5.8 (12) | 1450 | 5 (12) | 10 (15) | 10 (10) | 5 (13) | 6 (6) | Kruskal-Wallis X2 = 12.7; (df)4; P=.010 P=.23 | 8.8 (12) | 6.5 (13) | 5.3 (12) | 5 (9) | Kruskal-Wallis X2=11.2; df(3); P=.01P=.06 | 10 (15) | 7.3 (11) | 5 (7.5) | 4 (5) | Kruskal-Wallis X2 = 96.2; (df(3); <0.001 P<.001 |
| Nulliparous [N(%)] | 782 (55.7%) | 1405 | 531 (52.5%) | 74 (74.0%) | 43 (58.1%) | 84 (59.2%) | 50 (64.1%) | X2 = 20.8; (df)4; P<.001; P=.01 | 165 (64.7%) | 50 (64.1%) | 155 (54.8%) | 397 (51.8%) | X2=15.5; df(3); P=.001P<.001 | 171 (66.3%) | 341 (60.7%) | 201 (48.2%) | 58 (38.9%) | X2 = 43.8; df(3); P<.001P<.001 |
| History of miscarriage [N(%)] | 590 (40.9%) | 1442 | 439 (42.2%) | 30 (30.0%) | 32 (41.6%) | 58 (39.7%) | 31 (39.7%) | X2 = 5.8; (df)4; P=.22 P=.14 | 96 (36.5%) | 33 (40.7%) | 131 (44.7%) | 322 (41.2%) | X2=3.9; df(3); P=.28 P=.12 | 96 (36.0%) | 229 (39.5%) | 176 (41.8%) | 80 (52.0%) | X2= 11.1; df(3); P=.01 P=.48 |
| Completed fertility treatment (vs. currently seeking/undergoing Tx)[N(%)] | 866 (59.3%) | 1460 | 646 (61.3%) | 54 (52.9%) | 41 (51.9%) | 80 (54.8%) | 45 (57.0%) | X2 = 6.6; (df)4; P=.16P=.84 | 155 (58.7%) | 45 (54.2%) | 184 (61.3%) | 474 (60.1%) | X2=1.5; df(3); P=.68P=.57 | 147 (54.2%) | 344 (58.4%) | 264 (62.1%) | 101 (65.2%) | X2 = 6.7; df(3); P=.08P=.95 |
| Referral type | N(%) | |||||||||||||||||
| Friend/relative/coworker N(%) | 301 (20.7%) | 1455 | 224 (21.3%) | 18 (17.8%) | 17 (21.8%) | 32 (22.1%) | 10 (12.7%) | X2 = 4.1; df(4); P=.40 P=.21 | 62 (23.5%) | 14 (16.9%) | 65 (21.8%) | 154 (19.6%) | X2=2.8; df(3); P=.42 P=.41 | 40 (14.8%) | 123 (20.9%) | 98 (23.2%) | 36 (23.4%) | X2 = 8.2; df(3); P=.04 P=.07 |
| Obstetrician/gynecologist Physician N(%) | 707 (48.6%) | 1455 | 533 (50.7%) | 46 (45.5%) | 29 (37.2%) | 61 (42.1%) | 38 (48.1%) | X2 = 8.7; df(4); P=.07 P=.18 | 109 (41.3%) | 42 (50.6%) | 144 (48.3%) | 402 (51.2%) | X2=7.8; df(3); P=.05 P=.08 | 123 (45.4%) | 284 (48.3%) | 225 (53.3%) | 69 (44.8%) | X2 = 5.8; df(3); P=.12 P=.34 |
| Primary care physician N(%) | 72 (5.0%) | 1455 | 53 (5.0%) | 7 (6.9%) | 3 (3.9%) | 3 (2.1%) | 6 (7.6%) | X2 = 4.8; df(4); P=.31 P=.66 | 17 (6.4%) | 6 (7.2%) | 16 (5.4%) | 33 (4.2%) | X2=3.1; df(3); P=.37 P=.45 | 21 (7.8%) | 25 (4.3%) | 17 (4.0%) | 8 (5.2%) | X2 = 5.9; df(3); P=.12 P=.77 |
| Insurance company N(%) | 53 (3.6%) | 1455 | 37 (3.5%) | 3 (3.0%) | 2 (2.6%) | 9 (6.2%) | 2 (2.5%) | X2 = 3.4; df(4); P=.49 P=.14 | 10 (3.8%) | 3(3.6%) | 8 (2.7%) | 32 (4.1%) | X2 =1.2; df(3); P=.76 P=.36 | 15 (5.5%) | 25 (4.3%) | 9 (2.1%) | 4 (2.6%) | X2 = 6.5; df(3); P=.09 P=.08 |
| Internet N(%) | 168 (11.6%) | 1455 | 100 (9.5%) | 12 (11.9%) | 14 (18.0%) | 30 (20.7%) | 12 (15.2%) | X2 = 20.3; df(4); P<.001 P=.16 | 35 (13.3%) | 9 (10.8%) | 29 (9.7%) | 91 (11.6%) | X2 = 1.8; df(3); P=.62 P=.42 | 36 (13.3%) | 64 (10.9%) | 49 (11.6%) | 17 (11.0%) | X2 = 1.1; df(3); P=.78 P=.95 |
| Physician diagnosed cause of infertility | N(%) | |||||||||||||||||
| Ovulation problem N(%) | 307 (21.0%) | 1460 | 225 (21.4%) | 16 (15.7%) | 18 (22.8%) | 30 (20.6%) | 18 (22.8%) | X2 = 2.1; df(4); P=.71 P=.95 | 45 (17.1%) | 16 (19.3%) | 68 (22.7%) | 168 (21.3%) | X2 = 3.1; df(3); P=.37 P=.36 | 61 (22.5%) | 120 (20.4%) | 90 (21.2%) | 33 (21.3%) | X2 = .51; df(3); P=.92P=.85 |
| Male factor N(%) | 233 (16.0%) | 1460 | 174 (16.5%) | 13 (12.8%) | 13 (16.5%) | 18 (12.3%) | 15 (19.0%) | X2 = 3.0; df(4); P=.56 P=.54 | 49 (18.6%) | 13 (15.7%) | 43 (14.3%) | 126 (16.0%) | X2 = 1.9; df(3); P=.59 P=.36 | 40 (14.8%) | 87 (14.8%) | 79 (18.6%) | 23 (14.8%) | X2 = 3.3; df(3); P=.35 P=.78 |
| Advanced age/decreased ovarian reserve N(%) | 382 (26.2%) | 1460 | 265 (25.1%) | 28 (27.5%) | 17 (21.5%) | 44 (30.1%) | 28 (35.4%) | X2 = 6.3; df(4); P=.18 P=.008 | 61 (23.1%) | 31 (37.4%) | 81 (27.0%) | 206 (26.1%) | X2 = 6.7; df(3); P=.08 P=.11 | 64 (23.6%) | 156 (26.5%) | 108 (25.4%) | 48 (31.0%) | X2 = 2.9; df(3); P=.40 P=.99 |
| Uterine Factor N(%) | 100 (6.9%) | 1460 | 70 (6.6%) | 15 (14.7%) | 1 (1.3%) | 12 (8.2%) | 2 (2.5%) | X2 = 16.5; df(4); P=.002; P<.001 | 15 (5.7%) | 8 (9.6%) | 20 (6.7%) | 56 (7.1%) | X2 = 1.7; df(3); P=.65 P=.35 | 22 (8.1%) | 34 (5.8%) | 33 (7.8%) | 7 (4.5%) | X2 = 3.7; df(3); P=.30 P=.57 |
| Blocked fallopian tubes N(%) | 90 (6.2%) | 1460 | 55 (5.2%) | 20 (19.6%) | 7 (8.9%) | 5 (3.4%) | 3 (3.8%) | X2 = 37.2; df(4); P<.001 P=.046 | 18 (6.8%) | 4 (4.8%) | 19 (6.3%) | 48 (6.1%) | X2 = 0.47; df(3); P=.93 P=.80 | 27 (10.0%) | 34 (5.8%) | 20 (4.7%) | 6 (3.9%) | X2 = 10.0; df(3); P=.02 P=.70 |
| Endometriosis N(%) | 89 (6.1%) | 1460 | 61 (5.8%) | 7 (6.9%) | 6 (7.6%) | 11 (7.5%) | 4 (5.1%) | X2=1.3; df(4); P=.87 P=.70 | 15 (5.7%) | 4 (4.8%) | 24 (8.0%) | 44 (5.6%) | X2 = 2.6; df(3); P=.46 P=.43 | 20 (7.4%) | 41 (7.0%) | 23 (5.4%) | 4 (2.6%) | X2 = 5.2; df(3); P=.16 P=.26 |
| Fertility preservation (cancer) N(%) | 34 2.3%) | 1460 | 25 (2.4%) | 4 (3.9%) | 4 (5.1%) | 1 (.7%) | 0 (0%) | X2 = 7.4; df(4); P=.12 P= .40 | 13 (4.9%) | 2 (2.4%) | 9 (.3.0%) | 10 (1.3%) | X2 = 12.1; df(3); P=.007 P=.04 | 11 (4.1%) | 15 (2.6%) | 4 (.9%) | 3 (1.9%) | X2 = 7.5; df(3); P=.06 P=.07 |
| Fertility preservation (elective) N(%) | 18 (1.2%) | 1460 | 17 (1.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.3%) | X2 = 5.3; df(4); P=.26 P=.85 | 8 (3.0%) | 1 (1.2%) | 6 (2.0%) | 3 (.4%) | X2 = 12.0; df(3); P=.005 P=.01 | 7 (2.6%) | 9 (1.5%) | 2 (0.5%) | 0 (0%) | X2 = 8.3; df(3); P=.04 P=.05 |
| Genetic factor N(%) | 36 (2.5%) | 1460 | 31 (2.9%) | 1 (1.0%) | 1 (1.3%) | 2 (1.4%) | 1 (1.3%) | X2 = 3.6; df(4); P=.46 P= .92 | 6 (2.3%) | 3 (3.6%) | 11 (3.7%) | 15 (1.9%) | X2 = 3.4; df(3); P=.34 P=.56 | 8 (3.0%) | 14 (2.4%) | 11 (2.6%) | 3 (1.9%) | X2 = 0.48; df(3); P=.92 P=.51 |
| Same-sex couple N(%) | 32 (2.2%) | 1460 | 29 (2.8%) | 0 (0%) | 2 (2.5%) | 0 (0%) | 1 (1.3%) | X2 = 7.5; df(4); P= .11 P=.28 | 5 (1.9%) | 2 (2.4%) | 3 (1.0%) | 22 (2.8%) | X2 = 3.4; df(3); P=.34 P=.11 | 4 (1.5%) | 20 (3.4%) | 5 (1.2%) | 3 (1.9%) | X2 = 6.6; df(3); P=.09 P=.09 |
| Unexplained N(%) | 550 (37.7%) | 1460 | 395 (37.5%) | 29 (28.4%) | 30 (38.0%) | 63 (43.2%) | 33 (42.8%) | X2 = 6.2; df(4); P=.19 P=.38 | 91 (34.5%) | 24 (28.9%) | 99 (33.0%) | 327 (41.4%) | X2 = 11.4; df(3); P=.01 P=.12 | 71 (26.2%) | 224 (38.0%) | 182 (42.8%) | 66 (42.6%) | X2 = 21.6; df(3); P<.001 P=.002 |
Approximately half of the respondents reported 1 (30.7%) or 2 (19.4%) previous pregnancies, while 27.4% reported no previous pregnancies. A history of miscarriage was reported by 40.8% of respondents, with no statistically significant racial or economic differences. The median duration of attempting to conceive was 23 months, and the median distance traveled to a clinic was 5.8 miles. Black and Hispanic respondents traveled twice as far (median 10 miles for both) compared with White and Asian respondents (median 5 miles for both) (Padjusted =.01). Respondents with an income <$100,000 also traveled significantly farther (median 10 miles) than those with income levels >$100,000.
Most respondents had an obstetrician/gynecologist (91.7%) and some insurance coverage for fertility treatment (81.8%). Among respondents with fertility treatment coverage, 67.2% reported that ≥75% of fertility treatment cost was covered by their plan. The most common referral type was through an obstetrician/gynecologist (48.6%), followed by a friend/relative/coworker (21.1%). Hispanic and Asian respondents were somewhat less likely to be referred by an obstetrician/gynecologist (37.2% and 41.8%, respectively) compared with White and Black respondents (50.7% and 45.5%, respectively; Padjusted =.18).
The most prevalent diagnosed causes of infertility were unexplained (37.2%), advanced age/decreased ovarian reserve (26.6%), and ovulatory dysfunction (21.0%). Black respondents were significantly more likely to have a uterine factor (14.7%) compared with White, Hispanic, and Asian respondents (6.6%, 1.3%, and 8.2% respectively; Padjusted <.001). Black and Hispanic respondents were significantly more likely to have blocked fallopian tubes (19.6% and 8.9%, respectively) compared with White and Asian respondents (5.2% and 3.4%, respectively; P<.001). A tubal factor was also a significantly more commonly reported cause of infertility among respondents with an income of <$100,000 in unadjusted models (P =.02), but this association was attenuated after adjustment for race and other covariates (Padjusted =.78).
Barriers to Accessing Fertility Care
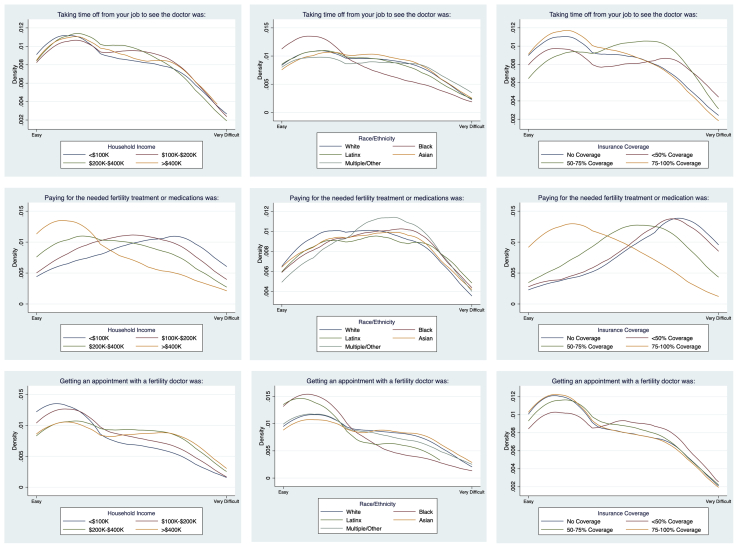
Participants were asked to mark on a scale from “easy” to “very difficult” the level of difficulty caused by “getting an appointment with a fertility doctor,” “taking time off from your job to see the doctor,” and “paying for the needed fertility treatment or medication.” As shown in Figure 1, there was no significant difference among racial groups reporting difficulty in paying for needed treatment and/or medications. However, as shown in Table 3, Black and Hispanic respondents were twice as likely to report income level (26.5% and 20.3%, respectively) as a barrier compared with White and Asian respondents. As shown in Figure 1, there were no significant racial differences in the degree of difficulty reported in taking time off work, paying for treatment, or getting an appointment with a fertility doctor. The proportion of patients identifying cost as a barrier to fertility care was inversely related to income level and the reported percentage of insurance coverage for treatment. Thus, as the degree of insurance coverage increased, the perceived cost burden of treatment lessened.
Figure 1.
Kernel density plots displaying respondents reported difficulty with taking time off work to see a doctor, paying for needed treatment or medication, or getting an appointment with a physician by income, race, and insurance coverage.
Table 3.
Self-reported barriers to access fertility care among 1,460 respondents presenting at Northwestern fertility clinics.
| Barrier | Overall |
White |
Black |
Hispanic |
Asian |
Multiple/Other |
Unadjusted χ2P Value Adjusted P value∗ |
No coverage |
<50% coverage |
50%–74% coverage |
75%–100% coverage |
Unadjusted X2P Value Adjusted P value∗ |
<$100,000 |
$100,001–$200,000 |
$200,001–$400,000 |
>$400,000 |
Unadjusted X2P value Adjusted P value∗ |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | No. (%) | ||||||||||||||
| Race/ ethnicity | 30 (2.1) | 0 (0) | 15 (14.7) | 4 (5.1) | 7 (4.8) | 4 (5.1) | X2 = 115.8; P<.001 P=.01 |
4 (1.5) | 6 (7.2) | 12 (4.0) | 8 (1.0) | X2 = 21.0; P<.001 P=.007 |
4 (1.5) | 6 (7.2) | 12 (4.0) | 8 (1.0) |
P<.001 P=.39 |
| Religion | 36 (2.5) | 27 (2.6) | 1 (1.0) | 1 (1.3) | 6 (4.1) | 1 (1.3) | X2 = 3.6; P=.47 P=.66 |
5 (1.9) | 4 (4.8) | 8 (2.7) | 19 (2.4) | X2 = 2.3; P=.52 P=.84 |
5 (1.9) | 4 (4.8) | 8 (2.7) | 19 (2.4) |
P=.52 P=.02 |
| Age | 153 (10.5) | 79 (7.5) | 26 (25.5) | 13 (16.5) | 24 (16.4) | 11 (13.9) | X2 = 44.0; P<.001 P=.02 |
36 (13.6) | 10 (12.1) | 34 (11.3) | 73 (9.3) | X2 = 4.4; P=.22 P=.44 |
36 (13.6) | 10 (12.1) | 34 (11.3) | 73 (9.3) |
P=.22 P=.44 |
| Profession | 139 (9.5) | 93 (8.8) | 5 (4.9) | 7 (8.9) | 22 (15.1) | 12 (15.2) | X2 = 11.3;P=.02 P=.16 |
21 (8.0) | 12 (14.5) | 30 (10.0) | 74 (9.4) | X2 = 3.2; P=.36 P=.40 |
21 (8.0) | 12 (14.5) | 30 (10.0) | 74 (9.4) |
P=.36 P=.30 |
| Income level | 184 (12.6) | 115 (10.9) | 27 (26.5) | 16 (20.3) | 15 (10.3) | 11 (13.9) | X2 = 25.6; P<.001 P=.54 |
64 (24.2) | 20 (24.1) | 41 (13.7) | 58 (7.4) | X2 = 61.9; P<.001 P<.001 |
64 (24.2) | 20 (24.1) | 41 (13.7) | 58 (7.4) |
P<.001 P<.001 |
| Insurance status | 243 (16.6) | 161 (15.3) | 19 (18.6) | 17 (21.5) | 33 (22.6) | 13 (16.5) | X2 = 6.8; P=.15 P=.12 |
115 (43.6) | 24 (28.9) | 46 (15.3) | 56 (7.1) | X2 = 197.7; P<.001 P<.001 |
115 (43.6) | 24 (28.9) | 46 (15.3) | 56 (7.1) |
P<.001 P<.001 |
| Sexuality | 27 (1.9) | 21 (2.0) | 2 (2.0) | 1 (1.3) | 1 (.7) | 2 (2.5) | X2 = 1.6; P=.82 P=.54 |
6 (2.3) | 0 (0) | 4 (1.3) | 16 (2.0) | X2 = 2.4; P=.49 P=.91 |
6 (2.3) | 0 (0) | 4 (1.3) | 16 (2.0) |
P=.49 P=.18 |
| Citizen status | 5 (0.3) | 2 (0.2) | 0 (0) | 0 (0) | 3 (2.1) | 0 (0 ) | X 2 = 14.2; P=.007 P= N.E. |
1 (0.4) | 1 (1.2) | 0 (0) | 3 (0.4) | X2 =2.8; P=.42 P= N.E. |
1 (0.4) | 1 (1.2) | 0 (0) | 3 (0.4) |
P=.42 P= N.E. |
| Gender identity | 5 (0.3) | 4 (0.4) | 1 (1.0) | 0 (0) | 0 (0) | 0 (0 ) | X2 = 2.3; P=N.E. |
2 (0.8) | 0 (0) | 2 (0.7) | 1 (0.1) | X2 = 3.6; P=.31 P= N.E. |
2 (0.8) | 0 (0) | 2 (0.7) | 1 (0.1) |
P=.31 P= N.E. |
| Weight | 61 (4.2) | 37 (3.5) | 8 (7.8) | 7 (8.9) | 5 (3.4) | 4 (5.1) | X2 = 9.3; P=.05 P=.69 |
12 (4.6) | 4 (4.8) | 16 (5.3) | 27 (3.4) | X2 = 2.3; P=.51 P=.62 |
12 (4.6) | 4 (4.8) | 16 (5.3) | 27 (3.4) |
P=.51 P=.90 |
| Relationship status | 58 (4.0) | 30 (2.9) | 14 (13.7) | 3 (3.8) | 5 (3.4) | 6 (7.6) | X2 = 31.8; P<.001 P=.79 |
19 (7.2) | 6 (7.2) | 13 (4.3) | 18 (2.3) | X2 = 15.8; P=.001 P=.04 |
19 (7.2) | 6 (7.2) | 13 (4.3) | 18 (2.3) |
P=.001 P<.001 |
| None | 774 (53.0) | 594 (56.4) | 42 (41.2) | 40 (50.6) | 57 (39.0) | 41 (51.9) | X2 = 22.1; P<.001 P=.08 |
93 (35.2) | 37 (44.6) | 155 (51.7) | 476 (60.3) | X2 = 53.1; P<.001 P<.001 |
93 (35.2) | 37 (44.6) | 155 (51.7) | 476 (60.3) |
P<.001 P<.001 |
| Other | 31 (2.1) | 23 (2.2) | 1 (1.0) | 1 (1.3) | 3 (2.1) | 3 (3.8) | X2 = 2.0; P=.73 P=.57 |
6 (2.3) | 4 (4.8) | 3 (1.0) | 17 (2.2) | X2 = 4.8; P=.19 P=.19 |
6 (2.3) | 4 (4.8) | 3 (1.0) | 17 (2.2) |
P=.19 P=.84 |
Note: N.E.= parameters not estimable due to sparse data.
Adjusted models include the following covariate set: age (<35, 35–37, 38–40, 41–42, >42); parity (parous vs. nulliparous); race/ethnicity (White, Black, Latinx, Asian, multiple/other); household income (<$100 $100–200K, $200–400K, >$400K); religion (Catholic, Protestant, Jewish, Nonreligious or Spiritual, other Christian, Hindu, other); education (less than bachelor’s, bachelor’s, master’s, terminal professional degrees); insurance coverage for fertility treatment (none, <50%, 50%–75% coverage; >75% coverage); and an indicator of whether the respondent is currently seeking/undergoing fertility treatment or if they have completed fertility treatment in the past.
Respondents also were asked to “select all that apply” from a list of aspects that made it “more difficult” to obtain fertility treatment. As shown in Table 3, the most commonly reported barrier was insurance status (16.6%), followed by income (12.5%). Respondents also identified their age (10.3%), profession (9.3%), weight (4.2%), and relationship status (3.8%) as reasons for difficulty obtaining treatment.
Among Black respondents, 14.7% reported that their race/ethnicity was a barrier to care compared with 0.0% of White, 5.1% of Hispanic, and 5.4% of Asian respondents (Table 3). Black (25%), Hispanic (16.5%), and Asian (16.3%) respondents were all more likely to report age as a barrier compared with White respondents (7.5%). Black and Hispanic respondents were roughly twice as likely to report weight (7.8% and 8.9%, respectively) as a barrier compared to White and Asian respondents.
Respondents with no insurance or <50% coverage for fertility care were at least twice as likely to report both income level and insurance status as barriers to care compared with respondents with 50%–100% coverage. Respondents with no insurance or <50% coverage (7.2%) also were more likely to report relationship status as a barrier compared to respondents with 50%–74% coverage (4.3%) and 75%–100% coverage (2.3%). Furthermore, 13.7% of Black respondents reported relationship status as a barrier, compared with 2.9% of White, 3.8% of Hispanic, and 3.4% of Asian respondents. Of respondents who reported relationship status as a barrier, 33.3% were divorced or separated, and 24.5% were single.
Within our sample, only 2.5% or fewer respondents reported religion, race/ethnicity, sexuality, gender identity, or citizen status as a barrier to treatment. Although 53.1% of respondents did not identify any personal characteristics that they perceived as barriers to fertility treatment, those within a lower-income bracket, <75% insurance coverage, and non-White race/ethnicity had significantly lower odds of reporting no difficulties.
Discussion
Our study demonstrates that access to fertility care is highly intersected with race and socioeconomic status. Despite prior research identifying such disparities and national efforts put in place by ASRM to improve access to care, major inequities persist. It is particularly disturbing that such disparities are present in a state that has a long-standing insurance mandate (since 1991) to cover fertility testing and treatment (including IVF) (9).
If there were truly no financial, racial, or cultural barriers to accessing fertility care, we would expect to see the demographics of those accessing such care to reflect the general population in the area of the clinic (17). Although our sample was geographically representative of the greater Chicago area (Supplemental Fig. 1, available online), it was disproportionately White, highly educated, and of dramatically higher socioeconomic status than the overall population of metropolitan Chicago. Only 52.0% of Chicago metropolitan area residents are non-Hispanic White, whereas this population comprised 75.5% of participants and 71.9% of the invited sample (18). In Chicago, the median household income in 2018 was $70,760 (18). However, 81.4% of survey respondents reported an annual household income >$100,000. Demographics alone demonstrate that racial and socioeconomic barriers exist that are preventing some women, particularly those from lower-income backgrounds and women of color, from seeking the treatment they need.
Our study was designed to update and expand on data collected via a survey administered in 2005 by Missmer and colleagues (5) to patients at a different Chicago fertility center. Respondents in our study waited less time before seeking treatment than those in the 2005 survey (25 vs. 35 months, respectively). Although it is promising to see a shorter duration before seeking fertility care, this time of trying to conceive unsuccessfully on their own is still too long. Missmer et al. (5) found that, compared with White women, Black and Hispanic women attempted to conceive for a longer time and found it harder to get appointments, take time off work, and pay for treatment. It is encouraging that we did not find significant racial disparities among these factors. These differences, however, may be attributable to the fact that our sample was composed of more White respondents than the 2005 sample (75.5% vs. 41.2% respectively). This may indicate that fertility care has likely become increasingly racially selective within the last 15 years.
In our study, compared with all other racial groups, White respondents reported the least difficulty in paying for treatments and/or medications. Our analysis also revealed that Black and Hispanic respondents traveled significantly further than White and Asian respondents traveled to reach the clinic, which is consistent with previous research (5, 17). The demographic composition of fertility patients, in addition to the economic and cultural barriers illuminated in this study, exemplify the various levels at which structural racism may contribute to health inequities across racial and ethnic groups (19, 20).
Despite our fertility center network being in a state with mandated insurance coverage for fertility treatment, economic concerns were the greatest barrier to accessing fertility care, with almost half of respondents reporting difficulty in paying for needed treatments and/or medications. Unfortunately, even in a mandated state like Illinois, exceptions exist to having fertility coverage. Employers may be exempt from following the mandate if the employer is headquartered outside of Illinois, has fewer than 25 employees, is not self-insured, or is a religious organization. Furthermore, public insurance options, such as Medicaid and Medicare, do not provide coverage for fertility treatment. Therefore, it is not surprising that approximately half of our respondents reported less than full coverage of fertility treatment. Our respondents with 0% or <50% coverage for fertility care were at least twice as likely to report both income level and insurance status as barriers to care compared with respondents with 50%–100% of care covered by insurance. According to an international economic analysis of fertility treatment use, only countries with funding systems that minimized out-of-pocket expenses met patient demand (4).
The socioeconomic barrier of fertility treatment continues to intersect with race and ethnicity, as twice as many Black and Hispanic respondents in our sample reported income level as a barrier compared with White and Asian respondents. This suggests that the financial burden of infertility disproportionately impacts Black and Hispanic women, in line with previous work highlighting the intersection between gender, race, and class and the compounded inequalities that exist between them, especially regarding healthcare (19).
Black respondents in this study were almost three times more likely than any other racial group to report that their race/ethnicity was a barrier to care, which is consistent with previous literature on racial inequities within access to fertility services (1, 5, 10). Black, Hispanic, and Asian respondents were significantly older than White respondents and more frequently reported their age as a barrier to treatment compared with White respondents. Studies report that women of color tend to wait to seek medical advice and care after a longer duration of infertility (5, 17). The term “structural reproduction” refers to postponing reproduction until financial stability is reached, making the right time to bear children too late for women to reproduce naturally (21). Other reports note a desire to conceive naturally, advice of physicians, exposure to racial discrimination, emotional stress, and function stress as reasons to delay starting treatment (21, 22, 23). This waiting period may be a reason why women of color in our study were more likely to report their age as a barrier. Age also may be a more likely issue for low-income individuals desiring greater financial stability before attempting to start a family. These disparities have been well-documented in the literature as a product of institutional and systemic racism that cause people of color frequently to experience worse health outcomes compared with White populations (19, 20).
Concerning reported causes of infertility, our study found that Black women were significantly more likely to have a uterine factor, and both Black and Hispanic women were significantly more likely to have tubal factor compared with White women. It is well-established that Black women have a two- to threefold greater incidence of uterine fibroids compared with White women (24, 25). Furthermore, Black women also develop fibroid-related symptoms on average four to six years younger and may even present with disease in their 20s (26, 27). Furthermore, consistent with national surveillance data from the Centers for Disease Control and Prevention, Black and Hispanic women have higher rates of gonorrhea and chlamydia infections, which are known contributors to tubal damage and infertility (28). Our findings also are consistent with prior studies (17, 28, 29) and highlight the importance of early education to prevent sexually transmitted infections, along with encouraging early testing for fibroids and tubal patency via hysterosalpingogram or saline infusion sonogram.
Strengths of our study include a large sample size (more than double from the Missmer et al. study) that was demographically similar to the population of infertility patients being studied. Furthermore, our respondents were geographically representative of the population in metropolitan Chicago. If this is the situation in a major city, access is likely worse in more rural areas. A potential limitation is that our entire population had already accessed fertility care and, therefore, had overcome other existing barriers to accessing care that we did not identify. Very few (≤2.5%) of our respondents reported religion, race/ethnicity, sexuality, gender identity, and/or citizen status to have inhibited their access to treatment, whereas previous literature shows that these barriers limit access to care (10, 19). Individuals who face such barriers, therefore, likely did not present to our fertility center for care. Furthermore, e-mail surveys also may have been inaccessible to patients without internet access. Although survey respondents were nearly identically similar to nonrespondents in age, sex, and race/ethnicity, the degree to which our sample is representative of the broader patient population with respect to income, education, and other factors is unknown because of the absence of these data within the electronic data warehouse.
In summary, significant racial and socioeconomic disparities persist among fertility patients accessing care in a large, demographically diverse city with a state mandate to cover fertility testing and treatment. If this situation is present in Chicago, Illinois, such disparities are likely amplified in other cities or states with no insurance mandate. The lack of demographic representation with respect to race and class among fertility patients provides evidence that many individuals in the US who may benefit from access to fertility care likely go untreated or undertreated (7). Our study supports policy recommendations that advance financial assistance programs to improve the affordability of fertility treatment, making it accessible to the general population rather than a select socioeconomically advantaged subgroup. Mandatory fertility counseling to all patients of reproductive age at annual medical appointments may also improve patient confidence in reproductive care options and ameliorate access to fertility care.
Further studies are needed in nonmandated states to see how the need for improved access to fertility care may differ across states with various insurance mandates. Our study also calls on future research to use similar measures in both private and community-based primary and fertility care settings to investigate the intersection of social, cultural, racial, and economic factors that may completely prohibit many individuals from accessing the fertility care they need and deserve.
Acknowledgments
The authors thank Angela Lawson, Ph.D., Jocyln Dorney, B.S., and Deepthi Devireddy, B.S. for their assistance with survey design.
Footnotes
All authors have nothing to disclose.
Supplementary data
Survey respondents on the basis of residential zip code displayed on map of Northeast Illinois (greater Chicago area), Northwest Indiana, and Southeast Wisconsin.
Survey instrument used for the study
References
- 1.Chandra A., Copen C.E., Stephen E.H. Infertility and impaired fecundity in the United States, 1982-2010: data from the National Survey of Family Growth. Natl Health Stat Report. 2013;67:1–18. [PubMed] [Google Scholar]
- 2.Jain T., Grainger D.A., Ball G.D., Gibbons W.E., Rebar R.W., Robins J.C. 30 years of data: impact of the United States in vitro fertilization data registry on advancing fertility care. Fertil Steril. 2019;111:477–488. doi: 10.1016/j.fertnstert.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 3.Jain T., Missmer S.A., Hornstein M.D. Trends in embryo-transfer practice and in outcomes of the use of assisted reproductive technology in the United States. N Engl J Med. 2004;350:1639–1645. doi: 10.1056/NEJMsa032073. [DOI] [PubMed] [Google Scholar]
- 4.Chambers G.M., Sullivan E.A., Ishihara O., Chapman M.G., Adamson G.D. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91:2281–2294. doi: 10.1016/j.fertnstert.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 5.Missmer S.A., Seifer D.B., Jain T. Cultural factors contributing to health care disparities among patients with infertility in Midwestern United States. Fertil Steril. 2011;95:1943–1949. doi: 10.1016/j.fertnstert.2011.02.039. [DOI] [PubMed] [Google Scholar]
- 6.Staniec J.F.O., Webb N.J. Utilization of infertility services: how much does money matter? Health Serv Res. 2007;42:971–989. doi: 10.1111/j.1475-6773.2006.00640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ethics Committee of the American Society for Reproductive Medicine. Disparities in access to effective treatment for infertility in the United States: an Ethics Committee opinion. Fertil Steril. 2015;104:1104–1110. doi: 10.1016/j.fertnstert.2015.07.1139. [DOI] [PubMed] [Google Scholar]
- 8.Guzman G. US Census Bureau; 2019. Household Income: 2018 American Community Survey Briefs. [Google Scholar]
- 9.Jain T., Hornstein M.D. Disparities in access to infertility services in a state with mandated insurance coverage. Fertil Steril. 2005;84:221–223. doi: 10.1016/j.fertnstert.2005.01.118. [DOI] [PubMed] [Google Scholar]
- 10.Kelley A.S., Qin Y., Marsh E.E., Dupree J.M. Disparities in accessing infertility care in the United States: results from the National Health and Nutrition Examination Survey, 2013-16. Fertil Steril. 2019;112:562–568. doi: 10.1016/j.fertnstert.2019.04.044. [DOI] [PubMed] [Google Scholar]
- 11.Jain T., Harlow B.L., Hornstein M.D. Insurance coverage and outcomes of in vitro fertilization. N Engl J Med. 2002;347:661–666. doi: 10.1056/NEJMsa013491. [DOI] [PubMed] [Google Scholar]
- 12.Jain T., Hornstein M.D. To pay or not to pay. Fertil Steril. 2003;80:27–29. doi: 10.1016/s0015-0282(03)00576-4. [DOI] [PubMed] [Google Scholar]
- 13.Reindollar R.H. Surfing the waves of change in reproductive medicine: past, present and future. A presentation of the 2014 ASRM Strategic Plan. Fertil Steril. 2015;103:35–38. doi: 10.1016/j.fertnstert.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 14.Adashi E, Bell A, Farquhar C, Allen B, de Ziegler D, Fujimoto V et al. White paper: Access to Care Summit 2015. Available at: https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/news-and-research/press-releases-and-bulletins/pdf/atcwhitepaper.pdf. Accessed February 16, 2021.
- 15.Seifer D.B., Sharara F.I., Jain T. Toward a better understanding of racial disparities in utilization and outcomes of IVF treatment in the USA. In: Sharara F.I., editor. Ethnic differences in fertility and assisted reproduction. Springer New York; New York, NY: 2013. pp. 239–244. [Google Scholar]
- 16.Fujimoto V.Y., Jain T., Alvero R., Nelson L.M., Catherino W.H., Olatinwo M. Proceedings from the conference on Reproductive Problems in Women of Color. Fertil Steril. 2010;94:7–10. doi: 10.1016/j.fertnstert.2009.12.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jain T. Socioeconomic and racial disparities among infertility patients seeking care. Fertil Steril. 2006;85:876–881. doi: 10.1016/j.fertnstert.2005.07.1338. [DOI] [PubMed] [Google Scholar]
- 18.United States Census Bureau. American Community Survey 2018. Available at: https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/2018/. Accessed February 16, 2021.
- 19.Gee G.C., Ford C.L. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8:115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 21.Bennett L.R., de Kok B. Reproductive desires and disappointments. Med Anthropol. 2018;37:91–100. doi: 10.1080/01459740.2017.1416609. [DOI] [PubMed] [Google Scholar]
- 22.Domar A., Gordon K., Garcia-Velasco J., La Marca A., Barriere P., Beligotti F. Understanding the perceptions of and emotional barriers to infertility treatment: a survey in four European countries. Hum Reprod. 2012;27:1073–1079. doi: 10.1093/humrep/des016. [DOI] [PubMed] [Google Scholar]
- 23.Sondik E.J., Huang D.T., Klein R.J., Satcher D. Progress toward the healthy people 2010 goals and objectives. Annu Rev Public Health. 2010;31:271–281. doi: 10.1146/annurev.publhealth.012809.103613. [DOI] [PubMed] [Google Scholar]
- 24.Baird D.D., Dunson D.B., Hill M.C., Cousins D., Schectman J.M. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–107. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 25.Marshall L.M., Spiegelman D., Barbieri R.L., Goldman M.B., Manson J.E., Colditz G.A. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997;90:967–973. doi: 10.1016/s0029-7844(97)00534-6. [DOI] [PubMed] [Google Scholar]
- 26.Huyck K.L., Panhuysen C.I., Cuenco K.T., Zhang J., Goldhammer H., Jones E.S. The impact of race as a risk factor for symptom severity and age at diagnosis of uterine leiomyomata among affected sisters. Am J Obstet Gynecol. 2008;198:168.e19. doi: 10.1016/j.ajog.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kjerulff K.H., Langenberg P., Seidman J.D., Stolley P.D., Guzinski G.M. Uterine leiomyomas. Racial differences in severity, symptoms and age at diagnosis. J Reprod Med. 1996;41:483–490. [PubMed] [Google Scholar]
- 28.From the Centers for Disease Control and Prevention Impact of closure of a sexually transmitted disease clinic on public health surveillance of sexually transmitted diseases--Washington, D.C., 1995. JAMA. 1999;281:127–128. [PubMed] [Google Scholar]
- 29.Fujimoto V.Y., Luke B., Brown M.B., Jain T., Armstrong A., Grainger D.A. Racial and ethnic disparities in assisted reproductive technology outcomes in the United States. Fertil Steril. 2010;93:382–390. doi: 10.1016/j.fertnstert.2008.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survey respondents on the basis of residential zip code displayed on map of Northeast Illinois (greater Chicago area), Northwest Indiana, and Southeast Wisconsin.
Survey instrument used for the study