Abstract
Objective
To study the feasibility of fertility preservation in a transgender man without an extended period of androgen cessation.
Design
Report of a foundational case of oocyte cryopreservation in a transgender man without stopping testosterone therapy before controlled ovarian stimulation. We performed a literature review, identifying five publications on oocyte cryopreservation outcomes in transgender men on testosterone.
Setting
A university-affiliated fertility clinic in Canada.
Patient(s)
A 28-year-old transgender man taking testosterone for 3 years requesting oocyte cryopreservation before gender-affirming surgery. He desired to proceed without stopping testosterone. Pretreatment antimüllerian hormone level was 1.89 ng/mL. The patient’s consent was obtained for written publication.
Intervention(s)
Testosterone was stopped for only three doses (immediately before and during ovarian stimulation). A standard antagonist protocol was used with letrozole to minimize estrogenic side effects.
Main Outcome Measure(s)
Number of oocytes retrieved and days off testosterone.
Result(s)
Thirteen oocytes were retrieved; 11 were mature and vitrified. The total time off testosterone was 24 days. In all prior publications, testosterone was stopped for 3–6 months.
Conclusion(s)
Transgender men have traditionally discontinued exogenous testosterone until the resumption of menses (≤6 months). This is known to be distressing. This is the first published case demonstrating the feasibility of ovarian stimulation without prolonged testosterone cessation in a transgender man. Future studies with a larger sample size should be performed to confirm these findings. The short duration off testosterone may improve patient’s experiences, increase treatment acceptability, and decrease gender dysphoria for transgender men considering fertility preservation.
Key Words: Fertility preservation, transgender, ovarian stimulation, testosterone, androgen, oocyte cryopreservation
Discuss: You can discuss this article with its authors and other readers at https://www.fertstertdialog.com/users/16110-fertility-and-sterility/posts/61706-xfre00006
When proceeding with hormone therapy or gender-affirming surgery, transgender patients should have the option of undergoing fertility preservation. Before assisted reproductive technology (ART), transgender men have traditionally had to discontinue their exogenous testosterone for ≤6 months, or until resumption of menses. The process and experience associated with stopping testosterone has proven to be distressing for patients.
This report explores the feasibility of proceeding with fertility preservation in a transgender man without an extended period of androgen cessation and without the resumption of menstruation. We also performed a literature review on oocyte cryopreservation outcomes in transgender men on testosterone.
Materials and methods
With the patient’s written informed consent, a retrospective chart review was performed at a university-affiliated fertility clinic in Burnaby, Canada. A literature review was performed in the search engines Ovid/ Medline, PubMed, and Google Scholar by one investigator (K.C.). Several combinations of the following search terms were used: transgender men, transgender, testosterone, ovarian stimulation, fertility preservation, and in vitro fertilization. All cases reported up until 2019 in the English literature were included. Additional review was carried out and “similar articles” were added as recommended by the search engines.
Results
Our patient is a 28-year-old transgender man who had been taking testosterone therapy for 3 years. He was referred for fertility preservation consultation before gender-affirming surgery in the form of hysterectomy and bilateral salpingo-oophorectomy. He was nulliparous with regular and unremarkable menses before the start of testosterone therapy. He denied previous hormonal contraceptive pill use. He was healthy and had already undergone bilateral mastectomy. He was taking testosterone (0.6 mg intramuscularly weekly). On examination, vital signs were normal, and his body mass index was 18.99 kg/m2. An internal pelvic examination was deferred at the patient’s request. Transabdominal ultrasound showed a normal anteverted uterus (volume, 38.63 cm3) and a thin endometrial stripe (2.1 mm) with normal ovaries bilaterally.
His serum antimüllerian hormone (AMH) level was 18.2 pmol/L (2.5 ng/mL), performed while on testosterone therapy. The options for fertility preservation were reviewed in detail and the patient expressed interest in oocyte cryopreservation. It was recommended that the patient discontinue testosterone therapy and wait for the resumption of menses before the initiation of ovarian stimulation. He also agreed to the use of letrozole during ovarian stimulation to suppress estrogen production and its associated biologic effects, including feminization. However, the patient did not return for follow-up until 1.5 years later. Repeat AMH was 13.5 pmol/L (1.89 ng/mL) (Table 1). He was uncomfortable with the prolonged discontinuation of testosterone in the initial treatment plan. He expressed a desire to proceed without stopping testosterone. He was counseled regarding the paucity of evidence for ovarian stimulation in transgender men previously using testosterone. Previous cases series report successful ovarian stimulation with a minimum of 3 months off testosterone. There are no reported cases of continuing testosterone therapy. After a thorough discussion of the risks and benefits, he elected to proceed with ovarian stimulation with a minimal duration of testosterone cessation.
Table 1.
Baseline laboratory test results before ovarian stimulation.
| Laboratory tests | The patient’s test result | Reference ranges |
|---|---|---|
| AMH | 13.5 pmol/L | 6.4–70.3 pmol/L |
| Hemoglobin | 156 g/L | 115–155 g/L |
| Ferritin | 160 μg/L | 15–247 μg/L |
| Follicle-stimulating hormone | 0.8 IU/L | <8.7 IU/L |
| Luteinizing hormone | 0.3 IU/L | 2.4–6.6 IU/L |
| Estradiol | 60 pmol/L | N/A |
| Progesterone | 0.4 nmol/L | N/A |
| Testosterone | 33.3 nmol/L | <1.8 nmol/L |
| DHEA sulphate | 5.0 μmol/L | <10.8 μmol/L |
| Androstenedione | 2.5 nmol/L | 0.91–7.47 nmol/L |
| HDL cholesterol | 1.56 mmol/L | >1.19 mmol/L |
| Cholesterol | 4.96 mmol/L | 2.00–5.19 mmol/L |
| Cholesterol:HDL risk ratio | 3.18 | <4.4 |
| Thyroid stimulating hormone | 0.99 mU/L | 0.32–5.04 mU/L |
AMH = antimüllerian hormone; DHEA = dehydroepiandrosterone; HDL = high-density lipoprotein; N/A = not available.
He stopped testosterone 1 week before gonadotropin administration. He received follitropin alfa 300 IU (Gonal-F, Merck Canada) and menotropins 150 IU (Menopur, Ferring Canada) subcutaneously for 13 consecutive days beginning on the seventh day after discontinuing testosterone. Daily ganirelix acetate 0.25mg (Orgalutran, Merck) was started on day 5 until the day of final oocyte maturation. Letrozole (7.5 mg) was taken orally from ovarian stimulation day 1 until 7 days after oocyte retrieval. His follicle tracking was performed by transabdominal ultrasound without difficulty. When the three lead follicles reached 17 mm on day 14, chorionic gonadotropin 5,000 IU (Pregnyl, Merck Canada), triptorelin 0.2 mg (Decapeptyl, Ferring Canada), and follitropin alfa (300 IU; Gonal-F) were given. The endometrium achieved a thickness of 5.3 mm, as assessed on the day of human chorionic gonadotropin administration. There were 12 follicles that measured >12 mm in mean follicular diameter. He underwent an uncomplicated transvaginal oocyte retrieval at 36 hours after human chorionic gonadotropin trigger. Thirteen oocytes were recovered, of which 11 were mature and vitrified (Fig. 1). He resumed testosterone the next day. In total, the duration of time off testosterone was 24 days. The patient reported no major side effects related to the ovarian stimulation aside from one episode of self-limiting vaginal spotting that occurred 14 days after retrieval, presumed to be a withdrawal bleed.
Figure 1.
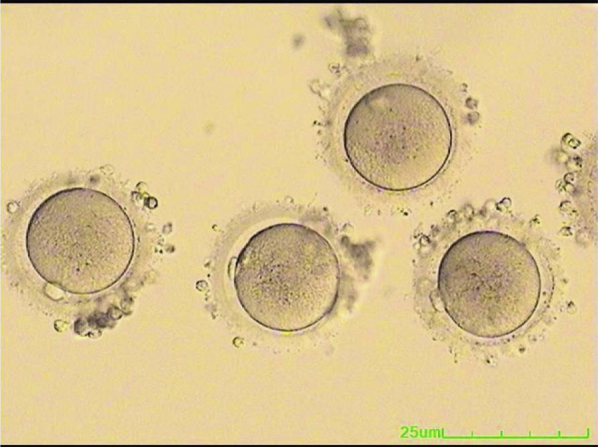
Mature oocytes from a transgender man who stopped testosterone use only 1 week before controlled ovarian stimulation.
The literature review identified five articles reporting on the outcomes of in vitro fertilization in transgender men previously on testosterone therapy (Table 2). There were two case reports and three cohort studies. Overall, 30 transgender men were included. In the abstract by Rodriguez-Wallberg et al. (2), the management of testosterone before and/or during controlled ovarian stimulation was not reported. All of the other 25 transmen stopped testosterone hormone therapy for 3–6 months or until the resumption of menses before undergoing controlled ovarian stimulation.
Table 2.
A summary of literature on the outcomes of in vitro fertilization in transgender men on testosterone therapy.
| Author, Year of publication | Type of study | Patient population (n), control group (n) | Testosterone management | Treatment | Outcomes |
|---|---|---|---|---|---|
| Gidoni et al., 2013 (1) | Case report (abstract) | 37-year-old transgender man on testosterone for 14 years (n = 1); no control group | Stopped testosterone, spontaneous menses start after 4 months | 2 cycles of ART | First cycle: 12 mature oocytes retrieved, 4 day 3 embryo Second cycle: 15 mature oocytes retrieved, 12 day 3 embryo |
| Rodriguez-Wallberg et al., 2014 (2) | Prospective study (abstract) | Transgender men referred for fertility consultation on androgen treatment (n = 5); no control group | Did not specify | ART | 6 patients underwent hormonal stimulation and oocyte cryopreservation; average oocyte number is 13 with a maturity rate of 88%. It is not reported what proportion of these patients were on testosterone treatment |
| Broughton et al., 2017 (3) | Case report | 30-year-old transgender man treated with testosterone for 26 months (n = 1); no control group | Testosterone was discontinued for 3 months before cycle start | ART | 16 oocytes retrieved, 13 mature oocytes, 7 embryos (2 were transferred, 1 was cryopreserved, 4 were discarded) Ongoing pregnancy was carried by his partner after the oocyte was fertilized with donor sperm |
| Leung et al., 2019 (4) | Matched retrospective cohort study | Transgender men on testosterone therapy (n = 16); cisgender women (n = 130) | All stopped testosterone before cycle start. The average time off testosterone treatment before ovarian stimulation was 4.5 months | ART | There was no statistically significant difference in age, AMH, number of oocytes retrieved, number of mature oocytes, or peak serum estradiol level between the cisgender patients and transgender patients previously exposed to testosterone |
| Adeleye et al., 2019 (5) | Retrospective cohort study | Transgender men with androgen use (n = 7); transgender men without androgen use (n = 6), cisgender women (n = 13) | Testosterone was stopped approximately 6 months before stimulation | ART | There was a higher number of oocytes retrieved in the transmen without testosterone (25.5, IQR 18–28) compared with those with history of testosterone use (12, IQR 4–26) (P = .038); however, when 2 outliers with AFC <5 were removed from the analysis, there was no difference in number of oocyte retrieved (P = .119). All 3 transgender men conceived with own oocyte after androgen exposure |
AFC = antral follicle count; IQR = interquartile range.
Discussion
In 2016, an estimated 1.4 million people identified as transgender in the United States (6, 7), with an increase in prevalence over time (4). Although the degree and the type of gender-affirming therapy pursued are individualized, ≤49% of those surveyed received hormone therapy and 25% reported surgical management (6). Gender-affirming medical and surgical treatments can impact fertility potential (6). For transgender men (female-to-male, transmen, transmasculine), the use of testosterone may affect gonadal histology and function with unknown long-term effects on fertility (6). Furthermore, surgical management for transmen with hysterectomy and oophorectomy will result in sterility (6). Importantly, >50% of transgender people may desire to have children (6); and in one study (7), close to 50% of participants would like to have biologic offspring. Thus, numerous medical associations, including the World Professional association for Transgender Health and the American Society of Reproductive Medicine, recommend reviewing the options for fertility preservation before gender-affirming hormone or surgical therapy (6). Despite this, there is a dearth of literature regarding the most effective fertility preservation protocol in transgender men currently taking testosterone.
As there has been contrasting evidence regarding the effect of testosterone therapy on ovarian histopathology (6, 7), patient counseling on the success rates of oocyte cryopreservation can be challenging. Grynberg et al. (8) reported a histologic trend toward polycystic ovarian morphology with stromal hyperplasia, increased ovarian volume, and numerous ovarian follicles in hormonally transitioned transgender men who underwent oophorectomy. In contrast, De Roo et al. (9) reported no change in the distribution of ovarian follicles after the use of testosterone for >1 year. They also reported that the number of ovarian follicles detected was not associated with the duration of testosterone therapy, and the mitotic spindle patterns appeared normal with a normal complement of chromosomes in most mature oocytes obtained from in vitro maturation of the ovaries exposed to testosterone (7, 9, 10). It is important to note that prior studies did not report whether the gonadal effects observed reversed after testosterone cessation (7).
There is also conflicting evidence regarding the oocyte yield in testosterone-primed ovaries. In the largest retrospective cohort study in transgender men by Leung et al. (4; Table 2), there is a trend toward a higher number of oocyte retrieved in the transgender cohort (18.6 ± 9.3) compared with the cisgender group (14.4 ± 8.9) (P = .11). The biologic basis for increased oocyte yield may be comparable to the use of testosterone pretreatment before ART in cisgender women with low ovarian reserve. It is postulated that low-dose transdermal testosterone may improve follicular response and sensitivity to follicle-stimulating hormone (11). It was also shown in animal studies that androgens can promote the number and survival of small antral follicles (12). It can be theorized that the biochemical environment resulting from androgen use may be similar to those with polycystic ovary syndrome, a condition associated with high ovarian reserve (4). However, in the study by Caanen et al. (13), transvaginal ultrasound assessment of the antral follicle count and ovarian volume in 56 transgender men on testosterone did not show statistically significant differences compared with the older cisgender control group. Furthermore, in a similar but smaller study (5), there was no difference in the number of follicles at cycle start between the transgender men with prior androgen exposure and those without. There was a higher number of oocytes retrieved in the group of transmen not undergoing testosterone therapy compared with those with a history of testosterone use. However, when the two outliers with antral follicle counts more than five were removed from the analysis, there was no difference in number of oocytes retrieved (P = .12) (5). Overall, there is limited clinical evidence on the outcomes of fertility preservation in patients on testosterone (7).
One notable challenge is that there is no professional guidelines specifying the duration or necessity of testosterone cessation before ovarian stimulation (7, 4, 3). Theoretical concerns of testosterone exposure during ART includes adverse effect on the hormonal milieu, negative influence on IVF outcomes, and virilization of the female fetus in the case of pregnancy after fresh embryo transfer (3). In primates, the use of high-dose testosterone therapy 5 days before and throughout gonadotropin stimulation has been shown to oppose ovarian function (11). In our patient, his prestimulation AMH was below average for his age and showed an expected decrease in the 1.5-year delay before ovarian stimulation (14). This may be explained by reproductive aging or the suppression of the reproductive axis by high-dose testosterone. In a prospective study by Caanen et al. (13), they reported a significantly lower serum AMH level 16 weeks after starting testosterone and aromatase inhibitor compared with baseline. Although the previous studies have used a varied and arbitrary range of 3–6 months off testosterone before ART and demonstrated good oocyte yield (4, 5, 3), our case report is important as it is the first report in the literature to show the feasibility of a short duration of testosterone cessation.
It is known that gender dysphoria may be exacerbated during the process of fertility preservation (7, 15). Transgender men who undergo ART can experience distress with the use of hormones during their treatment (6, 4). Approaches to minimize patient distress currently include the use of aromatase inhibitors to suppress serum estradiol, transabdominal pelvic ultrasound for follicular monitoring, and demonstration of contextual sensitivity by health care professionals (7, 15). Physical changes from the cessation of testosterone, such as fatigue, feminization of voice, menstrual function, can escalate gender dysphoria and incongruence (6, 15). Recently, in the largest cohort study (4) of transgender men undergoing fertility preservation with ART, all participants stopped testosterone and either experienced the resumption of menses or had serum testosterone in the female range before ovarian stimulation. The average duration of androgen cessation was 4.5 months (4). In addition, ≤50% of transgender men who presented to consider fertility treatment at the study site did not proceed with treatment, citing androgen cessation as one of the major barriers to treatment (4). In the study by Adeleye et al. (5), all patients discontinued androgen use for approximately 6 months and they were menstruating before starting ovarian stimulation. Our patient delayed oocyte cryopreservation by 1.5 years due to his apprehension regarding androgen cessation. Given the known distress that transmen may experience in this situation, it would be invaluable to have the option to continue testosterone therapy until just before ovarian stimulation.
In conclusion, this is the first case report demonstrating the feasibility of ovarian stimulation for fertility preservation in a transgender man without a prolonged cessation of testosterone. Future studies with a larger sample size should be carried out to confirm these findings. Longer term outcomes, including fertilization, euploid embryo, and live birth rates, would also be valuable. A short duration of time off of testosterone may improve the patient’s experience, increase treatment acceptability, and decrease gender dysphoria for transgender men considering fertility preservation.
Acknowledgments
The authors thank the patient for providing consent for written publication and to our embryology team for the oocyte photos.
Footnotes
K.C. has nothing to disclose. R.H. has nothing to disclose. J.R. has nothing to disclose. C.D. has nothing to disclose.
References
- 1.Gidoni Y.S., Raziel A., Strassburger D., Kasterstein E., Ben-Ami I., Ron-El R. Can we preserve fertility in a female to male trangender after a long term testosterone treatment- case report. Fertil Steril [Internet] 2013;100:S169–S170. [Google Scholar]
- 2.Rodriguez-Wallberg K.A., Dhejne C., Stefenson M., Degerblad M., Olofsson J.I. Preserving eggs for men’s fertility. a pilot experience with fertility preservation for female-to-male transsexuals in sweden. Fertil Steril [Internet] 2014;102:e160–e161. [Google Scholar]
- 3.Broughton D., Omurtag K. Care of the transgender or gender-nonconforming patient undergoing in vitro fertilization. Int J Transgenderism. 2017;18(4):372–375. [Google Scholar]
- 4.Leung A., Sakkas D., Pang S., Thornton K., Resetkova N. Assisted reproductive technology outcomes in female-to-male transgender patients compared with cisgender patients: a new frontier in reproductive medicine. Fertil Steril. 2019;112(5):858–865. doi: 10.1016/j.fertnstert.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Adeleye A.J., Cedars M.I., Smith J., Mok-Lin E. Ovarian stimulation for fertility preservation or family building in a cohort of transgender men. J Assist Reprod Genet. 2019;36(10):2155–2161. doi: 10.1007/s10815-019-01558-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng P.J., Pastuszak A.W., Myers J.B., Goodwin I.A., Hotaling J.M. Fertility concerns of the transgender patient. Transl Androl Urol. 2019;8(3):209–218. doi: 10.21037/tau.2019.05.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moravek M.B. Fertility preservation options for transgender and gender-nonconforming individuals. Curr Opin Obstet Gynecol. 2019;31(3):170–176. doi: 10.1097/GCO.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 8.Grynberg M., Fanchin R., Dubost G. Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reprod Biomed Online. 2010;20(4):553–558. doi: 10.1016/j.rbmo.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 9.De Roo C., Lierman S., Tilleman K. Ovarian tissue cryopreservation in female-to-male transgender people: insights into ovarian histology and physiology after prolonged androgen treatment. Reprod Biomed Online. 2017;34(6):557–566. doi: 10.1016/j.rbmo.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Lierman S., Tilleman K., Braeckmans K. Fertility preservation for trans men: frozen-thawed in vitro matured oocytes collected at the time of ovarian tissue processing exhibit normal meiotic spindles. J Assist Reprod Genet. 2017;34(11):1449–1456. doi: 10.1007/s10815-017-0976-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fábregues F., Peñarrubia J., Creus M. Transdermal testosterone may improve ovarian response to gonadotrophins in low-responder IVF patients: a randomized, clinical trial. Hum Reprod. 2009;24(2):349–359. doi: 10.1093/humrep/den428. [DOI] [PubMed] [Google Scholar]
- 12.Caanen M.R., Soleman R.S., Kuijper E.A. Antimüllerian hormone levels decrease in female-to-male transsexuals using testosterone as cross-sex therapy. Fertil Steril. 2015;103(7):1340–1345. doi: 10.1016/j.fertnstert.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Caanen M.R., Schouten N.E., Kuijper E.A.M. Effects of long-term exogenous testosterone administration on ovarian morphology, determined by transvaginal (3D) ultrasound in female-to-male transsexuals. Hum Reprod. 2017;32(7):1457–1464. doi: 10.1093/humrep/dex098. [DOI] [PubMed] [Google Scholar]
- 14.Seifer D.B., Baker V.L., Leader B. Age-specific serum anti-Müllerian hormone values for 17,120 women presenting to fertility centers within the United States. Fertil Steril. 2011;95(2):747–750. doi: 10.1016/j.fertnstert.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 15.Armuand G., Dhejne C., Olofsson J.I., Rodriguez-Wallberg K.A. Transgender men’s experiences of fertility preservation: a qualitative study. Hum Reprod. 2017;32(2):383–390. doi: 10.1093/humrep/dew323. [DOI] [PubMed] [Google Scholar]


