Abstract
Background
A correct visual skill demonstration is important when learning cardiopulmonary resuscitation (CPR) and the use of an automated external defibrillator (AED). Basic life support (BLS) instructors are expected to master and demonstrate CPR/AED skills correctly. The aim of this study was to evaluate certified BLS instructors’ competencies in demonstrating CPR and the use of an AED.
Methods
Certified BLS instructors demonstrated CPR and the use of an AED on a resuscitation manikin. Skills were evaluated using data collected from the manikin and video recordings and compared to resuscitation guidelines. Further, instructors completed questionnaires on resuscitation guidelines and rating of their own CPR/AED skills.
Results
Overall, we analyzed data from 125 instructors. Of all chest compressions, only 22% were within guideline recommendations regarding depth. Instructors performed chest compressions with excessive depth (mean depth 64 mm (7.3)) and a mean rate of 115 min−1 (10.8). Only 25% of instructors placed the left AED electrode correctly (median distance 7.6 cm (5.0;10.5)), while the right AED electrode usually was placed correctly (median distance 2.9 cm (1.5;4.0), 85% placed correctly). Nearly half of the instructors failed to state correct answers regarding how to diagnose a cardiac arrest and where to place the AED electrodes. Despite their performance, instructors rated their BLS skills as good.
Conclusion
Certified BLS instructors’ have poor CPR/AED skills and several important knowledge gaps on CPR/AED guidelines in contrast to instructors’ self-reported skills. This highlights a need for improving BLS instructor education, including continuous faculty development to ensure optimal learning conditions for BLS course participants.
Keywords: Basic life support, Instructor, Training, Cardiopulmonary resuscitation, Automated external defibrillator
Introduction
Out-of-hospital cardiac arrest carries a poor prognosis with a survival of approximately 10%.1 High-quality bystander cardiopulmonary resuscitation (CPR)2 and early defibrillation with an automated external defibrillator (AED)3 can more than triple survival. Therefore, it is essential that laypeople learn to perform high-quality CPR and to use an AED correctly.
A majority of laypeople attend basic life support (BLS) courses to learn CPR and the use of an AED. During these courses, an instructor is responsible for communicating correct skill performance through, e.g. a skill demonstration. Previous studies have found poor skills among laypeople after completion of a BLS training course.4, 5, 6 Therefore, many studies have explored the efficiency of different teaching and feedback methods6, 7, 8, 9, 10 to improve BLS courses’ learning outcome.11, 12, 13 However, BLS instructors’ competencies in CPR/AED skills and their ability to correctly demonstrate and describe the curriculum to learners is likely to affect learning outcome. Indeed, previous studies have suggested that the poor outcomes among laypeople after attending BLS courses may result from the instructors’ lack of competence in the skills they are teaching or deviation from the curricula.11, 12, 14, 15 The main focus of previous studies has been participants’ learning outcomes, requiring that the instructors are competent. However, a quantitative assessment of BLS instructors’ CPR and AED usage skills has not yet been undertaken.
The aim of this study was to evaluate certified BLS instructors’ competence in demonstrating CPR/AED skills. Additionally, to study BLS instructors’ knowledge on BLS guidelines and self-reported skills.
Methods
Study design
This study was a prospective observational study where certified BLS instructors were asked to demonstrate CPR and use an AED in a simulated teaching situation, and complete a questionnaire on theoretical BLS knowledge and their self-reported skills.
Participants
BLS instructors (age ≥18 years) certified by The Danish First Aid Council and/or the European Resuscitation Council (ERC) were recruited at BLS instructor gatherings (e.g. general assemblies and symposia). Instructors were informed about the study and the possibility of participating at the beginning of the specific event and/or sent information by e-mail prior to the gatherings, e.g. a newsletter for the specific event. Instructors were encouraged to participate, e.g. during intermissions. Instructors were not aware of the specific outcome measures of the study. Instructors were excluded if they were physically unable to perform CPR and/or use an AED on the day of the skill test.
Test protocol
Instructors were asked to demonstrate CPR and operate a training AED on a resuscitation manikin with arms (AMBU Man®, AMBU, Ballerup, Denmark) as they would do in a teaching situation but without verbal explanations or pauses. The test was conducted in two parts: (1) instructors demonstrated three full cycles of CPR on a manikin capable of collecting data on CPR quality, and (2) instructors demonstrated the use of an AED (Lifepak CR-T AED Trainer, Physio Control, Redmond, WA, USA [semi-automatic external defibrillator]) programmed to a single shock scenario. After shock delivery, the test was stopped. In-between the two parts, the manikin was reset to the “starting position” with the arms along the side and the manikin’s shirt fully zipped. Neither feedback nor help were given during the test.
The entire test was video recorded for subsequent analysis. Before the test, instructors completed a questionnaire collecting demographic information and instructors’ rating of their own ability to perform CPR and use an AED using a 5-point Likert scale. After the test, instructors completed a questionnaire on resuscitation guidelines. Instructors were asked to reevaluate their own ability to perform CPR and use an AED after receiving an individual performance report per e-mail that showed data on how well the instructor performed chest compressions and rescue breathing.
Data collection and assessment
Data from the manikin on chest compression and rescue breathing quality was collected via AMBU© Software (AMBU, Ballerup, Denmark). The first three cycles of CPR were analyzed for each instructor. Correctly performed CPR was defined in accordance with the European Resuscitation Council (ERC) Guidelines 201516; 30 (±2) chest compressions at a depth of 50−60 mm with a rate of 100–120 min−1, and rescue breaths with a tidal volume of 500−600 mL.
After the skill test, a measuring tape forming a X–Y-coordinate system was placed on the manikin to measure the distance from the center of the AED electrode to the position recommended by the ERC, i.e. the right electrode to the right of the sternum, below the clavicle and the left apical-lateral electrode in the left mid-axillary line approximately level with the V6 ECG electrode. The placement of the electrodes was digitally photographed and subsequently analyzed in ImageJ (version 1.48v, National Institutes of Health, USA).5 Placement of electrodes within 5 cm of the recommended position was considered correct as in previous studies5, 17, 18, 19.
The test was video recorded to collect data on hand placement during chest compressions, rate of rescue breaths, movement of the left arm of the manikin during electrode placement, and time to shock delivery. Two assessors independently reviewed the videos. In case of discrepancies, the videos were jointly re-assessed until consensus was reached.
The questionnaire on resuscitation guidelines consisted of ten open-ended questions, as presented in Table 3. All questions were based on the BLS curriculum and were therefore considered basic knowledge necessary to teach correct BLS. Answers were reviewed and assessed by two experienced resuscitation researchers. A third and senior resuscitation researcher was consulted to achieve consensus in cases of disagreement. If the answers could be interpreted as corresponding to ERC Guidelines 2015,16, 20 they were coded as correct. In case of doubt, the conclusion correct/in-correct was made in favor of the participant.
Table 3.
Theoretical knowledge of resuscitation guidelines.
| Theoretical knowledge | |
|---|---|
| Question | Correct answers |
| What are the diagnostic criteria for cardiac arrest? | 58% (73) |
| What is the Danish emergency telephone number? | 100% (125) |
| How many chest compressions should be given per CPR cycle? | 100% (125) |
| How many rescue breaths should be given per CPR cycle? | 100% (125) |
| What is the correct hand position for chest compressions? | 82% (103) |
| What is the recommended chest compression depth? | 87% (109) |
| What is the recommended chest compression rate? | 92% (113)a |
| State the correct position of the right AED electrode | 50% (62) |
| State the correct position of the left AED electrode | 46% (58) |
| How often does an AED analyze the heart rhythm? | 86% (107)b |
Translated questions (open questions) regarding theoretical knowledge among the instructors. Data presented as percentages (n).
Data missing for 2 instructors.
Data missing for 2 instructors.
Outcome measures
The primary outcome was chest compression depth. Secondary outcomes were chest compression rate, AED electrode placement (i.e. distance from the center of the left and right AED electrode to the respective recommended positions), the fraction of correctly placed left and right AED electrodes, number of instructors who moved the manikin’s left arm when applying the left AED electrode, time-to-first shock (from the beginning of test scenario to shock delivery), correct theoretical knowledge of the recommended guidelines, and own rating of competence in BLS skills.
Further, we report chest wall recoil, hand positioning, rescue breath volume, rate of rescue breaths, and correct chest compression:ventilation ratio.
Ethics
According to the Danish Act on Research Ethics Review of Health Research Projects, Act number 593 of July 14th, 2011 section 14, no study approval was required from the Danish National Committee on Biomedical Research Ethics. Verbal and written consent was obtained from all instructors, and instructors were informed that participation was voluntary and they could withdraw their consent.
Statistics
Normally distributed data are presented as mean (standard deviation), and non-normally distributed data are presented as median (1st quartile;3rd quartile). Categorical data are presented as percentages (n). Normality was determined by histograms and Q–Q plots. A p-value <0.05 was considered significant. Data were analyzed using R-statistics (version 3.4.0, R Core Team 2017, R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 129 instructors were recruited during the period from April 1st, 2017 to March 11th, 2018. Two instructors withdrew consent and were excluded from the analysis. Further, two instructors were excluded from the analysis because they were not certified by the Danish First Aid Council or the ERC. Therefore, data from 125 instructors were analyzed. Table 1 shows the demographics of the instructors.
Table 1.
Demographics.
| Demographics | |
|---|---|
| Age (years) | 45 (30;56) |
| Gender (male) | 72% (90) |
| BMI | 26 (23;29) |
| Healthcare professionala | 38% (46)b |
| Time since initial training and certification (years) | 8 (3;14)c |
| Time since last training and re-certification (years)d, e | 2 (1;4)f |
| Number courses taught per year | 14 (6;44)c |
BMI: Body Mass Index. Data presented as median (Q1;Q3) or percentages (n).
Healthcare professional e.g. physiotherapist, nurse, doctor, emergency medical technician etc.
Data missing for 3 instructors.
Data missing for 2 instructors.
If no supplementary training and re-certification, time since initial training and certification was stated.
Recertification mandatory by the Danish First Aid Council every fifth year.
Data missing for 5 instructors.
CPR demonstration
The mean chest compression depth was 64 mm (7.3) (Fig. 1) with a mean chest compression rate of 115 min−1 (10.8). Data regarding chest wall recoil and hand positioning during CPR are presented in Table 2.
Fig. 1.
Chest compression depth per cycle.
Each dot represents one instructor’s mean chest compression depth for the respective cycle. Lines represent mean (SD). Gray area represents the recommended chest compression depth by the ERC (50−60 mm).
Table 2.
Cardiopulmonary resuscitation.
| Cardiopulmonary resuscitation | |
|---|---|
| Chest compressiona | |
| Chest compressions <50 mm | 5% |
| Chest compressions between 50−60 mm | 22% |
| Chest compressions >60 mm | 72% |
| Chest compressions with full recoil | 86% |
| Correct hand position | 98% |
| Rescue breaths | |
| Rescue breaths <500 mL | 52% |
| Rescue breaths between 500−600 mL | 11% |
| Rescue breaths >600 mL | 37% |
Data presented as percentages.
Data missing for 2 instructors.
Of all attempted rescue breaths, 94% resulted in any amount of air registered. Of these, the mean volume was 499 mL (291). Data on rescue breaths within guideline recommendations are presented in Table 2.
When performing rescue breaths, 2% of instructors (n = 3) attempted three rescue breaths per cycle instead of the recommended two rescue breaths. Furthermore, 2% of instructors (n = 2) provided rescue breaths before compressions opposite of the guideline recommendation.16
AED demonstration
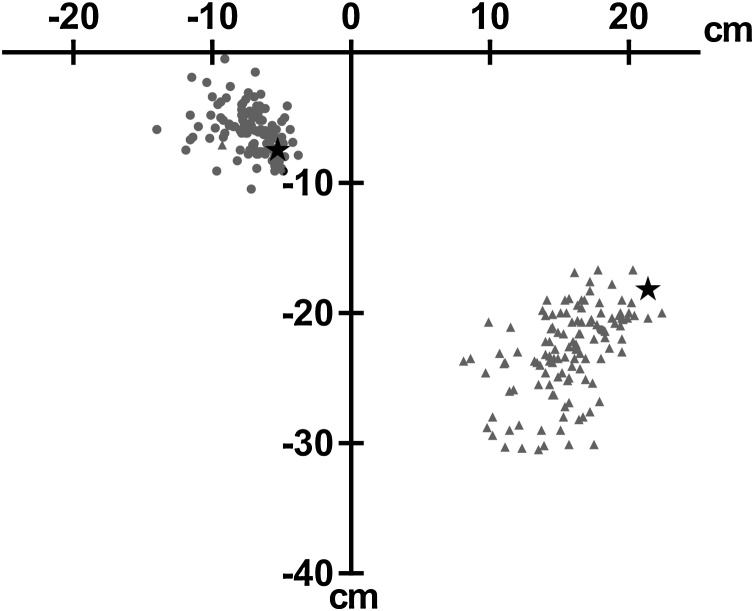
The positioning of the left and right AED-electrodes is shown in Fig. 2. The median distance from placement to the recommended position of the left AED electrode was 7.6 cm (5.0;10.5) (data missing for four instructors), whereas the median distance of the right AED electrode was 2.9 cm (1.5;4.0) (data missing for five instructors). The left AED electrode was placed within 5 cm of the recommended position by 25% (n = 30) of instructors, and the right AED electrode was placed within 5 cm of the recommended position by 85% (n = 102) of instructors. Instructors, who moved the manikin’s left arm for placement of the left AED electrode (36%, n = 42), had a median distance from the center of the left electrode to the recommended position of 4.8 cm (2.7;7.6). Instructors, who did not move the manikin’s left arm (64%, n = 75), had a median distance of 8.7 cm (6.9;11.6) (p < 0.0001) (data missing for eight instructors). The mean time-to-shock was 60 s (12). In total, 82% (n = 102) of instructors “bypassed” the voice prompt of the AED (default time duration 67 s), while 18% (n = 22) of instructors followed the voice prompt (data missing for one instructor).
Fig. 2.
AED electrode placement.
Coordinate (0,0) represents the jugular notch on the manikin. Triangles represent placement of the left AED electrode. Dots represent placement of the right AED electrode. Stars represent AED electrode position recommended by the ERC.
Theoretical knowledge
Table 3 presents the proportion of correct answers for each question in the theoretical questionnaire.
Own rating
Instructors rated their own BLS skills highly both before completing the test and after receiving a performance report. All instructors but one completed the questionnaire on rating their own skills before the test, and 58 % (n = 73) of instructors responded after receiving their performance report (Table 4).
Table 4.
Instructors own rating of their skills.
| Own ratings | ||
|---|---|---|
| Beforea | Afterb | |
| I feel confident in diagnosing a cardiac arrest | ||
| Strongly agree/agree | 98% (122) | 99% (72) |
| Neither agree nor disagree | 1% (1) | – |
| Disagree/strongly disagree | 1% (1) | 1% (1) |
| In the event of a cardiac arrest, I can provide effective chest compressions | ||
| Strongly agree/agree | 99% (123) | 97% (71) |
| Neither agree nor disagree | 1% (1) | 3% (2) |
| Disagree/strongly disagree | – | – |
| In the event of a cardiac arrest, I can provide effective rescue breathing | ||
| Strongly agree/agree | 98% (122) | 92% (67) |
| Neither agree nor disagree | 2% (2) | 7% (5) |
| Disagree/strongly disagree | – | 1% (1) |
| In the event of a cardiac arrest, I can use an AED | ||
| Strongly agree/agree | 100% (124) | 99% (72) |
| Neither agree nor disagree | – | – |
| Disagree/strongly disagree | – | 1% (1) |
Data are presented as percentages (n).
Data missing for 1 instructor (questionnaire completed before testing).
Data missing for 52 instructors (questionnaire and performance report sent per e-mail to all participants).
Subgroup analysis
We divided instructors into quartiles based on the number of courses taught per year to see if more active instructors performed better. There was no difference in chest compression depth, chest compression rate, recoil, ventilation volume, AED electrode placement, or theoretical knowledge between the groups. We also conducted a subgroup analysis based on years since the last re-certification and did not find any difference between groups.
Discussion
We found that certified BLS instructors performed chest compressions with an excessive depth when demonstrating CPR in a simulated teaching situation. During demonstrations, instructors often misplaced the left AED electrode. Also, instructors showed fundamental theoretical BLS knowledge gaps. Despite their low performance, instructors rated their own CPR/AED skills as good.
Instructors demonstrating chest compressions with an excessive depth may lead learners to copy the wrong chest compression technique. However, a previous study found that laypeople were more likely to achieve a deeper chest compression depth six months after training, if they trained with an excessive chest compression depth during BLS courses.21 In contrast to our findings, previous studies investigating chest compression depth report that BLS instructors and laypersons often perform chest compressions that are too shallow.4, 10, 22, 23, 24 Our BLS instructors were mainly male and had a median BMI of 26 kg/m2, which are two factors known to contribute to a deeper chest compression depth.25, 26 Regardless of this, instructors should be able to perform to the recommended chest compression depth. The consequences of performing chest compressions with excessive depth can be injuries on the victim, such as sternal and costal injuries.27 Importantly, these injuries were by and large not fatal. Further, an excessive chest compression depth has been associated with greater risk of rescuer fatigue.28 In our study, instructors only provided three full cycles of CPR. Therefore, it is unknown if the instructors would experience fatigue faster than rescuers providing chest compressions within the recommended range of 5−6 cm.
Only a quarter of instructors managed to place the left AED electrode as recommended. Misplaced AED electrodes may result in a lower defibrillation success and hence a lower chance of survival. An experimental porcine study found that as little as a 3 cm deviation of electrodes affects defibrillation success.29 Further, a case report describes a fatal outcome possibly due to electrode misplacement.30 Frequent misplacement of the left AED electrode was also evident in previous studies investigating AED electrode placement among trained and untrained laypeople and healthcare professionals.5, 17, 18, 19, 31 This may be due to incorrect demonstration by instructors which may result in transferal of incorrect skills to the learners. We found that instructors that moved the manikin’s left arm placed the left AED electrode closer to the recommended position. Overall, our results suggest that placement of the left AED electrode should be a focus area in the future training of BLS instructors.
Instructors in this study were tested on basic knowledge, which is essential for performing high-quality BLS. Nearly half of the certified instructors were unable to state how to diagnose a cardiac arrest. Misperceptions among certified BLS instructors may likely be passed on to their learners which ultimately may be fatal if the diagnosis of cardiac arrest is delayed or missed. Moreover, the majority of instructors lacked basic knowledge on the recommended AED electrode placement, which correlates well with the results from the skill test. This indicates that the left AED electrode’s overall poor placement in the skill test may be due to a general lack of knowledge rather than imprecise performance. Our results suggest a need for further emphasis on these topics during training, certification, and re-certification of BLS instructors in the future. Unlike the findings of the skill test when evaluating chest compression and ventilation ratio, all instructors answered the questions regarding the chest compression and ventilation ratio correctly.
Despite our findings, instructors were confident in their own skills with diagnosing a cardiac arrest, performing CPR, delivering rescue breaths, and using an AED. Even after receiving a performance report of their own results from the CPR/AED test, instructors remained confident in their own skills. This lack of self-knowledge may be an important barrier for acknowledging the need for faculty development and additional CPR/AED skill training.
From a learning perspective, any mistake during a demonstration made by an instructor should be avoided because this may lead to negative learning. Negative learning occurs when learners acquire a skill incorrectly, which can be due to, e.g. technical factors (i.e. physical settings not as in the real world), instructional, or environmental factors (i.e. artificial time factors or tasks).32, 33 An example of negative learning is the 2001 American Airlines Flight 587 crash. The crash investigation concluded that a contributing factor to the crash was a pilot error due to negative learning from the flight simulator.34 Failure in CPR training may not be equally dramatic but indeed equally severe for the person suffering from cardiac arrest, especially given the number of cardiac arrests in a year. Given the short amount of time during a BLS course to demonstrate skills and the limited time to supervise learners and give feedback during practical skill sessions, it is crucial that the demonstration is correct and the feedback is sufficient.13 In our study, instructors taught a median of 14 courses per year. With an estimated 16 participants per course (maximum number according to the Danish First Aid Council), this could potentially lead to 224 participants per instructor per year and a total of up to 28.000 participants per year for this cohort leading to a massive amount of errors passed on to laypeople attending BLS courses.
Overall, our study suggests that BLS instructors need further education on identifying a cardiac arrest as well as theoretical and practical skill training on AED electrode placement in order to avoid dissemination of negative learning. Ultimately, this may help to improve the learning outcome from BLS courses in the future.
Limitations
This study was conducted in a simulated teaching environment and may not fully reflect the demonstration that instructors would perform during an actual BLS course. Instructors may have been unfamiliar with the resuscitation manikin and AED used in the study. However, we used commonly used and commercially available equipment. Instructors should be able to adapt to the subtle differences between equipment types, but we cannot rule out that the type of equipment may have impacted performance. Instructors included in this study were recruited during volunteer meetings and courses targeting certified BLS instructors and may therefore likely represent the top tier of certified BLS instructors. The study included certified ERC instructors trained using the generic ERC’s standardized instructor course. In the current study, instructors certified by the Danish First Aid Council were also included. The instructor courses by the Danish First Aid Council are not standardized to the same degree as the ERC instructor course. This should be kept in mind when extrapolating the results to other countries where instructor certification and re-certification may differ. The direct effect of the instructors’ skill level on BLS course participants’ learning outcomes cannot be extrapolated from these results. Studies evaluating both instructors’ and learners’ skills after a BLS course are warranted to evaluate the actual implications of instructors’ skills on learning outcomes.
Conclusion
Certified BLS instructors’ have poor CPR/AED skills and several important knowledge gaps on BLS guidelines in contrast to instructors’ self-reported skills. This highlights a further need for improving BLS instructor education, including continuous faculty development to ensure optimal learning conditions for BLS course participants.
Conflict of interest
None.
CRediT authorship contribution statement
Mathilde Stærk: Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft, Writing - review & editing, Visualization, Project administration. Lauge Vammen: Methodology, Investigation, Formal analysis, Writing - review & editing, Visualization, Project administration. Camilla Fuchs Andersen: Methodology, Investigation, Writing - review & editing, Supervision. Kristian Krogh: Methodology, Formal analysis, Writing - review & editing, Supervision. Bo Løfgren: Methodology, Resources, Writing - review & editing, Supervision.
Acknowledgements
All instructors are thanked for their participation in the study. We thank the Association of Independent First Aid Instructors, Denmark (Foreningen af Selvstændige Førstehjælpsinstruktører, FSFI), Nordic First Aid, and Laerdal for allowing us to collect data during their events. We are thankful to Camilla Bang, Ditte Kamille Rasmussen, Josephine Johnsen, Julie Lyngholm Madsen, Louise Nørkjær, Martin Oskar Broe, Martin Thomsen, and Søren Rahbek for their contribution during data collection. We thank Research Center for Emergency Medicine, Aarhus University Hospital for providing funding for the study.
References
- 1.Wissenberg M., Lippert F.K., Folke F. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 2.Talikowska M., Tohira H., Finn J. Cardiopulmonary resuscitation quality and patient survival outcome in cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2015;96:66–77. doi: 10.1016/j.resuscitation.2015.07.036. [DOI] [PubMed] [Google Scholar]
- 3.Blom M.T., Beesems S.G., Homma P.C. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130:1868–1875. doi: 10.1161/CIRCULATIONAHA.114.010905. [DOI] [PubMed] [Google Scholar]
- 4.Boet S., Bould M.D., Pigford A.-A. Retention of basic life support in laypeople: mastery learning vs. time-based education. Prehosp Emergency Care. 2017;21:362–377. doi: 10.1080/10903127.2016.1258096. [DOI] [PubMed] [Google Scholar]
- 5.Staerk M., Bodtker H., Lauridsen K.G., Lofgren B. Automated external defibrillation training on the left or the right side — a randomized simulation study. Open Access Emerg Med. 2017;9:73–79. doi: 10.2147/OAEM.S140220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bang C., Cordsen A.-S.N., Hoe M.B. Abstract 20087: the inflatable mini Anne® manikin may be used as an inexpensive alternative to a standard life-size resuscitation manikin during instructor-led BLS/AED training — a randomized controlled study. Circulation. 2017;136 [Google Scholar]
- 7.Hansen C., Bang C., Rasmussen S.E. Basic life support training: demonstration versus lecture — a randomised controlled trial. Am J Emerg Med. 2019;38(4):720–726. doi: 10.1016/j.ajem.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Reder S., Cummings P., Quan L. Comparison of three instructional methods for teaching cardiopulmonary resuscitation and use of an automatic external defibrillator to high school students. Resuscitation. 2006;69:443–453. doi: 10.1016/j.resuscitation.2005.08.020. [DOI] [PubMed] [Google Scholar]
- 9.de Vries W., Handley A.J. A web-based micro-simulation program for self-learning BLS skills and the use of an AED. Can laypeople train themselves without a manikin? Resuscitation. 2007;75:491–498. doi: 10.1016/j.resuscitation.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Bjornshave K., Krogh L.Q., Hansen S.B., Nebsbjerg M.A., Thim T., Lofgren B. Teaching basic life support with an automated external defibrillator using the two-stage or the four-stage teaching technique. Eur J Emerg Med. 2016;25(1):18–24. doi: 10.1097/MEJ.0000000000000410. [DOI] [PubMed] [Google Scholar]
- 11.Kaye W., Rallis S.F., Mancini M.E. The problem of poor retention of cardiopulmonary resuscitation skills may lie with the instructor, not the learner or the curriculum. Resuscitation. 1991;21:67–87. doi: 10.1016/0300-9572(91)90080-i. [DOI] [PubMed] [Google Scholar]
- 12.Wagner P., Lingemann C., Arntz H.R., Breckwoldt J. Official lay basic life support courses in Germany: is delivered content up to date with the guidelines? An observational study. Emerg Med J. 2015;32:547–552. doi: 10.1136/emermed-2014-203736. [DOI] [PubMed] [Google Scholar]
- 13.Parnell M.M., Larsen P.D. Poor quality teaching in lay person CPR courses. Resuscitation. 2007;73:271–278. doi: 10.1016/j.resuscitation.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Wynne G., Marteau T., Evans T.R. Instructors—a weak link in resuscitation training. J R Coll Physicians Lond. 1992;26:372–373. [PMC free article] [PubMed] [Google Scholar]
- 15.Breckwoldt J., Lingemann C., Wagner P. [Resuscitation training for lay persons in first aid courses: transfer of knowledge, skills and attitude] Anaesthesist. 2016;65 doi: 10.1007/s00101-015-0113-8. p. 22–26, 28-29. [DOI] [PubMed] [Google Scholar]
- 16.Perkins G.D., Handley A.J., Koster R.W. European Resuscitation Council Guidelines for Resuscitation 2015: section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. doi: 10.1016/j.resuscitation.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 17.Nurmi J., Castren M. Layperson positioning of defibrillation electrodes guided by pictorial instructions. Resuscitation. 2005;64:177–180. doi: 10.1016/j.resuscitation.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 18.Nurmi J., Rosenberg P., Castren M. Adherence to guidelines when positioning the defibrillation electrodes. Resuscitation. 2004;61:143–147. doi: 10.1016/j.resuscitation.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 19.Heames R.M., Sado D., Deakin C.D. Do doctors position defibrillation paddles correctly? Observational study. BMJ. 2001;322:1393–1394. doi: 10.1136/bmj.322.7299.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soar J., Nolan J.P., Bottiger B.W. European Resuscitation Council Guidelines for Resuscitation 2015: section 3. Adult advanced life support. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 21.Mpotos N., Lemoyne S., Wyler B. Training to deeper compression depth reduces shallow compressions after six months in a manikin model. Resuscitation. 2011;82:1323–1327. doi: 10.1016/j.resuscitation.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 22.Isbye D.L., Rasmussen L.S., Lippert F.K., Rudolph S.F., Ringsted C.V. Laypersons may learn basic life support in 24min using a personal resuscitation manikin. Resuscitation. 2006;69:435–442. doi: 10.1016/j.resuscitation.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 23.Al-Rasheed R.S., Devine J., Dunbar-Viveiros J.A. Simulation intervention with manikin-based objective metrics improves CPR instructor chest compression performance skills without improvement in chest compression assessment skills. Simul Healthc. 2013;8:242–252. doi: 10.1097/SIH.0b013e31828e716d. [DOI] [PubMed] [Google Scholar]
- 24.Stiell I.G., Brown S.P., Nichol G. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130:1962–1970. doi: 10.1161/CIRCULATIONAHA.114.008671. [DOI] [PubMed] [Google Scholar]
- 25.Oh J.H., Kim C.W. Relationship between chest compression depth and novice rescuer body weight during cardiopulmonary resuscitation. Am J Emerg Med. 2016;34:2411–2413. doi: 10.1016/j.ajem.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Hansen C., Bang C., Staerk M., Krogh K., Lofgren B. Certified basic life support instructors identify improper cardiopulmonary resuscitation skills poorly: instructor assessments versus resuscitation manikin data. Simul Healthc. 2019;14(5):281–286. doi: 10.1097/SIH.0000000000000386. [DOI] [PubMed] [Google Scholar]
- 27.Hellevuo H., Sainio M., Nevalainen R. Deeper chest compression — more complications for cardiac arrest patients? Resuscitation. 2013;84:760–765. doi: 10.1016/j.resuscitation.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 28.McDonald C.H., Heggie J., Jones C.M., Thorne C.J., Hulme J. Rescuer fatigue under the 2010 ERC guidelines, and its effect on cardiopulmonary resuscitation (CPR) performance. Emerg Med J. 2013;30:623–627. doi: 10.1136/emermed-2012-201610. [DOI] [PubMed] [Google Scholar]
- 29.Esibov A., Chapman F.W., Melnick S.B., Sullivan J.L., Walcott G.P. Minor variations in electrode pad placement impact defibrillation success. Prehosp Emerg Care. 2016;20:292–298. doi: 10.3109/10903127.2015.1076095. [DOI] [PubMed] [Google Scholar]
- 30.Goksu T., Borggrefe M., Haghi D. Inappropriate placement of defibrillator self-adhesive electrode pads with possible fatal outcome. Emerg Med J. 2011;28:158. doi: 10.1136/emj.2009.082198. [DOI] [PubMed] [Google Scholar]
- 31.Bødtker H., Stærk M., Lauridsen K.G., Jæger A., Løfgren B. Abstract 19549: automated external defibrillation: not that easy! untrained laypeople place AED pads poorly. Circulation. 2015;132 [Google Scholar]
- 32.Bond W.F., Lammers R.L., Spillane L.L. The use of simulation in emergency medicine: a research agenda. Acad Emerg Med. 2007;14:353–363. doi: 10.1197/j.aem.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 33.Krogh K.B., Hoyer C.B., Ostergaard D., Eika B. Time matters—realism in resuscitation training. Resuscitation. 2014;85:1093–1098. doi: 10.1016/j.resuscitation.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 34.In-Flight Separation of Vertical Stabilizer, American Airlines Flight 587. Airbus Industrie A300-605R, N14053, Belle Harbor, New York, November 12, 2001, in Aircraft Accident Report NTSB/AAR-04/04. 2004, National Transportation Safety Board: Washington D.C.