Graphical abstract
Abbreviations: EMS, emergency medical services; OHCA, out of hospital cardiac arrest; IHCA, in hospital cardiac arrest; CPR, cardiopulmonary resuscitation; AHA, American Heart Association; ROSC, return of spontaneous circulation; HA, hospital admission; HD, discharged alive from the hospital; ETT, endotracheal intubation; NRM, non-rebreather mask; BVM, bag-valve mask; PEA, pulseless electrical activity; AED, automated external defibrillator
Keywords: Pediatric cardiac arrest, Resuscitation, CPR
Abstract
Objective
To determine which aspects of prehospital care impact outcomes after pediatric cardiac arrest.
Methods
In this study, the authors examine 5 years of consecutive data from their county emergency medical system (EMS), to identify predictors of good outcome after pediatric cardiac arrest, including return of spontaneous circulation (ROSC), survival to hospital admission (HA) and survival to hospital discharge (HD). Three logistic regression models were performed using JMP 14.1 Pro for Windows, each with the following nine predictors: age, sex, ventilation method (endotracheal intubation vs. supraglottic airway), initial rhythm (pulseless electrical activity vs. asystole), epinephrine administration, bystander treatment prior to EMS arrival, time from collapse to EMS arrival, automatic external defibrillator (AED) placement, and whether the arrest was witnessed. Odds ratio confidence intervals were calculated using the Wald method, and corresponding p-values were obtained with the likelihood ratio χ2 test.
Results
From January 1, 2012 to December 31, 2016, there were 133 pediatric cardiac arrests, of which we had complete data on 109 patients for pediatric cardiac arrest. The median age was 8 months, with an IQR of 2.25–24 months, and a range of 0–108 months (0–9 years). There was return of spontaneous circulation (ROSC) in 20% of cases overall, with 16% making it to hospital admission, and 9% making it alive out of the hospital.
The median time to EMS arrival for witnessed events was 10 min, with an interquartile range (IQR) of 6.5−16 min, and a range of 0−25 min. The median time to EMS arrival for unwitnessed events was 30 min, with an IQR of 19–62.5 min, and a range of 9−490 min.
Predictors of ROSC included epinephrine administration (p = .00007), bystander treatment before EMS arrival (p = .0018), older age (p = .0025), shorter time to EMS arrival (p = .0048), and AED placement. Predictors of hospital admission included epinephrine NOT being administered (p = .0004), bystander treatment before EMS arrival (p = .0088), shorter time to EMS arrival (p = .0141), and AED placement (p = .0062). The only significant predictor of survival to hospital discharge alive that was identified was shorter time to EMS arrival (p = .0014), as there was insufficient data for many of the predictor variables in this analysis.
Conclusion
Shorter time to EMS arrival from time of arrest, any bystander treatment prior to EMS arrival, and AED placement resulted in significantly higher rates of return of spontaneous circulation. Epinephrine administration significantly improved ROSC, but had the opposite effect on HA. Only shorter time to EMS arrival from time of arrest was significantly associated with survival to hospital discharge. Each additional minute for the EMS to arrive resulted in 5% decreased odds of ROSC and hospital admission, and 12% decreased odds of surviving to hospital discharge.
Introduction
Pediatric cardiac arrest is one of the most frightening and challenging calls facing emergency medical services (EMS) personnel.
Pediatric out of hospital cardiac arrest (POHCA) in children has an incidence rate between 3 and 9 per 100,000/year.1 The survival to discharge from POHCA is 3% for infants and 9% for children.2 Sadly, these numbers have not changed substantially in the past 20 years.
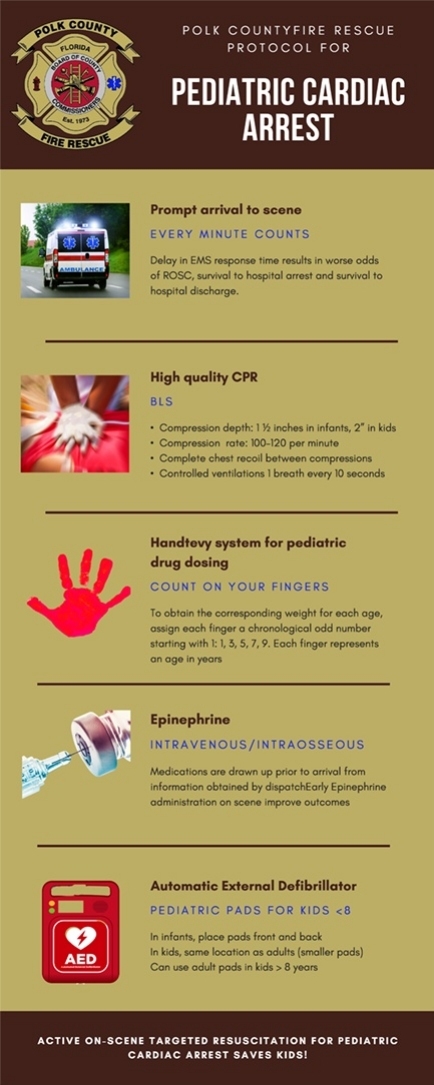
Some of the challenges with pediatric cardiac arrest include lack of high-quality CPR, protocols that prevent paramedics from performing pediatric intubation, and general lack of ongoing training. Another major challenge during pediatric resuscitation is the correct dosing of medication. One study demonstrated a medication dosing error rate of 34% among 5547 pediatric patients treated in the out of hospital setting.3 Visual estimation of pediatric weight, by parents, nurses and physicians, has been shown to be unreliable.4 Thus, the AHA recommends a weight-based system with pre-calculated doses in cases where the weight is unknown.5 In 2010, the American Heart Association (AHA) also changed the sequence of pediatric resuscitation for children in cardiac arrest from "A-B-C" i.e. Airway, Breathing, and Chest Compression to "C-A-B" i.e. Chest Compressions first, so that circulation is not arrested while performing breathing.
Polk County Fire Rescue (PCFR), our county EMS system, recognized the challenges with POHCA and was an early adopter of the above AHA guidelines. We placed an emphasis on active on-scene management of pediatric cardiac arrest, training of personnel on high quality CPR and implemented a weight-based medication dosing system in an effort to improve these dismal survival rates. We published our successful experience with the implementation of this protocol6 that focused on consistent attention to quality, feedback, and focused on-scene management which resulted in a steady improvement in survival after pediatric cardiac arrest.
In this paper, we report on an additional year of data and examine the effect of time from collapse to EMS arrival on each of the following outcomes: return of spontaneous circulation in the field (ROSC), survival to hospital admission (HA) and survival to hospital discharge (HD)
Methods
Study design
This was a prospective observational study conducted as part of our county EMS system’s quality and research program. Our IRB approved prehospital research registry uses a comprehensive Utstein-style database and record-keeping system that prospectively identifies and collects relevant data for all POHCA cases. This study is an expanded analysis of previously published subset of cases.6
Study setting and population
Polk County Fire Rescue is one of the largest EMS systems in our state, responding to more than 115,000 calls per year, and covering a geographic footprint of over 2010 square miles. All patients under the age of 18 for whom a call was made for unresponsiveness were included in the dataset. Patients who were identified as having sinus tachycardia (i.e., not cardiac arrest) were later excluded from the database.
Measures
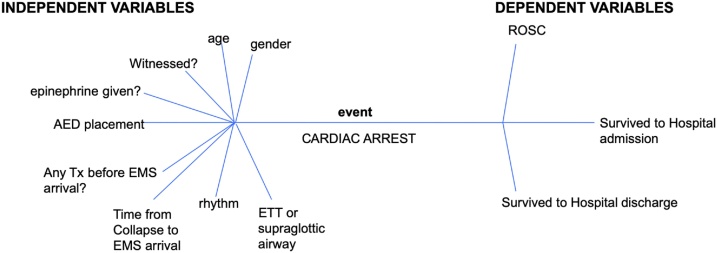
Our pediatric cardiac arrest registry incorporated the following variables collected at the scene: age, time of arrest, interventions performed on scene, and ROSC. These were collected in real time. ROSC was defined as resumption of sustained cardiac activity by means of a palpable pulse or equivalent for at least 30 s. Data on survival to hospital admission and hospital discharge were collected by our dedicated research officer within 30 days of the event via data capture at our mandatory quality meetings with each receiving facility. The independent and dependent variables are summarized in Fig. 1
Fig. 1.
Variables collected and analyzed in pediatric cardiac arrest dataset.
Data analysis
All variables were stored in a secure database system. Statistical analyses were performed in JMP 14.1 Pro for Windows (SAS institute, Cary, NC). Descriptive analyses were done for baseline characteristics, using nonparametric methods for non-normally distributed variables. Three multiple nominal logistic regression analyses were performed in order to determine predictive factors for ROSC, hospital admission (HA), and being discharged alive from the hospital (HD). In each of these models, the 9 predictors evaluated were age, sex, ventilation method (endotracheal intubation [ETT] or supraglottic airway [i-Gel] vs. non rebreather mask [NRM] or bag-valve-mask [BVM]), initial rhythm (pulseless electrical activity [PEA] vs. asystole), epinephrine administration, bystander treatment prior to EMS arrival, time from collapse to EMS arrival, automatic external defibrillator (AED) placement, and whether the arrest was witnessed. The time from collapse to EMS arrival was further stratified into witnessed versus unwitnessed events, since estimating the time of collapse in an unwitnessed arrest is exceedingly difficult.7
Odds ratios were calculated for each predictor, with a Wald confidence interval for the odds ratio and p-values based on the likelihood ratio χ2 test.
We opted to calculate odds ratios, rather than relative risk, for our regression analyses because it enables the computation of a unit odds ratio; that is, for every unit change in our predictor, the odds of a certain outcome change by a constant factor. As two of our predictive factors (age and time from collapse to EMS arrival) are continuous, this gives us greater insight into the effect of, for example, having EMS arrive one minute later. Our logistic regression analyses were run on 109 patients for ROSC and hospital admission, and 108 patients for hospital discharge. This is the subset of our cohort for which we had data on all 9 predictor variables as well as the respective outcome variable.
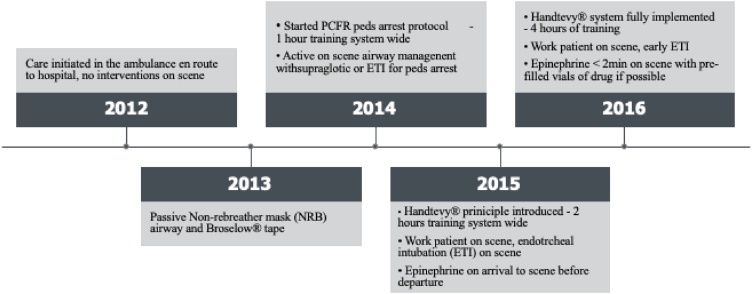
Data are presented overall across the 5 years of study to date (January 1, 2012 to December 31, 2016). As reported previously, beginning in 2014, a deliberate change in protocol was made where our paramedics provided targeted resuscitation at the scene, instead of immediate transport (Fig. 2). On scene interventions included active chest compressions and airway management. Prior to 2014, our paramedics could not intubate per protocol. In 2015, the Handtevy system8 for pediatric drug dosing was implemented to increase comfort with pediatric resuscitation drugs.
Fig. 2.
Timeline of interventions.
Results
There were 133 calls received for pediatric cardiac arrest during the study period. 17 patients were excluded from the study as they were found by EMS to have sinus tachycardia, making our study population 116, Of these 116, 7 did not have outcome data so the final cohort was 109. Our cohort was 64% female. The median age was 8 months, with an IQR of 2.25–24 months, and a range of 0–108 months (9 years). The causes of arrest were drowning (34%); respiratory (50%); trauma (9%); seizure (3%) cardiac/medical (2%); and choking (2%). Forty-eight % received treatment by a bystander prior to EMS arrival. The initial rhythm upon EMS arrival was 84% asystole and 16% PEA.
In terms of on scene management, 58% were ventilated with a bag valve mask (BVM). Forty percent of children were ventilated by an ETT or from 2014 with an ETT or a supraglottic airway. The frequency of each intervention by year is summarized in Table 1.
Table 1.
| Year | # arrests | age in months (median) | % female gender | % witnessed arrests | %who received drugs (epinephrine) | % with any treatment before EMSa arrival | % who had AED placed | mean #minutes from collapse to EMS arrival | % who got ETTc or igel (2014 onwards) or king tube (prior to 2014) | %who got BVM | %each rhythm upon EMS arrival |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 20 | 4 | 35 | 20 | 80 | 40 | 35 | 27 | 30 | 70 | 90% asystole; 10% PEA |
| 2013 | 17 | 6 | 35 | 6 | 94 | 47 | 35 | 40 | 41 | 59 | 64% asystole; 6% PEA |
| 2014 | 17 | 4 | 35 | 18 | 82 | 53 | 71 | 31 | 24 | 76 | 82% asystole; 18% PEA |
| 2015 | 35 | 16 | 46 | 100 | 71 | 51 | 66 | 26 | 34 | 66 | 77% asystole; 23% PEA |
| 2016 | 27 | 12 | 26 | 19 | 96 | 48 | 52 | 28 | 81 | 19 | 85% asystole; 15% PEA |
AED = automatic external defibrillator.
BVM = bag valve mask.
EMS = emergency medical services.
ETT = endotracheal intubation.
PEA = pulseless electrical activity.
There was ROSC in 20% of cases overall, with 16% surviving to hospital admission (HA), and 9% surviving to hospital discharge (HD). In 95% of cases, the arrest was determined by a bystander, rather than EMS. The interquartile range (IQR) for time to EMS arrival was 19–62.5 min, with a range of 5−490 min. For witnessed arrests, the range was 0−25 min, median 10 min, and IQR 6.5−16 min. For unwitnessed arrests, the range was 9−490 min, median 30 min, and IQR 19–62.5 minutes.
As shown in Table 2, Table 3, Table 4, each additional minute for the EMS to arrive resulted in 5% decreased odds of ROSC and hospital admission, and 12% decreased odds of surviving to hospital discharge. Specifically, looking at the row “minutes from collapse to vehicle stopped” in Table 2, Table 3 yields an odds ratio (OR) of 0.952 and 0.954 for the outcomes of ROSC and survival to hospital arrival (HA) respectively. This translates to an approximately 5 percent decreased odds of these outcomes for every 1 min longer delay or time from collapse to vehicle stopped (because the odds are per minute odds). Similarly, in Table 4, the OR for “minutes from collapse to vehicle stopped” is 0.881, which would translate to a 12 percent decreased odds of survival to hospital discharge.
Table 2.
| Odds Ratio (95% CI) | p-value | |
|---|---|---|
| Epinephrine administration | 75.19 (6.115−924.5) | .00007 |
| Bystander treatment before EMS arrival | 12.70 (2.024−79.65) | .0018 |
| Age in months | 1.051 (1.016−1.094) | .0025 |
| Minutes from collapse to vehicle stopped | 0.952 (0.−863 to 0.993) | .0048 |
| AED placement | 9.389 (1.419−62.12) | .0073 |
| Female sex | 0.274 (0.052−1.459) | NS |
| ETT or I-gel ventilation | 2.778 (0.485−15.89) | NS |
| Witnessed arrest | 0.514 (0.040−6.654) | NS |
| Initial rhythm of PEA, rather than asystole | 0.928 (0.139−6.176) | NS |
AED = automatic external defibrillator.
EMS = emergency medical services.
ETT = endotracheal intubation.
NS = not significant.
PEA = pulseless electrical activity.
ROSC = return of spontaneous circulation.
Table 3.
Predictors of Hospital admission (HA) Factor [n = 109].a.
| Odds Ratio (95% CI) | p-value | |
|---|---|---|
| Epinephrine administration | 0.022 (0.002−0.245) | .0004 |
| Bystander treatment before EMS arrival | 7.759 (1.407−42.79) | .0088 |
| Age in months | 1.023 (0.994−1.058) | NS |
| Minutes from collapse to vehicle stopped | 0.954 (0.866−0.996) | .0141 |
| AED placement | 10.19 (1.408−73.71) | .0062 |
| Female sex | 0.677 (0.153−3.001) | NS |
| ETT or I-gel ventilation | 2.635 (0.518−13.41) | NS |
| Witnessed arrest | 0.878 (0.081−9.533) | NS |
| Initial rhythm of PEA, rather than asystole | 1.107 (0.177−6.907) | NS |
NS = not significant.
Table 4.
| Odds Ratio (95% CI) | p-value | |
|---|---|---|
| Epinephrine administration | Unstable | N/A |
| Bystander treatment before EMS arrival | Unstable | N/A |
| Age in months | 1.000 (0.927−1.079) | NS |
| Minutes from collapse to vehicle stopped | 0.881 (0.687−0.977) | .0014 |
| AED placement | Unstable | N/A |
| Female sex | 0.274 (0.004−17.40) | NS |
| ETT or I-gel ventilation | 0.311 (0.008−12.40) | NS |
| Witnessed arrest | Unstable | N/A |
| Initial rhythm of PEA, rather than asystole | Unstable | N/A |
N/A = not applicable.
NS = not significant.
For cells marked “Unstable” or “N/A”, there was insufficient data to calculate the Wald confidence interval or perform the likelihood ratio test. ROSC and survival to hospital admission jumped significantly (from 0 to 26%, p < 0.0001) upon implementation of the protocol that emphasized targeted on scene intervention rather than immediate transport.
Discussion
In this Polk County Fire Rescue pediatric out of hospital cardiopulmonary arrest prospective observational study that included 109 pediatric cardiopulmonary arrests, we found that shorter time from arrest to EMS arrival, and any treatment prior to EMS arrival (including bystander CPR, or placement of an AED) resulted in significantly higher rates of return of spontaneous circulation. ROSC was achieved in 20% of the cases, along with 16% of cases with survival to hospital admission and 9% of cases survived to hospital discharge.
A deliberate revision of POHCA protocols was instituted in 2014, including a system that simplified the medication dosing administration by using an age-based method for pediatric arrests. In addition, PCFR personnel were trained to change their focus from the traditional scoop-and-run model that existed to active on-scene resuscitation. With on scene resuscitation, the time to life-saving interventions such as obtaining peripheral access and administering medications was reduced. Other PCFR revisions to POHCA protocol included paramedics being trained to use Intraosseous (IO) over Intravenous (IV) access to reduce time to medication administration and initiation of chest compressions. Delays or diminished quality CPR while obtaining intravenous access were avoided. A study in Japan found that pre-hospital IV access attempts in out of hospital cardiac arrest was negatively associated with 30-day survival.9 The authors theorized that the quality of compressions to adequate depth may be hindered during IV access attempts. Paramedics are trained to preferentially place IO access if not rapidly able to get IV access. This minimizes interruptions in CPR during difficult venous access.
Our finding of initial cardiac rhythm affecting ROSC is similar to prior studies. For example, a study in Taiwan, found that patients with ventricular fibrillation (VF) were more than three times as likely to survive to discharge than those with a non-VF rhythm.10 Although shockable rhythms are rare in pediatric cardiac arrest, on scene resuscitation allows for earlier defibrillation in pulseless ventricular tachycardia or ventricular fibrillation. The earlier the shock is delivered, the more likelihood of obtaining ROSC. This leads to a decreased duration of a no flow state and improved outcomes in ROSC.
Spending adequate time on scene allows EMS personnel to deliver lifesaving interventions. One study found that the on-scene time of 10−35 min was associated with improved survival compared to on scene time of <10 min. The study also found that on scene time >35 min was associated with worse outcomes.11 Contrary to the findings of the current study, this study found that attempts at advanced airways were not associated improved outcomes. The authors theorized that attempts at intubation in the field may have led to interruptions/cessation of CPR and possible harmful hyperventilation.
Multiple studies have shown the duration of out of hospital cardiac arrest is inversely related to 30-day mortality and favorable neurological outcomes. One study found the duration of EMS initiated CPR beyond which the 30-day favorable outcomes decreased to less than 1% was 42 min.11 The current study supports the findings of these prior studies. In the current study, the overall interquartile range for time to arrival was 19–62.5 min with a range of 9−490 min. A shorter time from arrest to EMS arrival, was significantly associated with ROSC, HA, and HD. A large multicenter cluster randomized study of 11,368 adults with cardiac arrest found that 90% of patients with favorable neurological outcome had achieved ROSC in 20 min.12 Data for out of hospital pediatric cardiac arrest CPR duration is limited.
The current study found that bystander CPR and any treatment prior to EMS arrival was associated with improved ROSC, and HA. These findings are in support of the current literature. A systematic review of pediatric cardiac arrest in schools found that survival rate ranged from 31 to 71%.13 The authors attributed improved survival in school setting to early bystander CPR and defibrillation. Cardiac arrests occurring in schools are more likely to be witnessed and have increased access to defibrillators. The most common causes of out of hospital pediatric cardiac arrests are respiratory, trauma and Sudden Unexpected Infant Death Syndrome14 Prompt recognition and early CPR are crucial factors in the chain of survival in out of hospital pediatric cardiac arrest.
Limitations
The current study has important limitations, namely the possible misdiagnosis of cardiac arrest by bystanders by bystanders who actually had cardiac output, which could favorably skew the return of spontaneous circulation. Thus, it is possible that the results may not be extrapolatable to other populations. However, this was mitigated by performing statistical analyses on only the population that was pulseless at EMS arrival. Further, the sample size of this cohort precludes a multiple regression model adjusting for all confounders and allowing full assessment of the likely relationship between EMS changes in care and outcomes for children in cardiac arrest. The low number of patients who survived to hospital discharge did not allow us to conduct meaningful analysis for several of the predictors, where the rows marked “Unstable” in Table 3 indicate that the Wald confidence interval is (0, ∞) due to too few observations.
Future directions
A 30-day survival endpoint would be a useful outcome to look at as sometimes the survival to hospital discharge (which may be just a few days after the cardiac arrest)may not tell the whole story. In terms of predictors variables, it would be interesting to study whether there is a difference in outcome between ETT and SGA. In this paper, the data for ETT and SGA was collected as a single variable “advanced airway.” There is ingoing debate whether an advanced airway impacts outcome, and also which type. As we maintain an ongoing prospective POCHA registry, we plan to incorporate these two data points into future iterations of our work.
Conclusion
Shorter time to EMS arrival from time of arrest, and any bystander treatment prior to EMS arrival, administration of epinephrine and automatic external defibrillator (AED) placement resulted in significantly higher rates of return of spontaneous circulation, and survival to hospital admission. Younger age also resulted in significantly higher ROSC. Only Shorter time to EMS arrival from time of arrest was significantly associated with survival to hospital discharge. Each additional minute for the EMS to arrive resulted in 5% decreased odds of ROSC and hospital admission, and 12% decreased odds of surviving to hospital discharge.
Our study underscores the importance of prompt EMS dispatch and arrival and active on scene intervention by EMS.
Disclaimer
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
CRediT authorship contribution statement
Paul Banerjee: Conceptualization, Resources, Investigation, Writing - review & editing, Supervision, Project administration. Latha Ganti : Conceptualization, Methodology, Software, Validation, Formal analysis, Writing - original draft, Writing - review & editing, Visualization. Tej G. Stead: Methodology, Software, Validation, Formal analysis, Writing - original draft, Writing - review & editing. Ariel E. Vera: Writing - review & editing. Raf Vittone: Project administration, Writing - review & editing. Paul E. Pepe: Writing - review & editing.
Contributor Information
Paul Banerjee, Email: paulbanerjee@polk-county.net.
Latha Ganti, Email: latha.ganti@ucf.edu.
Tej G. Stead, Email: Tej@Brown.edu.
Ariel E. Vera, Email: arieleveramd@outlook.com.
Raf Vittone, Email: rafvittone@polk-county.net.
Paul E. Pepe, Email: Paul.Pepe@UTSW.edu.
References
- 1.Atkins D.L., Everson-Stewart S., Sears G.K. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nadkarni V.M., Larkin G.L., Peberdy M.A. National Registry of Cardiopulmonary Resuscitation Investigators. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295(January (1)):50–57. doi: 10.1001/jama.295.1.50. PMID: 16391216. [DOI] [PubMed] [Google Scholar]
- 3.Harris M., Patterson J., Morse J. Doctors, nurses, and parents are equally poor at estimating pediatric weights. Pediatric Emergency Care. 1999;15(1):17–18. doi: 10.1097/00006565-199902000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Kleinman Monica E., Chameides Leon, Schexnayder Stephen M. 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S876–S908. doi: 10.1161/CIRCULATIONAHA.110.971101. [DOI] [PubMed] [Google Scholar]
- 5.Young K.D., Seidel J.S. Pediatric cardiopulmonary resuscitation: a collective review. Ann Emerg Med. 1999;33:195–205. doi: 10.1016/s0196-0644(99)70394-x. [DOI] [PubMed] [Google Scholar]
- 6.Banerjee P.R., Ganti L., Pepe P.E., Singh A., Roka A., Vittone R.A. Early On-Scene Management of Pediatric Out-of-Hospital Cardiac Arrest Can Result in Improved Chances for Neurologically-Intact Survival. Resuscitation. 2018;S0300–9572(18):31080–31083. doi: 10.1016/j.resuscitation.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Perkins G.D., Jacobs I.G., Nadkarni V.M. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132(13):1286–1300. doi: 10.1161/CIR.0000000000000144. Epub 2014 Nov 11. Erratum in: Circulation. 2015 Sep 29;132(13):e168-9. PMID: 25391522. [DOI] [PubMed] [Google Scholar]
- 8.Antevy P. First-hand approach. A novel method to rapidly calculate pediatric drug dosages. JEMS. 2013;38(8):32–35. [PubMed] [Google Scholar]
- 9.Hansen Matthew, Schmicker Robert H., Newgard Craig D. Time to Epinephrine Administration and Survival from Non-Shockable Out-of-Hospital Cardiac Arrest Among Children and Adults. Circulation. 2018 doi: 10.1161/CIRCULATIONAHA.117.033067. March 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai C.Y., Lin F.H., Chu H., Ku C.H., Tsai S.H. Survival factors of hospitalized out-of-hospital cardiac arrest patients in Taiwan: A retrospective study. PLoS One. 2018;13(1):e0191954. doi: 10.1371/journal.pone.0191954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goto Yoshikazu, Funada Akira, Goto Yumiko. Duration of Prehospital Cardiopulmonary Resuscitation and Favorable Neurological Outcomes for Pediatric Out-of-Hospital Cardiac Arrests. Circulation. 2016;134 doi: 10.1161/CIRCULATIONAHA.116.023821. no. 25 (December 20, 2016): 2046. [DOI] [PubMed] [Google Scholar]
- 12.Reynolds Joshua C., Grunau Brian E., Rittenberger Jon C., Sawyer Kelly N., Kurz Michael C., Callaway Clifton W. Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest. Circulation. 2016;134 doi: 10.1161/CIRCULATIONAHA.116.023309. no. 25 (December 20, 2016): 2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith, Christopher Matthew, Michael C. Colquhoun. Out-of-hospital cardiac arrest in schools: a systematic review. Resuscitation 96 (n.d.): 296–302. 10.1016/j.resuscitation.2015.08.021. [DOI] [PubMed]
- 14.Gerein R.B., Osmond M.H., Stiell I.G., Nesbitt L.P., Burns S. What are the etiology and epidemiology of out-of-hospital pediatric cardiopulmonary arrest in Ontario, Canada? Acad Emerg Med. 2006;13:653–658. doi: 10.1197/j.aem.2005.12.025. [DOI] [PubMed] [Google Scholar]