Highlights
-
•
A proportion of out of hospital cardiac arrests are associated with poor prognoses.
-
•
Prolonged resuscitation on medically futile cases results in financial burden for the health system and distress for health care workers.
-
•
‘Termination of Resuscitation’ protocols enable ceasing resuscitation efforts for certain cases.
-
•
Successfully adopting a protocol over existing practices demonstrates fewer cases transported to hospital, fewer emergency treatments and fewer inpatient bed days used.
-
•
The protocol can lead to reduced costs and fewer non-beneficial hospital admissions.
Keywords: Out-of-hospital cardiac arrest, Termination of Resuscitation, Emergency medical services, Markov model
Abstract
Background
Out-of-hospital cardiac arrests with negligible chance of survival are routinely transported to hospital and many are pronounced dead thereafter. This leads to some potentially avoidable costs. The ‘Termination of Resuscitation’ protocol allows paramedics to terminate resuscitation efforts onsite for medically futile cases. This study estimates the changes in frequency of costly events that might occur when the protocol is applied to out-of-hospital cardiac arrests, as compared to existing practice.
Methods
We used Singapore data from the Pan-Asian Resuscitation Outcomes Study, from 1 Jan 2014 to 31 Dec 2017. A Markov model was developed to summarise the events that would occur in two scenarios, existing practice and the implementation of a Termination of Resuscitation protocol. The model was evaluated for 10,000 hypothetical patients with a cycle duration of 30 days after having a cardiac arrest. Probabilistic sensitivity analysis accounted for uncertainties in the outcomes: number of urgent transports and emergency treatments, inpatient bed days, and total number of deaths.
Results
For every 10,000 patients, existing practice resulted in 1118 (95% Uncertainty Interval 1117 to 1119) additional urgent transports to hospital and subsequent emergency treatments. There were 93 (95% Uncertainty Interval 66 to 120) extra inpatient bed days used, and 3 fewer deaths (95% Uncertainty Interval 2 to 4) in comparison to using the protocol.
Conclusion
The findings provide some evidence for adopting the Termination of Resuscitation protocol. This policy could lead to a reduction in costs and non-beneficial hospital admissions, however there may be a small increase in the number of avoidable deaths.
Introduction
Traditionally it has been mandatory for out-of-hospital cardiac arrest (OHCA) cases, regardless of risks of medical futility, to be resuscitated and transported to hospital. Only there can an emergency physician terminate resuscitation and pronounce death. Sudden cardiac arrests have been associated with poor prognosis1 with overall survival to hospital discharge rates as low as 10% in the United States and Europe,2, 3 between 0.5% and 8.5% in the Asia-Pacific region4 and approximately 3% in Singapore.5 Medically futile resuscitations have stimulated the development of Termination of Resuscitation (TOR) protocols for emergency medical services (EMS). Basic and advanced life support TOR protocols have been established by the American Heart Association.6 The basic life support TOR rule recommends transportation in case of any spontaneous return of circulation, if a shock was delivered or if the arrest was witnessed by EMS personnel. The advanced life support TOR rule has additional criteria where transportation is recommended if the arrest was witnessed by a bystander or EMS personnel and/or if bystander CPR was performed.7
There are some reasons why TOR for OHCA may be a sensible policy. TOR protocols are validated in various settings with prospective and retrospective cohort studies conducted in Canada, Japan, Singapore and the United States revealing 100% specificity and positive predictive value in predicting poor neurological outcomes and death.8, 9, 10, 11 With a substantial increase in demand on EMS,12 the effective use of TOR protocol could reduce urgent transports without reducing survival to hospital discharge.9 The Singapore Civil Defence Force reported an increase of 7.4% emergency calls in 2016 compared to 2015, and 75.3% of calls received in 2016 were related to chest pain, breathlessness, unconsciousness and cardiac arrest.13 In addition, the absence of a TOR protocol will likely result in all OHCA, including futile cases, being treated in hospital incurring potentially avoidable costs. In the United States, an annual cost of $500 million was estimated nationwide for transporting futile OHCA cases,14 and an annual cost of $58 million was estimated to have incurred nationally for resources such as ambulance, physician and hospital reimbursement on failed resuscitation attempts on OHCA cases.15
While there have been studies predicting health care costs relating to OHCA16, 17 and costs arising from non-adherence of TOR protocol,18 there is little published information on how the use of TOR protocol can reduce costs in managing OHCA. The aim of this study is to estimate the change in the frequency of costly events from the application of an advanced life support TOR protocol versus traditional practice in Singapore. We use a Markov model in this study to represent a stochastic processes that can change over time.19 The method enables costs and health outcomes to be predicted and the effects of uncertainty to be included and evaluated.
Methods
Setting and population
Singapore is a densely populated city-state, with a population of over 5 million within a land area of 710 km2, 20 The Singapore Civil Defence Force is the single provider of emergency services. Responses are activated via a centralised system and cases are sent to any of the six major public hospitals.21 Prior to implementation of advanced life support TOR rule in Singapore in mid-2019, it was mandatory for all OHCA cases to be transported to hospital for continued resuscitation.
Study data
We used Singapore data from the Pan-Asian Resuscitation Outcomes Study (PAROS).22 This collaborative research effort was formed in 2010 by pre-hospital and emergency care providers in the Asia-Pacific region. A large registry has emerged for the purpose of improving outcomes across the Asia-Pacific region through the creation of a platform to support and stimulate research. For this analysis we were able to retrieve data of OHCA cases between 1 Jan 2014 to 31 Dec 2017.
TOR protocol
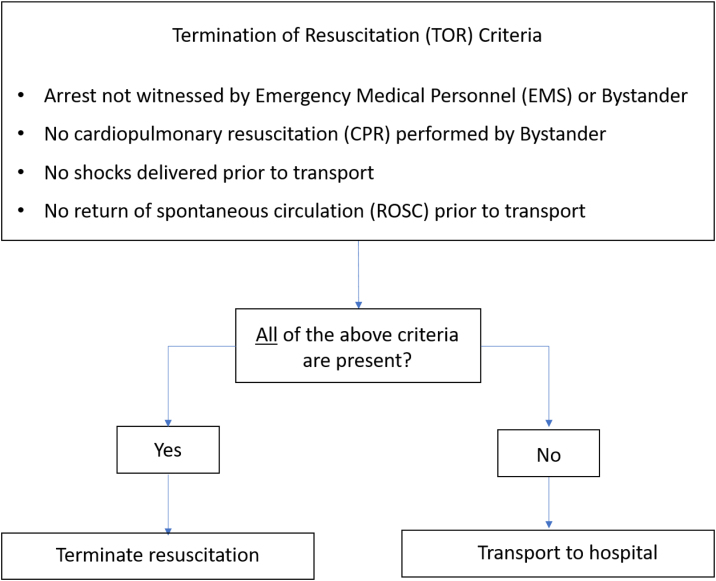
The advanced life support TOR protocol was chosen for this analysis as this protocol was adopted across Singapore in July 2019. Retrieved data of OHCA cases were reviewed by an emergency physician who determined the inclusion and exclusion criteria according to the TOR protocol designed for implementation in Singapore. Therefore, OHCA cases were excluded if: the patient was aged 16 and below; the cause of the arrest was non-cardiac, including trauma; the patient was visibly dead onsite, from rigour mortis, lividity, decomposition or decapitation; the paramedics were presented with a ‘do not resuscitate order’; or, it was concluded that the event was a non-arrest after review.23 All included cases were categorised for two outcomes based on the advanced life support TOR protocol shown in Fig. 1: either transportation to hospital is recommended, or, Termination of Resuscitation efforts is recommended.
Fig. 1.
Criteria for Termination of Resuscitation.
We used information on whether the patient survived to admission, whether they died as an inpatient and the dates of key events such as arrival at hospital, discharge from hospital and date of death.
Markov model
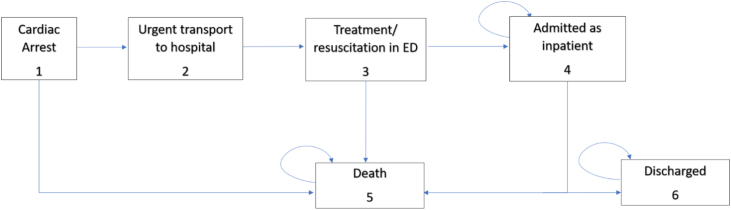
The Markov model in Fig. 2 has 6 independent states: cardiac arrest, urgent transport to hospital, treatment/resuscitation in emergency department (ED), admitted as inpatient, discharged, or death. Arrows connecting two different states signify that a patient can transition from one state to the indicated state. Looping arrows signify that a patient can remain in a particular state for consecutive cycles or that the state is permanent (i.e. death). For this analysis, the initial state of all OHCA cases is cardiac arrest. Individuals can then be urgently transported to hospital or be declared dead prior to transport. Transported cases are treated in ED, and can survive and be admitted as inpatients or be pronounced dead. To end the process, survivors can remain as an inpatient, be discharged from hospital or declared dead. The model was simulated for 10,000 hypothetical patients, where daily transitions are estimated from the initial state to 30 days after inpatient admission to show the number of bed days used.
Fig. 2.
Markov model path for out-of-hospital cardiac arrest patients. The initial state of patients is cardiac arrest. Arrows indicate possible transitions of patients from one state to another. Looping arrows indicate a patient can remain in that state for consecutive cycles.
The outcomes for the baseline comparator of ‘Existing Practice’ arise from modelling the actual events recorded in the data, where all OHCA cases were urgently transported to hospital. The use of a TOR protocol generates plausible different outcomes as some proportion of cases are to be declared dead prior to urgent transport and so become unavailable for the remaining states of the model. We show the changes to events by comparing a simulation of ‘TOR’ protocol used versus ‘Existing Practice’ for a cohort of 10,000 hypothetical patients.
Transition probabilities
The probability of cases moving between the states at the end of each model cycle was calculated for ‘Existing Practice’ and for ‘TOR’. Both time fixed probabilities and time varying probabilities were specified by counts of the number of cases eligible to transition from a state and the actual number of cases that transitioned. To evaluate the impact of uncertainty on the model parameters, Dirichlet prior distributions were fitted to the transition probabilities.24
Model evaluation
An analysis was performed to estimate the outcomes of number of urgent transports and ED treatments, number of inpatient bed days, and total number of deaths arising from the ‘Existing Practice’ and ‘TOR’ models. A simulation for 10,000 hypothetical patients was performed; and 5000 random resamples from the model parameters was required to provide stable estimates for the key outcomes. Model parameters have values from fitted prior statistical distributions that were obtained from a sample of individuals in the PAROS registry.
Results
We retrieved data of 9753 individual cases of OHCA, of which 4357 cases were excluded if the patient was below 16 years old, visibly dead onsite, had a ‘do not resuscitate order’, had an arrest of non-cardiac aetiology, or the event was concluded as a non-arrest. A total of 5396 OHCA cases who were transported to hospitals and diagnosed with cardiac arrest were deemed eligible to be included in the analysis.
The mean age of the included patients was 67.5 (Standard Deviation 15.6), and 67% of them were male. The transition probabilities matrix uses the data to estimate outcomes for a cohort of 10,000 hypothetical patients. The information in Table 1 shows the time fixed probabilities of the 5396 included individuals transitioning from one state to another for both ‘Existing Practice’ and ‘TOR’. Appendix Table A1 and A2 lists the time dependent probabilities for inpatients who transition to ‘discharged’ or ‘death’, or remain in ‘inpatient’ state.
Table 1.
Transition probabilities for ‘Existing Practice’ and ‘TOR’ for each state.
| Transition |
Existing practice |
TOR |
||||||
|---|---|---|---|---|---|---|---|---|
| From | To | Mean value (%) | Distr. | E, NE | Mean value (%) | Distr. | E, NE | |
| Cardiac Arrest | Death | Time fixed | 0 | 0, 5396 | 11.2 | 603, 4793 | ||
| Urgent Transport to ED | Time fixed | 100 | 5396, 0 | 88.8 | 4793, 603 | |||
| Urgent Transport | Treatment/resuscitation in ED | Time fixed | 100 | 5396, 0 | 100 | 4793, 0 | ||
| Treatment/resuscitation in ED | Inpatient Admission | Time fixed | 16.3 | Dirichlet | 880, 4516 | 17.6 | Dirichlet | 843, 3950 |
| Death | Time fixed | 83.7 | Dirichlet | 4516, 880 | 82.4 | Dirichlet | 3950, 843 | |
| Inpatient Admission | Inpatient Admission | Time dependent | Appendix A1 | Dirichlet | 40, 840 | Appendix A2 | Dirichlet | 39, 804 |
| Discharged Alive | Time dependent | Appendix A1 | Dirichlet | 267, 613 | Appendix A2 | Dirichlet | 266, 577 | |
| Death | Time dependent | Appendix A1 | Dirichlet | 573, 307 | Appendix A2 | Dirichlet | 538, 305 | |
ED, Emergency Department; Distr. = Distribution type; E = count of Events, NE count of non-events.
A decision to adopt a TOR protocol for OHCA cases reduced the proportion of patients facing urgent transport to hospital by 11.2% as they were to be declared dead at the scene by emergency services. Of those treated in ED under Existing Practice, 83.7% died and 16.3% were admitted to an inpatient bed. With the use of TOR protocol, 82.4% of those treated in ED died and 17.6% were admitted. Under Existing Practice, among those admitted to an inpatient bed 65.1% died, 30.3% were discharged alive after admission and average length of stay in hospital was 9.2 days. With TOR, among those admitted to an inpatient bed 63.8% died, 31.6% were discharged alive and average length of stay was 9.4 days.
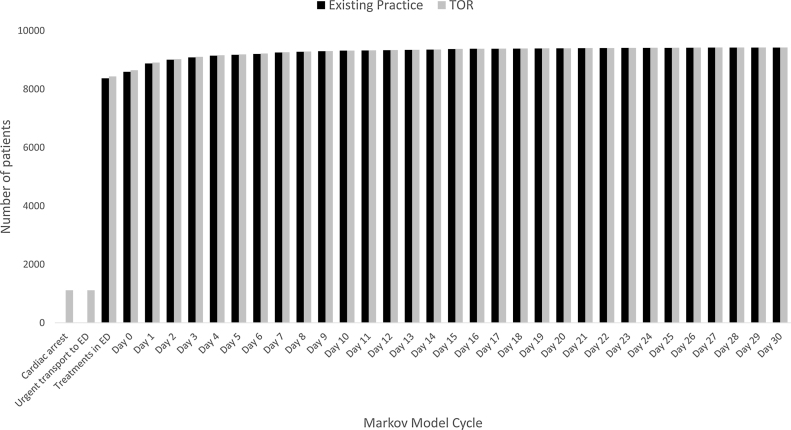
The simulation revealed that for Existing Practice all 10,000 cases are transported to hospital and treated in ED, while under conditions of the TOR protocol, 8883 cases are transported and treated. The remaining cases under TOR do not get transported and progress to the ‘death’ state. Fig. 3 shows the 1117 deaths arising from the TOR adoption in the ‘cardiac arrest’ and ‘treatments in ED’ states, whereas no deaths are incurred at these states for Existing Practice.
Fig. 3.
Cumulative number of deaths in Markov Model cycle for Existing Practice and TOR models.
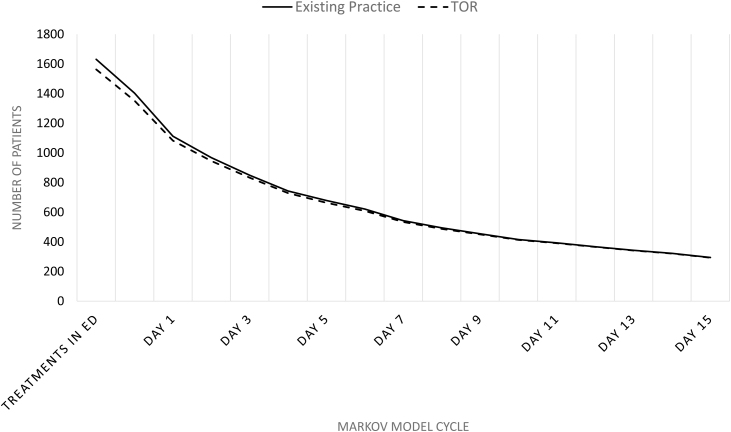
Fig. 4 reveals the number of cases admitted as inpatients following ED treatments. A small difference is noticed between Existing Practice and TOR in the initial state, 1631 versus 1562 inpatients, and subsequently converges to be approximately the same from Day 10 onwards.
Fig. 4.
Number of inpatients after ED treatments for Existing Practice and TOR models.
Table 2 reveals summary statistics for the differences in key outcomes between the ‘Existing Practice’ and ‘TOR’ models arising from the simulation. The mean number of cases urgently transported to receive ED treatments was 1118 more with Existing Practice versus TOR. In addition, there was a usage of 93 more inpatient bed days and three fewer deaths with Existing Practice in comparison to TOR.
Table 2.
Difference in key outcomes between Existing Practice and TOR models.
| No. of cases urgently transported to hospital for ED treatments | No. of inpatient bed days used | Total no. of deaths | |
|---|---|---|---|
| Mean | 1118 | 93 | −3 |
| Standard deviation | 43 | 978 | 45 |
| 95% uncertainty interval | 1117 to 1119 | 66 to 120 | 2 to 4 |
Discussion
Our findings show reduction in the costly events of ‘urgent transports to hospital for ED treatments’ and ‘inpatient bed days’ used. It was also observed that applying the TOR protocol would be associated with a small increase in the number of deaths as compared to existing practice. We do not have estimates of the expected associated savings to monetary costs but this information would be useful to consider against the expected lives lost. A notion of disinvesting in health care services that currently deliver benefits, albeit small ones, is rarely considered in the cost effectiveness framework.25 Yet, the economics of the use of TOR protocol are somewhat driven by the amount of cost saved per life year lost. Building on the analyses presented here to answer this empirical question is a useful way to inform a future adoption decision.
With TOR, our study found urgent transports to reduce from 100% to 88.8%. This is comparable to other studies reporting projected transport rates with the adoption of advanced life support TOR rule. In a systematic review on TOR performance including studies from 7 countries, the mean projected transport rate was 76% and ranged from 66% to 94%.7 These findings suggest that a significant reduction in transport rate can result with TOR implementation, and that the rate varies in different settings and populations.
Other studies have reported substantial health care costs for cardiac arrest patients as a result of extended hospital stays. A Japanese study of 21,750 OHCA patients identified inpatient stays of 23–32 days with costs of $28,097–$31,161.17 A German study involving sudden cardiac arrest patients found high costs related to ICU stays.26 Another study found hospital charges amounting to $3.8 million from the resuscitation of six out-of-hospital traumatic cardiopulmonary arrest patients, who were recovered into a neurologically devastated state.18 Two cost-effectiveness studies reported relatively high costs for additional health gains from treating OHCA.16, 27
Pre-hospital services and EDs are high cost services as they need to be available on demand, able to respond to multiple simultaneous calls, and are equipped with sophisticated technical equipment and trained personnel to handle various crises.28 Proper adherence to TOR protocol could save valuable time and preserve scarce hospital resources, such as emergency services, treatment equipment and inpatient beds, for other patients with true emergency medicine needs and better survivability. This would be of particular importance to Singapore setting, where ambulance call volume has increased over recent years.13, 29 Also, Singapore's built environment consisting of high-rise buildings and congested streets contributes to delays in reaching patients in time of emergencies.30 Adopting TOR protocol will allow resources to be channelled to other time sensitive conditions with a higher chance of good outcomes such as stroke, myocardial infarction and trauma.
Our findings of three extra deaths per 10,000 cases with TOR is important. The difference arises from two patients in the PAROS dataset who were transported to hospital, survived past 30 days and were neurologically intact with a cerebral performance category (CPC) score of 2, despite being ineligible for transportation and treatment according to TOR protocol. The factors which contributed to their survival are unclear given the retrospective nature of this study. In a recent systematic review on diagnostic performance of the TOR protocol, it reported that despite an overall high positive predictive value, a lower specificity and positive predictive value was noticed in non-Western regions.7 Thus, the review highlighted the importance of local validation of TOR protocols to prevent the loss of potential survivors. Nevertheless, a study conducted in 2012 in Singapore reaffirmed a 100% specificity and positive predictive values in predicting poor neurological outcomes in OHCA patients with the application of basic and advanced life support TOR guidelines.8
There are several limitations to this study. First, there were no data on the length of time spent in ICUs by inpatients, and these beds are much higher cost than a normal ward bed. It is possible that patients under existing practice who were admitted will have incurred higher costs than an average inpatient. This would have provided a richer understanding of the expected cost savings and changes to health outcomes from the use of TOR protocol. Second, this hypothetical implementation may differ from a real world implementation of TOR, as there may be circumstances where pre-hospital providers fail to adhere to TOR protocol once implemented. Third, it is possible that survival rates following hospitalisation for cardiac arrest has improved in the interim from when these data were collected by PAROS. Finally, our study does not take into consideration the extra costs that could occur with TOR protocol implementation. Such as the additional time required by paramedics to do the following if TOR protocol needs to be adhered to: explaining to family about TOR and handling of grief reaction; completing resuscitation protocol; and waiting for police to arrive as part of pronouncement of death procedure. There could also be patient and family-oriented benefit to transporting an OHCA case to the hospital for resuscitation even if the patient ultimately does not survive, which would be absent with TOR adoption. Finally, our model may underestimate the benefits of implementing TOR in the Singapore context, as the protocol is not applicable to arrests of non-cardiac aetiology. Treating medical-type collapses, which has a higher mortality than arrest from a cardiac cause, would similarly benefit from the implementation of TOR protocol. We acknowledge that some of these limitations can be addressed with the use of post-implementation real world data. For this reason, we aim to perform a follow-up study after TOR's implementation in Singapore.
Conclusion
The findings of this study provide some evidence for directing resources towards the implementation of TOR. The use of TOR protocol was shown to result in a reduced number of urgent transports to hospital, fewer patients requiring ED treatments and shorter duration of admission compared to existing practice. This study also demonstrated a marginal difference in the number of deaths between both scenarios, highlighting the need for a comprehensive economic evaluation of using TOR criteria. Although further evidence is needed to strengthen these findings, potential reduction in costs pertaining to transport, emergency treatments and hospital admissions is anticipated by adhering to TOR guidelines.
Using pre-hospital services for medically futile resuscitations of OHCA cases can take away valuable resources needed for other time sensitive conditions with better chances of survival. Hence, TOR protocol could play an effective role in resource allocation so that cardiopulmonary resuscitation is performed on those who will potentially benefit from it.
Ethics
The Centralised Institutional Review Board (2013/604/C) and Domain Specific Review Board (2013/00929) granted approval for this study with a waiver of patient informed consent. This project was deemed exempt from Duke Institutional Review Board (Pro00103613).
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding information
This research was supported by funding under Duke/Duke-NUS Research Collaboration Pilot Project Award, provided by Duke-NUS Medical School.
Credit author statement
Nicholas Graves: conceptualised and supervised the analysis, and reviewed the manuscript.
Nuraini Nazeha: developed the methodology and analysis models, and wrote the manuscript.
Jinny J. Y: reviewed the data, and determined inclusion and exclusion criteria.
Marcus Eng Hock Ong, Alexander T. Limkakeng Jr, Anjni Patel Joiner, Audrey Blewer, Nur Shahidah, Gayathri Devi Nadarajan, Desmond Renhao Mao: reviewed and edited the manuscript for intellectual content.
Declaration of Competing Interest
The authors report no declarations of interest.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.resplu.2021.100092.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Daya M., Schmicker R., Zive D., Rea T., Nichol G., Buick J. Out-of-hospital cardiac arrest survival improving over time: results from the resuscitation outcomes consortium (ROC) Resuscitation. 2015;91:108–115. doi: 10.1016/j.resuscitation.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CARES . 2017. United States: cardiac arrest registry to enhance survival. Available from: https://mycares.net/sitepages/uploads/2018/2017flipbook/index.html?page=26 [13.01.21] [Google Scholar]
- 3.Gräsner J.-T., Lefering R., Koster R.W., Masterson S., Böttiger B.W., Herlitz J. EuReCa ONE-27 Nations, ONE Europe ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Ong M.E.H., Shin S.D., De Souza N.N.A., Tanaka H., Nishiuchi T., Song K.J. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS) Resuscitation. 2015;96:100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 5.Lai H., Choong C.V., Fook-Chong S., Ng Y.Y., Finkelstein E.A., Haaland B. Interventional strategies associated with improvements in survival for out-of-hospital cardiac arrests in Singapore over 10 years. Resuscitation. 2015;89:155–161. doi: 10.1016/j.resuscitation.2015.01.034. [DOI] [PubMed] [Google Scholar]
- 6.Morrison Laurie J., Kierzek G., Diekema Douglas S., Sayre Michael R., Silvers Scott M., Idris Ahamed H. Part 3: Ethics. Circulation. 2010;122 doi: 10.1161/CIRCULATIONAHA.110.970905. S665–S75. [DOI] [PubMed] [Google Scholar]
- 7.Nas J., Kleinnibbelink G., Hannink G., Navarese E., Royen N., Boer M.-J. Diagnostic performance of the basic and advanced life support termination of resuscitation rules: a systematic review and diagnostic meta-analysis. Resuscitation. 2019:148. doi: 10.1016/j.resuscitation.2019.12.016. [DOI] [PubMed] [Google Scholar]
- 8.Cheong R.W., Li H., Doctor N.E., Ng Y.Y., Goh E.S., Leong B.S. Termination of resuscitation rules to predict neurological outcomes in out-of-hospital cardiac arrest for an intermediate life support prehospital system. Prehosp Emerg Care. 2016;20:623–629. doi: 10.3109/10903127.2016.1162886. [DOI] [PubMed] [Google Scholar]
- 9.Drennan I.R., Case E., Verbeek P.R., Reynolds J.C., Goldberger Z.D., Jasti J. A comparison of the universal TOR Guideline to the absence of prehospital ROSC and duration of resuscitation in predicting futility from out-of-hospital cardiac arrest. Resuscitation. 2017;111:96–102. doi: 10.1016/j.resuscitation.2016.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kashiura M., Hamabe Y., Akashi A., Sakurai A., Tahara Y., Yonemoto N. Applying the termination of resuscitation rules to out-of-hospital cardiac arrests of both cardiac and non-cardiac etiologies: a prospective cohort study. Crit Care. 2016;20:49. doi: 10.1186/s13054-016-1226-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morrison L.J., Verbeek P.R., Zhan C., Kiss A., Allan K.S. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation. 2009;80:324–328. doi: 10.1016/j.resuscitation.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 12.Andrew E., Nehme Z., Cameron P., Smith K. Drivers of increasing emergency ambulance demand. Prehosp Emerg Care. 2020;24:385. doi: 10.1080/10903127.2019.1635670. [DOI] [PubMed] [Google Scholar]
- 13.SCDF . 2016. Singapore: Singapore civil defence force. Available from: https://www.scdf.gov.sg/docs/default-source/scdf-library/publications/amb-fire-inspection-statistics/ems-stats-2016.pdf [13.01.21] [Google Scholar]
- 14.Bonnin M.J., Pepe P.E., Kimball K.T., Clark P.S., Jr. Distinct criteria for termination of resuscitation in the out-of-hospital setting. JAMA. 1993;270:1457–1462. doi: 10.1001/jama.1993.03510120079035. [DOI] [PubMed] [Google Scholar]
- 15.Suchard J.R., Fenton F.R., Powers R.D. Medicare expenditures on unsuccessful out-of-hospital resuscitations. J Emerg Med. 1999;17:801–805. doi: 10.1016/S0736-4679(99)00086-4. [DOI] [PubMed] [Google Scholar]
- 16.Ginsberg G.M., Kark J.D., Einav S. Cost-utility analysis of treating out of hospital cardiac arrests in Jerusalem. Resuscitation. 2015;86:54–61. doi: 10.1016/j.resuscitation.2014.10.024. [DOI] [PubMed] [Google Scholar]
- 17.Fukuda T., Yasunaga H., Horiguchi H., Ohe K., Fushimi K., Matsubara T. Health care costs related to out-of-hospital cardiopulmonary arrest in Japan. Resuscitation. 2013;84:964–969. doi: 10.1016/j.resuscitation.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 18.Mollberg N., Wise S., Berman K., Chowdhry S., Holevar M., Sullivan R. The consequences of noncompliance with guidelines for withholding or terminating resuscitation in traumatic cardiac arrest patients. J Trauma. 2011;71:997–1002. doi: 10.1097/TA.0b013e3182318269. [DOI] [PubMed] [Google Scholar]
- 19.Briggs A., Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13:397–409. doi: 10.2165/00019053-199813040-00003. [DOI] [PubMed] [Google Scholar]
- 20.2020. Singapore department of statistics. Available from: https://www.singstat.gov.sg/ [14.10.20] [Google Scholar]
- 21.Tay P.J.M., Pek P.P., Fan Q., Ng Y.Y., Leong B.S.-H., Gan H.N. Effectiveness of a community based out-of-hospital cardiac arrest (OHCA) interventional bundle: Results of a pilot study. Resuscitation. 2020;146:220–228. doi: 10.1016/j.resuscitation.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 22.Doctor N.E., Ahmad N.S., Pek P.P., Yap S., Ong M.E. The Pan-Asian Resuscitation Outcomes Study (PAROS) clinical research network: what, where, why and how. Singap Med J. 2017;58:456–458. doi: 10.11622/smedj.2017057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morrison L.J., Verbeek P.R., Vermeulen M.J., Kiss A., Allan K.S., Nesbitt L. Derivation and evaluation of a termination of resuscitation clinical prediction rule for advanced life support providers. Resuscitation. 2007;74:266–275. doi: 10.1016/j.resuscitation.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 24.Briggs A., Sculpher M., Claxton K. Oxford University Press; 2006. Decision modelling for health economic evaluation. [Google Scholar]
- 25.Karnon J., Carlton J., Czoski-Murray C., Smith K. Informing disinvestment through cost-effectiveness modelling: is lack of data a surmountable barrier? Appl Health Econ Health Policy. 2009;7:1–9. doi: 10.1007/bf03256137. [DOI] [PubMed] [Google Scholar]
- 26.Graf J., Mühlhoff C., Doig G.S., Reinartz S., Bode K., Dujardin R. Health care costs, long-term survival, and quality of life following intensive care unit admission after cardiac arrest. Crit Care. 2008;12 doi: 10.1186/cc6963. R92-R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naess A.C., Steen P.A. Long term survival and costs per life year gained after out-of-hospital cardiac arrest. Resuscitation. 2004;60:57–64. doi: 10.1016/s0300-9572(03)00262-4. [DOI] [PubMed] [Google Scholar]
- 28.Simonet D. Cost reduction strategies for emergency services: insurance role, practice changes and patients accountability. Health Care Anal. 2009;17:1–19. doi: 10.1007/s10728-008-0081-0. [DOI] [PubMed] [Google Scholar]
- 29.Ng Y.Y. Optional use of emergency services. Singap Family Physician. 2013;39:8–13. [Google Scholar]
- 30.Lateef F. The emergency medical services in Singapore. Resuscitation. 2006;68:323–328. doi: 10.1016/j.resuscitation.2005.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.