Abstract
Aim
To review the literature on briefing and debriefing in neonatal resuscitation using International Liaison Committee on Resuscitation (ILCOR) methodology to see if a formal systematic review is justified.
Methods
This scoping review was undertaken by an ILCOR Newborn Life Support scoping review team and guided by the ILCOR methodological framework and the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR). Studies were eligible for inclusion if they were peer-reviewed, compared briefing/debriefing of healthcare professionals who had completed a neonatal resuscitation or simulated resuscitation and reported outcomes for infants, families or staff. PubMed, Embase, Cochrane, and Web of Science databases were searched.
Results
This review included four studies that reported on three briefing/debriefing interventions: video debriefing, the use of checklists with a briefing/debriefing component and rapid cycle deliberate practice. Video debriefing was associated with improvements in the process of care and adherence to resuscitation guidelines. Use of checklists was associated with improvements in short term clinical outcomes and a reduction in communication problems. Rapid cycle deliberate practice may lead to short but not sustained improvements in algorithm compliance and timely completion of resuscitation steps.
Conclusion
This scoping review did not identify sufficient new evidence to justify conducting new systematic reviews or review of current resuscitation guidelines. Improvements in the process of care, short term clinical outcomes and reduction in communication problems were associated with briefing/debriefing supported by video, checklists or rapid, cycle deliberate practice. It highlights knowledge gaps, including the need to consider briefing/debriefing separately from other interventions, the effect of briefing/debriefing on short- and long-term clinical outcomes and the effect of rapid cycle deliberate practice on resuscitation training.
Keywords: Neonatal resuscitation, Neonatal cardiopulmonary resuscitation, Neonatal CPR, Neonatal basic life support, Neonatal advanced life support, Scoping review
Introduction
A previous International Liaison Committee on Resuscitation (ILCOR) systematic review on Debriefing of Resuscitation Performance (EIT #645)1 considered debriefing following in hospital and out of hospital cardiac arrest in adults and children. It recommended data-driven, performance-focused debriefing of rescuers but acknowledged it as a weak recommendation based on very low certainty of evidence.
However, no review has been carried out to evaluate the impact of briefing or debriefing on outcomes in neonatal resuscitation. The United States Joint Commission on Accreditation of Healthcare Organizations recommended that maternity hospitals should ‘conduct team training’ and ‘conduct debriefings to evaluate team performance and identify areas for improvement’ with the aim of preventing perinatal mortality and morbidity.2 A previous systematic review of briefing/debriefing by the ILCOR Neonatal Life Support (NLS) Task Force in 2010 primarily focused on use of these techniques in the context of training rather than clinical care.3 This scoping review was performed to review the current literature on the effects of briefing and debriefing on outcomes of neonatal resuscitation in order to determine whether the body of published evidence supported proceeding to a systematic review.
Methods
This scoping review was based on a PICOST question (Population, Intervention, Comparator, Outcome, Study Designs and Timeframe) created by the ILCOR NLS Task Force and approved by the ILCOR Scientific Advisory Committee (SAC) (Table 1).
Table 1.
PICOST question.
| Population | Among health care professionals involved in the resuscitation or simulated resuscitation of a neonate (P) |
| Intervention | does briefing/debriefing (I) |
| Comparator | in comparison to no briefing/debriefing (C) |
| Outcomes | improve outcomes for infants, families or staff (O) |
| Study designs | Randomised controlled trials (RCTs) and non-randomised studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies) were eligible for inclusion. Manikin studies were eligible for inclusion but animal studies were excluded. Conference abstracts and unpublished studies (e.g. trial protocols) were excluded. |
| Timeframe | All years and all languages are included as long as there is an English abstract. Literature search updated to January 27, 2020. |
Terms used in the PICOST were pre-defined (Appendix 1) and a structured search strategy was developed by an information specialist (Appendix 2). Study inclusion and exclusion criteria were pre-defined:
Inclusion
Controlled studies addressing the PICOST question were eligible for inclusion. Checklist-based studies were included if the checklist was specifically used for the purposes of conducting a team briefing/debriefing. Briefing/debriefing studies were included if performed in the context of real or simulated resuscitation with humans or manikins. Psychomotor skills studies were only included if accompanied by debriefing.
Exclusions
Conference abstracts, published protocols without a subsequently published paper, studies that only had an abstract and papers without an English abstract were excluded. Briefing/debriefing in paediatric or adult resuscitation were excluded. Studies of bundles of care where the impact of briefing/debriefing could not be separated from the rest of the bundle were excluded.
Studies were screened for eligibility using Covidence.4 This allowed independent title and abstract review by two authors (JF,NY) to evaluate if full text review was warranted. Studies put forward by both authors were included, conflicting opinions were reviewed, discussed and resolved by consensus.
Studies identified for full text review were independently reviewed by two authors (JF,NY) who reached consensus regarding inclusion or exclusion of the study. For the purposes of this scoping review, the authors agreed that psychomotor skill feedback device studies would only be included if supported by a briefing or debriefing component.
Studies that underwent full text review were analyzed for type of briefing or debriefing intervention, relevant learning points and knowledge gaps. The findings of the literature review were considered to inform an assessment of remaining knowledge gaps in the literature on this topic. The draft scoping review was circulated to the ILCOR Neonatal Life Support Task Force for review and feedback. The scoping review was posted on the ILCOR website for public comment. These comments were reviewed and incorporated, as appropriate, into this manuscript.
Results
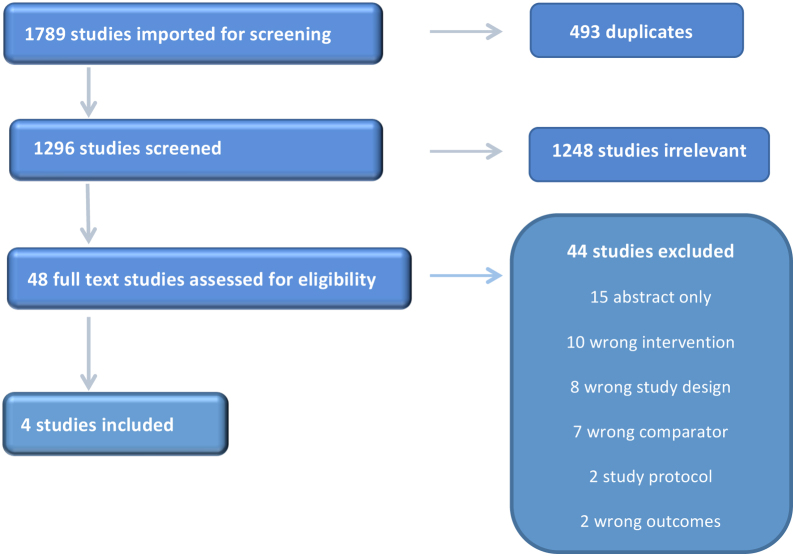
A total of 1789 studies were identified using the structured search strategy. Studies screened by title and abstract, those that underwent full text review and studies selected for data extraction are shown in the PRISMA5 flow chart (Fig. 1) along with reasons for exclusion following full text review. Of note a number of papers about the Helping Babies Breathe programme were excluded because the intervention was a bundle of care and often included implementation of health system wide logistical components. Thus, the effects of briefing or debriefing could not be isolated from effects of other interventions. Ultimately, four studies were included in the scoping review.
Fig. 1.
Scoping review PRISMA flow chart.
The four studies are listed in the included studies evaluation (Table 2). One study considered video debriefing,6 one considered the use of a checklist along with video debriefing,9 one considered the use of a checklist with a team brief/debriefing as the main part of a quality improvement bundle8 and one looked at rapid cycle deliberate practice compared to standard simulation debriefing.10
Table 2.
Evaluation of included studies.
| Study | Study details | Participants | Interventions | Comparisons | Outcomes |
|---|---|---|---|---|---|
| Skåre6 | Prospective, pre/post interventional study. Initial phase of a multi-faceted quality improvement initiative. | Midwives and physicians involved in resuscitation of compromised infants at a Norwegian teaching hospital in 2014. | Introduction of weekly video assisted debriefing (3rd April–23rd June 2014) | NRPE scores in the pre, peri and post intervention period. | Pre vs post implementation |
| Skill performance and process of care evaluation before, during and after introducing video debriefing of resuscitation events. | 73 resuscitation events pre- implementation were compared to 45 events post- implementation | Followed by monthly video assisted debriefing in a post implementation period (24th June–24th August 2014) | Baseline evaluations were performed 15th January–2nd April 2014. | Total NRPE scores (77% vs 89%, p < 0.001) | |
| Evaluation used a modified Neonatal Resuscitation Evaluation Performance (NRPE) tool. | Improved preparation & adherence to the initial steps of a neonatal resuscitation algorithm (75% vs 90%, p < 0.001) | ||||
| NRPE scores by single investigator but intra-rater reliability and inter-rater reliability checked by a 2nd investigator. | Improved PPV (70% vs 100%, p < 0.001) | ||||
| Improved group function, communication–88% vs 100%, p < 0.001) | |||||
| Sauer8 | Single centre pre-post quality improvement initiative. | High risk delivery team | Described as a bundle of delivery room interventions. Individual interventions are not clearly described. | Pre vs post intervention: Data for 249 infants prior to the intervention were compared to data for 299 born after the intervention. | Functioning pulse oximeter by 2 min (26% to 55%, p value unclear) |
| Data on 548 infants representing every admission to the Palomar Rady Children’s Hospital NICU during a 35 month period (1st Jan 2010–30th November 2012). | (not further specified) | The delivery room checklist is shown in the paper and appears to be the main intervention. | % intubated (14% vs 5%, p < 0.001) | ||
| It aimed to achieve: | Briefing/debriefing is included within the checklist. | Surfactant use (2.8 vs 1.0%, p = 0.198) | |||
| ● Placement of a functioning pulse oximeter by two minutes after birth | Normothermia on NICU admission (78% vs 86%, p = 0.017) | ||||
| ● Delayed intubation in favour of CPAP use | % using checklist (25% to 92%, p < 0.001) | ||||
| ● Normothermia at NICU admission | Outcome data collected for RDS, BPD, death, PDA, pneumothorax, NEC, ROP, post haemorrhagic hydrocephalus (PHH), IVH, length of stay. Univariable & multivariable logistic regression done. (MV regression not for BPD, death, ROP, PHH) | ||||
| ● Use of a team briefing, debriefing and delivery room checklist to promote teamwork and communication between the obstetrician, labour and delivery room staff and the neonatal resuscitation team | No significant differences except for ↓ROP in univariable logistic regression for post intervention group (OR 0, 0.696; p = 0.008) | ||||
| Katheria9 | Pre/post study to evaluate the implementation of a checklist that included pre-brief and debrief components. Outcomes were measured at video resuscitation quality assurance (QA) meetings. The completed pre-brief checklist was reviewed prior to seeing each video to see if planned preparation happened. The completed debrief findings were reviewed after watching each video to see if team conclusions matched video review conclusions. | Neonatal faculty, neonatal fellows, pediatric residents in training, nurses, respiratory therapists. | Pre-brief: | First two years of using the delivery room checklist (March 2009–November 2011, 260 completed checklists) were compared with the 3rd year of using the delivery room checklist (185 completed checklists). | Most common problems: |
| The components of the checklist were informed by crew resource management training previously undertaken by NICU staff and ongoing video reviews of neonatal resuscitations. | Introduction of team members, role assignments, specific considerations, team empowered to voice concerns and to call back orders. | Communication (n = 58) | |||
| Equipment checklist with duty specific sub lists and required setup with the requirement to acknowledge completion. | Equipment preparation and use (n = 56) | ||||
| Debrief: | Inappropriate decisions (n = 87) | ||||
| Free form questions on what went well, what didn’t go well and what needed to be improved. Debrief completed soon after resuscitation with all team members involved. Members responded in order of seniority, most junior first. | Leadership (n = 56) | ||||
| QA review: | Procedures (n = 25) | ||||
| Completed checklists were reviewed with special emphasis on the debrief section at twice monthly video resuscitation quality assurance meetings | During the 3rd year of use (Nov 2011 to May 2012), 185 checklists were reviewed. | ||||
| Communication problems ↓ from 22% to 4% (p < 0.001). This finding was reported on the checklists and validated in audio & video recordings. | |||||
| Non-significant changes: | |||||
| ● Lack of equipment preparation & use (21% vs 23%) | |||||
| ● Inappropriate decisions (33% vs 27%) | |||||
| ● Leadership (21% vs 18%) | |||||
| ● Procedures-sequence, timing, technique (10% vs 6%) | |||||
| Magee10 | Prospective, randomised control study of Rapid Cycle Deliberate Practice (RCDP) vs. traditional simulation debriefing methods for neonatal resuscitation training. | 38 pediatric interns in a large academic training programme. | Instructional simulation session with RCDP | Instructional simulation session with standard debriefing that occurred at the conclusion of the simulation scenario | 34 interns included in the analysis. 4 were excluded due to changes in study protocol and technical issues. |
| Study occurred over 1.5 years with 3−4 interns enrolled each month. | All the interns held a current NRP certification and were on a neonatology or newborn nursery rotation when enrolled. | Immediate simulation retest | Immediate simulation retest | RCDP group compared to simulation debriefing group: | |
| Randomisation occurred in blocks of 4 interns to account for variations in abilities in the first year of academic training. | . | Higher MCAF scores | |||
| Pre-survey looking at confidence in neonatal resuscitation and previous experience completed. | (89% vs 84%, p < 0.026) | ||||
| Primary outcome was the interns’ score on the megacode assessment form (MCAF) on immediate testing. | Initiated PPV ventilation within 1 min (100% vs 71%, p < 0.05) | ||||
| Secondary outcomes measured at a 4-month follow-up were: confidence level in neonatal resuscitation, recall MCAF scores and time to perform critical interventions. | More consistently provided PPV for the appropriate duration of time before starting CC (17 s vs 12 s, p < 0.05) | ||||
| Administered epinephrine earlier (152 s vs 180 s, p = 0.039) | |||||
| Self-reported confidence levels increased in both groups but were not different between the two groups. | |||||
| MCAF scores and time to perform critical interventions at 4 months were not different between the two groups. |
Three types of interventions were identified: video debriefing, the use of checklists with a brief/debriefing component and rapid cycle deliberate practice.
Video debriefing
Skåre et al installed motion-activated video cameras in every neonatal resuscitation bay in a Norwegian teaching hospital.6 Using recorded footage from resuscitations of compromised infants, they first conducted baseline skill performance and process of care assessments on 74 resuscitation events using the Neonatal Resuscitation Performance Evaluation (NRPE) Tool.7 Then they implemented weekly video assisted debriefing using this footage. The debriefing was led by two experienced facilitators and focused on guideline adherence and non-technical skills. Video-assisted debriefing was reviewed in departmental meeting and by the end of the study period, 78% of the pediatric residents had attended.
The study period was 7 months and the team evaluations were carried out pre, peri and post implementation and the number of events evaluated was 74, 69 and 45, respectively. Subcategories of group function/communication, preparation and initial steps, communication of heart rate, administration of oxygen, positive pressure ventilation, endotracheal intubation, chest compressions, administration of medicines, and intravenous access were considered.
A before and after comparison of implementation of video assisted debriefing evaluation showed that overall NRPE score improved from a median (IQR) of 77% (75, 81) to 89% (86,93) p < 0.001. Improvements in the NRPE score were seen in the following subcategories:
-
•
Group function/communication88% (75,90) to 100% (92,100)p = 0.001
-
•
Preparation and initial steps75% (70, 80) to 90% (80, 100)p < 0.001
-
•
Positive pressure ventilation70% (67, 75) to 100% (80, 100)p < 0.001
No significant differences were reported for communication of heart rate, administration of oxygen, endotracheal intubation or administration of medicines.
One limitation of the study is the before and after design. Improvements could have been due to a “Hawthorne effect” (i.e. the candidates changed their behavior because they were aware they were being observed). Additional limitations were that the video reviewer was not blinded to the phase of the trial as videos had to be deleted immediately after review at their institutional review board’s request, and the video reviewer was a member of the clinical service being reviewed, and so may have been able to recognize participants, as no measures were taken to mask their identity. Few of the pediatric residents were able to attend every video debriefing session, and only 78% attended at least one video debriefing. The authors acknowledge that whilst they have shown improvements in the process of care and adherence to resuscitation guidelines the study was not powered to detect changes in clinically relevant outcomes.
Checklists
Two studies were identified that utilized checklists specifically for the purposes of briefing or debriefing in neonatal resuscitation.
Sauer et al implemented a quality improvement bundle that included briefing, debriefing, and delivery room checklists.8 Other aspects of the quality improvement bundle were emphasis on placement of a functioning pulse oximeter, measures directed at achieving normothermia on NICU admission and avoiding intubation by using CPAP. Prompts related to pulse oximeters and thermal care were included on the checklist.
This was a single centre, before and after quality improvement study and involved all deliveries attended by the high-risk delivery team over a 35-month period. The intervention was the use of a delivery room checklist that included brief and debriefing components. A total of 249 infants were studied prior to introducing the checklist and were compared with 299 infants studied after introduction of the checklist. Data were collected retrospectively for 5 months before the intervention and then prospectively for 6 months from the start of the intervention. There was no intervening washout period. The study reported the process variables that measured the implementation of components of the bundle. These were the use of the checklist and rates of: intubation, surfactant use, normothermia on NICU admission and having a functioning pulse oximeter by 2 min of age.
With the introduction of the checklist documentation that a briefing and debriefing had been performed, increased from 25% to 92% (p < 0.001). The proportion of intubated babies decreased from 14.1% to 5.4% OR 0.35 (95% CI 0.17, 0.66, p < 0.001). Normothermia on NICU admission improved from 78.3% to 86.3% (OR 1.74, 95% CI 1.09, 2.8, p = 0.017). The proportion of babies with a stable signal on a pulse oximeter yielding oxygen saturation at 2 min of age increased from 26% to 55% during the period the checklist was implemented. The authors reported that improvements in all the measured process variables increased with increasing use of the checklist.
In unadjusted analysis of patient outcome data, there was a decrease in rates of retinopathy of prematurity between time periods, but the authors advised cautious interpretation as this may have been due to chance. No differences were found for respiratory distress syndrome, death, bronchopulmonary dysplasia, patient ductus arteriosus, pneumothorax, necrotising enterocolitis, post-haemorrhagic hydrocephalus, IVH and length of stay.
Limitations of the study included that it was from a single centre and baseline data were retrospectively collected. Wider unit policy changes regarding early intubation also could have impacted intubation rates, making the singular impact of the checklist harder to assess.
Katheria et al conducted a quasi before/after study evaluating the early and later implementation of a checklist including brief and debriefing components.9 The components of the checklist were informed by crisis resource management training previously undertaken by NICU staff and ongoing video reviews of neonatal resuscitations. The first two years of using the delivery room checklist (260 completed checklists) were compared with the 3rd year of using the delivery room checklist (185 completed checklists). Outcomes were measured at video resuscitation quality assurance meetings where the completed briefing checklist was reviewed, prior to seeing each video, to see if planned preparation happened. The completed debriefing findings were reviewed after watching each video to see if team conclusions matched those from the video review.
The most common problems seen were communication (n = 58), equipment preparation and use (n = 56), inappropriate decisions (n = 87), leadership (n = 56) and procedures (n = 25). Common communications problems were absence of closed loop communication, ambiguous orders/requests from leader, multiple conversations occurring at once, or the team not vocalizing concerns. Neonatal faculty, fellows, residents in training, nurses and respiratory therapists attended the video resuscitation quality assurance sessions and learning was shared. These communication problems decreased from 22% to 4% (p < 0.001) between the first 2 years of checklist use and the 3rd year. This finding was reported on the review of briefing and debriefing checklists and validated in audio & video recordings. No other statistically significant changes were reported.
Limitations of the study were that it was from a single centre and considered early vs later in the intervention rather than true pre/post intervention study design.
Rapid cycle deliberate practice (RCDP) vs. standard debriefing
Magee et al performed a randomised controlled trial to compare rapid cycle deliberate practice (RCDP) to standard simulation debriefing for teaching neonatal resuscitation.10 Outcomes were the learners’ technical abilities as measured by the NRP Megacode Assessment Form (MCAF),11 confidence level as measured via survey, and recall in neonatal resuscitation measured using the MCAF at a follow-up session four months later. The study was conducted at a large academic center and enrolled 38 pediatric interns, all of whom had completed Neonatal Resuscitation Program (NRP) provider education. Self-reported baseline confidence and experience levels were recorded. All participants underwent either an instructional simulation session with standard debriefing that occurred at the conclusion of the simulation scenario or an instructional simulation session with RCDP.
Efforts were made to ensure standardization and consistency in teaching by using the same neonatology fellow to facilitate all sessions, using the same instructional simulation scenario, and using prewritten scripts, setup checklists, and teaching point checklists. A senior neonatologist NRP instructor who was trained in simulation also observed the teaching in order to monitor for inconsistencies. Outcomes for both groups were measured using a 15-min simulation test, using a scenario similar to the teaching scenario, that was conducted immediately after the instructional simulation. Both scenarios involved a term infant born with a heart rate of 50 beats per minute and no respiratory effort. Secondary outcomes were a post-instructional survey of confidence and a 2nd simulation test at 4 months after the initial session for both groups.
On immediate testing, subjects in the intervention (RCDP) group had higher scores on the NRP Megacode Assessment Form (MCAF), more frequently initiated positive pressure ventilation within one minute, ventilated the patient for at least 25 s prior to starting chest compressions, and administered epinephrine earlier. Learners in both groups reported increased confidence in neonatal resuscitation. At the 4-month follow up test, there was no difference in MCAF scores or timing of performing critical interventions.
Limitations of the study included that it was from a single centre. The study was also subject to the limitations of the MCAF tool for measuring neonatal resuscitation skills, which include subjectivity and that a high MCAF score could be achieved even if clinically harmful actions were performed. As outcome assessments were not blinded and participants were potentially known to the assessor this could be source of bias.
Discussion
Two prior ILCOR systematic reviews have considered (1) the effects of debriefing–but not briefing–on clinical outcomes in adult and paediatric resuscitation and (2) the use of briefing and debriefing in the context of training for neonatal resuscitation but not clinical care.3 In this scoping review, we reviewed more recent literature to address the impacts of briefing and debriefing on outcomes in neonatal resuscitation, and to assess the need for a formal systematic review of this topic. This review included both clinical and training outcomes as well as simulation-based studies.
This scoping review identified four studies assessing the use of briefing and/or debriefing in the context of neonatal resuscitation. Three studies were observational studies in clinical settings examining outcomes before and after implementation of a briefing or debriefing (in each case as components of a bimodal or multimodal intervention) and one study was a randomised controlled trial in a simulation setting comparing RCDP to standard debriefing. Three of the 4 studies evaluated clinical outcomes and all studies evaluated team performance outcomes, but there was wide variation in the specific outcomes chosen. For example, clinical outcomes included quality of PPV, proportion of patients intubated, temperature upon admission to the NICU, and adherence to the initial steps of the resuscitation algorithm. Team performance outcomes included evaluations of team communication, equipment preparation, leadership, and cumulative scores on different neonatal resuscitation scoring tools. Due to the diversity in study measures, the ability to draw conclusions about the value of briefing or debriefing is limited. In addition, the one randomised controlled trial in this scoping review found that rapid cycle deliberate practice resulted in learners achieving higher MCAF scores and completing potentially important aspects of resuscitation more rapidly than those trained using standard simulation debriefing. However this improvement was only seen immediately after training and was not evident 4 months later. The utility of RCDP may warrant further investigation including relating it to clinical rather than process outcomes and considering ways to confirm and sustain any training improvements that it may deliver.
The limited number of studies identified in this scoping review was insufficient to prompt a systematic review. Future investigations that address this PICOST question would benefit from a standard comparison of briefing or debriefing vs. no briefing or debriefing as well as the use of a more comprehensive and consistent set of outcome measures across studies in order to allow clearer comparison of studies and their interventions. Additionally, although the PICOST question considered outcomes for families, there were no studies that reported impact on families as an outcome measure.
The strengths of this scoping review include that it was underpinned by a PICOST question that had been refined by the ILCOR Neonatal Task Force, it used a pre-specified protocol and the literature review was carried out by an experienced information specialist. The Covidence systematic review software was used to provide structure to the review process and the 1296 papers identified were screened by two reviewers (JF,NY). Each reviewer was blinded to the other reviewer’s initial decision and papers were excluded only if consensus reasons were identified. The manuscript benefitted from review by the ILCOR Neonatal Task Force and Science Advisory Committee. This scoping review was posted for public comment on the ILCOR website prior to being finalised.
Weaknesses of the scoping review are that there was limited evidence available to inform this review and some interventions included a mixture of briefing, debriefing and other components. Briefing and debriefing often occurs as part of a package or bundle of interventions, which makes it more difficult to isolate the impact of that briefing or debriefing. In addition, the short and long term effects of briefing and debriefing on clinical outcomes can be hard to measure. Studies frequently report intermediate or process outcomes such as components of teamwork (e.g. communication or time to achieve a procedure) that are thought to have an important impact on clinical performance, rather than directly measuring a clinical outcome. Studies using simulation often provide only indirect evidence for improvements in patient care, as they most commonly evaluate whether briefing or debriefing in a simulation improves performance in a later simulation, rather than performance in the clinical environment, or patient outcomes. This limitation applied to the one simulation study included in this scoping review. All four included studies were conducted in teaching hospitals in well-resourced health settings, which may limit their applicability to other settings.
Conclusions
There is currently insufficient literature to evidence to warrant a systematic review of briefing/debriefing in neonatal resuscitation. Further research is needed to address the knowledge gaps identified by this scoping review, including
-
•
The effect of briefing/debriefing separate from other co-interventions.
-
•
The effect of briefing/debriefing in neonatal resuscitation on short- and long-term clinical outcomes.
-
•
The longer-term benefits of rapid cycle deliberate practice in neonatal resuscitation training.
ILCOR statement
This review includes information on resuscitation questions developed through the continuous evidence evaluation process, managed by the ILCOR. The questions were developed by ILCOR Task Forces, using strict conflict of interest guidelines. In general, each question was assigned to two experts to complete a detailed structured review of the literature, and complete a detailed evidence evaluation. Evidence evaluations are discussed at ILCOR meetings to reach consensus and produce a final summary document.
Conflicts of interest
The ILCOR Continuous Evidence Evaluation process is guided by a rigorous ILCOR Conflict of Interest policy. The following Task Force members and other authors were recused from the discussion as they declared a conflict of interest: none applicable
The following Task Force members and other authors declared an intellectual conflict of interest and this was acknowledged and managed by the Task Force Chairs and Conflict of Interest committees: none applicable
Credit author statement
All authors contributed to manuscript.
Acknowledgements
The authors would like to thank the following International Liaison Committee on Resuscitation Neonatal Life Support Task Force members who provided input to the review protocol, interpretation of the results and on the manuscript as experts in neonatal resuscitation.
Dr. Charles Roehr. University of Oxford, John Radcliffe Hospital, Oxford, UK.
Dr. Chris McKinlay. University of Auckland, Auckland, New Zealand.
Dr. Daniele Trevisanuto. University of Padua, Padua, Veneto, Italy.
Dr. Edgardo Szyld. University of Oklahoma, Oklahoma City, OK, USA.
Dr. Gary Weiner. University of Michigan, Ann Arbor, Michigan, USA.
Dr. Georg Schmölzer. University of Alberta, Edmonton, Alberta, Canada.
Dr. Han-Suk Kim. Seoul National University College of Medicine, Seoul, Korea.
Dr. Helen C. Liley. University of Queensland. South Brisbane, Queensland, Australia.
Dr. Jonathan Wyllie. James Cook University Hospital, Middlesbrough, UK.
Dr. Jorge Farbes. P. Universidad Catolica de Chile, Santiago, Chile.
Dr. Jeffrey Perlman. Weill Medical College, New York, NY, USA.
Dr. Khalid Aziz. Royal Alexandria Hospital, Edmonton, Alberta, Canada.
Dr. Lindsay Mildenhall. Middlemore Hospital, Auckland, New Zealand.
Dr. Maria Fernanda de Almeida. Federal University of Sao Paulo, Sao Paulo, SP Brazil.
Dr. Myra H. Wyckoff. University of Texas Southwestern Medical Center, Dallas, TX, USA.
Dr. Ruth Guinsburg. Federal University of Sao Paulo, Sao Paulo, SP Brazil.
Dr. Shigeharu Hosono. Jichi Medical University Saitama Medical Center, Saitama, Japan.
Dr. Sithembiso Velaphi. Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa.
Dr. Tetsuya Isayama. National Center for Child Health and Development, Tokyo Japan.
Dr. Vishal S. Kapadia. University of Texas Southwestern Medical Center, Dallas, TX, USA.
Dr. Yacov Rabi. Foothills Medical Center, Calgary, Alberta, Canada.
Appendix 1 PICOST term definitions
Neonate: a newborn baby up to 28 days of age.
Resuscitation: support provided at birth to consist of a minimum of positive pressure support of breathing (PEEP or breaths given via mask, supraglottic airway device or tracheal tube).
Briefing: an act or instance of giving precise instructions or essential information12 (source: Merriam-Webster medical dictionary).
Debriefing: discussions of actions and thought processes after an event to promote reflective learning and improve clinical performance.13
Simulation: an artificial representation of a real-world process to achieve educational goals through experiential learning.
Healthcare professionals: staff employed by a healthcare organization, who deliver resuscitation (as defined above) to neonates.
Appendix 2 Search Strategy
The following databases were searched: PubMed, Embase, Web of Science and Cochrane Library. The searches were carried out on the 26th November 2019 and updated on the 27th January 2020.
All dates up to the 27th January 2020 were included in the search.
PUBMED:
(“infant, newborn” [mesh] OR infant* [tw] OR preterm [tw] OR preemie* [tw] OR newborn* [tw] OR neonat* [tw]) AND (“resuscitation” [mesh] OR resuscitat* [tw] OR cpr [tw]) AND (“critical reflection” [tw] OR reflection [tw] OR “post simulation” [tw] OR “pre briefing” [tw] OR prebrief* [tw] OR debrie* [tw] OR brief [tw] OR briefing [tw] OR “after action review” [tw] OR feedback [tw] OR “communication” [mesh]) AND (English [lang] OR English Abstract[ptyp]).
EMBASE:
('newborn'/exp OR 'newborn' OR infant*:ti,kw,ab OR preterm:ti,kw,ab OR preemie*:ti,kw,ab OR newborn*:ti,kw,ab OR neonat*:ti,kw,ab) AND ('resuscitation'/exp OR 'resuscitation' OR resuscitat*:ti,kw,ab OR cpr:ti,kw,ab) AND ('interpersonal communication'/exp OR 'interpersonal communication' OR 'debriefing'/exp OR 'debriefing' OR 'critical reflection':ti,kw,ab OR 'reflection'/exp OR 'reflection' OR reflection:ti,kw,ab OR 'post simulation':ti,kw,ab OR 'pre briefing':ti,kw,ab OR prebrief*:ti,kw,ab OR debrie*:ti,kw,ab OR brief:ti,kw,ab OR briefing:ti,kw,ab OR 'after action review':ti,kw,ab OR feedback:ti,kw,ab) AND ([embase]/lim OR [embase classic]/lim).
WEB OF SCIENCE:
(infant* OR preterm OR preemie* OR newborn* OR neonat*) AND (resuscitat* OR cpr) AND (“critical reflection” OR reflection OR “post simulation” OR “pre briefing” OR prebrief* OR debrie* OR brief OR briefing OR “after action review” OR feedback).
COCHRANE LIBRARY:
(infant* OR preterm OR preemie* OR newborn* OR neonat*) AND (resuscitat* OR cpr) AND (communicat* OR “critical reflection” OR reflection OR “post simulation” OR “pre briefing” OR prebrief* OR debrie* OR brief OR briefing OR “after action review” OR feedback).
Appendix 3 Excluded studies
| Study | Reason for Exclusion |
|---|---|
| Halamek L, Cady R, Sterling M. Using briefing, simulation and debriefing to improve human and system performance. Semin Perinatol Aug 10 2019;():151178 | Wrong study design |
| Halamek L. The simulated delivery-room environment as the future modality for acquiring and maintaining skills in fetal and neonatal resuscitation. Semin Fetal Neonatal Med Dec 2008;13(6):448−53 | |
| Finan, E.; Aylward, D.; Aziz, K. et al. Neonatal resuscitation guidelines update: A case-based review. Paediatrics and Child Health 2011;16(5):289−291 | |
| Cheng A, Nadkarni V, Vinay M. et al. Resuscitation Education Science: Educational Strategies to Improve Outcomes From Cardiac Arrest: A Scientific Statement From the American Heart Association. Circulation Aug 7 2018;138(6):E82–E122 | |
| De Garmo N, Rodriguez N, Amer M, Wang E. Simulation in neonatal resuscitation. Dis Mon Dec 2011;57(12):775−9 | |
| Lemoine J. Daigle S. Neonatal resuscitation simulation: improving safety while enhancing confidence and competence. Nurs Womens Health Apr 2010;14(2):143−5 | |
| Patricia K, Arnold J, Lemke D. Rapid Cycle Deliberate Practice: Application to Neonatal Resuscitation. MedEdPORTAL Jan 30 2017;13():10534 | |
| Kalaniti K. In situ simulation: Let's work, practice and learn together. Acta Paediatrica, International Journal of Paediatrics 2014;103(12):1219−1220 | |
| Greer, J. A.; Haischer-Rollo, G.; Delorey, D.; Kiser, R.; Sayles, T.; Bailey, J.; Blosser, C.; Middlebrooks, R.; Ennen, C. S. In-situ Interprofessional Perinatal Drills: The Impact of a Structured Debrief on Maximizing Training While Sensing Patient Safety Threats. Cureus Feb 19 2019;11(2):e4096 | Wrong comparator |
| Finer, N.; Rich, W. Neonatal resuscitation for the preterm infant: Evidence versus practice. Journal of Perinatology 2010;30(SUPPL. 1):S57-S66 | |
| Cheng A, Hunt E, Donoghue A. Examining pediatric resuscitation education using simulation and scripted debriefing: a multicenter randomized trial. JAMA Pediatr Jun 2013;167(6):528−36 | |
| den Boer M, Houtlosser M, Foglia E. et al. Benefits of recording and reviewing neonatal resuscitation: the providers' perspective. Arch Dis Child Fetal Neonatal Ed Sep 2019;104(5):F528–F534 | |
| Palmer E, Labant A, Edwards T, Boothby J. A Collaborative Partnership for Improving Newborn Safety: Using Simulation for Neonatal Resuscitation Training. J Contin Educ Nurs Jul 1 2019;50(7):319−324 | |
| Nadler I, Sanderson P, Van Dyken C, Davis, P, Liley, H. Presenting video recordings of newborn resuscitations in debriefings for teamwork training. BMJ Qual Saf 2011;20():163–169 | |
| Sawyer T, Sierocka-Castaneda A, Chan, D, et al. The effectiveness of video-assisted debriefing versus oral debriefing alone at improving neonatal resuscitation performance: a randomized trial. Simul Healthc Aug 2012;7(4):213−21 | |
| Gonzalez, A. B.; Farner, R. C.; Vasquez, M. M. Evaluating the need for a delivery room checklist in extremely low birth weight deliveries via simulation. Journal of Investigative Medicine 2019;67(2):519 | Abstract only |
| Hodgson, K.; Vawser, T.; Gilbert, S.; Sokol, J. Rapid cycle deliberat practice compared with immersive simulation and standard debriefing for neonatal simulation-based education. J Paediatr Child Health 2017;53():45 | |
| Campbell, D. M.; Finan, E. Impact of video-debriefing following simulated neonatal resuscitation in inter-professional teams. Paediatrics and Child Health (Canada) 2014;19(6):e88 | |
| Davies L, Osano B, Lewis A. et al. Qualitative mid-term evaluation of a maternal, newborn and child health training and research capacity building program in Kenya. Annals of Global Health 2015;81(1):144 | |
| Safety M, LeVan J, Gonzaba G, et al. Utilizing rapid cycle deliberate practice simulation to improve nicu resuscitation. Pediatrics 2019;144(2): | |
| LeVan J.; Gonzaba G.; Solis S.; Seitz R. Comparison of rapid cycle deliberate practice vs traditional simulation education regarding team preparedness and time to intervention in NICU emergencies. Pediatrics 2019;144(2): | |
| Ska˚re C, Kramer-Johansen, J, Calisch T, et al. Video based debriefing improves neonatal resuscitation. Resuscitation 2015;96():35−36 | |
| Shivananda S, Silenzi L. Effect of facilitating identification of roles on team performance during emergency neonatal resuscitation (NR). Paediatrics and Child Health 2011;16():28A | |
| Lee G, Hyde T, Patel D, Watts T. Quality of care of the preterm infant project - A multidisciplinary approach to service improvement. Archives of Disease in Childhood: Fetal and Neonatal Edition 2011;96():Fa47–Fa48 | |
| Wood A, Delaney C. Rosenberg A, Barry J. Delivery room education during a nicu rotation improves resuscitation skills. Acad Pediatr 2010;10(4):e7 | |
| Lai A, Bennett L. Improving confidence in neonatal resuscitation skills in residents in the NICU and newborn nursery. Acad Pediatr 2018;18(5):e51 | |
| NCT. Evaluation of Two Strategies for Debriefing in the Development of Skills for Neonatal Resuscitation. https://clinicaltrials.gov/show/NCT03606278 2018;(): | |
| Amin H, Singhal N, Beran T, Use of simulation-based skill acquisition instruction (SSAI) for manual mask ventilation (MMV) improves the ability of neonatal resuscitation program (NRP) providers to deliver and retain effective MMV skills. Paediatrics and Child Health (Canada) 2018;23():e48 | |
| Taylor A, Lewis P, Nugent M, Montague J, Mitra S. Improving safety at the very beginning: A novel neonatal delivery safety checklist. Arch Dis Child 2018;103():A88–A89 | |
| Pennaforte T, Lizotte M, Barrington K, et al. Death during simulation: Is auto-feedback accurate compared to providers' or parents' evaluations? J Pain Symptom Manage 2016;52(6):e140–e141 | |
| Finer, N. N.; Rich, W. Neonatal resuscitation: toward improved performance. Resuscitation Apr 2002;53(1):47−51 | Wrong intervention |
| Cordero L, Hart B, Hardin R, et al. Deliberate practice improves pediatric residents' skills and team behaviors during simulated neonatal resuscitation. Clin Pediatr (Phila) Aug 2013;52(8):747−52 | |
| Brown T, Tu J, Profit J, et al. Optimal Criteria Survey for Preresuscitation Delivery Room Checklists. Am J Perinatol Jan 2016;33(2):203−7 | |
| Sawyer T, Sierocka-Castaneda A, Chan D, et al. Deliberate practice using simulation improves neonatal resuscitation performance. Simul Healthc Dec 2011;6(6):327−36 | |
| Lee J. Cheng T. In brief: Newborn resuscitation. Pediatrics in Review 2006;27(7):e52–e53 | |
| Kakkilaya V, Jubran I, Mashruwala V, et al. Quality Improvement Project to Decrease Delivery Room Intubations in Preterm Infants. Pediatrics Feb 2019;143(2): | |
| Baldoli, Ilaria; Tognarelli, An active simulator for neonatal intubation: Design, development and assessment. Medical Engineering & Physics Jan 2017;39():57−65 | |
| Talati A, Scott T, Barker B, Grubb P. Improving neonatal resuscitation in Tennessee: a large-scale, quality improvement project. J Perinatol Aug 15 2019;(): | |
| Skare, C.; Boldingh, A. M.; Kramer-Johansen, J.; Video performance-debriefings and ventilation-refreshers improve quality of neonatal resuscitation. Resuscitation Nov 2018;132():140−146 | |
| Balakrishna M, Falk-Smith N, Detman L, et al. Promoting teamwork may improve infant care processes during delivery room management: Florida perinatal quality collaborative's approach. J Perinatol Jul 2017;37(7):886−892 | |
| Chang C, Perlman, J. Anticipation and preparation for delivery room emergencies. Semin Fetal Neonatal Med Sep 23 2019;():101031 | Wrong outcomes |
| Bennett S, Finer N, Halamek L. Implementing Delivery Room Checklists and Communication Standards in a Multi-Neonatal ICU Quality Improvement Collaborative. Jt Comm J Qual Patient Saf Aug 2016;42(8):369−76 | |
| Mywtr R. Knowledge of the Nursing Team about Basic Life Support in Pre and Post-Qualification Babies. http://www.who.int/trialsearch/Trial2.aspx?TrialID=RBR-4mywtr 2017;(): 2017 | Study protocol |
| Szyld E, Szyld D, Self-directed Video Versus Instructor-based Neonatal Resuscitation Training. https://clinicaltrials.gov/show/NCT01847911 2013;(): |
References
- 1.International Liaison Committee on Resuscitation (ILCOR) Systematic Review on Debriefing of Resuscitation Performance (EIT #645), 2020. https://costr.ilcor.org/document/debriefing-of-resuscitation-performance-eit-645-systematic-review.
- 2.The Joint Commission . Sentinel Event Alert; 2004. Preventing Infant Death and Injury During Delivery; p. 30. https//www.jointcommission.org/assets/1/18/SEA_30.pdf. [PubMed] [Google Scholar]
- 3.Perlman J.M., Wyllie J., Kattwinkel J. Part 11: neonatal resuscitation: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122(16 Suppl 2):S516–S538. doi: 10.1161/CIRCULATIONAHA.110.97112. [DOI] [PubMed] [Google Scholar]
- 4.Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia, 2020. Available at www.covidence.org.
- 5.Preferred reporting items for systematic reviews and meta-analyses (PRISMA) diagram, Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal. pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Skåre C., Calisch T.E., Saeter E. Implementation and effectiveness of a video-based debriefing programme for neonatal resuscitation. Acta Anaesthesiol Scand. 2018;62(3):394–403. doi: 10.1111/aas.13050. [DOI] [PubMed] [Google Scholar]
- 7.van der Heide P.A., van Toledo-Eppinga L., van der Heide M., van der Lee J.H. Assessment of neonatal resuscitation skills: a reliable and valid scoring system. Resuscitation. 2006;71:212–221. doi: 10.1016/j.resuscitation.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 8.Sauer C.W., Boutin M.A., Fatayerji A.N., Proudfoot J.A., Fatayerji A.N.I., Golembeski D.J. Delivery room quality improvement project improved compliance with best practices for a community NICU. Sci Rep. 2016;6:37397. doi: 10.1038/srep37397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katheria A., Rich W., Finer N. Development of a strategic process using checklists to facilitate team preparation and improve communication during neonatal resuscitation. Resuscitation. 2013;84(11):1552–1557. doi: 10.1016/j.resuscitation.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 10.Magee M.J., Farkouh-Karoleski C., Rosen T.S. Improvement of immediate performance in neonatal resuscitation through rapid cycle deliberate practice training. J Grad Med Educ. 2018;10(2):192–197. doi: 10.4300/JGME-D-17-00467.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lockyer J., Singhal N., Fidler H., Weiner G., Aziz K., Curran V. The development and testing of a performance checklist to assess neonatal resuscitation megacode skill. Pediatrics. 2006;118(December (6)):e1739–e1744. doi: 10.1542/peds.2006-0537. [DOI] [PubMed] [Google Scholar]
- 12.Merriam-Webster. (n.d.). Briefing. In Merriam-Webster.com dictionary. Retrieved June 7, 2020, from https://www.merriam-webster.com/dictionary/briefing.
- 13.Sawyer T., Loren D., Halamek L.P. Post-event debriefings during neonatal care: why are we not doing them, and how can we start? J Perinatol. 2016;36(6):415–419. doi: 10.1038/jp.2016.42. [DOI] [PubMed] [Google Scholar]