Abstract
Aims
Many countries reported an increase of out-of-hospital cardiac arrests (OHCAs) and mortality during the COVID-19 pandemic. However, all these data refer to regional settings and national data are still missing. We aimed to assess the OHCA incidence and population mortality during COVID-19 pandemic in whole Switzerland and in the different regions (Cantons) according to the infection rate.
Methods
We considered OHCAs and deaths which occurred in Switzerland after the first diagnosed case of COVID-19 (February 25th) and for the subsequent 65 days and in the same period in 2019. We also compared Cantons with high versus low COVID-19 incidence.
Results
A 2.4% reduction in OHCA cases was observed in Switzerland. The reduction was particularly high (−21.4%) in high-incidence COVID-19 cantons, whilst OHCAs increased by 7.7% in low-incidence COVID-19 cantons. Mortality increased by 8.6% in the entire nation: a 27.8% increase in high-incidence cantons and a slight decrease (−0.7%) in low-incidence cantons was observed. The OHCA occurred more frequently at home, CPR and AED use by bystander were less frequent during the pandemic. Conversely, the OHCAs percentage in which a first responder was present, initiated the CPR and used an AED, increased. The outcome of patients in COVID-19 high-incidence cantons was worse compared to low-incidence cantons.
Conclusions
During the COVID-19 pandemic in Switzerland mortality increased in Cantons with high-incidence of infection, whilst not in the low-incidence ones. OHCA occurrence followed an opposite trend showing how variables related to the health-system and EMS organization deeply influence OHCA occurrence during a pandemic.
Keywords: Out-of-hospital cardiac arrest, Mortality, COVID-19, Switzerland
Introduction
Many countries affected by SARS-CoV-2 reported a major increase in mortality compared to the same period of the previous years. The percentage of excess death ranged from +38.7% in Italy to +111.9% in New York City.1, 2 Part of the deaths have been attributed to out-of-hospital cardiac arrests (OHCAs). An increase in OHCAs has been identified in Northern Italy, in the Paris area in France, in London in the UK and in New York City in the U.S.A.3, 4, 5, 6, 7, 8 The increased incidence in cardiac arrests may be related to the virus infection, but also to the collateral damages caused by the pandemic in challenging the health-care system whilst handling emergencies.6 In an effort to contain the virus spread, lockdown and restriction movement imposed by governments,9 as well as the postponement of non-urgent medical consultations and interventions,10 as requested by national medical authorities, have profoundly affected patients’ care. The social distancing of vulnerable groups of aged individuals, possibly on a single household, may have ultimately resulted in a lack of hospitalization and death before the arrival of emergency medical service (EMS) at the onset of symptoms or worsening thereof, as well as in a reduction of witnessed OHCA with delayed alarm,6 and lack of bystander cardiopulmonary resuscitation (CPR) manoeuvre initiation because of fear of infection.11 As recently highlighted by Perkins and Couper, the long-term effects of COVID-19 on the community response to cardiac arrest, may result in a reduction in OHCA survival.12
A large variation in the OHCA incidence has been reported in urban regions of Paris, which contrasted the overall uniform increase in OHCA incidence in Northern Italy and in New York City. These findings conflict with very recent data from Seattle & King County in the USA which show an unchanged number of EMS treated OHCA when comparing the pandemic period to the previous years.13
Data regarding OHCA incidence and the COVID-19 infection so far, refer to regional settings or urban areas with high-density population. It is unknown whether patients’ characteristics, circumstances of OHCA occurrence and management by EMS was affected by the COVID-19 pandemic on a national basis. Furthermore, an analysis of OHCA in regions with different incidence of COVID-19 infection may help to better understand the disease management and, possibly, develop counteractions to be adopted during possible recurrent outbreaks.
In this study, we assessed the OHCA incidence and population mortality in Switzerland during the COVID-19 pandemic, compared with the 2019 non-pandemic period. We also analyzed regional (Cantonal) differences in population mortality and the COVID-19 reported infection rate, comparing regions with high versus low COVID-19 incidence, with specific attention to age groups.
Methods
Study design and participants
This population-based, observational study is reported according to the strengthening of the reporting of observational studies in epidemiology guidelines. We considered the OHCAs and the number of deaths which occurred in the Swiss Confederation after the first case of COVID-19 was diagnosed in Switzerland (February 25th, 2020) and for the subsequent 65 days (until to April 30th). OHCA data were retrieved from the Swiss Registry of Cardiac Arrest (SWISSRECA), whilst death data and population data were retrieved from the Federal Statistical Office of the Swiss Confederation.14 We also computed data for the same time period in 2019.
SWISSRECA is a long-term, web-based, multi-center cardiac arrest registry set up by the Interassociation for Rescue Services (IVR-IAS) at the end of 2018, which collects OHCAs of every etiology occurring in the whole of the Switzerland, irrespective of whether resuscitation was attempted or not (mandatory registration). Data were collected using Utstein templates.15 SWISSRECA is approved by Swissethics (ID-2016-01844) and IVR-IAS is responsible for its maintenance. No additional informed consent was required.
Emergency Medical System (EMS) description and adaptation to the COVID-19 outbreak
In Switzerland (8.57-million inhabitants), OHCAs are managed by local EMS, a two-tiered response system, coordinated via a cantonal dispatch center (unchanged during the pandemic): the first tier consists of paramedics who can provide advanced life support, the second tier is made up of teams (ambulance or helicopter) with an emergency physician, alerted if required. Paramedics are instructed to initiate resuscitation unless clear signs of death are present or in case of a Do Not Attempt Resuscitation order. The decision to stop resuscitation and the death declaration are based on the physician’s clinical judgment. During the COVID-19 pandemic, the EMS personnel was instructed to wear personal protective equipment (such as face shields, protective glasses, N95 face masks and isolation gowns), before initiating resuscitation attempts.
In some cantons, there is a network of first responders (FR), made up of off-duty EMS personnel, fire-fighters, police and laypeople trained in CPR, who are alerted via a mobile application and can provide basic life support and use an automatic external defibrillator (AED). However, the organization and the type of first-responders involved are locally defined and may differ among Swiss Cantons. The FR activation during the COVID-19 pandemic, has been amended in a number of manners according to local choices. In some Cantons the activation of all the FR types was maintained, but whilst using modified protocols; in other Cantons lay FR were de-activated. Finally, in a few Cantons the FR network was completely deactivated.
The COVID-19 outbreak at Swiss cantonal level
The daily new cases and the cumulative incidence of COVID-19 (defined as cases with positive reverse transcription polymerase chain reaction tests of SARS-CoV-2), were computed from the Federal Office of Public Health of Swiss Confederation.16
The 26 Swiss cantons (number of inhabitants, surface area, and population density of each Canton are indicated in the Annexed Table A), were grouped according to the national average cumulative incidence (352.4 cases) of COVID-19 cases per 100,000 inhabitants as recorded on May 7th, 2020. Eight cantons were high-incidence cantons with 608.9 cases (IQR 373.6–934.5 cases) per 100,000 inhabitants, and the remaining 18 Cantons (low-incidence cantons) had 191.6 cases per 100,000 inhabitants (IQR 147.7–236.8 cases). No data regarding the number of OHCA patients suspected or diagnosed for COVID-19 were available.
Statistical analysis
We present categorical variables as counts and percent; we computed the difference in percentage between 2020 and 2019 along with its 95% confidence interval (CI), using a binomial regression model with identity link. We present continuous variables using the median and 25th–75th percentiles; we computed the difference in medians and 95%CI using quantile regression. We computed the Spearman R and its 95%CI to measure the strength of the correlation of difference in cumulative incidence in OHCAs between 2020 and 2019 per 100,000 inhabitants, and COVID-19 cumulative incidence per 100,000 inhabitants for the Cantons with high- and low-incidence of COVID-19. We report the 2020 change in mortality and OHCA cumulative incidence with respect to 2019, together with its 95% binomial exact CI. The statistical analyses were performed with Stata software (version 16, StataCorp, USA). All tests were 2-sided and a p-value below 0.05 was considered statistically significant.
Results
Overall, 933 and 911 OHCAs occurred in the 2019 and 2020 study period, respectively representing 0.069% and 0.062% of the total mortality recorded in the same period. Patient characteristics and circumstances of OHCA occurrence are reported in Table 1. The median age, gender and etiology of cardiac arrests were similar in 2019 and 2020. In contrast, during the pandemic, OHCA location was significantly more frequent at home, a bystander CPR was less frequently started and an AED was less frequently used. Conversely, there was an increase in the percentage of OHCAs in which a first responder was present on the scene, initiated CPR and used an AED before EMS arrival (Table 1).
Table 1.
Comparison between patients’ and OHCAs’ characteristics in the period 2019–2020.
| Variable | 2020 | 2019 | Differencea | p |
|---|---|---|---|---|
| n = 911 | n = 933 | |||
| Males, n (%) | 623 (68.4) | 636 (68.2) | 0.2 (95%CI, −4 to 4) | 0.92 |
| Age, years [IQR] | 70 [56−80] | 71 [58−82] | −1 (95%CI, −3.01 to 1.01) | 0.33 |
| EMS arrival time, min [IQR] | 10 [7–14] | 10 [7–15] | 0 (95%CI, −0.8 to 0.8) | 1 |
| Etiology of arrest, n (%) | ||||
| Medical | 774 (85) | 761 (81.6) | 3.4 (95%CI, −0.1 to 7) | 0.5 |
| Trauma | 84 (9.2) | 98 (10.5) | −1 (95%CI, −4 to 1) | 0.35 |
| Drowning | 4 (0.4) | 9 (1) | −0.6 (95%CI, −1 to 0.4) | 0.17 |
| Overdose | 18 (2) | 33 (3.5) | −1.5 (95%CI, −3 to −0.2) | 0.04 |
| Electrocution | 2 (0.2) | 3 (0.3) | −0.1 (95%CI, −1 to 0.4) | 0.67 |
| Asphyxial (external causes) | 29 (3.2) | 29 (3.1) | 0.1 (95%CI, −2 to 2) | 0.93 |
| OHCA location, n (%) | ||||
| Home | 633 (71.4) | 598 (66.6) | 4.8 (95%CI, 0.1 to 9) | 0.03 |
| Nursing residence | 35 (3.9) | 29 (3.2) | 0.7 (95%CI, −1 to 2) | 0.4 |
| Workplace | 21 (2.4) | 32 (3.6) | −1.2 (95%CI, −3 to 0.3) | 0.136 |
| Street | 112 (12.6) | 121 (13.5) | −1 (95%CI, −4 to 2) | 0.59 |
| Public building | 56 (6.3) | 71 (7.9) | −2 (95%CI, −4 to 1) | 0.19 |
| Sport | 30 (3.4) | 47 (5.2) | −1.8 (95%CI, −4 to 0.1) | 0.054 |
| Witnessed status, n (%) | ||||
| Unwitnessed | 452 (53.3) | 462 (52.1) | 1.2 (95%CI, −4 to 6) | 0.6 |
| Bystander witnessed | 318 (37.5) | 343 (38.7) | −1.2 (95%CI, −6 to 3) | 0.6 |
| Witnessed by EMS | 75 (8.8) | 77 (8.7) | 0.1 (95%CI, −3 to 3) | 0.9 |
| Resuscitation attempted by EMS, n (%) | 564 (61.9) | 558 (59.8) | 2.1 (95%CI, −2 to 7) | 0.35 |
| Bystander CPR, n (%)b | 282 (56.5) | 309 (62.8) | −6.3 (95%CI, −12 to −0.2) | 0.04 |
| AED used by bystander, n (%)b | 43 (8.6) | 64 (13) | −4.4 (95%CI, −8 to −1) | 0.03 |
| Presence of first responder, n (%)b | 179 (35.9) | 132 (26.8) | 9.1 (95%CI, 3 to 15) | 0.002 |
| Minutes to FR arrival, min [IQR]b | 4 [1–8] | 3 [1–7] | 1 (95%CI, −0.04 to 2.04) | 0.06 |
| CPR initiated by FR, n (%)b | 139 (27.9) | 101 (20.5) | 7.4 (95%CI, 2 to 13) | 0.007 |
| AED used by FR, n (%)b | 85 (17) | 61 (12.4) | 4.6 (95%CI, 0.4 to 9) | 0.04 |
| Shockable presenting rhythm, n (%)c | 188 (33.3) | 174 (31.2) | 2.1 (95%CI, −3 to 8) | 0.44 |
| Minutes to ROSC, min [IQR]c | 28 [19−37] | 25 [18−40] | 3 (95%CI, −0.5 to 6.5) | 0.09 |
| Outcome, n (%)c | ||||
| Death in the field | 356 (64.1) | 343 (62.1) | 2 (95%CI, −4 to 8) | 0.49 |
| Transported with ongoing CPR | 45 (8.1) | 43 (7.8) | 0.3 (95%CI, −3 to 4) | 0.84 |
| Transported with ROSC | 154 (27.7) | 166 (30.1) | −2.4 (95%CI, −8 to 3) | 0.39 |
EMS: emergency medical service; OHCA: out-of-hospital cardiac arrest; CPR: cardio-pulmonary resuscitation; FR: first responder; AED: automatic external defibrillator; ROSC: return of spontaneous circulation.
Differences are expressed as rate difference or median difference and 95% confidence interval.
Among those in whom resuscitation was attempted by EMS and excluding those witnessed by EMS.
Among those in whom resuscitation was attempted by EMS.
Cantonal differences in OHCA characteristics, circumstances and outcome
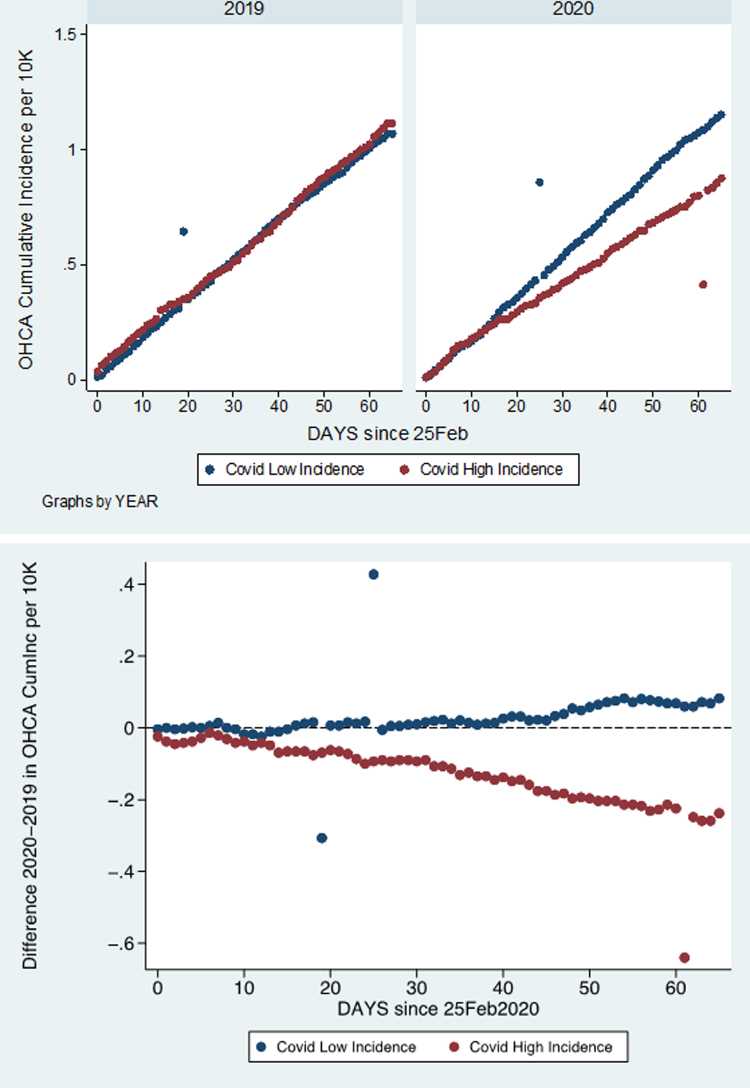
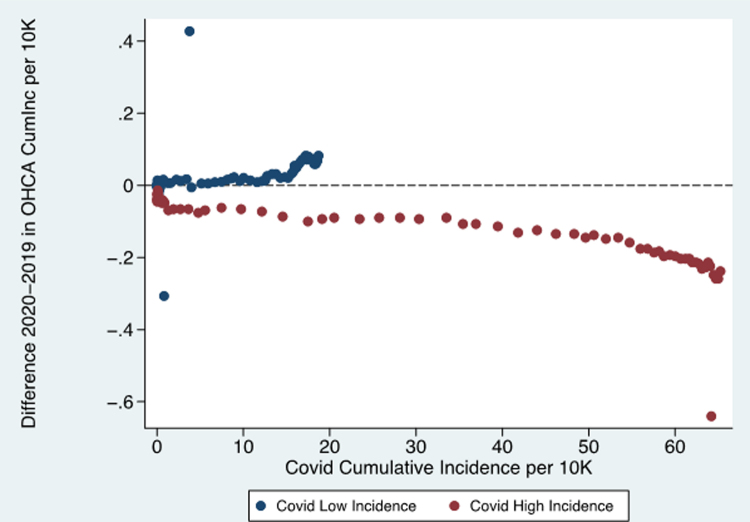
In 2019, the OHCA cumulative incidence per 100,000 inhabitants was very similar in high-incidence and low-incidence Cantons, but diverged in the year 2020 (Fig. 1). During the pandemic, there was a progressive decrease in the difference in OHCA incidence (per 100,000 inhabitants) between 2020 and 2019 in high-incidence Cantons (Pearson correlation coefficient between difference and days −0.84, 95%CI −0.89 to −0.79), whereas there was a progressive, though modest, increase in the difference in OHCA incidence (per 100,000 inhabitants) for low-incidence Cantons (Pearson correlation coefficient between difference and days 0.38, 95%CI 0.23–0.52) (Fig. 1). As shown in Fig. 2, in cantons with high-incidence of COVID-19, there was a strong correlation between the COVID-19 incidence (per 100’000 inhabitants) and the difference in OHCA incidence (per 100’000 inhabitants) observed between 2020 and 2019 (Pearson's product-moment correlation coefficient −0.81, 95%CI −0.88 to −0.7). In contrast, in those cantons with low-incidence of COVID-19, this correlation was significantly weaker (Pearson’s product-moment correlation coefficient 0.38, 95%CI 0.15 to 0.57).
Fig. 1.
OHCA cumulative incidence per 100,000 inhabitants in high-incidence and low-incidence of COVID-19 Cantons in the first 65 days of the pandemic in 2020 and in the same period of 2019 (upper panel). Difference 2020–2019 in OHCA cumulative incidence per 100,000 inhabitants in high-incidence and low-incidence of COVID-19 Cantons in the first 65 days of the pandemic in 2020 and in the same period of 2019 (lower panel).
Fig. 2.
Association between the difference in OHCA cumulative incidence per 100,000 inhabitants between 2020 and 2019 periods and COVID-19 cumulative incidence per 100,000 inhabitants in high-incidence and low-incidence of COVID-19 Cantons.
There was no difference in OHCA characteristics and circumstances in cantons with high- and low-incidence of COVID-19 infection in 2020 (Supplemental Table B). Despite this fact, the outcome of patients in those cantons with high-incidence of COVID-19 was worse. Cantons with high-incidence of COVID-19 reported a higher number of deaths in field (70.2% versus 61.7%, p = 0.05), and a lower number of patients (21.7% versus 30.2%, p = 0.03) transported with a spontaneous circulation to the hospital (Supplemental Table B).
The comparison of the OHCA characteristics occurring in the 2019 and the 2020 period, showed some differences (Table 2, Table 3) in both low- and in high-incidence of COVID-19. In cantons with low-incidence of COVID-19 (Table 2), etiology of cardiac arrest increased for medical causes but decreased for overdose, and the first responders’ arrival took longer than in the year 2019, whilst a lower proportion of bystanders used an AED; finally, resuscitation was attempted more frequently by EMS personnel. In those cantons with high-incidence of COVID-19, there were marginal differences. The OHCA location was less frequent during sport and leisure activities, first responders were more frequently on the scene and initiated CPR.
Table 2.
Comparison of patients’ and OHCAs’ characteristics in low-incidence of COVID-19 cantons in the period 2019–2020.
| Variable | Low-incidence | Low-incidence | Differencea | p |
|---|---|---|---|---|
| 2020 | 2019 | |||
| n = 657 | n = 610 | |||
| Males, n (%) | 445 (67.7) | 413 (67.7) | 0 (95%CI, −5 to 5) | 0.99 |
| Age, years [IQR] | 70 [56−80] | 72 [59−82] | −2 (95%CI, −4.46 to 0.46) | 0.11 |
| EMS arrival time, min [IQR] | 10 [7–14] | 10 [7–14] | 0 (95%CI, −8 to 8) | 1 |
| Etiology of arrest, n (%) | ||||
| Medical | 564 (85.8) | 497 (81.5) | 4.3 (95%CI, 0.2 to 8) | 0.04 |
| Trauma | 59 (9) | 63 (10.3) | −1.4 (95%CI, −5 to 2) | 0.42 |
| Drowning | 3 (0.5) | 5 (0.8) | −0.3 (95%CI, −1 to 1) | 0.4 |
| Overdose | 12 (1.8) | 25 (4.1) | −2.3 (95%CI, −4 to −0.3) | 0.02 |
| Electrocution | 2 (0.3) | 2 (0.3) | 0 (95%CI, −1 to 1) | 0.94 |
| Asphyxial (external causes) | 17 (2.6) | 18 (2.9) | −0.3 (95%CI, −2 to 1) | 0.7 |
| OHCA location, n (%) | ||||
| Home | 457 (71.5) | 398 (68.3) | 3.2 (95%CI, −2 to 8) | 0.22 |
| Nursing residence | 23 (3.6) | 16 (2.7) | 1.1 (95%CI, −1 to 3) | 0.39 |
| Workplace | 19 (3) | 23 (3.9) | −0.9 (95%CI, −3 to 1) | 0.35 |
| Street | 79 (12.4) | 81 (13.9) | −1.5 (95%CI, −5 to 2) | 0.43 |
| Public building | 40 (6.3) | 43 (7.4) | −0.9 (95%CI, −4 to 2) | 0.44 |
| Sport | 21 (3.3) | 22 (3.8) | −0.5 (95%CI, −3 to 2) | 0.64 |
| Witnessed status, n (%) | ||||
| Unwitnessed | 338 (54.7) | 322 (55.5) | −0.8 (95%CI, −6 to 5) | 0.77 |
| Bystander witnessed | 222 (35.9) | 216 (37.2) | −1.3 (95%CI, −7 to 4) | 0.64 |
| Witnessed by EMS | 56 (9.1) | 41 (7.1) | 2 (95%CI, −1 to 5) | 0.2 |
| Resuscitation attempted by EMS, n (%) | 403 (61.3) | 339 (55.6) | −5.7 (95%CI, 0.2 to 11) | 0.04 |
| Bystander CPR, n (%)b | 201 (57.1) | 194 (63.8) | −6.7 (95%CI, −14 to 1) | 0.08 |
| AED used by bystander, n (%)b | 30 (8.5) | 50 (16.4) | −7.9 (95%CI, −13 to −3) | 0.002 |
| Presence of first responder, n (%)b | 125 (35.5) | 87 (28.6) | 6.9 (95%CI, −0.1 to 14) | 0.06 |
| Minutes to FR arrival, min [IQR]b | 5 [1–9] | 3 [1–7] | 2 (95%CI, 0.5 to 3.5) | 0.009 |
| CPR initiated by FR, n (%)b | 95 (27) | 63 (20.7) | 6.3 (95%CI, −0.1 to 13) | 0.06 |
| AED used by FR, n (%)b | 60 (17) | 42 (13.8) | 3.2 (95%CI, −2 to 9) | 0.25 |
| Shockable presenting rhythm, n (%)c | 143 (35.5) | 115 (33.9) | 1.6 (95%CI, −5 to 8) | 0.66 |
| Minutes to ROSC, min [IQR]c | 29 [20−37] | 25.5 [18−40] | 3.5 (95%CI, −1.3 to 7.3) | 0.17 |
| Outcome, n (%)c | ||||
| Death in the field | 243 (61.7) | 204 (60.9) | 0.8 (95%CI, −6 to 8) | 0.83 |
| Transported with ongoing CPR | 45 (8.1) | 43 (7.8) | 0.3 (95%CI, −4 to 4) | 0.86 |
| Transported with ROSC | 119 (30.2) | 105 (31.3) | −1.1 (95%CI, −8 to 6) | 0.74 |
EMS: emergency medical service; OHCA: out-of-hospital cardiac arrest; CPR: cardio-pulmonary resuscitation; FR: first responder; AED: automatic external defibrillator; ROSC: return of spontaneous circulation.
Differences are expressed as rate difference or median difference and 95% confidence interval.
Among those in whom resuscitation was attempted by EMS and excluding those witnessed by EMS.
Among those in whom resuscitation was attempted by EMS.
Table 3.
Comparison of patients’ and OHCAs’ characteristics in high-incidence of COVID-19 cantons in the period 2019–2020.
| Variable | High-incidence | High-incidence | Differencea | p |
|---|---|---|---|---|
| 2020 | 2019 | |||
| n = 254 | n = 323 | |||
| Males, n (%) | 178 (70.1) | 223 (69) | 1.1 (95%CI, −7 to 9) | 0.79 |
| Age, years [IQR] | 71 [58−81] | 71 [57−81] | 0 (95%CI, −4.1 to 4.1) | 1 |
| EMS arrival time, min [IQR] | 10 [7–13] | 10 [7–15] | 0 (95%CI, −0.9 to 0.9) | 1 |
| Etiology of arrest, n (%) | ||||
| Medical | 210 (82.7) | 264 (81.7) | 1 (95%CI, −5 to 7) | 0.77 |
| Trauma | 25 (9.8) | 35 (10.8) | −1 (95%CI, −5 to 2) | 0.42 |
| Drowning | 1 (0.4) | 4 (1.2) | −0.8 (95%CI, −2 to 1) | 0.25 |
| Overdose | 6 (2.4) | 8 (2.5) | −0.1 (95%CI, −3 to 2) | 0.93 |
| Electrocution | 0 (0) | 1 (0.3) | – | |
| Asphyxial (external causes) | 12 (4.7) | 11 (3.4) | 1.3 (95%CI, −2 to 5) | 0.43 |
| OHCA location, n (%) | ||||
| Home | 176 (71) | 200 (63.5) | 6.5 (95%CI, −0.1 to 15) | 0.06 |
| Nursing residence | 12 (4.8) | 13 (4.1) | 0.7 (95%CI, −3 to 4) | 0.69 |
| Workplace | 2 (0.8) | 9 (2.9) | −2.1 (95%CI, −4 to 0.2) | 0.06 |
| Street | 33 (13.3) | 40 (12.7) | 0.6 (95%CI, −5 to 6) | 0.83 |
| Public building | 16 (6.4) | 28 (8.9) | −2.5 (95%CI, −7 to 2) | 0.28 |
| Sport | 9 (3.6) | 25 (7.9) | −4.3 (95%CI, −8 to −1) | 0.03 |
| Witnessed status, n (%) | ||||
| Unwitnessed | 114 (49.6) | 140 (45.7) | −3.9 (95%CI, −5 to 12) | 0.38 |
| Bystander witnessed | 96 (41.7) | 127 (41.5) | 0.2 (95%CI, −8 to 9) | 0.96 |
| Witnessed by EMS | 19 (8.3) | 36 (11.8) | −3.5 (95%CI, −9 to 2) | 0.17 |
| Resuscitation attempted by EMS, n (%) | 161 (63.4) | 219 (67.8) | −4.4 (95%CI, −12 to 3) | 0.27 |
| Bystander CPR, n (%)b | 81 (55.1) | 115 (61.2) | −6.1 (95%CI, −17 to 5) | 0.26 |
| AED used by bystander, n (%)b | 13 (8.8) | 14 (7.4) | 1.4 (95%CI, −5 to 7) | 0.64 |
| Presence of first responder, n (%)b | 54 (36.7) | 45 (23.9) | 12.8 (95%CI, 3 to 23) | 0.01 |
| Minutes to FR arrival, min [IQR]b | 4 [1–7] | 2.5 [1–6] | 1.5 (95%CI, −0.66 to 2.66) | 0.24 |
| CPR initiated by FR, n (%)b | 44 (29.9) | 38 (20.2) | 9.7 (95%CI, 0.3 to 19) | 0.04 |
| AED used by FR, n (%)b | 25 (17) | 19 (10.1) | 6.9 (95%CI, −1 to 14) | 0.07 |
| Shockable presenting rhythm, n (%)c | 45 (27.9) | 59 (26.9) | 1 (95%CI, −8 to 10) | 0.83 |
| Minutes to ROSC, min [IQR]c | 26.5 [16–35] | 25 [19–40] | 1.5 (95%CI, −4.4 to 8.4) | 0.54 |
| Outcome, n (%)c | ||||
| Death in the field | 113 (70.2) | 139 (64.1) | 6.1 (95%CI, −3 to 16) | 0.21 |
| Transported with ongoing CPR | 13 (8.1) | 17 (7.8) | 0.3 (95%CI, −5 to 6) | 0.93 |
| Transported with ROSC | 35 (21.7) | 61 (28.1) | −6.4 (95%CI, −15 to 2) | 0.15 |
EMS: emergency medical service; OHCA: out-of-hospital cardiac arrest; CPR: cardio-pulmonary resuscitation; FR: first responder; AED: automatic external defibrillator; ROSC: return of spontaneous circulation.
Differences are expressed as rate difference or median difference and 95% confidence interval.
Among those in whom resuscitation was attempted by EMS and excluding those witnessed by EMS.
Among those in whom resuscitation was attempted by EMS.
OHCA frequency and mortality according to age groups and incidence of the COVID-19 infection
A negligible reduction in OHCA cases, amounting to 2.4%, was observed in the entire nation. The reduction was particularly high (−21.4%) in those cantons with a high incidence of COVID-19; in contrast, OHCA cases increased by 7.7% in low-incidence COVID-19 cantons. In those cantons with high-incidence of COVID-19, the reduction in OHCA occurred in the age group 20–39 (−44.8%) and 65–79 (−36.6%), and less in the age group of 80 years and older (−17.5%) (Supplemental Table C).
Compared to the previous year, in 2020 overall mortality increased by 8.6% in Switzerland. A 27.8% increase in mortality in 2020 was observed in the high-incidence cantons when compared with the previous year, which contrasted with a slight decrease of 0.7% in low-incidence cantons. The mortality increase in high-incidence Cantons was evident in both the age group 65–79 years of age (+16.9%), and the 80 years of age and older (+37.6%) (Supplemental Table D).
Mortality and OHCA comparison between cantons with high-incidence and low-incidence of COVID-19 in 2020 is shown in Supplemental Table E. There was no difference in the median population density between Cantons with high-incidence of COVID-19 (206.24, IQR 95.5–1017.4) and those with low-incidence (240.03, IQR 93.5–348.1) (p = 0.82).
Discussion
Our study is the first one to report the OHCA incidence at national level during the peak period of the COVID-19 pandemic, which, in Switzerland, lasted nearly 9 weeks, as of February 25, 2020. Furthermore, this is the first study to compare OHCA incidence and overall mortality during the lockdown in an entire nation as well as in regions experiencing high- and low-incidence of COVID-19 infection.
In line with other European countries (Italy, The Netherlands, England, Wales, and Scotland) and densely the populated US cities (New York City, Seattle),1, 17 Switzerland also experienced an overall increase of the mortality rate during the COVID-19 pandemic compared to a similar period of the previous year. As expected, a relationship between increase in mortality and incidence of COVID-19 cases also occurred in our country. In fact, the mortality risk difference was 6.3 times higher in those cantons with a higher incidence of COVID-19 cases compared to cantons with a low incidence of COVID-19 cases. The overall increased mortality strongly contrasted with an unchanged number of OHCAs occurring within the peak period in Switzerland. Therefore our results conflict with the data for Italy, the UK and New York City, and in part with the French data3, 4, 5, 6, 7, 8; all regions in which a significant increase in OHCAs during the lockdown period was reported. However, during the last 2 weeks of the study period, there was a relative decrease in OHCA incidence in the Paris area, possibly due to an EMS reorganization allowing a progressively better response to non-COVID-19 related calls during the study period. Our findings are well in line with recent US data regarding Seattle & King County, and with those coming from the Victoria region in Australia, showing an unchanged number of OHCAs in 2020 compared to previous years.13, 18 A further confirmation that, at least in Switzerland, COVID-19 mortality and OHCA incidence were not directly associated is also shown by the progressive and constant decrease – week after week – of OHCA incidence only in those Swiss cantons with high incidence of COVID-19 cases. In contrast, OHCA incidence remained unchanged in those cantons with low incidence of COVID-19 cases. COVID-19 incidence in Switzerland (352 cases 1 per 100’000 inhabitants) was similar to the one in Seattle & King County (229 cases per 100’000 inhabitants)13 and both were much higher than in the Paris area (194 cases per 100’000 inhabitants)4 as well as in the Victoria region in Australia (159 cases per 100,000 inhabitants).18 On the other hand, these four geographies had a considerably lower COVID-19 incidence than Lombardy (956 cases per 100’000 inhabitants) and New York City (1868 cases per 100’000 inhabitants).6, 7 Altogether, these data suggest that countries with similar incidences of COVID-19 cases have different trends in OHCA incidence, thus resulting in a weak correlation, if any, between the COVID-19 cases and the OHCA incidence. Therefore, the mismatch between OHCA cases and overall mortality observed in Switzerland, as well as between OHCA cases and the incidence of COVID-19 cases is not surprising. Similarly, also the different trends in the OHCAs incidence in the different cantons is likely to recognize other causes than just the incidence rate of COVID-19 cases. Although it is difficult to understand the reasons for these differences with absolute certainty, some factors can be hypothesised.
The first point to be considered is represented by age, a non-modifiable factor in mortality and OHCA risk. During the pandemic, the risk of mortality linearly increased with age, it thus being the highest in the age-group 80 years and older; in particularly in cantons with high incidence of COVID-19 cases. This observation is line with data from England and Wales1 and data from New York City, where risk of mortality increased by 1.16 per 10 years of age. In contrast, the largest reduction in OHCA was observed in patients aged 65–79 and only in cantons with a high COVID-19 incidence. To explain this observation, one may postulate that during the entire pandemic, the hospital capacities were readily available19 thus, enabling hospitalization of patients presenting early symptoms who, however, later died in hospital. Therefore, the early hospitalization of a group of individuals at risk of sudden death, with possibly significant concomitant cardiovascular pathologies or co-morbidities have artificially been removed them from a group of individuals who, in other geographical areas, may have experienced an OHCA. Several reasons, other than early hospitalization, may have contributed to a lower OHCA incidence in younger age groups (<65 years). Firstly, younger patients less frequently experienced severe COVID-19 symptoms requiring hospitalization and/or systemic complications leading to OHCA. Another possibility may be related to a change in the frequency of non-medical OHCA etiologies such as trauma and/or overdose as a result of the lockdown. These OHCA causes are by far more common in young people. Finally, the absolute number of young patients was numerically much lower than patients 65+.
An alternative explanation of our findings is the possibility that individuals were either treated and died at home without alerting EMS, or were simply found dead at home and the family doctor or the nurse practitioner rather than EMS were informed/alerted. As mentioned above, it is very difficult to retrospectively evaluate the most likely scenario, also considering the recommendations for EMS issued in Switzerland by the Swiss Society of Emergency and Rescue Medicine,20 which suggest to carefully consider hospitalization of people of over 80 years of age presenting severe respiratory distress, most likely COVID-19 related, which may have played a role in the decision to start resuscitation or on-field treatment.
The clinical and demographic characteristics of our patients are similar to other OHCA populations,3, 4, 5, 6, 7, 8, 18, 21 which have also been the focus of recent meta-analyses.22, 23 In contrast with the study by Baldi et al.6 and by Marijon et al.,4 we did not observe a change in etiology, witnessed status and presenting rhythm of OHCA when comparing the year 2020–2019. The exact reason for the unchanged characteristics of OHCA despite high incidence of COVID-19 cases remains unknown. On the other hand, consistent with the Lombardy and Paris area experience, we noticed an increase in OHCAs at home and a reduction in OHCA occurring during sport or leisure activities, which is certainly related to the quarantine and lockdown orders issued in Switzerland9, as in the neighboring countries. A decrease in the bystander CPR rate and AED use, as well as a markedly reduced OHCA survival rate to hospital admission in those cantons with high incidence of COVID-19 cases, represent the indirect effects of the lockdown, changes in citizen behaviour, and pandemic related health system issues.6, 9, 10, 24 On the other hand, there was a surprisingly higher proportion of OHCA managed by first responders which may in part explain both the decrease in AED use by bystander and, most importantly, the unchanged outcome of OHCA during the pandemic compared to the previous year thus, confirming the key role played by this group in the chain of survival.25 The larger availability of FR may be due to a relative reduction in calls for other emergency situations alongside reduction in work commitments for lay FR. The larger FR availability and the reduction in city traffic following the lockdown, resulted in shorter arrival time of FR and EMS.
Although our study is the first to describe the indirect effect of the ongoing COVID-19 pandemic at national level, some limitations need to be acknowledged. We covered the first 65 days of the pandemic, until the moment the government announced the plan to lift coronavirus lockdown (April 27th, 2020) instead of considering the end of the pandemic. However according to the Swiss Federal Office of Public Health, at end of April the number of COVID-19 cases already significantly decreased and thus the majority of the effect on mortality and OHCA occurrence was included in our period analysis. Another limitation is given by the fact that there are no data regarding the number of patients suspected or diagnosed for COVID-19 among OHCAs which occurred in the first and second quarter of 2020. However, our analysis dividing Cantons according to the incidence rate of the COVID-19 infection, allows us to estimate how COVID-19 could have impacted the population. Moreover, the indication to reverse transcription polymerase chain reaction test of SARS-CoV-2, the implementation strategy and the ability to perform them, were independently implemented by different Swiss cantons; however they were implemented near simultaneously following the recommendations of the Federal Office of Public Health of the Swiss Confederation. A further limitation of our study is represented by the fact that we cannot compare 2020 to other years previous to 2019, as the SWISSRECA was established during 2018. Our analysis considers OHCAs occurring in a small populated nation (about 8 million inhabitants) living in large rural areas and small mid-size cities, thus results need confirmation in other nations having a similar population as well as coming from much larger populations. Finally, given the small FR sample size and OHCA cases, at the present time it is difficult to make a hypothesis about the different behavior of FR in low and high incidence Cantons.
Conclusions
Our study indicated a divergent trend between overall mortality and OHCA incidence during the COVID-19 pandemic in Switzerland. Although our data do not allow us to determine the precise physio-pathological mechanism for the observation, it is unlikely related to biological factors or to a direct effect of the disease. It is possibly multifactorial and related to an unsaturated hospital capacity during the pandemic or fast reorganization of EMS across the country, or to health care system management and organization of medical service at home even outside the pandemic.
Funding
The present study received no specific funding.
EB salary is partially funded from the European Union Horizon 2020 research and innovation programme under the acronym ESCAPE-NET, registered under grant agreement No 733381.
Conflict of interest
No conflict of interest to declare.
SWISSRECA Researchers and Acknowledgments
We would like to thank all the SWISSRECA researchers and all the EMS personnel.
SWISSRECA researchers: Michael Würsten, Hans-Peter Wyss, Markus Hilsenbeck, Christian Hartkopf, Daniel Martin Kreis, Marc Willhelm Hattler, Gaston Pascal Voney, Erika Csatlos, Regula Brülisauer, Friedhelm Braun, Jens Sonntag, Marc Stiller, Eva-Maria Kiffmann, Nadine Nieuwkamp, Patrik Müller, Matthias Volken, Jean-Luc Crevoisier, Thomas Giger, Marco Harder, Patrick Siebenpfund, Marc Lüthy, Michel Eigenmann, Jean-Pierre Boschung, Marc Rosso, Stéphane Jaccard, Etienne Benoît, Manuela Spicher, Emanuelle Bourgeay, Tony Billieux, Patricia Petter, Guillaume Gallet, Valérie Froidevaux, Alex Borel, Loric Stuby, Robert Larribau, Karl Gisler, Ulrich Bauerschmidt, Alex Gisler, Gian Martin Sommerau, Ferruccio Pedretti, Laura Raveglia, Fadri Erni, Sergio Calabresi, Catherine Rehm Marchand, Micha Dambach, Gian Cajöri, Iris Weber, Jordan Charpilloz, Cédric Jaccoud, Yves-André Challandes, Jean-Daniel Zimmerli, Paul Imboden, Remo Degani, Oliver Reisten, Kerstin Riesterer, Damian Aegerter, Reto Hauser, René Eichhorn, Michael Achermann, Steve Polster, Stephan Beuerlein, Christian Hollenstein, Susanne Schwörer, Cesare Bruno, Matteo Pauli, Myriam Meyerhans-Schild, Andreas Müller, Emiliano Cossu, Michela Panzini, Philippe Michel, André Baumann, Karin Volken, Stéphane Rigo, David Neel, Pascal Bucheli, Tobias Laner, Cédric Stadelmann, Julien Sierro, Alexandre Briguet, Martin Mühlemann, Klaus Homburg, Stefan Eschenmoser, Flavia Schmidli, Barbara Kirtz, Paul Rohner, Walter Scarnato, Daniel Button, Fabian Widmer, Roland Albrecht, Stiafen Furger.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.resplu.2021.100105.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Docherty K., Butt J., de Boer R. Excess deaths during the Covid-19 pandemic: an international comparison. medRxiv. 2020 doi: 10.1101/2020.04.21.20073114. Published online 2020:2020.04.21.20073114. [DOI] [Google Scholar]
- 2.Odone A., Delmonte D., Scognamiglio T., Signorelli C. COVID-19 deaths in Lombardy, Italy: data in context. Lancet Public Health. 2020;5:e310. doi: 10.1016/S2468-2667(20)30099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the COVID-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marijon E., Karam N., Jost D. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong Laura E., Hawkins Jessica E., Langness Simone, Murrell Karen L., Iris Patricia, Sammann Amanda. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal. 2020:1–12. doi: 10.1056/CAT.20.0193. (Figure 1) [DOI] [Google Scholar]
- 6.Baldi E., Sechi G.M., Mare C. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai P.H., Lancet E.A., Weiden M.D. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;11201:1–10. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fothergill R.T., Smith A.L., Wrigley F., Perkins G.D. Out-of-hospital cardiac arrest in London during the COVID-19 pandemic. Resusc Plus. 2020;5:100066. doi: 10.1016/j.resplu.2020.100066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parmet W.E., Sinha M.S. Covid-19 — the law and limits of quarantine. N Engl J Med. 2020;382:E281–E283. doi: 10.1056/NEJMp2004211. [DOI] [PubMed] [Google Scholar]
- 10.Elizabeth Brindle M., Gawande A. Managing COVID-19 in surgical systems. Ann Surg. 2020;272 doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scquizzato T., Olasveengen T.M., Ristagno G., Semeraro F. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi: 10.1016/j.resuscitation.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perkins G.D., Couper K. COVID-19: long-term effects on the community response to cardiac arrest? Lancet Public Health. 2020;5:e415–e416. doi: 10.1016/S2468-2667(20)30134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sayre M.R., Barnard L.M., Counts C.R. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander cardiopulmonary resuscitation. Circulation. 2020:507–509. doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 14.Federal Statistical Office . 2020. Deaths.https://www.bfs.admin.ch/bfs/en/home/statistics/population/births-deaths/deaths.html [Google Scholar]
- 15.Perkins G.D., Jacobs I.G., Nadkarni V.M. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a Task Force of the International Liaison Committee. Circulation. 2015;132:1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 16.FOPH Federal Office of Public Health . 2021. New coronavirus: situation in Switzerland.https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international.html [Google Scholar]
- 17.Kontopantelis E., Mamas M.A., Deanfield J. Excess mortality in England and Wales during the first wave of the COVID-19 pandemic. J Epidemiol Community Health. 2021;75:213–223. doi: 10.1136/jech-2020-214764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ball J., Nehme Z., Bernard S., Stub D., Stephenson M., Smith K. Collateral damage: hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020;156:157–163. doi: 10.1016/j.resuscitation.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.European Commission . 2020. Health at a Glance: Europe 2020.https://ec.europa.eu/health/sites/health/files/state/docs/2020_healthatglance_rep_en.pdf [Google Scholar]
- 20.2020. Swiss Society of Emergency and Rescue Medicine.https://www.sgnor.ch/covid-19-empfehlungen-sgnor-v20/ [Google Scholar]
- 21.Rosell Ortiz F., Fern P., Knox E.C. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. 2020;157:230–240. doi: 10.1016/j.resuscitation.2020.09.037. Published online 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim Z.J., Ponnapa Reddy M., Afroz A., Billah B., Shekar K., Subramaniam A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: a systematic review and meta-analysis. Resuscitation. 2020;157:248–258. doi: 10.1016/j.resuscitation.2020.10.025. Published online 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scquizzato T., Landoni G., Paoli A. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: a systematic review. Resuscitation. 2020;157:241–247. doi: 10.1016/j.resuscitation.2020.10.020. Published online 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Filippo O., D’Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:1–3. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caputo M.L., Muschietti S., Burkart R. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: a comparison with SMS-based system notification. Resuscitation. 2017;114:73–78. doi: 10.1016/j.resuscitation.2017.03.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.