Abstract
Aim
Recent studies have shown that the integration of a trained cardiopulmonary resuscitation (CPR) Coach during resuscitation enhances the quality of CPR during simulated paediatric cardiac arrest. The objective of our study was to evaluate the effect of a CPR Coach on adherence to Paediatric Advanced Life Support (PALS) guidelines during simulated paediatric cardiac arrest.
Methods
This was a secondary analysis of data collected from a multicentre randomized controlled trial assessing the quality of CPR in teams with and without a CPR Coach. Forty paediatric resuscitation teams were equally randomized into 2 groups (with or without a CPR Coach). The primary outcome was adherence to PALS guidelines during a simulated paediatric cardiac arrest case as measured by the Clinical Performance Tool (CPT). Video recordings were assigned to 2 pairs of expert raters. Raters were trained to independently score performances using the tool.
Results
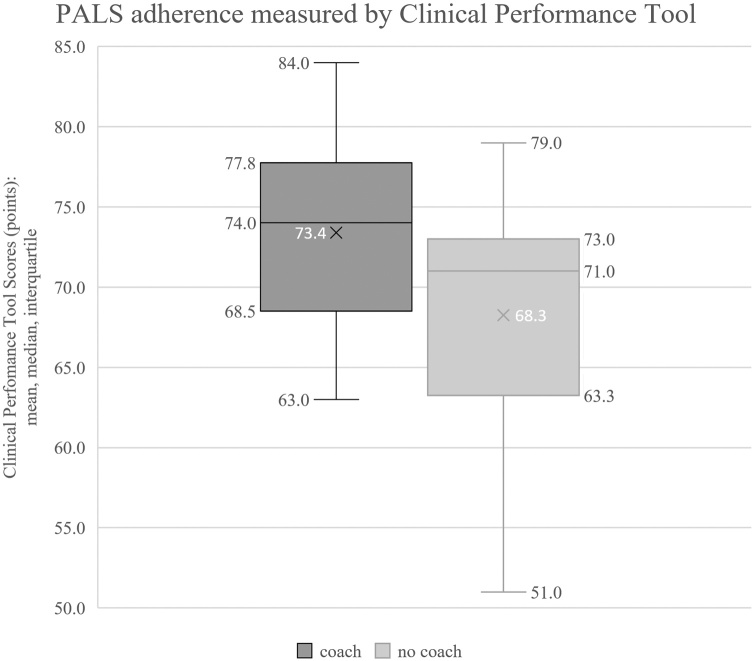
The reliability of the rating was adequate for the Clinical Performance Tool with an intraclass coefficients of 0.67 (95%CI: 0.22 to 0.84). Performance scores of the different teams varied between 51 and 84 points on the Clinical Performance Tool with a mean score of 70. Teams with a CPR Coach demonstrated better adherence to PALS guidelines (i.e. CPT score 73 points) compared to teams without a CPR Coach (68 points, difference 5 points; 95%CI: 1.0–9.3, p = 0.016).
Conclusion
In addition to improving CPR quality, the presence of a CPR Coach improves adherence to PALS guidelines during simulated paediatric cardiac arrests when compared with teams without a CPR Coach.
Keywords: Pediatric, Emergency, Simulation, PALS, Resuscitation, CPR, CPR coach
Introduction
Paediatric teams struggle providing guideline compliant Cardiopulmonary resuscitation (CPR) during cardiac arrest.1, 2 Strategies implemented to enhance CPR quality, include simulation-based training,3 CPR feedback devices,4 and integration of a CPR Coach.5, 6 The CPR Coach is a role created at The Johns Hopkins Hospital in 2007 and iteratively refined over the past decade as reported by Hunt et al.5 The primary objectives of the CPR Coach are to ensure high quality Basic Life Support or CPR and to cognitively unload the resuscitation leader so they can concentrate on the more complex components of a resuscitation, such as: rhythm recognition, identifying and following the advanced life support algorithm, diagnosing and treating reversible causes, and communicating with the family.
In addition to optimizing CPR delivery, adhering to Paediatric Advanced Life Support (PALS) guidelines is essential. Critical interventions in paediatric resuscitation such as advanced airway ventilation, cardiac rhythm recognition and adequate treatment (defibrillation and/or epinephrine) have shown to add substantial survival benefit in the adult population.7 In addition, adherence to PALS guidelines is associated with improved neurological outcomes and survival in children,8 though simulation studies reveal major deviations in adherence to PALS.9 The broad range of patient sizes require variations in equipment size and medication doses that creates a cognitive load unique to managing children.10 For years, cognitive aids have been recommended11 but showed poor efficacy12 supporting the need for a “human cognitive aid”. A CPR Coach might be considered a human cognitive aid, as the team leader is relieved of tasks, leaving more cognitive space for advanced clinical performance.5, 13
CPR coaching is associated with improved CPR quality, but its’ effect on general clinical performance in paediatric cardiac arrest has not been evaluated.
Objective
The objective of this study was to assess if the presence of a CPR Coach would improve adherence to PALS guidelines during simulated paediatric resuscitations.
Methods
This was a secondary analysis of data from a multicentre Randomized Controlled Trial (RCT) assessing the impact of a CPR Coach on CPR quality during simulated paediatric cardiac arrests.6 The study was approved by research ethics boards from all study sites. Informed consent was obtained from participants. The initial study was registered at clincaltrials.gov (Id: NCT03204162). The research question of the current study was developed after completing the initial study.
Setting
The study was conducted at four Simulation Centres across North America between March 2017 and February 2018.6 Participants were video-recorded during standardized 18-minute paediatric resuscitation scenarios (cardiopulmonary arrest from hyperkalemia with progression from pulseless ventricular tachycardia to ventricular fibrillation, then pulseless electrical activity) with identical equipment across sites (manikin Laerdal® SimJunior and a Zoll® CPR feedback defibrillator). Debriefings used the PEARLS method, and occurred at the end of simulations.14
Study population
Participants were senior residents, fellows or nurses with greater than five years of practice and PALS certified.6 They were divided into 40 teams comprised of five people: CPR providers, a team leader, an airway provider, and either a CPR Coach or bedside provider depending on randomization.
Intervention
Teams were randomized to one of two study arms: intervention (with CPR Coach) or control. Randomization was conducted to ensure equal allocation of teams across study arms and in each centre. The CPR Coach stood close to the defibrillator and actively coached CPR providers. CPR Coaches were trained to coordinate four key tasks: initiation of CPR, provider switch and pulse/rhythm check, defibrillation, and intubation. A one-hour training session was provided to designated coaches.6 CPR Coach training was not accessible for other participants, but participants from the intervention arm received a description of the CPR Coach role.
Outcome
The primary outcome was adherence to PALS guidelines as measured by a tailored version of the Clinical Performance Tool (CPT). The tool is a task-based scoring instrument, developed and validated by Donoghue et al.15 and further validated by Levy et al. to evaluate clinical performance during paediatric resuscitation simulated scenarios.16 The score is highly reliable with an intra-class coefficient of 0.95.16 It assesses critical tasks every few minutes using a scale from 0 to 2 points (except defibrillation during non-shockable rhythm which were scored 0–1 point). We tailored the tool for the standardized 18-minute scenario giving a minimum of 0 and a maximum of 87 points.
All 40 videos were evaluated in duplicate, by two sets of independent raters. The eight raters were paediatric critical care or paediatric emergency physicians with experience in simulation. A first set of four raters was blinded to our study hypothesis and the identity of participants, but not to the study arm. The second set was not blinded to the study hypothesis and rated the same scenarios as the first set, to be used for inter-rater reliability. Each blinded rater was paired with a non-blinded rater, and IRR were calculated separately for each video. Results from non-blinded raters were not included in the main analysis. Raters were trained to score scenarios and to gather data on performances by the principal investigator. Standardized, individual training sessions initially clearly defined each item of the score and addressed how to evaluate the videos. This was followed by a scoring session of two videos, different from those they were expected to rate. Each pair of raters independently rated ten videos (five with and five without a CPR Coach, duration of three hours).
Sample size
The sample size was 40 teams (20 with and 20 without a coach), identical to the original study.6
Analysis
Interrater reliability was initially assessed using the intra-class coefficient for the absolute scores assigned in duplicate using a two-way mixed model. A priori, it was decided to include only items with an average coefficient higher than 0.6.
The primary analysis was the difference in mean scores for the two groups with 95% Confidence interval (95%CI) on the CPT assuming normal distribution for the scores. This was used because a Shapiro-Wilk test failed to reject normal distribution (P: 0.282). As an exploratory analysis, the difference in mean scores for each item of the tool were compared for each group.
Results
In the original study, one team was excluded because of a technical issue. The remaining 40 teams (200 participants) were equally randomized between intervention and control groups. Demographic data revealed no significant differences between study groups at baseline.6 The reliability of the rating was adequate for the CPT with intraclass coefficients of 0.67 (95%CI: 0.22 to 0.84).17, 18
Performance scores of the different teams varied between 51 and 84 points on the CPT, with a mean score of 70. Scenarios involving the presence of a Coach demonstrated better performances than the group without a Coach as shown in Fig. 1 (difference: 5.2 points; 95%CI: 1.0–9.3; p = 0.016). This represent a large difference with a Cohen-D effect size of 0.797. Of the 45 items of the score, 8 demonstrated a statistically significant difference between the two groups. The largest difference was a significantly higher proportion of CPR providers change within the first 2 min in teams with a CPR Coach (1.85 vs. 0.95 points; p = 0.001). Other major improvements for teams with a CPR Coach included better diagnosis of the first rhythm (0.4 point; p = 0.027) and adequate ventilation initiation (0.2 point; p = 0.04) as shown in Table 1.
Fig. 1.
Score of PALS adherence with coach and no coach.
Discussion
Our study demonstrates presence of a CPR Coach is associated with improved clinical performance and adherence to PALS guidelines during simulated paediatric cardiac arrests. Previous studies have demonstrated improvement in CPR metrics such as chest compression depth, rate, fraction and pauses when using a CPR Coach in adult13 and paediatric cardiac arrests.5, 6 To our knowledge, this is the first study to show having a CPR Coach on the team is associated with better recognition of the first rhythm, a crucial step to determining the correct PALS algorithm.
Previous studies showed major deviations in PALS adherence19, 20 even after simulation training.9, 21 Our results might be explained by using the concept of “divide and conquer” to provide relief in cognitive overload.5, 13 For example, teams with a CPR Coach had a better initiation of ventilation and first CPR provider change (i.e. attention to BLS) presumably because the CPR Coach made sure key elements of CPR (compressions and ventilations) occurred. Simultaneously, the Resuscitation Leader quickly assessed the initial rhythm.
An improvement of 5.2 out of 87 points on CPT score might be considered slight. However, 2 points represent a timely defibrillation in a 2-minute interval (vs no defibrillation) or a correct rhythm identification. Hunt et al. showed that these elements are often delayed and may worsen outcomes. Therefore, differences of 5 points in CPT scores might indeed have an important clinical impact.8
Our results support the progressive implementation of CPR Coach in paediatric code teams of North America.22 In-hospital paediatric resuscitations are usually overcrowded, so this could be re-allocation of roles. Provider confidence, satisfaction or stress23 may be impacted by communication and teamwork. CPR Coach training must include communication tips for the CPR team and Resuscitation Leader, such that the leader truly empowers the CPR Coach to be an excellent manager of the Airway and Compressor roles and then concentrates on advanced components of the resuscitation. This should lead to faster recognition of shockable rhythms and defibrillation, faster recognition and treatment of obstructed endotracheal tubes, and diagnosis and treatment of other reversible causes. If the leader does not delegate, empower or trust their CPR Coach then the resuscitation will not improve. This requires training of the CPR Coaches as well as the Resuscitation Leaders.
Limitations
Our study has limitations. It was impossible to blind raters to the intervention. However, primary raters were blinded to the study question and hypothesis and there was an adequate inter-rater agreement between both set of assessors. The simulated setting may have influenced behaviours, but both groups had the same standardized scenario with identical resources. In some videos, the ventilation frequency or number of joules used in the defibrillation were not visible. Assessors may have given scores despite insufficient information, causing biases in results towards a smaller difference between groups. No study has defined what is a clinically significant difference using the CPT score or if all items of the score have the same clinical impact. The information from this study can be used to design future studies on how to optimize the impact of the CPR Coach on PALS.
Conclusion
In conclusion, the presence of a CPR Coach correlated with an improvement in adherence to PALS guidelines during simulated paediatric resuscitations. Emergency settings should consider adopting and implementing this new role during paediatric resuscitations.
Author contribution
Michael Buyck and Arielle Levy initiated the study and they had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Michael Buyck, Yasaman Shayan, Jocelyn Gravel, Elizabeth A. Hunt, Adam Cheng, and Arielle Levy contributed to the study design, organization of data acquisition and to interpretation of the results.
The first draft of the manuscript was written by Michael Buyck.
All authors contributed to amend it and approved the final version.
Conflicts of interest
Dr. Adam Cheng is a volunteer for the American Heart Association (Resuscitation Education Summit and Education Writing Group) and the International Liaison Committee for Resuscitation (Domain Lead, Education).
Dr. Elizabeth A. Hunt is a volunteer for the American Heart Association (Resuscitation Education Summit and Education Writing Group and ECC Science Subcommittee). She is a consultant for the Zoll Medical Corporation and has received reimbursement for travel and honoraria for speaking. She and research colleagues have patents on educational technology that they developed and have non-exclusive licenses with Zoll Medical Corporation to use that technology.
Dr. Arielle Levy is a volunteer for the American Heart Association (2020 AHA Paediatric Guidelines Education Writing Group).
The other authors (Michael Buyck, Yasaman Shayan, and Jocelyn Gravel) have no other relevant disclosures.
Acknowledgement
We acknowledge the four blinded raters who dedicated their free time to analyse the video recordings: Dre. Lydia DiLiddo, Dr. Michael Arsenault, Dr. Antonio D’Angelo, Dr. Baruch Toledano.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.resplu.2020.100058.
Contributor Information
Michael Buyck, Email: michael.buyck@umontreal.ca.
Yasaman Shayan, Email: yrshayan@gmail.com.
Jocelyn Gravel, Email: graveljocelyn@hotmail.com.
Elizabeth A. Hunt, Email: ehunt@jhmi.edu.
Adam Cheng, Email: chenger@me.com.
Arielle Levy, Email: arielle.levy@umontreal.ca.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Sutton R.M., Niles D., French B. First quantitative analysis of cardiopulmonary resuscitation quality during in-hospital cardiac arrests of young children. Resuscitation. 2014;85 doi: 10.1016/j.resuscitation.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kitamura T., Iwami T., Kawamura T. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. The Lancet. 2010;375:1347–1354. doi: 10.1016/S0140-6736(10)60064-5. [DOI] [PubMed] [Google Scholar]
- 3.Weinstock P.H., Kappus L.J., Kleinman M.E., Grenier B., Hickey P., Burns J.P. Toward a new paradigm in hospital-based pediatric education: the development of an onsite simulator program*. Pediatr Crit Care Med. 2005;6:635–641. doi: 10.1097/01.PCC.0000185489.07469.AF. [DOI] [PubMed] [Google Scholar]
- 4.Cheng A., Brown L.L., Duff J.P. Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES Study): a randomized clinical trial. JAMA Pediatr. 2015;169:137–144. doi: 10.1001/jamapediatrics.2014.2616. [DOI] [PubMed] [Google Scholar]
- 5.Hunt E.A., Jeffers J., McNamara L. Improved cardiopulmonary resuscitation performance with CODE ACES2: a resuscitation quality bundle. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2018;7 doi: 10.1161/JAHA.118.009860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng A., Duff J.P., Kessler D. Optimizing CPR performance with CPR coaching for pediatric cardiac arrest: a randomized simulation-based clinical trial. Resuscitation. 2018;132:33–40. doi: 10.1016/j.resuscitation.2018.08.021. [DOI] [PubMed] [Google Scholar]
- 7.Bergum D., Haugen B.O., Nordseth T., Mjølstad O.C., Skogvoll E. Recognizing the causes of in-hospital cardiac arrest--a survival benefit. Resuscitation. 2015;97:91–96. doi: 10.1016/j.resuscitation.2015.09.395. [DOI] [PubMed] [Google Scholar]
- 8.Carcillo J.A., Kuch B.A., Han Y.Y. Mortality and functional morbidity after use of PALS/APLS by community physicians. Pediatrics. 2009;124:500–508. doi: 10.1542/peds.2008-1967. [DOI] [PubMed] [Google Scholar]
- 9.Hunt E.A., Walker A.R., Shaffner D.H., Miller M.R., Pronovost P.J. Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: highlighting the importance of the first 5 minutes. Pediatrics. 2008;121:e34–43. doi: 10.1542/peds.2007-0029. [DOI] [PubMed] [Google Scholar]
- 10.Luten R., Wears R.L., Broselow J., Croskerry P., Joseph M.M., Frush K. Managing the unique size-related issues of pediatric resuscitation: reducing cognitive load with resuscitation aids. Acad Emerg Med. 2002;9:840–847. doi: 10.1197/aemj.9.8.840. [DOI] [PubMed] [Google Scholar]
- 11.Rosenthal T.L., Downs A. Cognitive aids in teaching and treating. Adv Behav Res Ther. 1985;7:1–53. doi: 10.1016/0146-6402(85)90010-4. [DOI] [Google Scholar]
- 12.Nelson McMillan K., Rosen M.A., Shilkofski N.A., Bradshaw J.H., Saliski M., Hunt E.A. Cognitive aids do not prompt initiation of cardiopulmonary resuscitation in simulated pediatric cardiopulmonary arrests. Simul Healthc. 2018;13:41–46. doi: 10.1097/SIH.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 13.Infinger A.E., Vandeventer S., Studnek J.R. Introduction of performance coaching during cardiopulmonary resuscitation improves compression depth and time to defibrillation in out-of-hospital cardiac arrest. Resuscitation. 2014;85:1752–1758. doi: 10.1016/j.resuscitation.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 14.Eppich W., Cheng A. Promoting excellence and reflective learning in simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc J Soc Simul Healthc. 2015;10:106–115. doi: 10.1097/SIH.0000000000000072. [DOI] [PubMed] [Google Scholar]
- 15.Donoghue A., Nishisaki A., Sutton R., Hales R., Boulet J. Reliability and validity of a scoring instrument for clinical performance during Pediatric Advanced Life Support simulation scenarios. Resuscitation. 2010;81:331–336. doi: 10.1016/j.resuscitation.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Levy A., Donoghue A., Bailey B. External validation of scoring instruments for evaluating pediatric resuscitation. Simul Healthc. 2014;9:360. doi: 10.1097/SIH.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 17.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 18.Gisev N., Bell J.S., Chen T.F. Interrater agreement and interrater reliability: Key concepts, approaches, and applications. Res Soc Adm Pharm. 2013;9:330–338. doi: 10.1016/j.sapharm.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Labrosse M., Levy A., Donoghue A., Gravel J. Delays and errors among pediatric residents during simulated resuscitation scenarios using Pediatric Advanced Life Support (PALS) algorithms. Am J Emerg Med. 2015;33:1516–1518. doi: 10.1016/j.ajem.2015.07.049. [DOI] [PubMed] [Google Scholar]
- 20.Hunt E.A., Vera K., Diener-West M. Delays and errors in cardiopulmonary resuscitation and defibrillation by pediatric residents during simulated cardiopulmonary arrests. Resuscitation. 2009;80:819–825. doi: 10.1016/j.resuscitation.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 21.Quan L., Shugerman R.P., Kunkel N.C., Brownlee C.J. Evaluation of resuscitation skills in new residents before and after pediatric advanced life support course. Pediatrics. 2001;108 doi: 10.1542/peds.108.6.e110. e110–e110. [DOI] [PubMed] [Google Scholar]
- 22.Pfeiffer S., Lauridsen K.G., Wenger J. Code team structure and training in the pediatric resuscitation quality international collaborative. Pediatr Emerg Care. 2020 doi: 10.1097/PEC.0000000000001748. Publish ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sørensen J.L., van der Vleuten C., Rosthøj S. Simulation-based multiprofessional obstetric anaesthesia training conducted in situ versus off-site leads to similar individual and team outcomes: a randomised educational trial. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-008344. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.