Abstract
Background
Regional cerebral oxygen saturation (rSO2) is a non-invasive method of measuring cerebral perfusion; However, serial changes in cerebral rSO2 values among out-of-hospital cardiac arrest (OHCA) patients in pre-hospital settings have not been sufficiently investigated. We aimed to investigate the association between the serial change in rSO2 pattern and patient outcome.
Methods
We evaluated rSO2 in OHCA patients using portable monitoring by emergency life-saving technicians (ELTs) from June 2013 to December 2019 in Osaka City, Japan. We divided the patterns of serial of rSO2 change into type 1 (increasing pattern) and type 2 (non-increasing pattern). Patients in whom measurement started after return of spontaneous circulation (ROSC) were excluded. The outcome measures were ‘Prehospital ROSC’, ‘Alive at admission’, ‘1-month survival’ and ‘Cerebral Performance Category (CPC) 1 or 2′.
Results
Eighty-seven patients were eligible for this analysis (type 1: n = 40, median age: 80.5 [IQR: 72–85.5] years, male: n = 20 [50.0%]; type 2: n = 47, 81 [72–85.5] years, male: n = 28 [59.6%]). In a multivariable logistic regression adjusted for confounding factors, outcomes of ‘Prehospital ROSC’ and ‘Alive at admission’ were significantly higher in type 1 than type 2 pattern (11/40 [27.5%] vs. 2/47 [4.26%], AOR 5.67, 95% CI 1.04–30.96, p < 0.045 and 17/40 [42.5%] vs. 6/41 [12.8%], AOR 3.56, 95% CI 1.11–11.43, p < 0.033). There was no significant difference in ‘1-month survival’ and ‘CPC 1 or 2′ between patterns.
Conclusion
Type 1 (increasing pattern) was associated with ‘Prehospital ROSC’ and ‘Alive at admission’. Pre-hospital monitoring of cerebral rSO2 might lead to a new resuscitation strategy.
Keywords: Near-infrared spectroscopy, Out-of-hospital cardiac arrest, Emergency medical technician, Emergency medical services, Emergency life-saving technician, Portable rSO2 monitor
Introduction
Regional cerebral oxygen saturation (rSO2) is a non-invasive method of measuring cerebral perfusion that has been reported in many studies in the resuscitation field.1, 2, 3 In this field, we have focused on measurement of serial changes in the values of rSO2 rather than measuring a single rSO2 value at one time point.3, 4, 5, 6 Some research groups have reported that one-point measurement of cerebral rSO2 on hospital arrival can predict neurological outcome in patients with out-of-hospital cardiac arrest (OHCA),7, 8, 9 but we thought this might not be correct because in our previous studies,3, 4, 6 the values of rSO2 always changed depending on the patient's situation at the time cerebral rSO2 was measured. In addition, many near-infrared spectroscopy (NIRS) measurement devices in clinical use have been created based on the Ito et al.10 study showing an estimated venous/arterial distribution of 70/30% or 75/25% in the cerebral cortex.11, 12 However, Watzman et al. reported that the exact arterial/venous ratio in the cerebral cortex is not constant, so use of a fixed ratio may not be a good model by which to validate the technology.13 Further, it is considered optimal to measure the change (relative value) from a patient-specific baseline because the values of rSO2 might change based on various physiological changes in such as cardiac output, PaCO2, and pH, and even if the rSO2 values are measured on the same patient, they will differ on different NIRS devices.14, 15
Meanwhile, in the prehospital setting, serial changes in cerebral rSO2 values among OHCA patients during cardiopulmonary resuscitation (CPR) have not been sufficiently investigated, and only limited data exist.16, 17 We developed a portable rSO2 monitor (HAND ai TOS®; TOSTEC CO., Tokyo, Japan) that is small enough (170 mm × 100 mm × 50 mm in size and 600 g in weight) to carry in pre-hospital settings, and for the first time in the world,18 measurement of cerebral rSO2 by emergency life-saving technicians (ELTs) was started from 2013 in the prehospital setting.5 In 2016, we preliminarily reported on serial changes in cerebral rSO2 during CPR in the prehospital setting, recognized their importance, and were convinced that pre-hospital monitoring of cerebral rSO2 might lead to a new resuscitation strategy.5 Since then, the number of OHCA patients we have registered has increased, and in this study, we aimed to evaluate the association between the pattern of serial change in rSO2 in the prehospital setting and patient outcome.
Methods
Study design, population, and setting
This was a prospective observational study in which we prospectively enrolled OHCA patients ≥18 years old with a measurable rSO2 value who were treated by ELT from June 2013 to December 2019 in Osaka City, Japan. Osaka City is located in the central area of Japan, covers an area of 225.30 km2, and has a population of 2,746,983 people (2020).19 Among the 63 emergency medical service (EMS) ambulance teams of the Osaka Municipal Fire Department, we equipped 9 of 63 ambulances with portable rSO2 monitors. We originally started with one rSO2 monitor at the beginning of this research and gradually increased the number of monitors to nine units. Patients in whom measurement was started after return of spontaneous circulation (ROSC) were excluded.
The ELTs performed CPR according to recommendations of the Japan Resuscitation Council Guidelines 2010 or 2015,20, 21 which are based on the International Liaison Committee on Resuscitation. The rSO2 sensor is attached to the patient's forehead by the ELT (Supplementary Figure 1). The ELT did not change patient treatment according to the rSO2 data.
We collected pre-hospital data (the EMS ambulance record, including patient age, sex, initial rhythm, bystander CPR status, and ambulance time courses) and in-hospital data (patient outcome from the hospital in charge according to the Utstein style). We then combined the pre-hospital database data with the rSO2 data.
The pre-hospital portable monitoring of cerebral rSO2 in patients with OHCA was approved by the Ethics Committee of Osaka University Graduate School of Medicine (No. 12446-7), and the institutional review board waived the need for informed consent because the subjects were all in cardiopulmonary arrest (CPA).
Portable NIRS rSO2 monitoring system
We previously developed a portable rSO2 monitor (HAND ai TOS®; TOSTEC CO., Tokyo, Japan) (Supplementary Figure 1).5, 18 To date, the HAND ai TOS has not been approved by the Medicines and Healthcare Products Regulatory Agency (MHRA) or the US Food and Drug Administration (FDA). The HAND ai TOS system measures oxygen saturation based on the Beer-Lambert law by using three different wavelengths of near-infrared LED light, which have specific absorbance to oxyhaemoglobin and deoxyhaemoglobin. The lights pass through the skin to a depth of approximately 3 cm, and the reflected lights are sensed by a photodiode. The reflected lights represent the haemoglobin information mainly in the cerebral cortex.
Evaluation of serial change of rSO2
The system can measure rSO2 data every second without the necessity of arterial pulsation, so it is possible to perform continuous monitoring in CPA patients. Two rSO2 values, one from the left side and one from the right side, are acquired continuously, and then the average of the two values is calculated. The normal range of cerebral rSO2 was previously determined from 15 healthy adult volunteers to be 71.2 ± 3.9% (on room air) (n = 15; 10 men, 5 women; 43.2 ± 8.9 years).22 We divided the pattern of serial rSO2 change into type 1 (increasing pattern) and type 2 (non-increasing pattern) depending on whether the rSO2 value increased by at least 5% from the start of monitoring.
Endpoint
The primary outcome measure was ‘Prehospital ROSC’. The secondary outcome measures were ‘Alive at admission’, ‘1-month survival’ and ‘Cerebral Performance Category (CPC) 1 or 2′.
‘Drop phenomenon’
During this study, we found a ‘Drop phenomenon’ to occur in which the rSO2 value would decrease sharply, possibly due to circulatory failure in the brain. Therefore, we decided to additionally evaluate patients in whom this phenomenon was recognized.
Statistical analysis
Patients’ characteristics and outcomes were compared between two groups using the Wilcoxon rank-sum test for continuous variables and the chi-square test or Fisher's exact test for categorical variables. Multivariable analysis of the eligible patients was used to assess factors associated with the outcomes by using logistic regression models, and adjusted odds ratios (AORs) and their 95% confidence intervals (CIs) were calculated. Potential confounding factors based on biological plausibility and previous studies were included in the multivariable analysis. These potential factors were age (continuous value), sex (male, female), witness, and bystander CPR. A p value of <0.05 was considered significant. All statistical analyses were performed with JMP Pro 13 (SAS Institute Inc., Cary, NC, USA).
Results
Patient characteristics
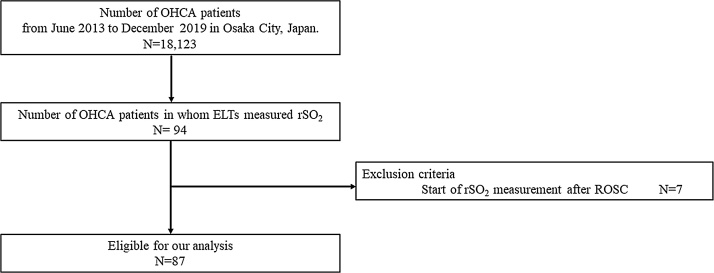
Fig. 1 shows the patient flow in this study. During the study period, the number of patients with OHCA in Osaka City was 18,123, and 94 OHCA patients were registered in this study. Seven patients were excluded because rSO2 measurement were started after ROSC. Fig. 2 showed representative cases of type 1 and 2 of serial changes in cerebral rSO2. Characteristics of the patient without ROSC when the ELT started monitoring rSO2 are shown in Table 1. In total, 87 patients were eligible for this analysis (type 1 [increasing rSO2 pattern]: n = 40, median age: 80.5 [IQR: 72–85.5] years, male; n = 20 [50.0%]; type 2 [non-increasing rSO2 pattern]: n = 47, 81 [71–84] years, male: n = 28 [59.6%]). The number of patients positive for the variables of ‘Witness’ and Administration of adrenaline by ELT’ were significantly larger in type 1 than type 2 pattern (p = 0.003 and p = 0.001, respectively).
Fig. 1.
Patient flow, OHACA, out-of-hospital cardiac arrest; rSO2, regional saturation of oxygen; ELTs, emergency life-saving technicians.
Fig. 2.
Representative cases of serial changes in cerebral rSO2. (A) Type 1: increasing pattern. This patient was a 95-year-old woman with an initial ECG of PEA (witness [+]; bystander CPR: unknown). Her rSO2 values increased gradually, and she achieved ROSC. After ROSC, her rSO2 values increased more sharply than before ROSC. (B) Type 2: non-increasing pattern. This patient was a 33-year-old man with an initial ECG showing asystole (witness [–]; bystander CPR [–]). His rSO2 values did not increase, and he did not achieve ROSC in the prehospital setting. CPR, cardiopulmonary resuscitation; ECG, electrocardiogram; EMS, emergency medical service; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; rSO2, regional saturation of oxygen.
Table 1.
Characteristics of patients without ROSC when ELT started rSO2 monitoring.
| Type of serial change in cerebral rSO2 |
p Value | ||
|---|---|---|---|
| Type 1: Increasing type (N = 40) | Type 2: Non-increasing type (N = 47) | ||
| Sex, n (%) | |||
| Male | 20 (50.0) | 28 (59.6) | 0.395 |
| Age, years, median (IQR) | 80.5 (72–85.5) | 81 (71–84) | 0.932 |
| Initial rhythm, n (%) | 0.097 | ||
| VF | 5 (12.5) | 3 (6.4) | |
| PEA | 16 (40.0) | 11 (23.4) | |
| Asystole | 19 (47.5) | 33 (70.2) | |
| Witness, n (%) | 0.003 | ||
| + | 25 (62.5) | 14 (29.8) | |
| - | 15 (37.5) | 33 (70.2) | |
| Bystander CPR, n (%) | 0.735 | ||
| + | 21(52.5) | 21 (44.7) | |
| − | 16 (40.0) | 21 (44.7) | |
| Unknown | 3 (7.5) | 5 (10.6) | |
| Administration of adrenaline by ELT, n (%) | 0.001 | ||
| + | 16 (40.0) | 4 (8.51) | |
| − | 24 (60.0) | 41 (87.2) | |
| Unknown | 0 (0.0) | 2 (4.7) | |
| Initial rSO2 value, median (IQR) | 42.1 (35.6–47.8) | 45.6 (40.1–49.7) | 0.114 |
| Drop phenomenon, n (%) | 0.33 | ||
| + | 3 (7.5) | 1 (2.13) | |
| - | 37 (92.5) | 46 (98.9) | |
CPR, cardiopulmonary resuscitation; ELT, emergency life-saving technician; IQR, interquartile range; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; rSO2, regional saturation of oxygen; VF, ventricular fibrillation.
Comparison of outcome by changing pattern of rSO2
Table 2 shows the outcomes by type of serial change in cerebral rSO2 by a multivariable logistic regression model. The outcomes of ‘Prehospital ROSC’ and ‘Alive at admission’ were both significantly higher in type 1 than type 2 (11/40 [27.5%] vs. 2/47 [4.26%], AOR 5.67, 95% CI 1.04–30.96, p < 0.045 and 17/40 [42.5%] vs. 6/41 [12.8%], AOR 3.56, 95% CI 1.11–11.43, p < 0.033). There was no significant difference in the outcomes of ‘1-month survival’ (5/40 [12.5%] vs. 1/47 [2.1%], AOR 3.21, 95% CI 0.32–32.72, p < 0.324) and ‘CPC 1 or 2′ (3/40 [7.5%] vs. 0/47 [0.0%]).
Table 2.
Outcomes by type of serial change in cerebral rSO2.
| Type 1: Increasing type |
Type 2: Non-increasing type |
Crude OR (95% CI) |
p Value | Adjusted OR* (95% CI) |
p Value | |
|---|---|---|---|---|---|---|
| Prehospital ROSC, % (n/N) | 27.5 (11/40) | 4.26 (2/47) | 8.53 (1.76–41.32) | 0.008 | 5.67 (1.04–30.96) | 0.045 |
| Alive at hospital admission, % (n/N) | 42.5 (17/40) | 12.8 (6/41) | 5.05 (1.75–14.60) | 0.003 | 3.56 (1.11–11.43) | 0.033 |
| 1-Month survival, % (n/N) | 12.5 (5/40) | 2.1 (1/47) | 6.57 (0.73–58.81) | 0.092 | 3.21 (0.32–32.72) | 0.324 |
| CPC 1 or 2, % (n/N) | 7.5 (3/40) | 0 (0/47) | N/A | N/A | N/A | N/A |
ORs were calculated for Increasing type vs. Non-increasing type.
CPR, cardiopulmonary resuscitation; CPC, Cerebral Performance Category; OR, odds ratio; CI, confidence interval; ROSC, return of spontaneous circulation; rSO2, regional saturation of oxygen.
Adjusted for age, sex, witness and bystander CPR.
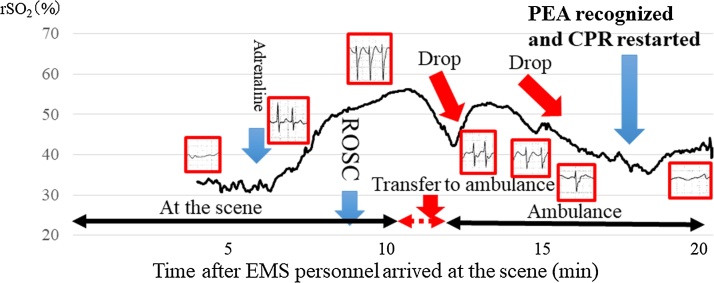
Drop phenomenon
We recognized this phenomenon in 6 of the 94 OHCA patients and show a typical case in Fig. 3. This 82-year-old woman showed pulseless electrical activity (PEA) on her initial ECG (witness [+] and bystander CPR [+]). Her rSO2 values gradually increased, and she achieved ROSC. However, during transport to hospital, although her ECG showed QRS waves, her rSO2 value suddenly dropped. After this, the ELT recognized PEA and restarted CPR. The other five patients also achieved ROSC in the prehospital setting, and the ELT also recognized PEA after the ‘Drop phenomenon’ in the serial change of rSO2 values. The ‘Drop phenomenon’ was only observed in patients after achieving ROSC. Table 3 shows the patient characteristics of these 6 patients with ‘Drop phenomenon’.
Fig. 3.
Representative case showing the ‘drop phenomenon’ in the serial change of rSO2 values. This patient was an 82-year-old woman with an initial ECG of PEA (witness [+]; bystander CPR [+]). Her rSO2 values increased gradually, and she achieved ROSC. However, during transport to hospital, although the ECG showed QRS waves, her rSO2 value suddenly dropped. After that, the ELT recognized PEA and restarted CPR. CPR, cardiopulmonary resuscitation; ECG, electrocardiogram; ELT, emergency life-saving technician; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; rSO2, regional saturation of oxygen.
Table 3.
Characteristics of the 6 patients with ‘Drop phenomenon’ in the serial change of rSO2 values.
| Case | Sex | Age | Initial rhythm | Witness | Bystander CPR | Administration of adrenaline by ELT |
Initial rSO2 value | Prehospital ROSC | Alive at hospital admission | 1-month survival | CPC 1 or 2 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1* | Female | 82 | PEA | + | – | + | 31.0 | Yes | Yes | No | No |
| 2 | Male | 64 | PEA | + | – | + | 40.5 (after ROSC) | Yes | No | No | No |
| 3 | Male | 58 | PEA | + | – | – | 50.3 | Yes | Yes | No | No |
| 4 | Male | 81 | PEA | + | + | – | 40.0 | Yes | Yes | No | No |
| 5 | Male | 79 | PEA | + | – | – | 53.3 | Yes | No | No | No |
| 6 | Male | 95 | PEA | + | – | – | 51.5 (after ROSC) | Yes | Yes | No | No |
CPR, cardiopulmonary resuscitation; CPC, Cerebral Performance Category; ELT, emergency life-saving technician; PEA, pulseless electrical activity; ROSC, return of spontaneous circulation; rSO2, regional saturation of oxygen.
See Fig. 3.
Discussion
Our analysis of the cerebral rSO2 measured by ELTs in patients with OHCA in the prehospital setting revealed that the pattern of serial change of rSO2 was significantly associated with the outcomes of ‘Prehospital ROSC’ and ‘Alive at admission’. To our knowledge, this is the first report to focus on the pattern of serial change of cerebral rSO2 measured by ELT in patients with OHCA in the prehospital setting. Our findings not only provide basic information about how rSO2 might change in these patients but may also help to develop a new resuscitation strategy in prehospital settings and improve the prognosis of these patients by allowing the immediate recognition of their rSO2 pattern and selection of the appropriate hospital for treatment.
The present multivariable logistic regression model showed that the outcomes of ‘Prehospital ROSC’ and ‘Alive at admission’ were significantly higher for patients with type 1 [increasing rSO2 pattern] than type 2 [non-increasing rSO2 pattern] (Table 2). Takegawa et al. reported that the combination of rSO2 (baseline) with the amount of maximum rise in rSO2 value over time might be a new index for the prediction of ROSC that could be useful in guiding CPR.3 This increasing rSO2 pattern in the prehospital setting was also reported by Genbrugge et al.16 and Prosen et al.17 However, Prosen et al.’s data were obtained from an evaluation made 5 min before ROSC. We thought they could not evaluate the rSO2 before loading the patient in an ambulance because the INVOS oximeter (Somanetics Corporation, Troy, MI, USA; 2010) they used is not portable like our monitor.5, 17 Further, both of these reports used absolute values of rSO2. We are paying attention to the amount and the pattern of the change rather than to the absolute value.
From the present results and those two previous papers,16, 17 it became clear to us that a one-point measurement of the rSO2 value no longer makes any sense. There is no doubt that the values of rSO2 always change depending on the patient's situation at the time cerebral rSO2 is measured even in the prehospital setting. The initial rSO2 values were not significantly different between the type 1 and type 2 patterns (p = 0.114) (Table 1).
There are several reports that an increase in rSO2 occurring before ROSC is associated with CPR quality.23, 24 We thought that certainly in some cases, the rSO2 values would increase slightly before ROSC by CPR in non-ROSC patients,4 but basically, an increase in rSO2 before ROSC is not associated with CPR quality. Parnia et al. showed that rSO2 is not increased in non-ROSC patients with in-hospital cardiac arrest (IHCA) during CPR.25 We thought IHCA patients would receive high-quality CPR early after cardiac arrest due to the hospital's rapid response system. In the present study as well, trained ELT are performing the CPR. Then, what does the increase of rSO2 before ROSC indicate? This point is still hypothetical, but we think that when the rSO2 increases before ROSC, the heartbeat is starting to increase slightly. If patients achieve ROSC, the pulse returns and the value of rSO2 rapidly rises as shown in Fig. 2. Further research is needed to confirm this hypothesis.
In contrast, the outcomes of patients with the type 2 (non-increasing rSO2) pattern were very poor (Prehospital ROSC: 4.26%, Alive at hospital admission: 12.8%, 1-month survival: 2.1%, CPC 1 or 2: 0%) (Table 2). Takegawa et al. reported no significant increase of rSO2 values during CPR in the emergency room in patients with non-sonographic cardiac activity or with Stanford type A aortic dissection diagnosed by CT scan.26 We did not examine whether these types of patients were included among those with type 2 (non-increasing rSO2) pattern. Further study to examine in detail what kind of patients show a type 2 pattern of rSO2 change is needed. Criteria for transport to hospitals based on patterns of rSO2 change may need to be developed in the future.
Another surprising result of this research was the discovery of the ‘Drop phenomenon’ (Fig. 3, Table 3). We show the relationship between the ECG waveform and serial change of rSO2 in Fig. 3. The ‘Drop phenomenon’, a rapid decrease in rSO2, might reflect a rapid decrease in cerebral perfusion, and its recognition might help to detect PEA earlier. The ELT can observe the patient's ECG in the ambulance but cannot check the actual pulse continuously. Therefore, if ELTs recognize a ‘Drop phenomenon’ on rSO2 monitoring, they should check the patient's pulse more frequently than usual and attempt to ascertain the presence of PEA as soon as they can. Recognition of the ‘Drop phenomenon’ may be the greatest benefit of pre-hospital rSO2 measurement.
Our study has some limitations. First, rSO2 monitoring was not performed in a blinded fashion. Therefore, the rSO2 value may have influenced the CPR procedures. Second, due to the high cost and limited number of rSO2 monitors, not all CPA patients during the period could be monitored. Third, since there were few cases of VF, it was not possible to examine the true initial ECG rhythm. Forth, in this study, we could not compare rSO2 values with etCO2 or some other substitute marker of perfusion. Fifth, it is possible that in the last 1–2 min before ROSC rSO2 value might increase as it is possible that ROSC has already occurred.
Conclusion
The type 1 (increasing) pattern of serial rSO2 change was significantly associated with the outcomes of ‘Prehospital ROSC’ and ‘Alive at admission’. Pre-hospital monitoring of cerebral rSO2 might lead to a new strategy of resuscitation.
Credit author statement
Tomohiko Sakai: Methodology, Investigation, Data curation, Tomoya Hirose: Formal analysis, Writing – Original Draft; Tadahiko Shiozaki: Conceptualization, Methodology, Project administration, Writing – Review & Editing: Ryosuke Takagawa: Validation, Mitsuo Ohnishi: Validation, Sumito Hayashida: Investigation, Shinji Shigematsu: Investigation, Keiichi Satou: Investigation, Yasunori Takemoto: Investigation, Takeshi Shimazu: Supervision, Writing – Review & Editing.
Conflict of interests
The authors declare that they have no conflicts of interest.
Funding
This work was supported by JSPS KAKENHI Grant NumberJP19H03758.
Acknowledgements
We gratefully acknowledge the devoted cooperation of the Osaka Municipal Fire Department.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.resplu.2021.100093.
Appendix A. Supplementary data
The following are the supplementary data to this article:
Supplementary Fig. I Photograph showing rSO2 measurement in a mock patient by ELTs and the portable near-infrared spectroscopy unit (portable rSO2 monitor). Circle: portable rSO2 monitor. rSO2, regional saturation of oxygen; ELTs, emergency life-saving technicians.
References
- 1.Jakkula P., Hästbacka J., Reinikainen M., Pettilä V., Loisa P., Tiainen M. Near-infrared spectroscopy after out-of-hospital cardiac arrest. Crit Care. 2019;23:171. doi: 10.1186/s13054-019-2428-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schnaubelt S., Sulzgruber P., Menger J., Skhirtladze-Dworschak K., Sterz F., Dworschak M. Regional cerebral oxygen saturation during cardiopulmonary resuscitation as a predictor of return of spontaneous circulation and favourable neurological outcome – a review of the current literature. Resuscitation. 2018;125:39–47. doi: 10.1016/j.resuscitation.2018.01.028. [DOI] [PubMed] [Google Scholar]
- 3.Takegawa R., Shiozaki T., Ogawa Y., Hirose T., Mori N., Ohnishi M. Usefulness of cerebral rSO2 monitoring during CPR to predict the probability of return of spontaneous circulation. Resuscitation. 2019;139:201–207. doi: 10.1016/j.resuscitation.2019.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Ogawa Y., Shiozaki T., Hirose T., Ohnishi M., Nakamori Y., Ogura H. Load-distributing-band cardiopulmonary resuscitation for out-of-hospital cardiac arrest increases regional cerebral oxygenation: a single-center prospective pilot study. Scand J Trauma Resusc Emerg Med. 2015;23:99. doi: 10.1186/s13049-015-0182-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirose T., Shiozaki T., Nomura J., Hamada Y., Sato K., Katsura K. Pre-hospital portable monitoring of cerebral regional oxygen saturation (rSO2) in seven patients with out-of-hospital cardiac arrest. BMC Res Notes. 2016;9:428. doi: 10.1186/s13104-016-2239-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehara N., Hirose T., Shiozaki T., Wakai A., Nishimura T., Mori N. The relationship between cerebral regional oxygen saturation during extracorporeal cardiopulmonary resuscitation and the neurological outcome in a retrospective analysis of 16 cases. J Intensive Care. 2017;5:20. doi: 10.1186/s40560-017-0216-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ito N., Nishiyama K., Callaway C.W., Orita T., Hayashida K., Arimoto H. Noninvasive regional cerebral oxygen saturation for neurological prognostication of patients with out-of-hospital cardiac arrest: a prospective multicenter observational study. Resuscitation. 2014;85:778–784. doi: 10.1016/j.resuscitation.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Hayashida K., Nishiyama K., Suzuki M., Abe T., Orita T., Ito N. Estimated cerebral oxyhemoglobin as a useful indicator of neuroprotection in patients with post-cardiac arrest syndrome: a prospective, multicenter observational study. Crit Care. 2014;18:500. doi: 10.1186/s13054-014-0500-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joo W.J., Ide K., Nishiyama K., Seki T., Tanaka H., Tsuchiya J. Prediction of the neurological outcome using regional cerebral oxygen saturation in patients with extracorporeal cardiopulmonary resuscitation after out-of-hospital cardiac arrest: a multicenter retrospective cohort study. Acute Med Surg. 2020;7:e491. doi: 10.1002/ams2.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ito H., Kanno I., Fukuda H. Human cerebral circulation: positron emission tomography studies. Ann Nucl Med. 2005;19:65–74. doi: 10.1007/BF03027383. [DOI] [PubMed] [Google Scholar]
- 11.Ohmae E., Ouchi Y., Oda M., Suzuki T., Nobesawa S., Kanno T. Cerebral hemodynamics evaluation by near-infrared time-resolved spectroscopy: correlation with simultaneous positron emission tomography measurements. Neuroimage. 2006;29:697–705. doi: 10.1016/j.neuroimage.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Murkin J.M., Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103 doi: 10.1093/bja/aep299. i3-13. [DOI] [PubMed] [Google Scholar]
- 13.Watzman H.M., Kurth C.D., Montenegro L.M., Rome J., Steven J.M., Nicolson S.C. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology. 2000;93:947–953. doi: 10.1097/00000542-200010000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Tobias J.D. Cerebral oxygenation monitoring: near-infrared spectroscopy. Expert Rev Med Devices. 2006;3:235–243. doi: 10.1586/17434440.3.2.235. [DOI] [PubMed] [Google Scholar]
- 15.Pisano A. Can we claim accuracy from a regional near-infrared spectroscopy oximeter? Anesth Analg. 2016;122:920. doi: 10.1213/ANE.0000000000001019. [DOI] [PubMed] [Google Scholar]
- 16.Genbrugge C., De Deyne C., Eertmans W., Anseeuw K., Voet D., Mertens I. Cerebral saturation in cardiac arrest patients measured with near-infrared technology during pre-hospital advanced life support. Results from Copernicus I cohort study. Resuscitation. 2018;129:107–113. doi: 10.1016/j.resuscitation.2018.03.031. [DOI] [PubMed] [Google Scholar]
- 17.Prosen G., Strnad M., Doniger S.J., Markota A., Stožer A., Borovnik-Lesjak V. Cerebral tissue oximetry levels during prehospital management of cardiac arrest – a prospective observational study. Resuscitation. 2018;129:141–145. doi: 10.1016/j.resuscitation.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Tajima G., Shiozaki T., Izumino H., Yamano S., Hirao T., Inokuma T. Portable system for monitoring of regional cerebral oxygen saturation during prehospital cardiopulmonary resuscitation: a pilot study. Acute Med Surg. 2015;2:48–52. doi: 10.1002/ams2.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.City of Osaka. Overview of Osaka City. Available from: https://www.city.osaka.lg.jp/toshikeikaku/page/0000402930.html.
- 20.Japanese Foundation Emergency Medicine. JRC resuscitation guideline 2010. Tokyo: Igaku-shoin.
- 21.Japanese Foundation Emergency Medicine. JRC resuscitation guideline 2015. Tokyo: Igaku-shoin.
- 22.Nakahori Y., Hirose T., Shiozaki T., Ogawa Y., Ohnishi M., Fujimi S. Serial changes in values of cerebral regional saturation of oxygen (rSO2) during resuscitation in patients with out-of-hospital cardiac arrest. Nihon Kyukyu Igakukai Zasshi. 2013;24:774–780. [Google Scholar]
- 23.Meex I., De Deyne C., Dens J., Scheyltjens S., Lathouwers K., Boer W. Feasibility of absolute cerebral tissue oxygen saturation during cardiopulmonary resuscitation. Crit Care. 2013;17:R36. doi: 10.1186/cc12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yagi T., Kawamorita T., Kuronuma K., Tachibana E., Watanabe K., Chiba N. Usefulness of a new device to monitor cerebral blood oxygenation using NIRS during cardiopulmonary resuscitation in patients with cardiac arrest: a pilot study. Adv Exp Med Biol. 2020;1232:323–329. doi: 10.1007/978-3-030-34461-0_41. [DOI] [PubMed] [Google Scholar]
- 25.Parnia S., Yang J., Nguyen R., Ahn A., Zhu J., Inigo-Santiago L. Cerebral oximetry during cardiac arrest: a multicenter study of neurologic outcomes and survival. Crit Care Med. 2016;44:1663–1674. doi: 10.1097/CCM.0000000000001723. [DOI] [PubMed] [Google Scholar]
- 26.Takegawa R., Shiozaki T., Ohnishi M., Muratsu A., Tachino J., Sakai T. The TripleCPR 16 Study: does rhythm truly needed to be checked every 2 minutes in cardiopulmonary arrest patients? Circulation. 2019;140:A459. [Google Scholar]