Abstract
Background
Research suggests rescuers deliver ventilations outside of recommendations during out of hospital cardiac arrest (OHCA), which can be deleterious to survival. We aimed to determine if ambulance clinician compliance with ventilation recommendations could be improved using the Zoll Accuvent real time ventilation feedback device (VFD).
Methods
Participants simulated a two-minute cardiac arrest scenario using a mannequin and defibrillator without ventilation feedback. Eligible for inclusion were all clinicians aged ≥18 years who perform cardiopulmonary resuscitation (CPR) as part of their role, who had completed an internal advanced life support (ALS) refresher. Following familiarisation of a few minutes with the VFD, participants repeated the two-minute scenario with ventilation feedback. Ventilation rate and volume and CPR quality were recorded. Primary outcome was % difference in ventilation compliance with and without feedback. Secondary outcomes were differences between paramedic and non-paramedic clinicians and compliance with chest compression guidelines.
Results
One hundred and six participants completed the study. Median ventilation rate without feedback was 10 (IQR 8–14, range 4–30) compared to 9 (IQR 9–9, range 6–17) with feedback; median tidal volume without feedback was 630 mls (IQR 518–725, range 201–1114) compared to 546 mls (IQR 531–560, range 490–750) with feedback. Proportion of clinicians ≥50% compliant with European Resuscitation Council ventilation recommendations were significantly greater with ventilation feedback compared to without, 91% vs. 9%, (McNemars test p = <0.0001). Paramedics out performed non-paramedic clinicians with and without feedback and compression quality was not compromised by using the VFD.
Conclusions
Ambulance clinician baseline ventilation quality was frequently outside of recommendations, but a VFD can ensure treatment is within evidence-based recommendations. Further research is required to validate the use of the VFD in true clinical practice and to evaluate the relationship between improved ventilation quality during OHCA and patient outcomes.
Keywords: Manual ventilation, Tidal volume, Respiratory rate, Out of hospital cardiac arrest, Simulation
Background
Out of hospital cardiac arrest (OHCA) is a leading cause of death and disability worldwide.1 In the UK, National Health Service (NHS) ambulance services treat approximately 30,000 OHCA's annually2 but survival rates remain poor. When treating an OHCA ambulance clinicians are required to deliver chest compressions and manual ventilations as part of cardiopulmonary resuscitation (CPR). Technology to support the delivery of high-quality chest compressions has been extensively studied and validated3, 4, 5 and is in widespread use. The quality of ventilations during CPR has not had the same attention.
After the initial phase of CPR, ventilation is essential to ensure adequate oxygenation and CO2 washout.6 Animal models have demonstrated progressive hypoxia, hypercapnia and acidosis develop if adequate ventilation is not provided during CPR.7, 8, 9 The European Resuscitation Council (ERC) recommends ventilating OHCA patients at a rate of 8–12 per minute and a tidal volume (Vt) of 500–600 ml.10 In the UK ventilation during CPR is commonly provided using a bag valve mask (BVM), supraglottic airway device or endotracheal tube (ETT). A recent simulation study suggests rescuers frequently deliver ventilations outside of recommendations,11 and often deliver excessive ventilation rates during advanced life support (ALS).12 This is associated with decreased cardiac output with increased intrathoracic pressure, impaired haemodynamics and cerebral vasoconstriction,11, 13 and is deleterious to survival.14 Currently it is challenging to manually deliver accurate ventilations consistent with recommendations and until very recently there has been no method to measure ventilation rate and tidal volume during OHCA resuscitation.
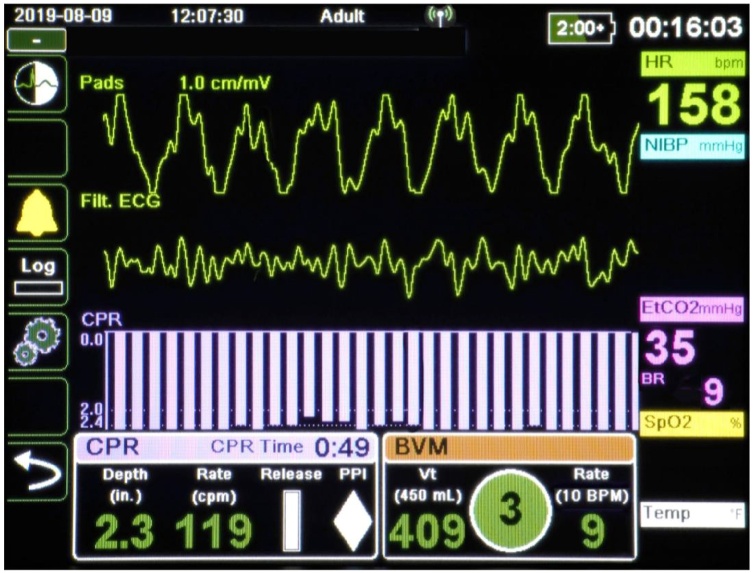
Zoll Medical Corporation has developed a non-invasive, real-time ventilation feedback device (VFD) to inform clinicians about the rate of ventilation and the tidal volume delivered during resuscitation. The VFD sensor is placed between the catheter mount and supraglottic or ETT airway (Image 1) and displays real time visual colour coded feedback on the defibrillator screen (Image 2). An onscreen prompt tells rescuers when to ventilate and when the Vt has been exceeded or under delivered. Prompts present in green when ventilations are compliant with recommendations and allows rescuers to respond to any over or under delivery of ventilations. There is no audio feedback given to the rescuer.
Image 1.
Ventilation feedback device.
Image 2.
Real time ventilation on screen feedback.
The aim of the study was to establish the clinical impact of the Zoll VFD on clinician compliance with ERC recommendations. Due to the lack of baseline data on ventilation quality and the absence of evidence on the impact of this technology on clinical practice we tested the VFD in OHCA scenarios using a mannequin.
Methods
Ambulance clinicians attending annual mandatory training sessions at North East Ambulance Service NHS Foundation Trust (NEAS) training centre during September 2020 were approached regarding study participation. Ambulance clinicians were either paramedics, or non-paramedics (Emergency Medical Technicians or Clinical Care Assistants who are non- registered ambulance personnel responsible for assisting and supporting paramedic delivered care). Eligible for inclusion were all clinicians aged ≥18 years who perform CPR as part of part of their clinical role and who had completed an internal ALS refresher which was part of their mandatory training session. All volunteers were given information regarding the study and provided written, informed consent prior to participation followed. Participants worked in pairs to complete the OHCA scenarios described below. After scenario completion participants were asked to complete a short questionnaire regarding the VFD.
OHCA scenarios
OHCA scenarios were conducted in a stationary NEAS training ambulance using a mannequin situated on the ambulance stretcher. The mannequin had a supraglottic airway in situ with the VFD and catheter mount connected to the BVM. In addition, defibrillator and CPR feedback pads were attached. A Zoll X Series defibrillator, which is in use in all NEAS front-line ambulances, was positioned in the usual place in the ambulance in view of both clinicians.
Each pair of clinicians completed ALS scenarios providing asynchronous chest compressions and ventilations over two 2-minute periods. During the first scenarios participants received compression quality feedback but were blinded to ventilation feedback, representing current practice. The clinicians were then introduced to the VFD and given a few minutes to familiarise themselves with it and the onscreen feedback.
Each pair of clinicians then undertook another two 2-minute scenarios providing asynchronous chest compressions and ventilations with real time ventilation feedback.
Each scenario was repeated so each participant had the opportunity to ventilate and provide chest compressions. Ventilation rate, tidal volume and chest compression quality were measured during both scenarios.
All scenarios were observed by one member of the research team, but no advice or support were provided once the scenarios were underway. Clinicians and researchers wore surgical face masks during the scenarios due to coronavirus restrictions.
Outcomes
The hypothesis was that the real time VFD would improve rescuer compliance with ERC recommendations. The primary outcome was the % difference in ventilation compliance with and without feedback. Compliance was defined as 8–12 ventilations per minute and tidal volume of 500–600 ml per ventilation.10 Secondary outcomes explored any differences between paramedic and non-paramedic clinicians and any impact on compliance with chest compression guidelines with the introduction of ventilation feedback. Chest compression compliance was defined as a rate of 100–120 compressions per minute, depth 5–6 cm and chest compression fraction >80%.10
Statistics
We hypothesised that the VFD would lead to a medium clinically important change (50%) in favour of improved ventilation compliance. Assuming statistical power (1 − β) of 95%, a significance level (α) of 5%, a medium effect size (0.5) and an odds ratio of 3, a minimum sample size of 98 participants was required. A McNemars test was used to compare the proportion of participants compliant with ventilation guidelines with and without ventilation feedback. Differences in compliance with chest compression recommendations were compared using a related samples wilcoxon signed rank test. Sample size calculations were determined using G*Power, version 3.1.9.2. Data were analysed using IBM SPSS Statistics v24.0.0.1.
Ethics
This study did not require approval from a research ethics committee as it only involved health professionals. Approval was sought and received from the Health Research Authority [IRAS ID 279472 dated 01/06/2020] and North East Ambulance Service (NEAS) NHS Foundation Trust Research & Development department.
Results
During September 2020, 118 NEAS clinicians participated in this study, 12 were excluded because of missing or incomplete data, resulting in 106 participants included in the analysis. The mean age of participating clinicians was 42 years (SD 10, range 23–64), 45/106 (42%) were female, mean length of service was 12 years (SD 8, range 1–33), 78/106 (74%) were paramedics and 28/106 (26%) were non-paramedic clinicians. Mean number of times ventilation support was performed by study participants in the last 12 months was 11 (SD 13, range 0–80) (n = 100).
The median ventilation rate was 10 per minute (IQR 8–14, range 4–30) without feedback compared to 9 (IQR 9–9, range 6–17) with feedback (Fig. 1). The median tidal volume without feedback was 630mls (IQR 518–725, range 201–1114) compared to 546mls (IQR 531–560, range 490–750) with feedback (Fig. 2). The proportion of clinicians who delivered ventilations at a rate and tidal volume within ERC guidelines were significantly greater with feedback, 96/106 (91%), compared to 10/106 (9%) without, (McNemars test p = <0.0001). The VFD was able to remove the extremes of hypo or hyperventilation, ensuring standardised ventilations were delivered (Table 1).
Fig. 1.
Ventilation rate with and without feedback.
Fig. 2.
Tidal volume (ml) with and without ventilation feedback.
Table 1.
Tidal volume, ventilation rate and chest compression quality.
| Without feedback | With feedback | p Value | |
|---|---|---|---|
| Tidal volume | |||
| Hypoventilation | 22 (20.75%) | 3 (2.83%) | |
| Within recommendations | 24 (22.65%) | 100 (94.34%) | |
| Hyperventilation | 60 (56.60%) | 3 (2.83%) | |
| Median tidal volume (mls) | 630 (IQR 518–725, range 201–1114) | 546 (IQR 531–560, range 490–750) | |
| Ventilation rate | |||
| Hypoventilation | 13 (12.20%) | 2 (1.88%) | |
| Within recommendations | 54 (51%) | 100 (94.34%) | |
| Hyperventilation | 39 (36.80%) | 4 (3.78%) | |
| Median ventilation rate (per minute) | 10 (IQR 8–14, range 4–30) | 9 (IQR 9–9, range 6–17) | |
| Compression quality (% of participants in range of recommendations) | |||
| Median depth | 73% | 76% | 0.151 |
| Median rate | 19% | 40% | 0.009 |
| Median fraction | 100% | 100% | 0.493 |
The ability to deliver ventilations and tidal volume compliant with guidelines differed significantly between clinical role. In the absence of ventilation feedback, 12% paramedics compared to 4% non-paramedics achieved compliancy >50% (McNemars test p = <0.0001). With ventilation feedback 94% of paramedics compared to 82% of non-paramedics achieved compliancy >50% (McNemars test p = 0.001).
Participants delivered chest compressions more compliant with ERC guidelines in the second scenarios when the VFD was used.
Participants compliance with chest compression rate guidelines did not change significantly (73% without vs. 76% with, p = 0.151) and the chest compression fraction was unchanged (100% vs. 100%, p = 0.493). Compliance with chest compression depth guidelines significantly increased in the second scenarios (19% without vs. 40% with, p = 0.009).
Study participants (98%) overwhelmingly found the VFD to be of benefit and almost all participants (99%) said they would use the VFD most, or all, of the time (Table 2).
Table 2.
Participant feedback on the VFD.
| Do you think that the ventilation feedback device is beneficial? (n = 104) | |||
|---|---|---|---|
| Yes | No | Unsure | |
| Total | 102 (98%) | 1 (1%) | 1 (1%) |
| Would you use the ventilation feedback device in practice? (n = 103) | |||||
|---|---|---|---|---|---|
| Never | Rarely | Sometimes | Most of the time | Always | |
| Total | 0 | 0 | 1 (1%) | 14 (14%) | 88 (85%) |
| Was the brief explanation sufficient to use the ventilation feedback device? (n = 103) | |||
|---|---|---|---|
| Not enough | Sufficient | More than enough | |
| Total | 0 | 36 (35%) | 67 (65%) |
| How did you find applying the feedback from the device in practice? (n = 104) | |||||
|---|---|---|---|---|---|
| Very difficult | Difficult | Neutral | Easy | Very easy | |
| Total | 0 | 0 | 4 (4%) | 24 (23%) | 76 (73%) |
Discussion
This study has given an insight into how professional rescuers provide ventilation support (tidal volume and ventilation rate) during simulated ALS. Most rescuers delivered ventilations outside of recommendations when no real time feedback was provided. A significant improvement was observed when the VFD was used with a notable decrease in tidal volume. Delivering optimum tidal volume and ventilation rates is challenging in the out of hospital environment and it has been difficult to measure the quality of ventilation support provided until recently. This associated with a misperception of patient ventilation requirements during OHCA may explain why hyperventilation is commonplace in paramedic practice.
This study demonstrated clinician baseline ventilation support rarely complies with international recommendations, regardless of clinical role or skills, but that a VFD can improve both the tidal volume and ventilation rate delivered during OHCA scenarios. These findings are not unique to the participants in our study or to UK paramedic practice. In a recent US study, 106 paramedic rescue teams comprising four participants attending scheduled training sessions, undertook simulated basic life support (BLS) resuscitation scenarios.15 Laerdal Debrief Viewer software recorded ventilation rate, tidal volume and minute ventilation but rescuers were unaware they were being observed and no feedback was provided. Only 3/106 (2.8%) provided ventilations within target, 26/106 (24.5%) delivered between 7–10 ventilations per minute, and 18/106 (17.0%) delivered tidal volume between 500–600 ml, demonstrating rescuer ventilations were frequently outside of recommendations.
Khoury et al. (2019) enrolled 40 healthcare professionals from France responsible for delivering CPR into a randomised crossover manakin based study to evaluate a VFD. Initial ventilation compliance was poor with all rescuers but the device improved ventilations with a BVM from 15% to 90% and with an ETT from 15% to 85%.16
Gould et al. (2020) found similar results when they used a VFD to improve poor rescuer performance when delivering ventilations. Ventilation rates improved from 41–71% and tidal volume from 31% to 78%.17
The effect of delivering ventilations during OHCA outside of recommendations are well documented and are known to reduce coronary perfusion pressure,18, 19 increase pulmonary vascular resistance and decrease cardiac output.20
Aufderheide et al. (2004) conducted a porcine study to determine the association between hyperventilation increased mortality.19 In their cardiac arrest model, they demonstrated a reduction in ventilation rate from 30 breaths per minute to 12, with 100% oxygen, increased survival rate from 17% to 86%.
Given that participants in this study were experienced clinicians undertaking a variety of clinical roles, who regularly ventilate patients in clinical practice, many were naive to the unintended consequences of delivering ventilations outside of recommendations. Non paramedic clinicians were the least compliant with recommendations with and without ventilation feedback, and yet it is suggested responsibility for ventilation is often assigned to the most junior clinician.20 It is well known that OHCA produces acute acidosis and many rescuers may believe hyperventilation is unharmful and indeed, may believe it to be beneficial.21 This may partly explain why hyperventilation appears commonplace in many emergency medical systems. We believe the ventilations delivered to the simulated patient in our study accurately reflects true clinical practice. In a real OHCA when clinicians are multi-tasking, adrenaline is flowing and feedback is unavailable, we believe ventilations are likely to be less compliant with recommendations than in these simulated scenarios. This has obvious implications for training delivered by NHS ambulance services as there are potential patient safety issues associated with hyperventilation, and professional rescuer training needs to focus on how to deliver quality ventilations in accordance with recommendations.
The improvement in ventilation quality using the VFD did not sacrifice the quality of chest compressions, rather the calibre of chest compressions delivered during the scenario improved.
This has been observed on other studies17, 21 and may be as a result of rescuers paying increased attention to the real time feedback displayed on the defibrillator or as a result of a learning effect where rescuers become more effective as the resuscitation evolves.
Participants received very little familiarisation with the VFD and were afforded only a few minutes to run through its use and the visual feedback. Despite this, clinician performance was significantly improved suggesting the VFD was easy to use and intuitive.
The clinicians involved in this study believed the VFD was beneficial and said they would frequently use it. This serves to demonstrate the acceptability of such a device in paramedic practice and enforces the need to explore the use of VFDs further.
In addition, it supports the notion that such a device is required by ambulance clinicians to improve the quality of ventilations they deliver.
Limitations
We have demonstrated clinicians involved in our study regularly delivered tidal volume and ventilation rates outside of recommendations and that this can be effectively remedied with the VFD but there are limitations to our study. Resuscitation scenarios were conducted in an ambulance with the mannikin situated on a stretcher.
In UK clinical practice, resuscitation rarely takes place in an ambulance, rather, ALS is delivered at the patients’ side, where CPR is known to be much more effective. The data collected during the resuscitation scenarios was designed to reflect the real world, but we were unable to reproduce the urgency and stresses of a real OHCA, or the adrenaline-driven responses experienced by rescuers which may influence the quality of care delivered. Participants were aware of the study aims prior to participation and may have adjusted their behaviour in response to this knowledge, however, given that many participants ventilated outside of recommendations, this is unlikely to have unduly influenced participants. Resuscitation scenarios were observed by at least one member of the research team which may have altered participants performance.
The design of the study required participants to take part in two scenarios, one with and one without the VFD. This gave participants the opportunity to practice the scenario, therefore the improvement in performance could be related in part to this opportunity and not just as a result of the VFD.
A similar effect may have been observed in the improvement in compression quality witnessed with the VFD. Furthermore, participants who provided ventilations second may have been influenced, or may have benefited, from observing the performance of the first participant.
The short duration of the scenarios and the lack of additional tasks and distractors also limit the applicability of these findings to real practice.
The significance of the findings are limited to the simulated patient. True patient-based studies are required to determine how the VFD can be accommodated in practice and its potential to affect patient outcomes.
Conclusion
Ambulance clinician baseline ventilation quality is frequently outside of recommendations. The use of a VFD can significantly improve the tidal volume and rate of ventilation to within evidence based recommendations.
Further research is required to validate the use of the VFD in true clinical practice and to evaluate the relationship between improved ventilation quality during OHCA and patient outcomes.
Ethical statement
This study did not require approval from a research ethics committee as it only involved health professionals. Approval was sought and received from the Health Research Authority [IRAS ID 279472 dated 01/06/2020] and North East Ambulance Service (NEAS) NHS Foundation Trust Research & Development department.
Declaration of interests
None declared.
Author contributions
KC and GM conceived and designed the study, hosted the clinical scenarios and collected data. GM analysed data. KC wrote the paper and GM provided critical review and comment. KM supported delivery of the clinical scenarios and reviewed the paper. DH, PAF and MN supported the study and reviewed the paper.
Funding
Zoll Medical Corporation provided defibrillators and the VFD but had no part in delivery of the project or preparation of this article. There was no additional funding associated with this research. The study team acknowledges the support of the National Institute for Health Research Clinical Research Network (NIHR CRN) North East and North Cumbria (NENC).
Data and materials
Study data involved is available upon reasonable request.
Contributor Information
Karl Charlton, Email: E-Karl.Charlton@neas.nhs.uk.
Graham McClelland, Email: E-Graham.McClelland@neas.nhs.uk.
Karen Millican, Email: E-Karen.Millican@neas.nhs.uk.
Daniel Haworth, Email: E-Daniel.Haworth@neas.nhs.uk.
Paul Aitken-Fell, Email: E-Paul.Aitken-Fell@neas.nhs.uk.
Michael Norton, Email: E-Michael.Norton@neas.nhs.uk.
References
- 1.Mawani M., Kadir M.M., Azam I. Epidemiology and outcomes of out-of-hospital cardiac arrest in a developing country-a multicenter cohort study. BMC Emerg Med. 2016;1:16(1):28. doi: 10.1186/s12873-016-0093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perkins G.D., Brace-McDonnell S.J. The UK out of hospital cardiac arrest outcome (OHCAO) project. BMJ Open. 2015;1:5. doi: 10.1136/bmjopen-2015-008736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kramer-Johansen J., Myklebust H., Wik L. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;1;71(3):283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 4.Handley A.J., Handley S.A. Improving CPR performance using an audible feedback system suitable for incorporation into an automated external defibrillator. Resuscitation. 2003;1;57(1):57–62. doi: 10.1016/s0300-9572(02)00400-8. [DOI] [PubMed] [Google Scholar]
- 5.Boyle A.J., Wilson A.M., Connelly K., McGuigan L., Wilson J., Whitbourn R. Improvement in timing and effectiveness of external cardiac compressions with a new non-invasive device: the CPR-Ezy. Resuscitation. 2002;1;54(1):63–67. doi: 10.1016/s0300-9572(02)00049-7. [DOI] [PubMed] [Google Scholar]
- 6.Charbonney E., Grieco D.L., Cordioli R.L., Badat B., Savary D., Richard J.C. Ventilation during cardiopulmonary resuscitation: what have we learned from models? Respir Care. 2019;1;64(9):1132–1138. doi: 10.4187/respcare.06998. [DOI] [PubMed] [Google Scholar]
- 7.Dorph E., Wik L., Stromme T.A., Eriksen M., Steen P.A. Oxygen delivery and return of spontaneous circulation with ventilation:compression ratio 2:30 versus chest compressions only CPR in pigs. Resuscitation. 2004;60(3):309–318. doi: 10.1016/j.resuscitation.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Chandra N.C., Gruben K.G., Tsitlik J.E. Observations of ventilation during resuscitation in a canine model. Circulation. 1994;90(6):3070–3075. doi: 10.1161/01.cir.90.6.3070. [DOI] [PubMed] [Google Scholar]
- 9.Idris A.H., Banner M.J., Wenzel V., Fuerst R.S., Becker L.B., Melker R.J. Ventilation caused by external chest compression is unable to sustain effective gas exchange during CPR: a comparison with mechanical ventilation. Resuscitation. 1994;28(2):143–150. doi: 10.1016/0300-9572(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 10.Soar J., Nolan J.P., Bottiger B.W. European Resuscitation Council Guidelines for Resuscitation 2015. Section 3. Adult advanced life support. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 11.Khoury A., Sall F.S., De Luca A. Evaluation of bag-valve-mask ventilation in manikin studies: what are the current limitations? Biomed Res Int. 2016 doi: 10.1155/2016/4521767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Neill J.F., Deakin C.D. Do we hyperventilate cardiac arrest patients? Resuscitation. 2007;1;73(1):82–85. doi: 10.1016/j.resuscitation.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Karlsson T., Stjernström E.L., Stjernström H., Norlen K., Wiklund L. Central and regional blood flow during hyperventilation: an experimental study in the pig. Acta Anaesthesiol Scand. 1994;38(2):180–186. doi: 10.1111/j.1399-6576.1994.tb03863.x. [DOI] [PubMed] [Google Scholar]
- 14.Aufderheide T.P., Sigurdsson G., Pirrallo R.G. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;27;109(16):1960–1965. doi: 10.1161/01.CIR.0000126594.79136.61. [DOI] [PubMed] [Google Scholar]
- 15.Neth M.R., Benoit J.L., Stolz U., McMullan J. Ventilation in simulated out-of-hospital cardiac arrest resuscitation rarely meets guidelines. Prehosp Emerg Care. 2020;24:1–9. doi: 10.1080/10903127.2020.1822481. [DOI] [PubMed] [Google Scholar]
- 16.Khoury A., De Luca A., Sall F.S., Pazart L., Capellier G. Ventilation feedback device for manual ventilation in simulated respiratory arrest: a crossover manikin study. Scand J Trauma Resusc Emerg Med. 2019;1;27(1):93. doi: 10.1186/s13049-019-0674-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gould J.R., Campana L., Rabickow D., Raymond R., Partridge R. Manual ventilation quality is improved with a real-time visual feedback system during simulated resuscitation. Int J Emerg Med. 2020;13:1–5. doi: 10.1186/s12245-020-00276-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Prost N., Ricard J.D., Saumon G., Dreyfuss D. Ventilator-induced lung injury: historical perspectives and clinical implications. Ann Intensive Care. 2011;1(1):1–5. doi: 10.1186/2110-5820-1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aufderheide T.P., Lurie K.G. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32(9):345–351. doi: 10.1097/01.ccm.0000134335.46859.09. [DOI] [PubMed] [Google Scholar]
- 20.Pitts S., Kellermann A.L. Hyperventilation during cardiac arrest. Lancet. 2004;24;364(9431):313–315. doi: 10.1016/S0140-6736(04)16740-8. [DOI] [PubMed] [Google Scholar]
- 21.Crowe C., Bobrow B.J., Vadeboncoeur T.F. Measuring and improving cardiopulmonary resuscitation quality inside the emergency department. Resuscitation. 2015;1;93:8–13. doi: 10.1016/j.resuscitation.2015.04.031. [DOI] [PubMed] [Google Scholar]