Abstract
Aims
We hypothesized that a decline in admissions with heart failure during COVID-19 pandemic would lead to a reciprocal rise in mortality for patients with heart failure in the community.
Methods and results
We used National Heart Failure Audit data to identify 36 974 adults who had a hospital admission with a primary diagnosis of heart failure between February and May in either 2018, 2019, or 2020. Hospital admissions for heart failure in 2018/19 averaged 160/day but were much lower in 2020, reaching a nadir of 64/day on 27 March 2020 [incidence rate ratio (IRR): 0.40, 95% confidence interval (CI): 0.38–0.42]. The proportion discharged on guideline-recommended pharmacotherapies was similar in 2018/19 compared to the same period in 2020. Between 1 February–2020 and 31 May 2020, there was a 29% decrease in hospital deaths related to heart failure (IRR: 0.71, 95% CI: 0.67–0.75; estimated decline of 448 deaths), a 31% increase in heart failure deaths at home (IRR: 1.31, 95% CI: 1.24–1.39; estimated excess 539), and a 28% increase in heart failure deaths in care homes and hospices (IRR: 1.28, 95% CI: 1.18–1.40; estimated excess 189). All-cause, inpatient death was similar in the COVID-19 and pre-COVID-19 periods [odds ratio (OR): 1.02, 95% CI: 0.94–1.10]. After hospital discharge, 30-day mortality was higher in 2020 compared to 2018/19 (OR: 1.57, 95% CI: 1.38–1.78).
Conclusion
Compared with the rolling daily average in 2018/19, there was a substantial decline in admissions for heart failure but an increase in deaths from heart failure in the community. Despite similar rates of prescription of guideline-recommended therapy, mortality 30 days from discharge was higher during the COVID-19 pandemic period.
Keywords: Heart failure, Acute heart failure, COVID-19, Hospitalization, Mortality
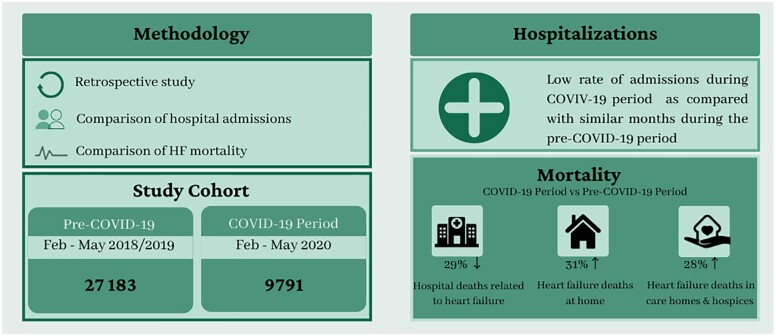
Graphical Abstract
Key questions
What is already known about this subject?
A decline in admission for many cardiovascular diseases was observed during first wave of COVID-19 pandemic.
What does this study add?
The reduction in heart failure admissions during the COVID-19 pandemic was accompanied by an increase in heart failure deaths in the community and 30-day after discharge.
How might this impact on clinical practice
Novel models of care at home and in the community should be explored for patients with heart failure during the COVID-19 pandemic, with public health messages towards this group of patients aimed at seeking medical assistance in the event of illness.
Introduction
Healthcare systems across the globe were restructured during the COVID-19 pandemic in anticipation of a large influx of emergency admissions. This reconfiguration resulted in closure of elective and out-patient services, reductions in speciality beds and the relocation of cardiology staff to other high-dependency areas of the hospital.1,2 Such measures may have affected both the provision of healthcare to patients with heart failure as well as their outcomes.
During the early and peak phases of the first wave of the COVID-19 pandemic, hospitals in the United Kingdom (UK) described a decline in admissions for many cardiovascular conditions, including heart failure.3,4 These reports are limited because they are either based on the activity of a small number of centres, lack granularity about treatments and processes of care, or do not report outcomes following hospital discharge.5
We hypothesized that a decline in admissions with heart failure would lead to a reciprocal rise in mortality for patients with heart failure in the community. England has a suite of clinical and administrative datasets that routinely collect detailed health information and outcomes for the population. We used such multi-sourced and linked electronic health records from the National Heart Failure Audit (NHFA), Hospital Episode Statistics (HES), and the Civil Registration of Death Data of the Office for National Statistics (ONS) to quantify the extent and impact of changes in admissions for heart failure and understand whether in-hospital management of patients and their post-discharge outcomes have been affected as a result of the COVID-19 pandemic.
Methods
The current study was based on English data from three national databases: NHFA, HES, and the Civil Registration of Deaths, ONS (Supplementary material online, Figures S1 and S2). The datasets used in this analysis are available through NHS digital on reasonable request with permission from relevant authorities. The first confirmed case of coronavirus in England was on 29 January 2020; thus, we took 1 February 2020 as the start date of the COVID-19 period.
The National Heart Failure Audit
The NHFA was established in 2007 for hospitals in England and Wales to monitor and improve the quality of care of patients admitted to hospital with a diagnosis of heart failure, capturing information on their clinical presentation, characteristics, investigations, specialist input, management, and outcomes in the real world.6,7 Further details about NHFA is presented in Supplementary material online, Method section. For the purpose of this analysis, we included data relating to an admission with a diagnosis of heart failure from 1 January 2018 to 31 May 2020 from England. We dichotomized study participants on the basis of their date of index hospitalization: COVID-19 period (1 February–31 May 2020) and pre-COVID-19 period (1 February–31 May 2018 and 1 February–31 May 2019). Furthermore, we excluded hospitals that did not submit data consistently each month during this period. We only included the first admission for heart failure during the whole study period (a patient could potentially be hospitalized more than once). Records with missing data for sex and National Health Service (NHS) identification number were excluded.
Hospital episode statistics
HES collects data for all hospital admissions, outpatient appointments and accident and emergency attendances for all NHS hospitals in England. HES data were extracted for the same study period as NHFA data. Index admissions for heart failure were identified using International Classification of Diseases (ICD)-10 recorded in the primary position. HES data are more complete, since they included patients from hospitals not include in the above NHFA dataset, and were used to calculate the daily rate of admissions for heart failure.
Civil registration of death
The Civil Registration of Deaths, ONS dataset comprises mortality information for all deaths in England. Deaths certification and registration is a legal requirement in the UK and a doctor who has seen the deceased during the last 14 days of life must complete a medical certificate of causes of death (MCCD) within 5 days unless a post-mortem examination or inquest is organized. During the COVID-19 pandemic, emergency guidance enabled any doctor in the UK (not just the attending) to complete the medical certificate of cause of death, the duration of time over which the deceased was not seen before referral to the coroner was extended from 14 to 28 days and causes of death could be ‘to the best of their knowledge and belief’ without diagnostic proof, if appropriate and to avoid delay. ICD-10 codes, corresponding to the principal and contributory causes of death on the MCCD, were used to identify deaths from heart failure. Individual patient data from the NHFA were linked using each patient’s unique NHS identification number to the ONS dataset to track mortality for 30 days from hospital discharge; this also allowed mortality within 30 days of admission to be calculated. We also collected ONS data for all adult deaths in England. We reported daily deaths for heart failure recorded in the primary position and in any position.
Rationale for using multiple databases
Each dataset utilized in this study has its own strengths and limitations and only a combination of datasets or linkage analysis can give a comprehensive overview of the impact of COVID-19 on heart failure services, and serve to validate our findings using more than one dataset. In summary, the NHFA dataset is the national heart failure dataset that was used to describe clinical characteristics, pharmacotherapy, and mortality during index admission and its linkage with ONS dataset provided further information about mortality during 30-day after admission and cause of death. The NHFA captures approximately 70% of total heart failure admissions captured in HES, which is an administrative dataset of all hospital admissions in the UK that we used to describe the overall rate of hospitalizations for heart failure. However, HES as an administrative dataset, lacks granular details around processes of care, and treatments of heart failure. Therefore, we used a combination of these two databases, to better define clinical pathways, treatments, admission rates and outcomes.
Outcomes
The main outcomes of interest were in-hospital all-cause mortality, 30-day all-cause mortality (measuring from the date of hospital admission), and the daily incidence of heart failure-related deaths by place of death up until 14 July 2020.
Statistical methods
Daily admissions and deaths from heart failure were depicted using a 7-day simple moving average (the mean number of daily deaths for that day and the preceding 6 days) from 1 February to 31 May of each year. Poisson regression was used to estimate the incidence rate ratio (IRR) of daily deaths related to heart failure during the pre-COVID-19 and COVID-19 periods, adjusted for time trends by including a cubic spline function of time. We calculated the excess deaths by subtracting the observed total deaths from March 2020 to the average total deaths in 2018 and 2019 in the same period.
Continuous data were presented as medians with interquartile ranges (IQRs), and categorical variables were presented as counts and proportions. We tested differences between the groups using the Chi-squared test for non-parametric data, Student’s T test for normally distributed continuous variables and Wilcoxon rank sum test where continuous data were not normally distributed.
For the NHFA, we used multiple imputation with chained equations to impute data for all variables with missing information. Multivariable logistic regression models were fit to estimate the risk of death for the COVID-19 and pre-COVID-19 periods. In a sensitivity analysis, we repeated the multivariable logistic regression analysis for 30-day mortality amongst patients discharged alive during each period (Supplementary material online, Method section for more details).
Analyses were performed using the Stata/MP 16.1 statistical software (College Station, TX, USA) and R version 4.0.0. All statistical analyses were two-tailed, and an alpha of 5% used throughout.
Ethics
All datasets used in our study collect information routinely used for audit research purposes without requiring informed patient consent fall under section 251 of the NHS Act 2006 and therefore institutional board review was not required for this study.8,9 The UK Secretary of State for Health and Social Care has released a time limited Notice, under Regulation 3(4) of the NHS (Control of Patient Information Regulations) 2002, to analyse confidential patient information. This study is a part of work stream authorized by the Scientific Advisory Group for Emergencies (SAGE), the body accountable for ensuring that appropriate and coordinated scientific advice is made available to UK government decision makers. SAGE helps UK cross-government decisions in the Cabinet Office Briefing Room and by NHS England, which supervises commissioning decisions in the NHS, and NHS Improvement, which is responsible for overseeing quality of care in NHS hospitals.
Results
Admissions with heart failure
There were 36 974 index events available from the NHFA, of which 27 183 (74%) occurred in pre-COVID-19 years and 9791 (26%) during the COVID-19 period (Supplementary material online, Figures S1 and S2). In the HES record, the total number of index admissions for heart failure was 38 470 and 14 150 for the same three time-periods.
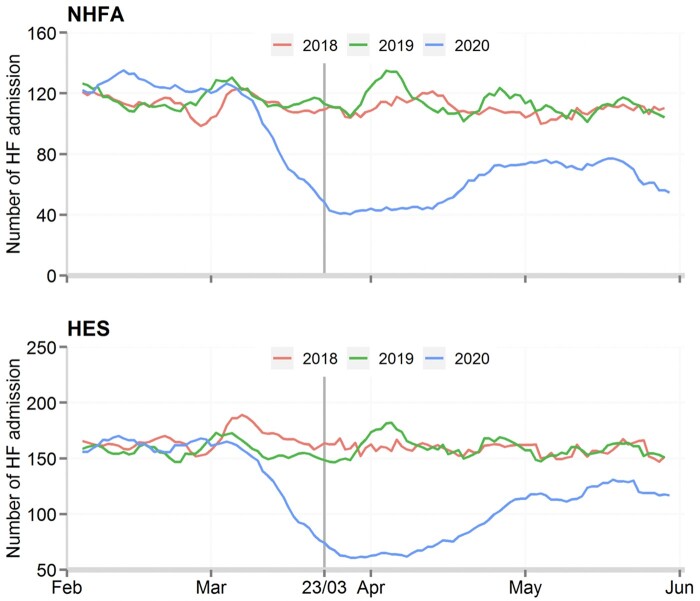
There was a decline in daily admissions for heart failure [NHFA: from 112 to 60 per day; IRR: 0.53, 95% confidence interval (CI): 0.52–0.55] (HES: from 157 to 92 per day; IRR: 0.60, 95% CI: 0.59–0.62) from the middle of March 2020 compared with daily admissions in the same period in 2018/2019. Thereafter, there was a persistently low rate of admissions as compared with similar months during the pre-COVID-19 period (Figure 1). These trends were similar across age groups, sex, and heart failure categories (Supplementary material online, Figures S3 and S4). There were similar distributions of ages, sex, and heart failure categories in patient cohorts admitted during the COVID-19 and pre-COVID-19 periods (Table 1). The prevalence of a prior history of hypertension, diabetes mellitus, valvular heart disease, asthma, chronic obstructive pulmonary disease, and cerebrovascular accident were similar. Patients admitted during the COVID-19 period had higher plasma concentrations of brain natriuretic peptide (BNP) or N-terminal brain natriuretic peptide (NT-Pro BNP) and a similar prevalence of atrial fibrillation and heart failure with reduced ejection fraction (HFrEF) relative to those admitted during the pre-COVID-19 era (Table 1). Prescription of pharmacotherapy was broadly similar between the two cohorts (Table 1). The median length of hospital stay was 7 days (IQR 3–13) during the COVID-19 period and 8 days (IQR 4–15) during the pre-COVID-19 period.
Figure 1.
Daily number of heart failure hospitalizations between 1 February and 31 May 2018, 2019 and 2020. Each curve represents a 7-day rolling average of daily heart failure hospitalizations. A decline in daily admissions for heart failure (NHFA: from 112 to 60 per day: IRR: 0.53, 95% CI: 0.52–0.55; HES: from 157 to 92 per day; IRR: 0.60, 95% CI: 0.59–0.62) from the middle of March 2020. There was a persistently low rate of admissions as compared with similar months during the pre-COVID-19 period. CI, confidence interval; COVID-19 period, February–May 2020; HES, Hospital Episode Statistic; IRR, incidence rate ratio; NHFA, National Heart Failure Audit; Pre-COVID-19 period, February–May 2018 and February–May 2019.
Table 1.
Baseline characteristics of patients admitted for heart failure during the pre-COVID-19 and COVID-19 periods (data derived from NHFA database)
| Variables | Pre-COVID-19 period | COVID-19 period | P-value |
|---|---|---|---|
| Number of patients | 27 183 | 9791 | |
| Age (IQR) | 80 (71–87) | 80 (71–87) | 0.47 |
| Women (%) | 11 925 (44%) | 4267 (44%) | 0.62 |
| Race | |||
| White | 12 985 (76%) | 4769 (79%) | <0.001 |
| BAME | 4046 (24%) | 1265 (21%) | <0.001 |
| Location of inpatient care | |||
| Cardiology | 11 281 (42%) | 3871 (40%) | 0.001 |
| General medicine | 9091 (33%) | 3344 (34%) | |
| Geriatric medicine | 4097 (15%) | 1477 (15%) | |
| Other | 2671 (10%) | 1071 (11%) | |
| NYHA Class at the time of hospitalization | |||
| Class 1 | 1550 (6%) | 654 (7%) | <0.001 |
| Class 2 | 4007 (15%) | 1359 (14%) | |
| Class 3 | 11 957 (46%) | 4495 (48%) | |
| Class 4 | 8525 (33%) | 2877 (31%) | |
| Peripheral oedema | |||
| No oedema | 5535 (22%) | 2137 (23%) | <0.001 |
| Mild oedema | 6185 (24%) | 1947 (21%) | |
| Moderate oedema | 8638 (34%) | 3150 (34%) | |
| Severe oedema | 5341 (21%) | 1951 (21%) | |
| Pre-existing co-morbid conditions | |||
| CAD | 10 917 (41%) | 3655 (39%) | <0.001 |
| Valve disease | 7670 (29%) | 2667 (28%) | 0.09 |
| Hypertension | 14 991 (56%) | 5443 (56%) | 0.35 |
| Diabetes mellitus | 9312 (35%) | 3263 (34%) | 0.13 |
| Asthma | 2447 (9%) | 917 (10%) | 0.25 |
| COPD | 2812 (18%) | 1678 (18%) | 0.23 |
| Prior device therapy | |||
| CRT-D/CRT-P | 1256 (5%) | 386 (4%) | 0.09 |
| ICD | 728 (3%) | 267 (3%) | |
| PPM | 2490 (9%) | 890 (9%) | |
| In-hospital clinical investigations | |||
| Heart rate at admission (beat/min) (IQR) | 83 (70–100) | 84 (71–101) | 0.002 |
| Systolic BP at admission (IQR) | 130 (111–149) | 130 (112–151) | 0.001 |
| Haemoglobin at discharge (g/dL) (IQR) | 12 (10–13) | 12 (10–13) | 0.89 |
| Creatinine at discharge (mg/dL) (IQR) | 108 (83–148) | 106 (82–147) | 0.01 |
| Serum Na at discharge (mmol/L) (IQR) | 138 (135–141) | 138 (135–141) | 0.77 |
| Plasma BNP during hospitalization (ng/L) (IQR) | 570 (82–1515) | 761 (263–1927) | <0.001 |
| Plasma NT-proBNP (ng/L) (IQR) | 4526 (1897–10 417) | 5046 (2198–11 372) | <0.001 |
| QRS interval (ms) | 106 (91–138) | 106 (91–136) | 0.67 |
| AF on ECG (%) | 11 827 (47%) | 4305 (47%) | 0.27 |
| HFrEF (%) | 14 371 (53%) | 5101 (52%) | 0.20 |
| Valve disease (%) | 8999 (33%) | 3208 (33%) | 0.55 |
| Echocardiogram performed during hospitalization | 23 935 (88%) | 8513 (87%) | 0.005 |
| Length of stay, pharmacotherapy at discharge and discharge planning | |||
| Length of hospital stay (IQR) | 8 (4–15) | 7 (3–13) | <0.001 |
| ACEi/ARB (%) | 12 738 (72%) | 4527 (74%) | 0.001 |
| Beta blockers (%) | 17 219 (85%) | 6234 (87%) | 0.001 |
| Loop diuretics (%) | 21 747 (94%) | 7784 (94%) | 0.65 |
| Thiazide diuretics (%) | 911 (6%) | 281 (5%) | 0.39 |
| MRA (%) | 8348 (50%) | 2945 (53%) | 0.001 |
| Digoxin (%) | 3633 (21%) | 1269 (22%) | 0.19 |
| Median weight loss during hospitalization (kg) (IQR) | −2.1 (−5.7 to 0) | −1.80 (−5.4 to 0) | 0.001 |
| Heart failure nurse follow-up (%) | 13 923 (58%) | 4969 (57%) | 0.46 |
| Cardiology follow-up (%) | 10 749 (45%) | 3615 (42%) | <0.001 |
ACEi, angiotensin-converting enzyme inhibitor; AF, atrial fibrillation; ARB, angiotensin receptor blockers; BAME, Black, Asian & Minority ethnic; BNP, brain natriuretic peptide; BP, blood pressure; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CRT, cardiac resynchronization therapy; CVA, cerebrovascular accident; ECG, electrocardiogram; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; ICD, implanted cardiac defibrillator; IQR, interquartile range; kg, kilogram; MRA, mineralocorticoid receptor antagonist; Na, sodium; NHFA, National Heart Failure Audit; NT-pro BNP, N-terminal pro type brain natriuretic peptide; NYHA, New York Heart Association; PPM, permanent pacemaker.
Deaths
Location and number of deaths (heart failure as a cause of death at primary position)
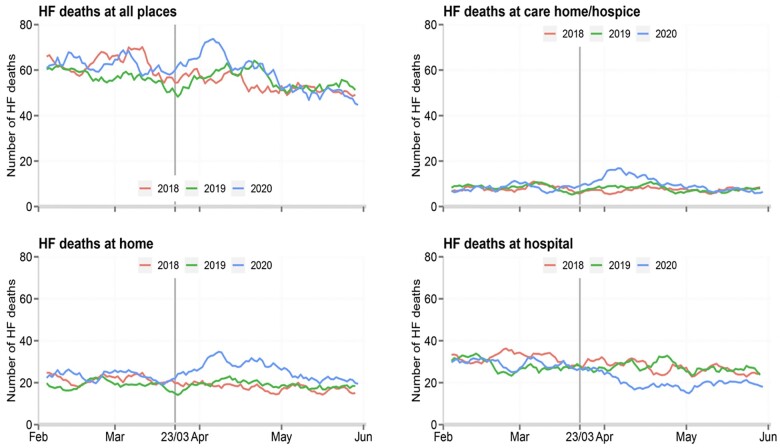
The numbers of deaths reported by ONS with heart failure as the primary cause were 6900, 6739, and 7187 between February and May in 2018, 2019, and 2020, respectively.
We observed an increase in deaths due to heart failure from middle of March to late April 2020 in the COVID-19 period compared with the pre-COVID period (Figure 2). There was a 29% decline in deaths related to heart failure in hospital (IRR: 0.71, 95% CI: 0.67–0.75, equivalent to a decrease of 448 deaths), a 31% increase in deaths at home (IRR: 1.31, 95% CI: 1.24–1.39, equivalent to an increase of 539 deaths), and a 28% increase in deaths in care homes and hospices (IRR: 1.28, 95% CI: 1.18–1.40, equivalent to an increase of 189 deaths). In total, we estimate an excess of 280 deaths from heart failure during the COVID-19 study period.
Figure 2.
Comparison of daily deaths in hospital, home and care home/hospice during study period with heart failure certified as the primary cause. Each curve represents a 7-day rolling average of daily deaths. There was an increase in deaths due to heart failure from middle of March to late April 2020 in the COVID-19 period compared to pre-COVID-19 period. A 29% decline in deaths related to heart failure in hospital (IRR: 0.71, 95% CI: 0.67–0.75, equivalent to a decrease of 448 deaths), a 31% increase of deaths at home (IRR: 1.31, 95% CI: 1.24–1.39, equivalent to an increase of 539 deaths) and a 28% increase in deaths in care homes and hospices (IRR: 1.28, 95% CI: 1.18–1.40, equivalent to an increase of 189 deaths). CI, confidence interval; COVID-19 period, February–May 2020; HF, heart failure; IRR, incidence rate ratio; Pre-COVI-19 period: February–May 2018 and February–May 2019.
Mortality in patients admitted with heart failure captured by the NHFA
Inpatient deaths: All-cause, inpatient mortality was similar in the COVID-19 and pre-COVID-19 periods [10% in both groups, odds ratio (OR): 1.02, 95% CI: 0.94–1.10] (Table 2).
Table 2.
Crude data and adjusted odds of inpatient and 30-day mortality from admission during the COVID-19 vs. pre-COVID-19 period (data derived from Civil Registration of Death and NHFA databases)
| Outcome | Total | Pre-COVID-19 period | COVID-19 period | P-value |
|---|---|---|---|---|
| No of patients | 36 974 | 27 183 | 9791 | |
| All-cause inpatient mortality (%) | 3752 | 2752 (10%) | 1000 (10%) | 0.80 |
| All-cause 30-day mortality from date of admission (%) | 5033 | 3594 (13%) | 1439 (15%) | <0.001 |
| Multivariable logistic regression analysis on non-imputed data (complete case analysis) | ||||
| Outcome | ORa | Lower bound 95% CI | Upper bound 95% CI | P-value |
| Inpatient mortality (n = 21 036) | 1.02b | 0.91 | 1.13 | 0.73 |
| 30-day mortality from date of admission (n = 21 036) | 1.17c | 1.07 | 1.29 | 0.001 |
| Multivariable logistic regression analysis on imputed data | ||||
| Outcome | ORa | Lower bound 95% CI | Upper bound 95% CI | P-value |
| Inpatient mortality (n = 36 956) | 1.02b | 0.94 | 1.1 | 0.66 |
| 30-day mortality from date of admission (n = 36 956) | 1.15c | 1.07 | 1.23 | <0.001 |
Thirty-day outcomes were measured from date of hospital admission.
CI, confidence interval; NHFA, National Heart Failure Audit; OR, odds ratio; ROC, receiver operator characteristics; SE, standard error.
a Adjusted for age, gender, prior medical conditions (coronary artery disease, valvular heart disease, diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease), prior smoking history, place of care. Atrial fibrillation on ECG, heart rate at hospitalization, blood pressure at hospitalization, QRS duration, New York Heart association class shortness of breath, severity of peripheral oedema, prior device implantation, and HFrEF (LVEF <40%).
b Area under ROC curve: 0.52, SE: 0.005, 95% CI 0.52–0.53.
c Area under ROC curve: 0.79, SE: 0.003, 95% CI 0.78–0.80.
30-day deaths: Mortality within 30 days from admission was higher in the COVID-19 vs. pre-COVID-19 period (15% vs. 13%, OR: 1.15, 95% CI: 1.07–1.23) (Table 2). A lower proportion of patients in the COVID-19 vs. pre-COVID-19 period had heart failure as a principal cause of death on the death certificate (48.3% vs. 53.3%) and a greater proportion, as expected, had COVID-19 as a principal cause of death (9.6% vs. 0) (Table 3 and Supplementary material online, Figure S5).
Table 3.
Comparison of inpatient and 30-day from admission cause of death during pre-COVID-19 and COVID-19 period (data derived from Civil Registration of Death and NHFA databases)
| Primary cause of death | In-patient (pre-COVID-19 period) | In-patient (COVID-19 period) | P-value | 30-day (pre-COVID-19 period) | 30-day from admission (COVID-19 period) | P-value |
|---|---|---|---|---|---|---|
| Cardiac causes | ||||||
| Heart failure | 1518 (56.0%) | 519 (53.3%) | 0.12 | 1883 (53.3%) | 682 (48.3%) | 0.002 |
| ACS | 59 (2.2%) | 24 (2.5%) | 0.62 | 103 (2.9%) | 39 (2.8%) | 0.78 |
| Other cardiac causes | 184 (6.8%) | 44 (4.5%) | 0.01 | 262 (7.4%) | 72 (5.1%) | 0.003 |
| Respiratory causes | ||||||
| Acute respiratory infection | 406 (15.1%) | 135 (13.9%) | 0.37 | 526 (14.9%) | 206 (14.6%) | 0.80 |
| Respiratory failure | 65 (2.4%) | 13 (1.3%) | 0.04 | 77 (2.2%) | 21 (1.5%) | 0.12 |
| COVID-19 | 0 | 82 (8.3%) | — | 0 | 136 (9.6%) | — |
| Sepsis | 55 (2.0%) | 19 (1.9%) | 0.87 | 79 (2.2%) | 23 (1.6%) | 0.18 |
| Other non-cardiac causes | 405 (15.0%) | 139 (14.2%) | 0.57 | 603 (17.1%) | 234 (16.6%) | 0.69 |
ACS, acute coronary syndrome; CAD, coronary artery disease; NHFA, National Heart Failure Audit.
Increasing age, longer QRS duration, worse New York Heart Association class, and increasing peripheral oedema were independently associated with increased risk of death in hospital in both study periods, whereas prior history of diabetes mellitus was independently associated with increased risk of death in COVID-19 period only (Table 4).
Table 4.
Factors independently associated with in-hospital mortality during the pre-COVID-19 and COVID-19 periods (data derived from Civil Registration of Death and NHFA databases)
| Variables |
Pre-COVID-19 period |
COVID-19 period |
||||
|---|---|---|---|---|---|---|
|
N
|
27 172 |
9784 |
||||
| Model performance |
Area under ROC curve: 0.68, |
Area under ROC curve: 0.68, |
||||
| SE: 0.004, 95% CI: 0.67–0.69 |
SE: 0.004, 95% CI: 0.67–0.69 |
|||||
| Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value | |
| Age | 1.04 | 1.03–1.05 | <0.001 | 1.03 | 1.02–1.04 | <0.001 |
| Female sex | 0.92 | 0.83–1.03 | 0.17 | 0.96 | 0.82–1.10 | 0.54 |
| Admission heart ratea (beat/min) | 1.03 | 1.02–1.04 | 0.02 | 1.01 | 0.99–1.02 | 0.09 |
| Admission BP (mmHg)b | 0.93 | 0.92–0.94 | <0.001 | 0.92 | 0.90–0.93 | <0.001 |
| QRS durationc | 1.06 | 1.04–1.07 | <0.001 | 1.04 | 1.01–1.06 | 0.01 |
| CAD | 0.98 | 0.90–1.07 | 0.69 | 0.99 | 0.86–1.40 | 0.86 |
| Valve disease | 1.13 | 1.03–1.22 | 0.01 | 1.03 | 0.88–1.22 | 0.73 |
| Hypertension | 0.88 | 0.81–0.95 | 0.002 | 0.76 | 0.66–0.87 | <0.001 |
| DM | 1.01 | 0.92–1.10 | 0.84 | 1.18 | 1.02–1.37 | 0.02 |
| Asthma | 0.73 | 0.64–0.86 | <0.001 | 1.01 | 0.82–1.27 | 0.96 |
| COPD | 1.26 | 1.22–1.65 | 0.003 | 0.98 | 0.82–1.18 | 0.88 |
| Atrial fibrillation | 1.02 | 0.93–1.12 | 0.63 | 0.90 | 0.77–1.05 | 0.20 |
| NYHA III/IVd | 1.17 | 1.05–1.31 | 0.006 | 1.27 | 1.05–1.52 | 0.01 |
| peripheral oedemae | 1.22 | 1.11–1.33 | 0.005 | 1.28 | 1.10–1.49 | 0.001 |
| Care in cardiology ward | 0.72 | 0.65–0.78 | <0.001 | 0.70 | 0.61–0.81 | <0.001 |
| IECD | 0.85 | 0.75–0.97 | 0.01 | 0.91 | 0.74–1.11 | 0.35 |
| HFrEF | 1.01 | 0.92–1.1 | 0.97 | 0.96 | 0.83–1.11 | 0.57 |
CAD, coronary artery disease; CI, confidence interval; COPD, chronic obstructive pulmonary disease; ECG, electrocardiogram; HF, heart failure; HFrEF, heart failure with reduced ejection fraction; IECD, implantable electrical cardiac device receptor antagonist (MRA) to the variables used in the above model; NYHA, New York Heart Association; ROC, receiver operator characteristics; SE, standard error. Bold are statistically significant variables which are independently associated with mortality.
a Per 1 unit change in model.
b Per 10° rise in blood pressure.
c Per 10 ms change.
d NYHA class I/II are reference.
e None or mild peripheral oedema are reference.
Sensitivity analysis: Death at 30 days from admission was higher for patients who discharged alive from hospital during the COVID-19 vs. pre-COVID-19 period (OR: 1.57, 95% CI: 1.38–1.78) (Supplementary material online, Table S1) and multivariable analysis revealed similar predictors of 30-day mortality (Supplementary material online, Table S2). Details about missing data in all variables by study cohort are presented in Supplementary material online, Table S3.
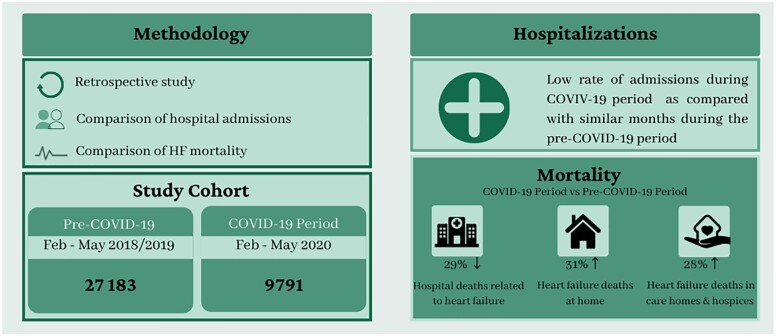
Figure 3 is our central illustration figure and visual take home graphics.
Figure 3.
Visual take home graphics. Comparison of in-patient and post-discharge clinical outcomes for hospitalized heart failure patients in pre-COVID-19 and COVID-19 period. Substantial decline in admissions for heart failure but an increase in deaths from heart failure in the community. HF, heart failure.
Discussion
In this analysis of national multi-sourced electronic health records, we examined the impact of the COVID-19 pandemic on heart failure hospitalizations and deaths in England. We observed a steady decline in heart failure hospitalizations from the middle of March 2020, with reductions ranging from 40% (HES) to 47% (NHFA); this was followed by persistently low rates of hospitalization during the COVID-19 period relative to the same months in the pre-COVID-19 period. Despite the restructuring of hospital services and diversion of resources to COVID-19 care, adjusted in-hospital mortality related to heart failure and provision of guideline-directed heart failure medications and investigations were similar in the COVID-19 and pre-COVID-19 periods in NHFA. Finally, the reduction in heart failure admissions during the COVID-19 pandemic was accompanied by an increase in heart failure deaths in the community, with 280 excess deaths with heart failure as a principal cause over the 4-month pandemic period.
The NHFA is the largest heart failure registry in the world. It was established to monitor and report hospital clinical activity against a set of key performance indicators. The large sample size provides sufficient statistical power to capture differences in clinical outcomes between the patient groups studied. This is the first national analysis to assess the direct and indirect impact of the COVID-19 pandemic on hospitalization rates and mortality for patients with heart failure in the hospital and community. We found a dramatic decline in heart failure hospitalizations during the COVID-19 pandemic. This reduction probably reflects successful attempts at hospital avoidance by patients to minimize the risk of hospital-acquired COVID-19 and, perhaps, increased support in the community. Patients with heart failure may have remained at home due to fears of exposure to COVID-19, breaking their shielding or social quarantine, leading to an increase in heart failure deaths in the community. Furthermore, some NHS trusts introduced new rapid access cardiology clinics and use of acute care services at home to reduced hospitalizations during COVID-19 pandemic but its impact on overall NHS service is relatively unknown.10–12 In addition, hospital services were reconfigured to create additional beds for COVID-19 patients by repurposing cardiology wards, cancelling out-patient clinics (or replacing them with remote clinics) and postponing elective procedural activities.
Our work suggests that the quality of care for patients hospitalized for heart failure was not compromised despite the structural and organizational changes during the COVID-19 pandemic. The rates of investigations, including echocardiography, were similar in the COVID-19 and pre-COVID-19 periods. Plasma concentrations of BNP/NT-proBNP were somewhat higher in the COVID-19 period, suggesting a higher threshold for admission and sicker patients. Simultaneously, it appears that these ‘sicker’ patients received on average less aggressive diuresis (less median weight loss during hospitalization) during the hospitalization and had shorter length of stay. Interestingly, we observed an increased odds of 30-day mortality during the COVID period that may be explained by our observation that sicker patients were less aggressively diuresed and had shorter lengths of stay. Patients may have been discharged prematurely to create more hospital beds or with arrangements to receive palliation for some end-stage heart failure patients in community. Gaps in post-discharge care due to closure of ambulatory care centres during the COVID-19 pandemic may have contributed to suboptimal care and increased risk of death following hospitalization. These are the possible main factors for observing higher natriuretic peptides values, shorter stay in the hospital and lesser weight loss during COVID-19 period compared to pre-COVID-19 period. Meanwhile, deaths attributed to heart failure in the community and care homes also increased during the COVID-19 pandemic.
A recent analysis of patients hospitalized with heart failure in Denmark did not report an increase in inpatient deaths during the COVID-19 period relative to a similar period in 2019 [142 vs. 132 per 1000 person-year; age- and sex-adjusted death rate ratio, 1.05 (95% CI, 0.93–1.18, P - 0.45].5 In contrast, a study of 1372 patients in two hospitals in London found that patients hospitalized for heart failure during the COVID-19 pandemic had worse outcomes (in-hospital deaths) than those hospitalized during a similar period in 2019 (hazard ratio; 2.23, 95% CI 1.34–3.72, P = 0.002).3 Small sample size, lack of robust multivariable analyses and non-availability of outcome data after discharge were the main limitations of these studies which may yield different results compared to current study.
Similar to any observational study there are limitations. While we had information about the proportion of patients with HFrEF, we could not differentiate between patients who had heart failure with mid-range ejection fraction and heart failure with preserved ejection fraction. Some general aspects of health such as frailty, mood, social network and cognitive functions were not recorded. More detailed assessments of cardiac function, especially with echocardiography or other imaging modalities were not available. During the earlier phase of the COVID-19 pandemic, widespread COVID-19 testing was not available in England for everyone and was limited to targeted and high-risk patients. It’s not possible to ascertain from current study how many heart failure patients actually had COVID-19 infection during hospital admission. It’s also possible that some patients were admitted due to COVID-19 infection and developed an acute exacerbation of heart failure that was not captured in the NHFA as the primary diagnosis for discharge or death was not heart failure. Other patients might have been admitted in hospital due to exacerbation of heart failure and became infected with COVID-19 during the hospital stay and ultimately died in the hospital or community. Finally, during the COVID-19 pandemic, emergency guidance enabled any doctor in the UK to complete the medical certificate of cause of death and causes of death could be ‘to the best of their knowledge and belief’. This may have resulted in misclassification or bias towards certain causes of death. However if anything, this would tend to under-estimate heart failure deaths in the community that may have been labelled as COVID-19 deaths. Moreover, the accuracy of a diagnosis of heart failure on death certificates is uncertain. One study published in 2017 reported that there was no prior record of heart failure in the primary or secondary care record for 55% of ONS records reporting heart failure as a cause of death.13 However, this limitation applied equally on both study cohorts.
Conclusion
This analysis of approximately 37 000 acute heart failure admissions is the first national study to compare incidence, processes of care, treatments, and clinical outcomes during and after hospitalization during the COVID-19 pandemic. We report a 47% reduction in heart failure hospitalizations during the COVID-19 pandemic, accompanied by an increase in heart failure deaths at home and in care homes and hospices. We estimate 280 excess heart failure deaths during this period, and 2165 deaths excess deaths in patients with heart failure. Despite restructuring of hospital services during the COVID-19 pandemic, standard of care appears to have been maintained for those patients hospitalized with heart failure with similar adjusted in-hospital mortality rates, but higher 30-day mortality rates compared to the pre-COVID-19 period. The reduction in heart failure hospitalization with concomitant increase in heart failure deaths in the community has important implications around public health messaging during the peak COVID-19 pandemic; ‘stay at home, protect the NHS’ should need to be elaborated further to the public that ‘stay at home’ does not mean to avoid attending hospitals or seeking healthcare advice in the event of illness as it may influence clinical outcome.14
Supplementary material
Supplementary material is available at European Heart Journal – Quality of Care and Clinical Outcomes online.
Supplementary Material
Acknowledgements
The authors acknowledge Chris Roebuck, Tom Denwood, and data support staff at the NHS digital for providing and creating the secure environment for data hosting and for analytical support.
Funding
J.W. and C.P.G. are funded by the University of Leeds. M.A.M. funded by the University of Keele. A.S. and M.R. funded by the National Institute of Health Research. The National Heart Failure Audit Project is commissioned by the Health Quality Improvement Partnership as part of the National Clinical Audit and Patient Outcomes Programme. The funding organizations for this study were not involved in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Data availability
The data underlying this article were provided by NHS digital by permission. Data will be shared on request to the corresponding author with permission of NHS digital.
Conflict of interest: none declared.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
References
- 1. Ogunleye OO, Basu D, Mueller D, Sneddon J, Seaton RA, Yinka-Ogunleye AF. et al. Response to the novel corona virus (COVID-19) pandemic across Africa: successes, challenges, and implications for the future. Front Pharmacol 2020;11:1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. First-year results of CABRI (Coronary Angioplasty versus Bypass Revascularisation Investigation). CABRI trial participants. Lancet 1995;346:1179–1184. [PubMed] [Google Scholar]
- 3. Cannatà A, Bromage DI, Rind IA, Gregorio C, Bannister C, Albarjas M. et al. Temporal trends in decompensated heart failure and outcomes during COVID-19: a multisite report from heart failure referral centres in London. Eur J Heart Fail 2020;22:2219–2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M. et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020;396:381–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Andersson C, Gerds T, Fosbøl E, Phelps M, Andersen J, Lamberts M. et al. Incidence of new-onset and worsening heart failure before and after the COVID-19 epidemic lockdown in denmark: a nationwide cohort study. Circ Heart Fail 2020;13:e007274. [DOI] [PubMed] [Google Scholar]
- 6. Cleland JG, McDonagh T, Rigby AS, Yassin A, Whittaker T, Dargie HJ; on behalf of the National Heart Failure Audit Team for England and Wales. The national heart failure audit for England and Wales 2008-2009. Heart 2011;97:876–886. [DOI] [PubMed] [Google Scholar]
- 7. Shoaib A, Mamas MA, Ahmad QS, McDonagh TM, Hardman SMC, Rashid M. et al. Characteristics and outcome of acute heart failure patients according to the severity of peripheral oedema. Int J Cardiol 2019;285:40–46. [DOI] [PubMed] [Google Scholar]
- 8. Bebb O, Hall M, Fox KAA, Dondo TB, Timmis A, Bueno H. et al. Performance of hospitals according to the ESC ACCA quality indicators and 30-day mortality for acute myocardial infarction: national cohort study using the United Kingdom Myocardial Ischaemia National Audit Project (MINAP) register. Eur Heart J 2017;38:974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hall M, Dondo TB, Yan AT, Goodman SG, Bueno H, Chew DP. et al. Association of clinical factors and therapeutic strategies with improvements in survival following non-ST-elevation myocardial infarction, 2003-2013. JAMA 2016;316:1073–1082. [DOI] [PubMed] [Google Scholar]
- 10. Ball S, Banerjee A, Berry C, Boyle JR, Bray B, Bradlow W. et al. ; CVD-COVID-UK Consortium. Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart 2020;106:1890–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brant LCC, Nascimento BR, Teixeira RA, Lopes MACQ, Malta DC, Oliveira GMM. et al. Excess of cardiovascular deaths during the COVID-19 pandemic in Brazilian capital cities. Heart 2020;106:1898–1905. [DOI] [PubMed] [Google Scholar]
- 12. Stokes AC, Lundberg DJ, Hempstead K, Elo IT, Preston SH.. Assessing the impact of the Covid-19 pandemic on US mortality: a county-level analysis. medRxiv 2020;2020.08.31.20184036. doi: 10.1101/2020.08.31.20184036. [Google Scholar]
- 13. Koudstaal S, Pujades-Rodriguez M, Denaxas S, Gho J, Shah AD, Yu N. et al. Prognostic burden of heart failure recorded in primary care, acute hospital admissions, or both: a population-based linked electronic health record cohort study in 2.1 million people. Eur J Heart Fail 2017;19:1119–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gov.UK. Coronavirus: Government launches campaign urging people to stay at home this Easter. 2020. https://www.gov.uk/government/news/coronavirus-government-launches-campaign-urging-people-to-stay-at-home-this-easter
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were provided by NHS digital by permission. Data will be shared on request to the corresponding author with permission of NHS digital.
Conflict of interest: none declared.