Abstract
Purpose
In response to the rapid spread of SARS-CoV-2, hospitals in Canada enacted temporary visitor restrictions to limit the spread of COVID-19 and preserve personal protective equipment supplies. This study describes the extent, variation, and fluctuation of Canadian adult intensive care unit (ICU) visitation policies before and during the first wave of the COVID-19 pandemic.
Methods
We conducted an environmental scan of Canadian hospital visitation policies throughout the first wave of the pandemic. We conducted a two-phased study analyzing both quantitative and qualitative data.
Results
We collected 257 documents with reference to visitation policies (preCOVID, 101 [39%]; midCOVID, 71 [28%]; and lateCOVID, 85 [33%]). Of these 257 documents, 38 (15%) were ICU-specific and 70 (27%) referenced the ICU. Most policies during the midCOVID/lateCOVID pandemic period allowed no visitors with specific exceptions (e.g., end-of-life). Framework analysis revealed five overarching themes: 1) reasons for restricted visitation policies; 2) visitation policies and expectations; 3) exceptions to visitation policy; 4) patient and family-centred care; and 5) communication and transparency.
Conclusions
During the first wave of the COVID-19 pandemic, most Canadian hospitals had public-facing visitor restriction policies with specific exception categories, most commonly for patients at end-of-life, patients requiring assistance, or COVID-19 positive patients (varying from not allowed to case-by-case). Further studies are needed to understand the consistency with which visitation policies were operationalized and how they may have impacted patient- and family-centred care.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12630-021-02049-4.
Keywords: intensive care unit, COVID-19, policy, visiting policies
Résumé
Objectif
En réponse à la propagation rapide du SRAS-CoV-2, les hôpitaux du Canada ont adopté des restrictions temporaires pour les visites afin de limiter la propagation de la COVID-19 et de préserver les stocks d’équipements de protection individuelle. Cette étude décrit l’ampleur, les variations et fluctuations des politiques canadiennes concernant les visites aux unités de soins intensifs (USI) pour adultes avant et pendant la première vague de la pandémie de COVID-19.
Méthode
Nous avons réalisé une étude de milieu des politiques hospitalières canadiennes concernant les visites tout au long de la première vague de la pandémie. Nous avons mené une étude en deux phases analysant des données quantitatives et qualitatives.
Résultats
Nous avons recueilli 257 documents faisant référence aux politiques de visites (pré-COVID, 101 [39 %]; mid-COVID, 71 [28 %]; et COVID-tardif, 85 [33 %]). Sur ces 257 documents, 38 (15 %) étaient spécifiques aux USI et 70 (27 %) faisaient référence aux USI. La plupart des politiques au cours de la période pandémique mid-COVID/COVID-tardif ne permettaient aucune visite sauf exception spécifique (p. ex., fin de vie). L’analyse du cadre a révélé cinq thèmes généraux : 1) les raisons des restrictions des politiques de visites; 2) les politiques et attentes en matière de visites; 3) les exceptions aux politiques de visites; 4) les soins aux patients et centrés sur la famille; et 5) la communication et la transparence.
Conclusion
Au cours de la première vague de la pandémie de COVID-19, la plupart des hôpitaux canadiens avaient des politiques de restriction des visites s’appliquant au public avec des catégories d’exception spécifiques, le plus souvent pour les patients en fin de vie, les patients nécessitant de l’aide ou les patients COVID-positifs (variant d’une interdiction au cas par cas). D’autres études sont nécessaires pour comprendre l’uniformité avec laquelle les politiques de visites ont été mises en œuvre et comment elles ont pu avoir une incidence sur les soins centrés sur le patient et la famille.
On 11 March 2020, the World Health Organization declared COVID-19 a global pandemic.1 To date (19 April 2021) there have been 1,131,773) reported cases across Canada, with 17.9% of hospitalized patients admitted to the intensive care unit (ICU).2 Intensive care unit patients are the sickest in the healthcare system; survivors often enduring lengthy and incomplete recovery.3,4 Family members of critically ill patients may also experience significant and long-lasting psychological distress.5 Family presence at the bedside can improve patient6–11 and family outcomes,8,9,12–15 increase communication and satisfaction,16 and promote shared decision-making.5 Nevertheless, this important source of support for critically ill patients was in jeopardy during the first wave of the COVID-19 pandemic, as widespread restrictions on family presence were implemented across healthcare settings to limit potential exposure to the virus.17 Many hospitals used alternate means of communication through frequent phone calls and virtual visits to ensure clinical updates and maintain family connections.18
On 30 April 2020, the Public Health Agency of Canada (PHAC) published recommendations prepared by the National Advisory Committee on Infection Prevention and Control for acute healthcare facilities to develop and implement restricted visitation policies19 to help prevent the spread of COVID-19 and conserve personal protective equipment (PPE).19 The PHAC recommendations included: limit visitors to those who are essential, limit visitor movement within the facility, ensure a hand hygiene program is in place, and screen every visitor entering the facility.19 These recommendations provided guidance to healthcare organizations to develop their own visitation policies aligned with provincial, territorial, and local legislation. The impact of these visitation policies on critically ill patients, their families, and ICU healthcare professionals in critical care settings is not clear.
Understanding the variability and fluctuation in ICU visitor restrictions is central to inform policy changes during subsequent waves of the COVID-19 pandemic and during future infectious disease outbreaks. Though restricted visitation policies in Canada have been posted publicly on hospital websites or announced through various media, to our knowledge there is no single comprehensive summary of these policies. We sought to describe the extent, variation, and fluctuation of Canadian adult ICU visitation policies before and during the first wave of the COVID-19 pandemic. While we focused this environmental scan on ICUs, we also included hospital policies because ICU-specific policies did not exist in some settings but were contextualized within the larger hospital system.
Methods
Study design
We conducted an environmental scan of Canadian hospital visitation policies before and during the first wave of the COVID-19 pandemic according to the Canadian Agency for Drugs and Technologies in Health (CADTH) environmental scan process.20 A sampling frame of Canadian hospitals with adult ICUs was created by combining a list of ICUs from previous studies21,22 and assessed for completeness through hospital lists from PHAC and internet searches for all Canadian hospitals (Electronic Supplementary Material [ESM] eTable 1). Research assistants conducted an internet search of Canadian hospital and ICU visitation policies. For hospitals or ICUs without online policies, we attempted to obtain hospital-specific policies by directly contacting hospital/ICU administrations.
Patient and public involvement
Patient partners were involved in study design to ensure the study included the patient perspective and were principal investigators on the resulting funding application. No patients participated in data acquisition or analysis.
Data extraction and analyses
We collected policies at three time points: preCOVID-19 (time point: preCOVID), after PHAC published recommendations for restricted visitation (time point: midCOVID; 5–7 May 2020), and when hospitals began to lift visitation restrictions23–26 (time point: lateCOVID; 1–30 June 2020).
We abstracted quantitative data using a standardized data extraction form including the following: hospital name/health authority, province, document type (official policy, webpage, brochure, poster, news bulletin, or other), type of policy (no visitors, structured, open), number of visitors allowed, and visiting hours/times. We piloted the extraction form to ensure comprehensiveness and relevance. Two research assistants extracted data for all collected policies independently and in duplicate. Disagreements were resolved through discussion or involvement of another reviewer as necessary. We summarized quantitative data descriptively using frequencies and percentages within categories.
We summarized qualitative data using a framework method to identify overarching themes and subthemes in preCOVID19 (preCOVID) and COVID-19 visitation policies (midCOVID/lateCOVID).27 All policies were imported into NVivo-12 (QSR International, Melbourne, Australia) for data management and analysis. Five coders used an iterative process to apply the framework method, which included the following five stages: 1) familiarization with policies (i.e., reading each policy); 2) open coding (i.e., independently coding the first few policies for anything relevant to visitation); 3) developing an analytical framework (i.e., grouping codes together to create themes); 4) applying the analytical framework to remaining policies; 5) interpreting the data. If there were no ICU-specific visitation policies, we coded the general visitation policies for the hospital. If there was a missing time point for any hospital, the visitation policies of the health region where the hospital was located were assumed to be applicable.
Results
Hospital visitation policy characteristics
Of 55 Canadian health regions and 230 identified hospitals with adult ICUs, 312 documents with reference to visitation policies were collected from 93 hospitals/hospital networks and 35 health regions (ESM eTable 1). At each timepoint, some hospitals had multiple documents that referenced visitation policies (e.g., frequently asked questions, poster, guidance for virtual visits) (ESM eTable 2), which were merged into one document for analysis, which means 257 documents were analyzed (preCOVID, 101/257 [39%]; midCOVID, 71/257 [28%]; lateCOVID, 85/257 [33%]). Of these 257 documents, 246 (96%) were publicly available and 11 were internal policies obtained from hospitals or ICU administration through direct request. Visitation rules were found for 77% (178/230) of hospitals/hospital networks preCOVID, 93% (215/230) of hospitals/hospital networks midCOVID, and 88% (203/230) of hospitals/hospital networks lateCOVID. No visitation policies were found for the Northern Health Region in British Columbia.
Intensive care unit-specific policies
Thirty-eight out of 257 (15%) documents were ICU-specific (Table 1), while the remainder were hospital-wide policies (219/257 [85%]). “Critical illness,” “critically ill,” “critical care,” “ICU,” or “intensive care (unit)” were mentioned in 70 (70/219 [32%]) of the hospital-wide visitation documents.
Table 1.
Total number of documents with reference to visitation policies at different time points before (preCOVID) and during (midCOVID/lateCOVID) the first wave of the COVID-19 pandemic
| preCOVID N = 101 |
midCOVID N = 71 |
lateCOVID N = 85 |
||||
|---|---|---|---|---|---|---|
| Hospital | ICU | Hospital | ICU | Hospital | ICU | |
| Province, n | ||||||
| Alberta | 1 | 1 | 1 | 0 | 1 | 1 |
| British Columbia | 3 | 4 | 6 | 0 | 6 | 0 |
| Manitoba | 3 | 2 | 3 | 0 | 5 | 0 |
| New Brunswick | 2 | 1 | 2 | 0 | 2 | 0 |
| Newfoundland and Labrador | 3 | 1 | 4 | 0 | 4 | 0 |
| Northwest Territories, Nunavut, Yukon Territories | 3 | 0 | 3 | 0 | 3 | 0 |
| Nova Scotia | 1 | 1 | 1 | 0 | 1 | 0 |
| Ontario | 25 | 16 | 48 | 0 | 51 | 1 |
| Prince Edward Island | 1 | 1 | 1 | 0 | 1 | 0 |
| Quebec | 19 | 6 | 1 | 0 | 7 | 1 |
| Saskatchewan | 5 | 2 | 1 | 0 | 1 | 0 |
| Total, n | 66 | 35 | 71 | 0 | 82 | 3 |
ICU = intensive care unit; lateCOVID = 1–30 June 2020; midCOVID = 5–7 May 2020; preCOVID = before the COVID-19 pandemic.
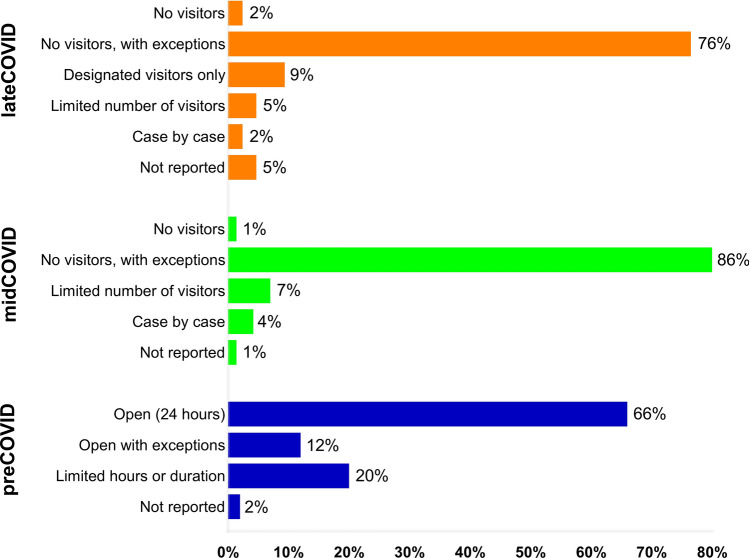
Extent of visitation restrictions
During preCOVID, most of the visitation policies (hospital-wide, 42/66 [64%]; ICU-specific, 24/35 [69%]) were open (i.e., 24-hr visiting) or open with some exceptions (hospital-wide, 6/66 [9%]; ICU-specific, 6/35 [17%]), e.g., during procedures/ handover/rounds or at the discretion of the care team (Figure). Some hospitals had limited visiting hours or duration of visit (e.g., 10 min·hr−1; hospital-wide, 16/66 [24%]; ICU-specific, 5/35 [14%]). Region-specific data are displayed in ESM eTable 3.
During midCOVID, one hospital had a “no visitors allowed” policy (Ontario; 1/71 [1%]) or allowed a limited number of visitors (e.g., one at end-of-life; Maritimes, 2/71 [3%]) (Fig. 1). Most hospitals had a no visitor policy with exceptions (61/71 [86%]), e.g., at end-of-life. As hospitals began to lift visitation restrictions (lateCOVID), most still had policies of no visitors with exceptions (65/85 [76%]) or on a case-by-case basis (2/85 [2%]). Few hospitals began allowing designated visitors (8/85 [9%]) or a limited number of visitors (4/85 [5%]). In some policies, this designated visitor had to be the same person throughout the hospital stay (midCOVID, British Columbia/Ontario; lateCOVID, Newfoundland and Labrador). During lateCOVID, one policy from Ontario stated that the designated visitor could have one designated alternate. In Quebec, the designated visitor could be three or four different people, but only one could visit at a time. Some policies stated when these visits could occur, which included once per stay (midCOVID, Ontario), once per day (midCOVID, Newfoundland and Labrador/Northwest Territories/Ontario; lateCOVID, Northwest Territories), or once per day for one (midCOVID, British Columbia) or two (lateCOVID, Ontario) hours maximum, or during designated visiting hours (lateCOVID, Alberta/Manitoba/Newfoundland and Labrador/Ontario/Quebec).
Figure.
Overview of the extent of visitation restrictions at different time points before (preCOVID, N = 101) and during (midCOVID, N = 71; lateCOVID, N = 85) the first wave of the COVID-19 pandemic.
Analysis showed five overarching themes describing restricted visitation policies in Canadian hospitals with adult ICUs: 1) reasons for restricted visitation policies; 2) visitation policies and expectations; 3) exceptions to visitation policy; 4) patient- and family-centred care (PFCC); and 5) communication and transparency. The proportions of the themes and subthemes at each timepoint are presented in Table 2. Exemplar quotations for themes are presented in ESM eTable 4.
Table 2.
Themes and subthemes for restricted visitation before (preCOVID) and during (midCOVID/lateCOVID) the first wave of the COVID-19 pandemic
| Theme and subtheme | preCOVID | midCOVID | lateCOVID |
|---|---|---|---|
| N = 101 | N = 71 | N = 85 | |
| Reasons for visitor restrictions, n (%) | |||
| Conserve and redeploy resources (e.g., PPE) | - | 6 (8%) | 3 (4%) |
| Discretion of the healthcare team | 40 (40%) | 7 (10%) | 11 (13%) |
| During handover (e.g., shift-to-shift) | 6 (6%) | - | - |
| Prevent the spread of COVID-19 | NA | 26 (37%) | 20 (24%) |
| Prevent the spread of infection | 20 (20%) | 3 (4%) | 2 (2%) |
| Privacy | 23 (23%) | - | 1 (1%) |
| Protect the public and hospital occupants | 10 (10%) | 52 (73%) | 52 (61%) |
| Exceptions to visitation policy, n (%) | |||
| COVID-19 positive patients (no visitors) | NA | 12 (17%) | 19 (22%) |
| End-of-life, MAID or compassionate care or critically ill patient (visitors allowed) | 13 (13%)) | 61 (86%) | 68 (80%) |
| Patients requiring assistance (visitors allowed) | - | 19 (27%) | 33 (39%) |
| Visitation policies and expectations, n (%) | |||
| Hand hygiene | 49 (49%) | 20 (28%) | 61 (72%) |
| Visitor screening | 50 (50%) | 58 (82%) | 61 (72%) |
| Personal protective equipment: | |||
| Public health measure | 6 (6%) | 18 (25%) | 35 (42%) |
| Contact and isolation precautions | 19 (19%) | 8 (11%) | 25 (29%) |
| Physical distancing | 3 (3%) | 11 (15%) | 25 (29%) |
| Patient and family-centred care, n (%) | |||
| Alternative ways to engage a patient (e.g., video call) | - | 36 (51%) | 38 (45%) |
| Resources (e.g., mental health, appeal, concerns) | 40 (40%) | 27 (38%) | 35 (41%) |
| Patient care and wellbeing (e.g., personal items) | 33 (33%) | 23 (32%) | 24 (28%) |
| Transparency, n (%) | |||
| End-of-life definitions | - | 4 (6%) | 10 (12%) |
| Active COVID-19 cases at hospital | NA | 10 (14%) | 8 (9%) |
| Phased return to visitation | NA | 1 (1%) | 4 (5%) |
lateCOVID = 1–30 June 2020; MAID = medical assistance in dying; midCOVID = 5–7 May 2020; NA = not applicable; preCOVID = before the COVID-19 pandemic; PPE = personal protective equipment.
Overarching themes
Reasons for restricted visitation policies
During preCOVID, 95% (96/101) of the documents listed reasons for visitation restrictions, which included discretion of the healthcare team (40/96 [42%]), protecting the privacy and rights of other patients (23/96 [24%]), preventing the spread of infection (20/96 [21%]), and avoiding distractions during handover (6/96 [6%]). During midCOVID/lateCOVID, all documents listed reasons for visitation restrictions, which included protecting the public and hospital occupants (i.e., patients, healthcare team) (52/71 [73%]), preventing the spread of COVID-19 (26/71 [37%]), and conserving resources (e.g., PPE) (6/71 [8%]). Twenty-four (24/71 [34%]) of the available documents provided a reason for their change in visitation policies from mid to lateCOVID. This included alignment with public health recommendations, lifting of restrictions, or phased reopening (18/24 [75%]; Manitoba/Newfoundland and Labrador/Nova Scotia/Ontario); maintenance of balance between the risk of COVID-19 and the wellbeing of patients (5/24 [21%], Alberta/Manitoba/Northwest Territories/Ontario); and the availability of space for physical distancing (1/24;4%, Ontario).
Exceptions to visitation policy
During preCOVID, exceptions to visitation policies were dependent on illness severity or patients at end-of-life (e.g., more flexible hours or increased number of visitors allowed). During midCOVID/lateCOVID, exceptions to visitation policies specific to COVID-19 included the following: 1) end-of-life circumstances (including medical assistance in dying [MAID]), palliative and/or compassionate care, and level of critical illness (visitors allowed); and 2) patients requiring assistance (e.g., cognitive or physical disabilities) (visitors allowed). Of note, a small number of policies made exceptions on a “case-by-case basis” (midCOVID/lateCOVID, Maritimes/Yukon/Ontario/Quebec). In some documents, this included an explicit, easily interpreted process for visitor exceptions (Yukon; ESM eTable 4). Policies varied for COVID-19 positive patients. Several policies explicitly stated that they did not allow visitors for known or suspected COVID-19 positive patients (midCOVID, 11/71 [15%], Alberta/Newfoundland and Labrador/Ontario; lateCOVID, 15/85 [18%], Newfoundland and Labrador/Ontario/Prince Edward Island), regardless of patient condition. During midCOVID, one policy stated that confirmed or suspected COVID-19 positive patients were allowed one visitor (Ontario). During lateCOVID, seven policies allowed COVID-19 positive patients to have visitors (7/85 [8%], Alberta/British Columbia/Ontario/Saskatchewan) or allowed COVID-19 positive patients to have visitors on a case-by-case basis (e.g., end-of-life; 6/85 [7%], Alberta/Manitoba/Ontario).
Few policies allowed culturally appropriate practices and protocols (midCOVID/lateCOVID, Alberta; lateCOVID, Yukon, Quebec) or visitors if a patient’s stay was prolonged (e.g., > seven days [Quebec] or reached 14 days with the patient not being expected to be discharged within the next 72 hr [Yukon]; lateCOVID, Manitoba).
Visitation policies and expectations
Visitation policies and expectations were defined as instructions or procedures by which visitors were expected to abide before or during their visit. This theme has four subthemes that were present during preCOVID, midCOVID, and lateCOVID: 1) rules of the visit (e.g., designated visitors, number of visitors, duration of visit, overnight protocol, age of visitors); 2) required routine practices to limit the spread of infection (e.g., PPE use, hand hygiene); 3) screening procedures to limit the entry of individuals (e.g., health screening prior to entering the facility); and 4) the use of physical space within the acute healthcare facility (e.g., physical distancing measures, use of washrooms and waiting rooms). During the COVID-19 pandemic (midCOVID/lateCOVID), the subthemes were more centred on issues specific to the pandemic. For example, if a visitor was feeling unwell preCOVID-19, they would be discouraged from visiting. Nevertheless, during the pandemic, proactive measures such as health screening at monitored hospital entryways were enforced to prohibit unwell visitors from entering or providing visitors with a mask. Some policies stated that visitors would be “shown how to put on” or “provided instructions” how to don/doff required PPE, though no policy stated if there was a dedicated healthcare professional responsible for this. Similarly, active physical distancing measures were enforced when physical spaces were used. Different age restrictions for visitation were reported, wherein visitors had to be a certain age to visit, which differed across the provinces (e.g., > 18 yr in Alberta/Ontario/Newfoundland and Labrador; ≥ 16 yr in Ontario; ≤ 75 yr in Ontario). Reasons for not allowing children or older adults to visit were not provided.
Patient- and family-centred care
Patient- and family-centred care was defined as “an approach to the planning, delivery, and evaluation of healthcare that is grounded in mutually beneficial partnerships among healthcare providers, patients, and families.”28 Subthemes included: 1) alternative ways to engage a patient (e.g., virtual visits, emails, phone calls, free television, Wi-Fi services [midCOVID/lateCOVID]); 2) resources for families (e.g., ways to address concerns [midCOVID/lateCOVID] and mental health coping strategies [preCOVID/midCOVID/lateCOVID]); and 3) patient care and wellbeing (e.g., personal items, designated family spokesperson, access to spiritual care). During the first wave of COVID-19, some hospitals included their alternative communication strategies in their public-facing documents (midCOVID, 30/71 [42%]; lateCOVID, 34/85 [40%]), which included virtual visits, online greetings through a website or email portal, and postcards. During midCOVID/lateCOVID, policies included limitations to what personal items could be dropped off at hospitals (e.g., items that had been disinfected).
Transparency
We defined transparency as clarity and openness regarding restricted visitation policies and the hospital’s level of risk in relation to COVID-19. During midCOVID and lateCOVID, transparency was divided into subthemes: 1) end-of-life or compassionate care definitions; 2) active COVID-19 cases (e.g., how many active cases are in the hospital; midCOVID/lateCOVID in Ontario); and 3) approaches to return to care (e.g., number of allowed visitors based on the burden of COVID-19 in the community during lateCOVID in Yukon) (ESM eTable 3). Examples of end-of-life definitions varied across Canada. Some considered end-of-life to be when a patient “Has a palliative performance score of 30% or less”29 (Ontario) while others based this on a clinical judgement (e.g., “dying (within 48–72 hr)” in Ontario or “The decision related to when an individual is reaching their end-of-life will be informed by the care team and is unique to the circumstances of each individual” in Manitoba). One policy deferred to a “…level removed from the direct care team (e.g., Site Command Post, site manager)” to determine when an individual was reaching the end-of-life (Alberta).
Discussion
This study provides an overview of visitation policies for Canadian hospitals with ICUs before and during the first wave of the COVID-19 pandemic. In the early stages of COVID-19, most hospitals did not allow visitors either outright or with few exceptions. Similar to PHAC recommendations, most restricted visitation policies included exceptions to visitation, instructions for hand hygiene, and recommendations for visitor screening and limiting visitor movement within the facility.19 Some differences were found in policies based on the patient population served and provincial/territorial guidance. Visitation policies were more restrictive during the COVID-19 pandemic compared with before the pandemic because of a need to react quickly during a time when there was limited information on COVID-19. We saw visitation restrictions loosen as more information about COVID-19 was available. In some jurisdictions, this included allowing children to visit and allowing patients (including COVID-19 positive patients) to have a designated visitor.
The changes in visitation policies are reminiscent of the historical era of restrictive ICU visiting policies (i.e., limited visitation time and frequency), which have become more open over recent years.5,30,31 This has important implications for PFCC.32 Restricted visitation policies affect family members who, when away from the ICU, experience uncertainty about the care provided for their loved ones.33 Many COVID-19 visitation policies identified ways to support patient-family interaction such as Halton Healthcare’s “Virtual Visiting Program”, which included a dedicated team member to schedule and facilitate virtual visits. Although most policies encouraged patients or families to keep in touch either virtually or by phone, few included information about how to actually do so and instead encouraged families to ask the care team. A recent study reported that the majority of families found virtual visitation to be a positive experience18; however, virtual visits without a dedicated facilitator may be limited in critically ill adults. Critically ill patients are generally sedated, intubated, or may have delirium, thereby precluding their ability to facilitate their own phone and virtual conversations. It may not be feasible for members of the care team to schedule and facilitate virtual visits during the COVID-19 pandemic, wherein time and resources are increasingly constrained. As such, health regions should consider providing guidance for ICU virtual visitation when in-person visits are not permitted or when family members choose not to visit in person because of concern for their own or others’ health, including details on who will be facilitating these virtual visits. Furthermore, per Healthcare Excellence Canada's suggestions, visitation policies should be revisited in collaboration with patients, families, and caregivers.34
Most of the restricted visitation policies represented universal visitor restrictions, with only 39% including ICU-specific public-facing policies. Though the implementation of visitor restrictions was well-intentioned to prevent the spread of COVID-19 and to conserve and redeploy resources (e.g., PPE), universal visitor restrictions may not be appropriate to all critically ill patients. Visitation restrictions likely contribute to distress for patients, families, and healthcare professionals.35–37 For example, “end-of-life” or “dying” was often included as an exception to restricted visitation policies. However, the operationalization of these terms was not well defined38 and predictions of mortality are unreliable39,40 Some policies were transparent with their definition of “end-of-life,” with some including scales (e.g., palliative performance score) or citing clinician judgement. Healthcare professionals faced with predicting end-of-life may experience moral distress due to the risk of feeling complicit in allowing patients to die alone without their family at the bedside as a result of incorrect predictions. Though some policies identified critical illness as an exception to visitor restrictions, the majority did not. Health regions should consider critical illness as an exception to visitor restriction. Nevertheless, the heterogeneous and unpredictable trajectory of patients with critical illness and unreliable mortality predictions must be weighed against the need to reduce COVID-19 transmission to both the patient and healthcare professionals. Health regions should also consider allowing only one visitor per patient and the impact that this may have on families in light of the well-described distress families experience pursuant to ICU stays.41 Ongoing studies are evaluating the impact that restricted visitation policies have on patients, families, and healthcare professionals.42 In addition, Healthcare Excellence Canada developed policy guidance in an effort to reintroduce families as “essential care partners” back into healthcare facilities.43
Regional or provincial and territorial guidance may motivate creation of hospital-specific policies. However, differences between hospitals within the same health region may create inequity. For example, despite Ontario having 14 Local Health Integration Networks, hospital-specific policies were found on several hospital websites. Differences included exceptions to the policies (e.g., some included critical illness as an exception or a process to appeal the restricted visitation policy), the number of visitors allowed at end-of-life (e.g., one or two), and age of family members who could visit (e.g., ≥ 16 yr, ≥ 18 yr of age). It is possible that patients who are transferred to another hospital may no longer be allowed visitors as permitted in the first hospital. As such, all hospitals within a health region should consider adopting the same visitation policy to maintain equity and consistent messaging.
There are limitations to this study. First, we mostly collected only public-facing or publicly available visitation policies from hospital websites. When hospital or ICU administration were contacted, many did not want to disclose their policies publicly or did not respond to our emails. It is possible that some policies were internal and not communicated externally (and hence were not identified by our review); however, the current study offers the most complete picture of public-facing hospital visitation policies available in Canada. Second, there are regional differences in how each Canadian province/territory was impacted by and responded to the COVID-19 pandemic. Given that policies were collected during three time points only, this study does not consider temporal differences for each province as the pandemic continues to evolve. There are several strengths for this study. These include following the CADTH reporting guidelines, using a sampling frame that included all hospitals with ICUs or ICU beds in Canada, and reviewing policies independently and in duplicate using both quantitative and qualitative methods.
Conclusions
Most health authorities or hospitals in Canada posted visitation policies on websites during the COVID-19 pandemic. Most policies were hospital-wide rather than ICU-specific. The current study identifies the breadth of restrictions imposed by visitation policies across Canadian hospitals and ICUs before and during the first wave of COVID-19, with increased guidance for virtual visitation being provided when in-person visitation was not possible. Studies are underway to understand the consistency of policy operationalization and their impact on patient- and family-centred care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Author contributions
All authors made substantial contributions to this work. Kirsten M. Fiest, Karla D. Krewulak, Carmen Hiploylee, Henry T. Stelfox, and Jeanna Parsons Leigh designed the study and facilitated acquisition of data and interpreted the data. All authors provided expert consultation. Kirsten M. Fiest, Karla D. Krewulak, and Carmen Hiploylee drafted the manuscript; and all authors critically revised successive versions of the manuscript. Kirsten M. Fiest has full access to all the study data and assumes responsibility for the integrity of the data and the accuracy of the analysis.
Acknowledgements
The authors would like to thank Thérèse Poulin, Brianna Rosgen, and Zara Stelfox for assisting with the environmental scan. This manuscript underwent and internal peer review process with the Canadian Critical Care Trials Group, and we thank the helpful contributions made by Dr. Kim Lewis and Dr. Julie Reid.
Disclosures
None.
Funding statement
This work was supported by a COVID-19 Rapid Response Grant from the Canadian Institutes of Health Research (grant number 447521). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
This study is not registered in a public registry of clinical trials.
Editorial responsibility
This submission was handled by Dr. Stephan K.W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Footnotes
This manuscript is accompanied by an editorial. Please see Can J Anesth 2021; this issue.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Henry T. Stelfox and Jeanna Parsons Leigh are co-senior authors.
References
- 1.World Health Organization. Rolling updates on coronavirus disease (COVID-19) - 2020. Available from URL: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed April 2021).
- 2.Government of Canada. COVID-19 daily epidemiology update 2021. Available from URL: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html (accessed April 2021).
- 3.Inoue S, Hatakeyama J, Kondo Y, et al. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019;6:233–246. doi: 10.1002/ams2.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rawal G, Yadav S, Kumar R. Post-intensive care syndrome: an overview. J Transl Int Med. 2017;5:90–92. doi: 10.1515/jtim-2016-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103–128. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 6.da Silva Ramos FJ, Fumis RR, Azevedo LC, Schettino G. Perceptions of an open visitation policy by intensive care unit workers. Ann Intensive Care. 2013 doi: 10.1186/2110-5820-3-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fumagalli S, Boncinelli L, Lo Nostro A, et al. Reduced cardiocirculatory complications with unrestrictive visiting policy in an intensive care unit: results from a pilot, randomized trial. Circulation. 2006;113:946–952. doi: 10.1161/CIRCULATIONAHA.105.572537. [DOI] [PubMed] [Google Scholar]
- 8.McAdam JL, Puntillo KA. Open visitation policies and practices in US ICUs: can we ever get there? Crit Care. 2013 doi: 10.1186/cc12763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nassar Junior AP, Besen BA, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: a systematic review and meta-analysis. Crit Care Med. 2018;46:1175–1180. doi: 10.1097/CCM.0000000000003155. [DOI] [PubMed] [Google Scholar]
- 10.Shulkin D, O’Keefe T, Visconi D, Robinson A, Rooke AS, Neigher W. Eliminating visiting hour restrictions in hospitals. J Healthc Qual. 2014;36:54–57. doi: 10.1111/jhq.12035. [DOI] [PubMed] [Google Scholar]
- 11.Rosa RG, Tonietto TF, da Silva DB, et al. Effectiveness and safety of an extended ICU visitation model for delirium prevention: a before and after study. Crit Care Med. 2017;45:1660–1667. doi: 10.1097/CCM.0000000000002588. [DOI] [PubMed] [Google Scholar]
- 12.Carroll DL, Gonzalez CE. Visiting preferences of cardiovascular patients. Prog Cardiovasc Nurs. 2009;24:149–154. doi: 10.1111/j.1751-7117.2009.00053.x. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez CE, Carroll DL, Elliott JS, Fitzgerald PA, Vallent HJ. Visiting preferences of patients in the intensive care unit and in a complex care medical unit. Am J Crit Care. 2004;13:194–198. doi: 10.4037/ajcc2004.13.3.194. [DOI] [PubMed] [Google Scholar]
- 14.Jacob M, Horton C, Rance-Ashley S, et al. Needs of patients’ family members in an intensive care unit with continuous visitation. Am J Crit Care. 2016;25:118–125. doi: 10.4037/ajcc2016258. [DOI] [PubMed] [Google Scholar]
- 15.Marco L, Bermejillo I, Garayalde N, Sarrate I, Margall MA, Asiain MC. Intensive care nurses’ beliefs and attitudes towards the effect of open visiting on patients, family and nurses. Nurs Crit Care. 2006;11:33–41. doi: 10.1111/j.1362-1017.2006.00148.x. [DOI] [PubMed] [Google Scholar]
- 16.Kleinpell R, Zimmerman J, Vermoch KL, et al. Promoting family engagement in the ICU: experience from a national collaborative of 63 ICUs. Crit Care Med. 2019;47:1692–1698. doi: 10.1097/CCM.0000000000004009. [DOI] [PubMed] [Google Scholar]
- 17.Frampton S, Agrawal S, Guastello S. Guidelines for family presence policies during the COVID-19 pandemic. JAMA Health Forum. 2020 doi: 10.1001/jamahealthforum.2020.0807. [DOI] [PubMed] [Google Scholar]
- 18.Sasangohar F, Dhala A, Zheng F, Ahmadi N, Kash B, Masud F. Use of telecritical care for family visitation to ICU during the COVID-19 pandemic: an interview study and sentiment analysis. BMJ Qual Saf. 2020 doi: 10.1136/bmjqs-2020-011604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Government of Canada. Infection prevention and control for COVID-19: Interim guidance for acute healthcare setting. Available from URL: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/infection-prevention-control-covid-19-second-interim-guidance.html (accessed April 2021).
- 20.Canadian Agency for Drugs and Technologies in Health (CADTH). Environmental Scan Process 2015. Available from URL: https://www.cadth.ca/sites/default/files/pdf/ES%20External%20Audience%20Process%20Doc.pdf (accessed April 2021).
- 21.Holodinsky J. Mapping current adult intensive care unit patient care rounding practices. 2015; 10.11575/prism/26828.
- 22.Fowler RA, Abdelmalik P, Wood G, et al. Critical care capacity in Canada: results of a national cross-sectional study. Crit Care. 2015 doi: 10.1186/s13054-015-0852-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Darbyson K. Province relaxing hospital visitor restrictions. The Brandon Sun 2020 June 4, 2020. Available from URL: https://www.brandonsun.com/local/province-relaxing-hospital-visitor-restrictions-571004752.html (accessed April 2021).
- 24.Kouniakis A. Hamilton hospitals to welcome back visitors this week. In the Hammer. 2020 June 24, 2020. Available from URL: https://quickbitenews.com/article/hamilton/hamilton-hospitals-to-welcome-back-visitors-this-week/ (accessed April 2021).
- 25.Thomas B. COVID-19 Updates: 40 new cases reported Saturday | AHS relaxes restrictions on hospital visitations. Calgary Sun 2020 June 6, 2020. Available from URL: https://calgaryherald.com/news/local-news/covid-19-updates-ahs-relaxes-restrictions-on-hospital-visitations-kenney-warns-of-future-waves-of-covid-19 (accessed April 2021).
- 26.Giles D. Coronavirus: Some visitor restrictions eased at Saskatchewan Health Authority facilities. Global News. June 3, 2020. Available from URL: https://globalnews.ca/news/7020963/sask-health-authority-visitor-restrictions-coronavirus/ (accessed April 2021).
- 27.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013 doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Institute for Patient- and Family-Centered Care. Patient- and Family-Centered Care. Available from URL: https://ipfcc.org/about/pfcc.html (acessed April 2021).
- 29.Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative performance scale (PPS): a new tool. J Palliat Care. 1996;12:5–11. doi: 10.1177/082585979601200102. [DOI] [PubMed] [Google Scholar]
- 30.Chapman DK, Collingridge DS, Mitchell LA, et al. Satisfaction with elimination of all visitation restrictions in a mixed-profile intensive care unit. Am J Crit Care. 2016;25:46–50. doi: 10.4037/ajcc2016789. [DOI] [PubMed] [Google Scholar]
- 31.Garrouste-Orgeas M, Philippart F, Timsit JF, et al. Perceptions of a 24-hour visiting policy in the intensive care unit. Crit Care Med. 2008;36:30–35. doi: 10.1097/01.CCM.0000295310.29099.F8. [DOI] [PubMed] [Google Scholar]
- 32.Berwick DM, Kotagal M. Restricted visiting hours in ICUs: time to change. JAMA. 2004;292:736–737. doi: 10.1001/jama.292.6.736. [DOI] [PubMed] [Google Scholar]
- 33.McAdam JL, Puntillo K. Symptoms experienced by family members of patients in intensive care units. Am J Crit Care. 2009;18:200–209. doi: 10.4037/ajcc2009252. [DOI] [PubMed] [Google Scholar]
- 34.Canadian Foundation for Healthcare Improvement (CFHI). Re-Integration of Family Caregivers as Essential Partners in Care in a Time of COVID-19. Ottawa, ON; 2020. Available from URL: https://www.cfhi-fcass.ca/about/news-and-stories/news-detail/2020/07/08/re-integration-of-family-caregivers-as-essential-partners-in-care-in-a-time-of-covid-19 (accessed April 2021).
- 35.Andrist E, Clarke RG, Harding M. Paved with good intentions: hospital visitation restrictions in the age of coronavirus disease 2019. Pediatr Crit Care Med. 2020;21:e924–e926. doi: 10.1097/PCC.0000000000002506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carnevale FA. Moral distress in the ICU: it’s time to do something about it! Minerva Anestesiol. 2020;86:455–460. doi: 10.23736/S0375-9393.19.14021-7. [DOI] [PubMed] [Google Scholar]
- 37.Kanaris C. Moral distress in the intensive care unit during the pandemic: the burden of dying alone. Intensive Care Med. 2020;47:141–143. doi: 10.1007/s00134-020-06194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hui D, Nooruddin Z, Didwaniya N, et al. Concepts and definitions for “actively dying,” “end of life,” “terminally ill,” “terminal care,” and “transition of care”: a systematic review. J Pain Symptom Manage. 2014;4(7):77–89. doi: 10.1016/j.jpainsymman.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.White N, Reid F, Vickerstaff V, Harries P, Stone P. Specialist palliative medicine physicians and nurses accuracy at predicting imminent death (within 72 hours): a short report. BMJ Support Palliat Care. 2020;10:209–212. doi: 10.1136/bmjspcare-2020-002224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Detsky ME, Harhay MO, Bayard DF, et al. Discriminative accuracy of physician and nurse predictions for survival and functional outcomes 6 months after an ICU admission. JAMA. 2017;317:2187–2195. doi: 10.1001/jama.2017.4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Crit Care Med. 2012;40:618–624. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 42.Lee J. Calgary researcher hopes to improve ICU visitor restrictions during pandemic - 2021. Available from URL: https://www.cbc.ca/news/canada/calgary/research-intensive-care-unit-visitor-restrictions-1.5897735 (accessed April 2021).
- 43.Canadian Foundation for Healthcare Improvement (CFHI). Policy Guidance for the Reintegration of Caregivers as Essential Care Partners - 2020. Available from URL: https://www.cfhi-fcass.ca/docs/default-source/itr/tools-and-resources/policy_guidance_en.pdf?sfvrsn=292a980e_4 (accessed April 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.