Abstract
Background:
Cancellation/postponement of ”non-emergent” surgeries during coronavirus disease of 2019 (COVID-19) pandemic has created a huge backlog of patients waiting for surgery and has put them at risk of disease progression. We share our institute's policy and our department's attempt to resume ”non-emergent” surgeries.
Materials and Methods:
We collected details of all patients operated under department of neurosurgery since the onset of COVID-19 pandemic in India and categorized them into ”lockdown” and ”unlock” groups for comparison. COVID-19 tests done in these patients were also analyzed. We also compared our surgical volume with the number of COVID-19 cases in the state.
Results:
One hundred and forty-eight patients (97 males, 51 females) with mean age of 37.8 years (range-2 months-82 years) underwent surgery in our department during the study period. The operative volume per week increased by 37% during the ”unlock” period as compared to ”lockdown” period. The proportion of elective/”non-emergent” surgeries increased from 11.3% during ”lockdown” to 34.7% during the ”unlock” period (P = 0.0037). During ”lockdown” period, number of surgeries declined steadily as the number of COVID-19 cases rose in the state (rs(8) = −0.914, P = 0.000). Whereas there was a trend toward increased number of cases done per week despite increase in the number of cases in the state during the “unlock” period. During the ”unlocking” process, in-patient department admissions and surgeries performed per month increased (P = 0.0000) and this increase was uniform across all specialties. COVID-19 test was done (preoperatively or postoperatively) for all surgeries during ”unlock” period compared to 12 (22.6%) surgeries during ”lockdown” period. Three neurosurgery patients who underwent surgery during the ”unlock” period tested positive for COVID-19.
Conclusions:
Our experience shows that proper evidence-based protocols, setting up of adequate COVID-19 testing facilities and provision of ample personal protective equipments are instrumental in re-starting “nonemergent” surgeries.
Keywords: Coronavirus disease of 2019 (COVID-19), coronavirus disease of 2019 testing, elective surgeries, emergency surgeries, nonemergent surgeries, pandemic, routine surgeries
Introduction
”Success lies not in never falling but in rising up after every fall.” Even 6 months after the WHO declared coronavirus disease of 2019 (COVID-19) as a global pandemic,[1] most countries are still trying to recover from the initial impact of COVID-19. India reported its first case on January 30, 2020[2] and by the month of March 2020, it was clear that the country's health infrastructure was highly inadequate for the incoming tsunami of patients. With a meager expenditure of 1.28% of its GDP on healthcare, India has only eight doctors per 10,000 people, compared to 41 in Italy and 71 in South Korea. According to data from National Health Profile and the World Bank, India has 0.55 government hospital bed per 1000 population[3,4] and one government hospital for over 55,000 people.[3] By the extra pressure created by the COVID-19 pandemic, these health resources would have been easily over-whelmed. The country was not manufacturing personal protective equipment (PPE) and because of the high cost of import, they were very expensive and in short supply.[5] In a survey conducted by the authors between 7 and 23 May 2020, most neurosurgeons in the country felt that there was a shortage of PPE in their respective hospitals.[6] Ventilators were highly inadequate in numbers.[4] There were handful of laboratories with facilities to do COVID-19 testing. Having witnessed the mayhem created by the virus in the western countries with more organized health-care facilities, the union government of India took the bold decision of a nation-wide “lockdown” from March 25, 2020, which lasted till May 31, 2020.
Ten weeks of nation-wide ”lockdown”
During these 10 weeks, the country went into ”fifth-gear” in its preparation against COVID-19. The country's masses were educated by social media and various other platforms about the preventive measures to be adopted. The third Empowered Group of Secretaries was tasked with the responsibility of ensuring the availability and production of essential medical equipments along with their procurement, import, and distribution.[7] Indian companies responded efficiently to the COVID-19 pandemic by fast-tracking innovation, revamping assembly lines, and expediting manufacturing of everything from N95 masks and PPE to diagnostic kits and ventilators in record time. Within a matter of 2 months, 600 companies were certified to make PPE kits and thus, India became the second-largest producer of PPE kits, producing 450,000 units per day.[5,8] Many small-and large-scale companies initiated the process of making low-cost ventilators in the country. Remarkably, from producing almost no ventilators domestically, India indigenously manufactured 60,000 ventilators in just 3 months.[7] Fully equipped virology laboratories for COVID-19 testing were set-up in various parts of the country according to Indian Council of Medical Research (ICMR) standards.
The hospitals and medical institutions utilized the “lockdown” period to prepare themselves for the incoming COVID-19 patients. Procurement of essential commodities like ventilators, monitors, PPE, and other protective equipment was expedited. In some areas, some hospitals dedicated for COVID-19 care were defined and non-COVID-19 work was delegated to certain hospitals. In some hospitals like ours, dedicated COVID-19 and non-COVID-19 areas were defined. Doctors, nurses, and support staff were deployed in these areas by rotation.[9]
Concerns about cancellation/postponement of “nonemergent” cases
During the lockdown period, the cases which were considered “nonemergent” were cancelled/postponed[10] in order to keep the beds and staff available for the expected steep rise in the COVID-19 patients and to keep the healthcare workers (HCWs) from contracting COVID-19 in the absence of adequate PPE. Such cancellation of cases was seen across the globe[11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] and was in accordance with recommendations from the American College of Surgeons and Centres for Medicare and Medicaid Services.[38,39,40]
However, there were concerns amongst HCWs about patients with ”nonemergent”-non-COVID-19 conditions being neglected care.[10] If denied care for too long, there was a risk of these patients presenting at a later stage with progressed disease and therefore, an alternative to postponing elective surgeries was required. The authors suggested that the best way forward would be to resume work with necessary precautions and universal effective COVID-19 testing.[6,9,10,14]
Return of ”normalcy” in the country
Ground-level work during the ”lockdown” had allowed the hospitals and the country to be somewhat ”prepared.” In order to sustain the economy and allow resumption of “normalcy,” the nation-wide ”lockdown” was eased from June 1, 2020. This was termed as ”unlocking,” which was done in phased manner-”unlock 1” from June 1, “unlock 2” from July 1 and “unlock 3” from August 1. Strict guidelines were issued for the public regarding the need to still maintain ”social distance,” avoid crowded places, wear masks while going out, going out of the house only when absolutely necessary and allow ”work-from-home” to employees whenever feasible. Large public gatherings like conferences, social and religious functions are still restricted and strictly regulated. The country was categorized into three different zones (”red zones,” ”orange zones” and ”green zones”) based on the COVID-19 case load. This categorization was dynamic in nature, based on the changing COVID-19 scenario in the country.[9]
Measures taken in our institute to bring back ”normalcy”
Rishikesh is a town in Dehradun district, in the Himalayan state of Uttarakhand. Dehradun district has been categorized as an ”orange zone.” The institute in Rishikesh, where the study was conducted is a 960-bedded hospital with 105 ICU beds. With 276 attending faculty, 694 residents and 1326 registered nurses, it is the major hospital providing tertiary medical care to the people of Uttarakhand and western Uttar Pradesh. In the pre-COVID-19 era, the institute had an overall out-patient department (OPD) volume of around 70,000–80,000 patients per month and a total of 28,949 surgeries were performed at the institute in 2019.
Looking at the need to resume ”non-emergent” health services, several measures were taken at the institute level in order to ensure some sense of ”normalcy” and allow HCWs to resume ”normal” work.
Supplies: Adequate PPEs were procured for the HCWs. Procurement of ventilators and monitors was expedited
Training of HCWs: During the ”lockdown” period, new virtual COVID-19-related educational programs were created for HCWs of all clinical and nonclinical departments to facilitate their deployment in common COVID-19 areas
Demarcation of COVID-19 areas: In our institute, the hospital is divided into COVID-19 areas and non-COVID-19 areas. Non-COVID-19 areas are meant for regular work of various specialties for patients who have been tested negative. COVID-19 areas are meant for COVID-19 suspect or confirmed cases with separate areas for each. Though the scenario is ever-changing with re-allocation of more and more ward and ICU beds for COVID-19 patients, at present the COVID-19 area has a bed strength of 260 ward beds and 164 ICU beds
Testing, testing, testing: COVID-19 testing using reverse transcriptase-polymerase chain reaction from nasopharyngeal and oropharyngeal swabs began in our institute on March 30, 2020 according to the ICMR protocol. Since May 2, 2020, COVID-19 testing has been made a prerequisite for all patients getting admitted to the hospital
Starting from June, there was a change in our policy to doing one COVID-19 test before admitting any patient to the hospital and doing another COVID-19 test before surgery/procedure to decrease the chances of transmission from false-negative patients
Physical OPDs had been completely replaced by telemedicine during the lockdown period. During the ”unlock” period, limited physical OPD was allowed with the provision of screening OPD, where all patients coming to the hospital undergo thermal screening and are asked for COVID-19-related history
Resumption of ”nonemergent” surgeries: Routine or ”nonemergent” surgeries which had been largely curtailed earlier were resumed. The department of neurosurgery was allotted an operation room (OR) slot on daily basis like in the pre-COVID times
Staffing had been reduced during the lockdown period to avoid spread of COVID-19. Now, more and more HCWs are encouraged to be present in order to resume nonemergent work. At the same time, they are advised to strictly follow guidelines to prevent the spread of the disease. Every employee is required on-site to wear face mask protection and to attest daily to symptom-free status
Physical meetings are still avoided as much as possible
Out-station leaves of HCWs had been curtailed since the onset of pandemic, but were allowed now for them to meet their near-and-dear ones. However, the institute followed strict policy of quarantine on their return
Any HCW suspected of having any COVID-19-related symptoms or ”high-risk” exposure to a COVID-19-positive patient was isolated and tested for COVID-19[9]
Protocol for COVID-19-positive HCWs: In spite of these measures, on certain days, up to 5–10 HCWs would become COVID-19 positive. Any HCW who would test positive for COVID-19 is isolated immediately. In the initial part of the pandemic, even the asymptomatic and mildly symptomatic patients were isolated in the COVID-19 area of the hospital. However, since the change in the state health policy on August 10, 2020, asymptomatic/mildly asymptomatic HCWs/patients are now allowed home isolation with strict instructions.[41] This helps in sparing the hospital beds for sicker patients. They are kept in isolation for 14 days and tested again for COVID-19 on days 7 and 14. They are allowed to resume work in case of negative test results.
Road-blocks on the way to ”normalcy”
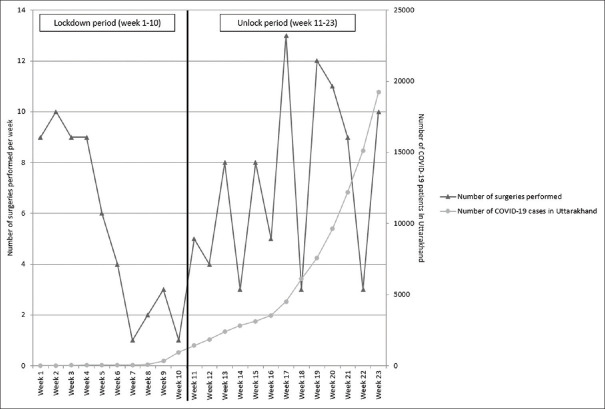
Looking at the surge in the number of COVID-19 cases in the state [Figure 1] as well as amongst the HCWs in the institute, it was again felt that maximum HCWs needed to be spared for the COVID-19-related work to allow further expansion of COVID-19-related services. Therefore, the staff posted for non-COVID-19 ”nonemergent” duties were re-deployed to COVID-19-related duties. Due to this change in policy, the number of routine OR slots for various surgical department was decreased and the neurosurgery department was allotted only two routine OR slots per week w.e.f. August 14, 2020. This again made it extremely difficult to attend to the patients with ”nonemergent” ailments. At the time of writing this article, the physical screening OPDs were again curtailed since September 2, 2020.
Figure 1.
Frequency polygon depicting the number of surgeries performed per week in relation to the rising trend of COVID-19 cases in Uttarakhand during the pandemic. During the lockdown period, there was a strongly negative correlation between the number of surgeries performed and the number of COVID-19 cases in the state and this result was statistically significant (rs (8) = −0.914, P = 0.000). While in the unlock phase, there was a weak correlation between the number of surgeries performed and the number of COVID-19 cases in the state. This result was not significant (rs (11) = 0.307, P = 0.307)
Objective of the study
The authors have previously demonstrated that during the ongoing COVID-19 pandemic, there was a substantial decrease in the volume and spectrum in the neurosurgical patients, especially those with ”non-emergent” conditions.[10] Following this analysis and with the proper hospital preparation during the ”lockdown” period, we felt an urgent need to restart ”nonemergent” work. The authors analysed the department census to assess the spectrum and volume of patients operated in order to assess the degree of return to ”normalcy” in the department functioning during the ”unlock” period compared to the ”lockdown” period.
Materials and Methods
We collected the details of all patients who underwent surgery under the Department of Neurosurgery at our institute since the onset of COVID-19 pandemic in the country (partially retrospectively and partially prospectively). The patients operated were categorized into two groups-”lockdown” group and ”unlock” group depending on whether they were operated in the ”lockdown” period (March 25 to May 31, 2020) or after the beginning of ”unlocking” (June 1 to August 31, 2020). The demographic profile, diagnoses, surgeries performed, type of surgery (routine/emergency, cranial/spinal and major/minor) in these two groups were compared. The patients were further categorized into various categories (i.e. neuro-oncology [brain and spine tumors], neuro-trauma [head injury and spinal trauma], congenital cases, degenerative spine, neuro-vascular, cerebrospinal fluid [CSF] diversion procedures, etc.) and compared between the two groups.
A comparison was made between the number of cases operated in our department weekly with the number of confirmed COVID-19 cases in the state of Uttarakhand. Data on the number of confirmed COVID-19 cases in the state of Uttarakhand were collected from the official website of the Ministry of Health and Family welfare.[42] Monthly data for the number of in-patient department (IPD) admissions and surgeries performed during the ongoing pandemic was retrieved from the institute's official data. This monthly data were compared with data from the same duration in 2019.
Statistical analysis was performed using IBM Statistical Package for Social Sciences (SPSS version 25.0, SPSS, Inc., Chicago, IL, USA). Continuous variables were expressed as mean and range while categorical variables were expressed as frequencies. Chi-square test was used to test for the association between groups of categorical variables. To assess the correlation between the number of surgeries performed and the number of COVID-19 cases in the state of Uttarakhand, we used Spearman's rank correlation coefficient.
Results
One hundred and forty-eight patients (97 males, 51 females) with a mean age of 37.8 years (range 2 months–82 years) underwent surgery in our department since the onset of COVID-19 pandemic in the country. Of these, 53 (6 elective, 47 emergency) were operated during the 10 weeks of ”lockdown” period and 95 (33 elective, 62 emergency) during the ”unlock” period (13 weeks) [Table 1]. Thus, the operative volume per week increased by 37% during the ”unlock” period as compared to the ”lockdown” period.
Table 1.
Comparing the data between the “lockdown” period and “unlock” period
| Lockdown period (March 25th to May 31st) | Unlock period (June 1st to August 31st) | |
|---|---|---|
| Duration (weeks) | 10 | 13 |
| Total cases operated | 53 | 95 |
| Male: female | 36:17 | 61:34 |
| Mean age of patients in years | 38.46 | 37.41 |
| Age range | 2 months-72 years | 5 months-82 years |
| Elective surgeries (%) | 6 (11.3) | 33 (34.7) |
| Emergency surgeries (%) | 47 (88.7) | 62 (65.3) |
| Major surgeries (%) | 31 (58.5) | 61 (64.2) |
| Minor surgeries (%) | 22 (41.5) | 34 (35.8) |
| Cranial cases (%) | 47 (88.6) | 83 (87.4) |
| Spinal cases (%) | 6 (11.3) | 12 (12.6) |
| Specialty-wise distribution (%) | ||
| Brain tumour | 12 (22.6) | 18 (18.9) |
| Congenital | 0 (0) | 3 (3.2) |
| Cranial infection | 1 (1.9) | 1 (1.1) |
| CSF diversion procedures | 16 (30.2) | 22 (23.2) |
| Degenerative spine | 0 (0) | 4 (4.2) |
| Head injury | 12 (22.6) | 30 (31.6) |
| Neurovascular (ruptured aneurysms) | 2 (3.8) | 5 (5.3) |
| Peripheral nerves | 0 (0) | 0 (0) |
| Spinal infection | 1 (1.9) | 0 (0) |
| Spinal trauma | 3 (5.7) | 0 (0) |
| Spinal tumour | 2 (3.8) | 5 (5.3) |
| Stroke | 2 (3.8) | 2 (2.1) |
| Miscellaneous | 2 (3.8) | 5 (5.3) |
| COVID-19 testing (%) | ||
| Number of surgeries done without any COVID-19 test (preoperative/postoperative) | 41 (77.4) | 0 (0) |
| Number of surgeries with one preoperative COVID-19 test | 7 (13.2) | 47 (49.5) |
| Number of surgeries with two or more preoperative COVID-19 tests | 0 (0) | 16 (16.8) |
| Number of surgeries in which COVID-19 test done postoperatively and not preoperatively | 5 (9.4) | 32 (33.6) |
| COVID-19 positive patients | 0 (0) | 3 (3.2) |
During the “unlock” period, there was an increase in the number of surgeries performed, across all specialties. COVID-19 test was done (either pre- or post-operatively) for all surgeries done during “unlock” period compared to 12 (22.6%) surgeries during the “lockdown” period. COVID-19 – Coronavirus disease 2019; CSF – Cerebrospinal fluid
No elective cases were done during the month of May, following which the number of elective cases steadily increased from July to August during the unlock phase. The proportion of elective/”non-emergent” surgeries increased from 11.3% during the ”lockdown” period to 34.7% during the ”unlock” period and this result was statistically significant (P = 0.0037) [Figure 2].
Figure 2.
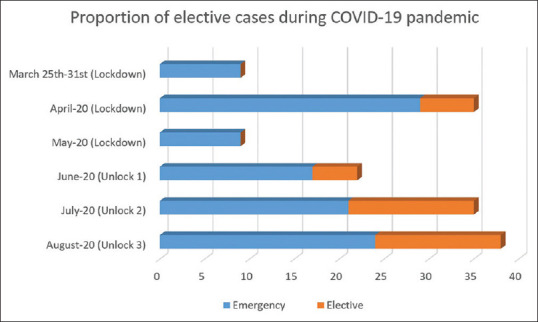
Horizontal stacked bar graph depicting the number of elective and emergency surgeries performed in each month since the onset of pandemic in the country. No elective cases were done during the month of May (lockdown period). The number of elective cases increased from 0 in May to 5 in June and 14 each in July and August. The proportion of nonemergent/elective surgeries increased from 11.3% during the “lockdown” period to 34.7% during the “unlock” period and this result was statistically significant (P = 0.0037)
When the monthly operative volume was compared to the data from last year, it was observed that the number of surgeries reached the lowest point during the ”lockdown” in May when only nine cases were operated. With the process of ”unlock” in the country, there was a trend towards increasing number of cases per month (22 in June, 35 in July and 38 in August) [Figure 3]. Similar trend was observed in the IPD admissions. In fact, IPD admissions in July and August 2020 exceeded those in July and August 2019, respectively [Figure 4].
Figure 3.
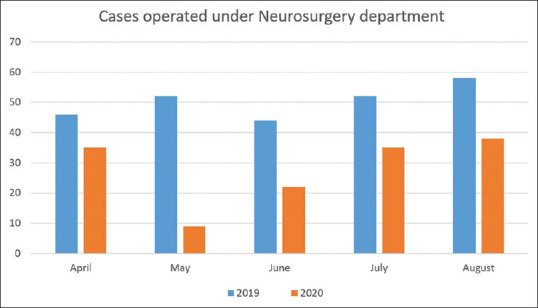
Vertical bar graph depicting number of surgeries performed from April to August in 2019 and 2020. During the ”lockdown” period of April and May, 44.9% surgeries were performed as compared to same months in 2019, whereas in the “unlock” period of June, July and August, this proportion increased to 63.6% compared to the same months in 2019 (P = 0.1889). However, when the same data for the 3 months of ”unlock” period was compared with month of May alone (17.3% surgeries in 2020 compared to last year), this difference was statistically significant (P = 0.0009)
Figure 4.
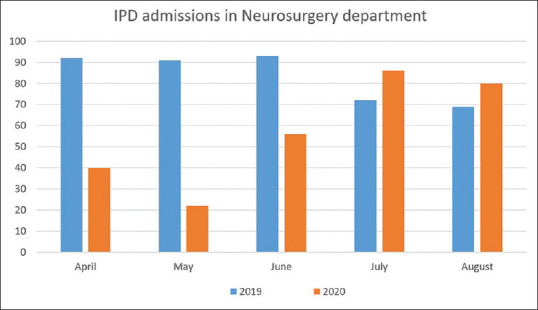
Vertical bar graph depicting the number of in-patient department admissions from April to August in 2019 and 2020. During the ”lockdown” period of April and May, there were only 33.9% hospital admissions as compared to same months in the previous year, whereas in the ”unlock” period of June, July and August, this proportion increased to 94.9% compared to the same months in the previous year. This change was found to be statistically significant (P < 0.00001)
Comparison with COVID-19 cases in the state
In the state of Uttarakhand, there were 907 COVID-19 patients at the end of ”lockdown” on May 31, 2020, while on August 31, 2020, the number had increased to 19,235. On comparing the number of COVID-19 cases in the state with the number of surgeries performed per week, it was observed that during the ”lockdown” period, a strong negative correlation was found between the number of surgeries performed per week and the number of COVID-19 cases in the state and this result was statistically significant (rs (8) = −0.914, P = 0.000). In other words, during the lockdown period, the number of surgeries performed declined steadily as the number of COVID-19 cases rose in the state. Whereas, during the “unlock” period, there was a weakly positive correlation between the number of surgeries performed per week and the number of COVID-19 cases in the state. However, this result was not statistically significant (rs (11) = 0.307, P = 0.307). This implies a trend toward increased number of cases done per week in spite of increase in the number of cases in the state during the “unlock” period [Figure 1].
During the ongoing COVID-19 pandemic, 56 cases (37.8%) were minor cases (burr hole tapping of abscess/chronic subdural hemorrhage, ventriculoperitoneal shunt, external ventricular drainage, endoscopic third ventriculostomy, lumbar discectomy), while 92 (62.2%) were major cases. One hundred and thirty cases (87.8%) were cranial while 18 (12.2%) were spinal [Table 1].
Specialty-wise distribution
Overall, majority of cases in the study were of neuro-trauma (45 cases, 30.4%); CSF diversion procedures (38 cases, 25.7%) and neuro-oncology (37 cases, 25.0%). The number of neuro-oncology increased from 14 (12 cranial, 2 spinal) in the ”lockdown” period to 23 (18 cranial, 5 spinal) during the ”unlock” period. Overall, two cases of brain tumor were operated by the trans-sphenoidal route (one each in ”lockdown” and ”unlock” period). Neuro-trauma cases also increased from 15 (12 head injuries, 3 spinal injuries) during the ”lockdown” period to 30 (all head injuries) during the ”unlock” period. Importantly, no patient underwent surgery for the congenital condition or degenerative spinal disorders during the ”lockdown” period, whereas three cases of congenital conditions and four cases of degenerative spine underwent surgery during the ”unlock” phase [Figure 5].
Figure 5.
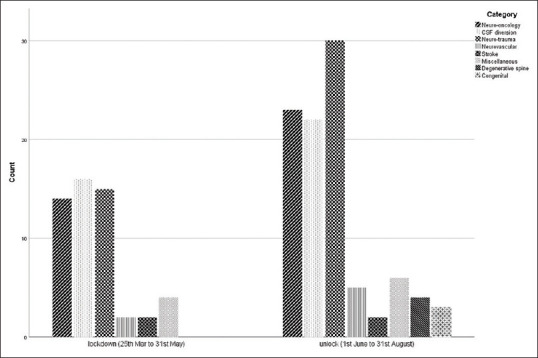
Clustered bar graph depicting the speciality-wise distribution of surgeries performed between lockdown period (March 25 to May 31, 2020) and 'unlock' period (June 1 to August 31, 2020). An increase in surgeries of all specialties is observed. No surgeries for congenital conditions and degenerative spinal conditions were performed during the lockdown period
COVID-19 testing
At our institute, from April 25, 2020 onward, COVID-19 testing was made a prerequisite for those undergoing any surgery. Following this rule, 12 surgeries were performed in the ”lockdown” period. Seven of these were done with a single preoperative COVID-19 test, while five (four head injuries and one ventriculo-peritoneal shunt) were taken up as acute emergencies without preoperative testing. In these five cases, testing was done following the surgery. Test results of all cases during the ”lockdown” phase were negative [Table 1].
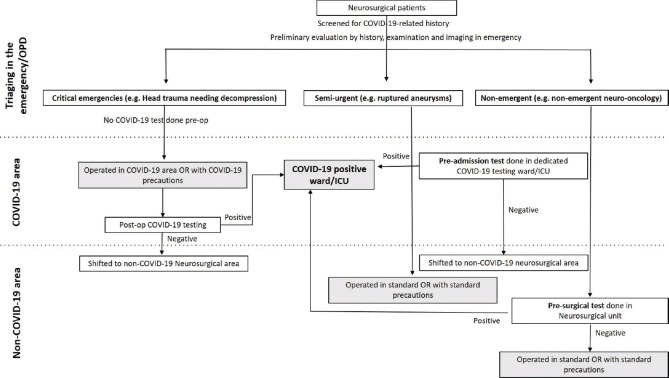
From June onward in the ”unlock” phase, the protocol was further changed to doing two COVID-19 tests before elective surgeries-one at admission and another before the day of surgery [Figure 6]. During the ”unlock” phase, all patients underwent COVID-19 testing. Forty-seven patients underwent single preoperative COVID-19 testing while 16 underwent two or more preoperative testing. Thirty-two patients (25 head injuries, one decompressive hemi-craniectomy for stroke and six CSF-diversion procedures) underwent emergency surgeries without preoperative COVID-19 tests. All these patients underwent COVID-19 testing following the surgery [Table 1].
Figure 6.
Protocol for triaging and COVID-19 testing at our institute during the COVID-19 pandemic
Three neurosurgery patients who underwent surgery during the ”unlock” period tested positive for COVID-19 [Table 1]. Two of these tested positive for COVID-19 on preoperative testing and were operated after being in isolation for 14 days and with three negative test results. The third patient initially tested negative for COVID-19 on preoperative testing and underwent surgery in the standard OR with standard precautions. In the postoperative period, as his relative tested positive for COVID-19, he was tested again for COVID-19 and was found to be positive this time. He was discharged after 14 days of isolation and with two negative COVID-19 test reports.
Discussion
In our previous articles, we have raised concerns about the impact of COVID-19 pandemic on non-COVID-19 patients considered to be ”non-emergent.”[6,9,10,15,43,44,45,46,47,48,49,50,51] If postponed for too long, these patients risk presenting with more advanced diseases at a later stage. In this article, we have presented the response of our institute and neurosurgery department during the ongoing COVID-19 pandemic in an attempt to highlight our attempts to attend to the ”nonemergent” patients along with COVID-19 and emergent cases. The ”lockdown” period gave us time to have a system in place so that we can take care of COVID-19 patients and plan delegation of the remaining resources to non-COVID-19 tasks so that patients with non-COVID-19 conditions are not completely neglected.
In a seminal study, patients with peri-operative COVID-19 infection had 30-day mortality of 23.8% following elective surgery and 51.2% had pulmonary complications.[52] At our center, all patients getting admitted to the hospital for elective surgery are being tested for COVID-19 in dedicated COVID-19 testing wards.[9] Surgery for those who test positive for COVID-19 is postponed until the test results are negative, where possible as was done in two of our cases. Once a patient tests negative for COVID-19, he/she is shifted to the non-COVID-19 area. If the patient's condition is semi-urgent, he/she undergoes surgery in the non-COVID-19 OR with standard precautions. If the patient's condition is ”non-emergent,” another COVID-19 test is done in the neurosurgical area before surgery. Patients who do require urgent surgery, are assumed to be COVID-19 positive until proven otherwise, and managed accordingly in the OR in the COVID-19 area. In accordance with this, a level-III PPE is worn. This is to mitigate the possible risk of operating on asymptomatic COVID-19-positive patients, which is increasing with the increased community prevalence,[53] and in the absence of preoperative COVID-19 testing. Such patients undergo COVID-19 testing in the postoperative period and are shifted to the non-COVID-19 area only after testing negative for COVID-19 [Figure 6].
Proper evidence-based protocols, setting up of adequate COVID-19 testing facilities, and provision of ample PPEs have allowed HCWs to feel protected while discharging their duties. This relative security has transpired into a motivated and confident healthcare work-force in the institute. These developments and proper planning have allowed neurosurgery team and other specialties to resurrect ”nonemergent” services especially since the ”unlock” process has begun. Our report highlights that the IPD admissions largely normalized during the ”unlock” period and the number of surgeries performed are on a rising trend in spite of the rising number of COVID-19 cases in the state. The proportion of ”non-emergent” cases has also increased significantly compared to the ”lockdown” period. The spectrum of surgeries during the ”unlock” phase has been broadened.
However, resuming work to the level of pre-COVID-19 times has not been easy, as despite vigorous testing policy being followed at our institute, we are witnessing large number of HCWs testing positive for COVID-19. The need to isolate these HCWs and quarantine their contacts often results in depletion in the available work-force at the hospital. We observed resumption of normal ”nonemergent” activity in June, July and early August 2020. However, increasing COVID-19 cases and depleted work-force halted this process of resumption. This forced us intermittently to decrease our ”nonemergent” work to deploy more working hands for COVID-19 care. These interuptions can be better appreciated in our weekly operative work-load [Figure 1], even though overall our monthly operative work-load and IPD admissions showed a reviving trend. Currently, in the second half of August 2020 we are hopeful that this phase of halting care is only temporary.
Conclusions
It is evident from our experience that proper-evidence based protocols are required to prevent the HCWs from contracting COVID-19 and make them feel safe. We have presented our institute's protocol in the hope that it will be beneficial to our colleagues around the world who are going through a similar phase of trying to achieve ”normalcy.” The HCWs will have to rise above the challenge and try to resume work with necessary precautions. At times, the virus will put us down, but we should still try to get back up as soon as possible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Coronavirus (COVID-19) Events as They Happen. [Last accessed on 2020 Sep 08]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen .
- 2.Reid D. CNBC; 2020. [Last accessed on 2020 Jun 21]. India Confirms its First Coronavirus Case. Available from: https://www.cnbc.com/2020/01/30/indiaconfirms-first-case-of-the-coronavirus.html . [Google Scholar]
- 3.Can India Keep Up with COVID-19? [Last accessed on 2020 Sep 08]. Available from: https://thediplomat.com/2020/03/india-challenged-by-covid-19/
- 4.Singh P, Ravi S, Chakraborty S. COVID-19 | Is India's Health Infrastructure Equipped to Handle an Epidemic? Brookings. 2020. [Last accessed on 2020 Sep 08]. Available from: https://www.brookings.edu/blog/upfront/2020/03/24/is-indias-health-infrastructure-equipped-tohandle-an-epidemic/
- 5.From Zero, India Now Manufactures 4.5 Lakh PPE Suits A Day To Fight Coronavirus. NDTV.Com. [Last accessed on 2020 Sep 08]. Available from: https://www.ndtv.com/india-news/from-zero-india-now-manufactures-4-5-lakh-ppe-suits-a-day-to-fight-coronavirus-2231742 .
- 6.Venkataram T, Goyal N, Dash C, Chandra PP, Chaturvedi J, Raheja A, et al. Impact of the COVID-19 pandemic on neurosurgical practice in India: Results of an anonymized national survey. Neurol India. 2020;68:595–602. doi: 10.4103/0028-3886.289004. [DOI] [PubMed] [Google Scholar]
- 7.Helping India Breathe: Ventilator Manufacturing During Covid-19. [Last accessed on 2020 Sep 08]. Available from: https://www.investindia.gov.in/siru/helping-india-breathe-ventilator-manufacturing-duringcovid-19 .
- 8.BOOM. COVID-19: How India Became A PPE Kit Manufacturing Hub. 2020. [Last accessed on 2020 Sep 08]. Available from: https://www.boomlive.in/videos/fact-file/covid-19-how-india-became-a-ppekit-manufacturing-hub-8408 .
- 9.Venkataram T, Goyal N, Kalita D, Bahurupi Y, Gangotri , Sadhasivam S, et al. Deployment of neurosurgeons at the warfront against coronavirus disease of 2019 (COVID-19) World Neurosurg. 2020;144:e561–7. doi: 10.1016/j.wneu.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goyal N, Venkataram T, Singh V, Chaturvedi J. Collateral damage caused by COVID-19: Change in volume and spectrum of neurosurgery patients. J Clin Neurosci. 2020;80:156–61. doi: 10.1016/j.jocn.2020.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–9. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathiesen T, Arraez M, Asser T, Balak N, Barazi S, Bernucci C, et al. A snapshot of European neurosurgery December 2019 vs. March 2020: Just before and during the Covid-19 pandemic. Acta Neurochir (Wien) 2020;162:2221–33. doi: 10.1007/s00701-020-04482-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fontanella MM, De Maria L, Zanin L, Saraceno G, Terzi di Bergamo L, Servadei F, et al. neurosurgical practice during the severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) pandemic: A worldwide survey. World Neurosurg. 2020;139:e818–26. doi: 10.1016/j.wneu.2020.04.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goyal N, Venkataram T, Dash C, Chandra P. Letter to the editor regarding: Impact of COVID-19 on an academic neurosurgery department: The johns hopkins experience. World Neurosurg. 2020;143:599–600. doi: 10.1016/j.wneu.2020.07.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khalafallah AM, Jimenez AE, Lee RP, Weingart JD, Theodore N, Cohen AR, et al. Impact of COVID-19 on an Academic Neurosurgery Department: The Johns Hopkins Experience. World Neurosurg. 2020;139:e877–84. doi: 10.1016/j.wneu.2020.05.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubansu A, Assamadi M, Barrit S, Dembour V, Yao G, Hadwe SE, et al. COVID-19 impact on neurosurgical practice: Lockdown attitude and experience of a European academic center. [Last accessed on 2020 Sep 06];World Neurosurg. 2020 144:e380–e388. doi: 10.1016/j.wneu.2020.08.168. Available from: http://www.sciencedirect.com/science/article/pii/S1878875020319379 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jayakumar N, Kennion O, Villabona AR, Paranathala M, Holliman D. Neurosurgical referral patterns during the COVID-19 pandemic: A United Kingdom experience. World Neurosurg. 2020;144:e414–20. doi: 10.1016/j.wneu.2020.08.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahuja S, Shah P, Mohammed R. Impact of COVID-19 pandemic on acute spine surgery referrals to UK tertiary spinal unit: Any lessons to be learnt. Br J Neurosurg. 2020:1–5. doi: 10.1080/02688697.2020.1777263. https://doi.org/10.1080/02688697.2020.1777263. [DOI] [PubMed] [Google Scholar]
- 19.Ham CH, Moon HJ, Kim JH, Park YK, Lee TH, Kwon WK. Coronavirus Disease (COVID-19) outbreak and its impact on spinal daily practice: Preliminary Report from a Single (Regional) University Hospital in Republic of Korea. J Korean Neurosurg Soc. 2020;63:407–14. doi: 10.3340/jkns.2020.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noureldine MH, Pressman E, Krafft PR, Greenberg MS, Agazzi S, van Loveren H, et al. Impact of the COVID-19 Pandemic on Neurosurgical Practice at an Academic Tertiary Referral Center: A comparative study. World Neurosurg. 2020;139:e872–6. doi: 10.1016/j.wneu.2020.05.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marini A, Iacoangeli M, Dobran M. Letter to the Editor Regarding “Coronavirus Disease 2019 (COVID-19) and Neurosurgery: Literature and Neurosurgical Societies Recommendations Update”. World Neurosurg. 2020;141:536–7. doi: 10.1016/j.wneu.2020.05.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deora H, Mishra S, Tripathi M, Garg K, Tandon V, Borkar S, et al. Adapting neurosurgery practice during the Covid-19 pandemic in the indian subcontinent. World Neurosurg. 2020;142:e396–406. doi: 10.1016/j.wneu.2020.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bajunaid K, Alqurashi A, Alatar A, Alkutbi M, Alzahrani AH, Sabbagh AJ, et al. Neurosurgical procedures and safety during the COVID-19 pandemic: A case-control multicenter study. [Last accessed on 2020 Aug 20];World Neurosurg. 2020 143:e179–e187. doi: 10.1016/j.wneu.2020.07.093. Available from: http://www.sciencedirect.com/science/article/pii/S1878875020316144 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alhaj AK, Al-Saadi T, Mohammad F, Alabri S. Neurosurgery residents' perspective on COVID-19: Knowledge, readiness, and impact of this pandemic. World Neurosurg. 2020;139:e848–58. doi: 10.1016/j.wneu.2020.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lara-Reyna J, Yaeger KA, Rossitto CP, Camara D, Wedderburn R, Ghatan S, et al. “Staying Home” – Early Changes in Patterns of Neurotrauma in New York City During the COVID-19 Pandemic. World Neurosurg. 2020;143:e344–50. doi: 10.1016/j.wneu.2020.07.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thapa A. COVID-19 and the Role of Neurosurgeons in Nepal. World Neurosurg. 2020;139:629–31. doi: 10.1016/j.wneu.2020.05.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abboud H, Abboud FZ, Kharbouch H, Arkha Y, El Abbadi N, El Ouahabi A. COVID-19 and SARS-Cov-2 Infection: Pathophysiology and clinical effects on the nervous system. World Neurosurg. 2020;140:49–53. doi: 10.1016/j.wneu.2020.05.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernucci C, Brembilla C, Veiceschi P. Effects of the COVID-19 outbreak in northern Italy: Perspectives from the bergamo neurosurgery department. World Neurosurg. 2020;137:465–8.e1. doi: 10.1016/j.wneu.2020.03.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.D'Amico RS, Baum G, Serulle Y, Silva D, Smith ML, Wallack RA, et al. A roadmap to reopening a neurosurgical practice in the age of COVID-19. World Neurosurg. 2020;139:289–93. doi: 10.1016/j.wneu.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mouchtouris N, Lavergne P, Montenegro TS, Gonzalez G, Baldassari M, Sharan A, et al. Telemedicine in neurosurgery: Lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–94. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ozoner B, Gungor A, Hasanov T, Toktas ZO, Kilic T. Neurosurgical practice during coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020;140:198–207. doi: 10.1016/j.wneu.2020.05.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pressman E, Noureldine MH, Kumar JI, Krafft PR, Mantei B, Greenberg MS, et al. The return back to typical practice from the “battle plan” of the coronavirus disease 2019 (COVID-19) pandemic: A comparative study. World Neurosurg. 2020;142:e481–6. doi: 10.1016/j.wneu.2020.07.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rispoli R, Diamond ME, Balsano M, Cappelletto B. Spine Surgery in Italy in the COVID-19 Era: Proposal for assessing and responding to the regional state of emergency. World Neurosurg. 2020;145:e1–6. doi: 10.1016/j.wneu.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rothrock RJ, Maragkos GA, Schupper AJ, McNeill IT, Oermann EK, Yaeger KA, et al. By the numbers analysis of effect of COVID-19 on a neurosurgical residency at the epicenter. World Neurosurg. 2020;142:e434–9. doi: 10.1016/j.wneu.2020.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saad H, Alawieh A, Oyesiku N, Barrow DL, Olson J. Sheltered neurosurgery during COVID-19: The emory experience. World Neurosurg. 2020;144:e204–9. doi: 10.1016/j.wneu.2020.08.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sivakanthan S, Pan J, Kim L, Ellenbogen R, Saigal R. Economic impact of COVID-19 on a high-volume academic neurosurgical practice. World Neurosurg. 2020;143:e561–6. doi: 10.1016/j.wneu.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wittayanakorn N, Weng Nga VD, Sobana M, Ahmad Bahuri NF, Baticulon RE. Impact of COVID-19 on neurosurgical training in Southeast Asia. World Neurosurg. 2020;144:e164–77. doi: 10.1016/j.wneu.2020.08.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures during COVID-19 Response | CMS. [Last accessed on 2020 Jun 12]. Available from: https://www.cms.gov/newsroom/press-releases/cms-releases-recommendationsadult-elective-surgeries-non-essential-medical-surgical-and dental .
- 39.COVID-19: Elective Case Triage Guidelines for Surgical Care. [Last accessed on 2020 Jun 12]. Available from: https://www.facs.org/covid-19/clinical-guidance/elective-case .
- 40.Gupta P, Muthukumar N, Rajshekhar V, Tripathi M, Thomas S, Gupta SK, et al. Neurosurgery and neurology practices during the novel COVID-19 pandemic: A consensus statement from India. Neurol India. 2020;68:246–54. doi: 10.4103/0028-3886.283130. [DOI] [PubMed] [Google Scholar]
- 41.Uttarakhand Allows Home Isolation for Asymptomatic Covid-19 Patients | Dehradun News – Times of India. [Last accessed on 2020 Aug 14]. Available from: https://timesofindia.indiatimes.com/city/dehradun/uttarakhandallows-home-isolation-for-asymptomatic-covid-19-patients/articleshow/77466201.cms .
- 42.MoHFW | Home. [Last accessed on 2020 Jul 27]. Available from: https://www.mohfw.gov.in/
- 43.Goyal N, Gupta K. Letter to the Editor Regarding “COVID-19 Impact on Neurosurgical Practice: Lockdown Attitude and Experience of a European Academic Center.”. [Last accessed on 2020 Oct 29];World Neurosurg. 2020 144:e380–e388. doi: 10.1016/j.wneu.2020.08.168. Available from: http://www.sciencedirect.com/science/article/pii/S1878875020321252 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goyal N, Chaturvedi J, Chandra PP, Raheja A. Letter to the Editor Regarding “Neurosurgery Services in Dr. Sardjito General Hospital, Yogyakarta, Indonesia, During the COVID-19 Pandemic: Experience from a Developing Country”. World Neurosurg. 2021;146:415–6. doi: 10.1016/j.wneu.2020.10.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goyal N, Venkataram T, Dash C, Chandra PP. Letter to the editor regarding “COVID-19's impact on neurosurgical training in Southeast Asia”. World Neurosurg. 2021;146:424–426. doi: 10.1016/j.wneu.2020.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Goyal N, Chandra PP, Raheja A, Sardhara J. Letter to the editor regarding “early effects of COVID-19 pandemic on neurosurgical training in the United States: A case volume analysis of eight programs”. World Neurosurg. 2021;146:411–3. doi: 10.1016/j.wneu.2020.10.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goyal N, Chaturvedi J, Chandra PP, Raheja A. Letter to the editor regarding “early changes to neurosurgery resident training during the COVID-19 pandemic at a large united states academic medical center”. World Neurosurg. 2020;146:420–2. doi: 10.1016/j.wneu.2020.10.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goyal N, Swain SK, Sardhara J, Raheja A. Letter to the editor regarding “'staying home' – Early changes in patterns of neurotrauma in New York City during the COVID-19 pandemic”. World Neurosurg. 2021;146:407–9. doi: 10.1016/j.wneu.2020.10.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goyal N, Swain SK, Gupta K, Chaturvedi J, Arora RK, Sharma SK. “Locked up inside home” – Head injury patterns during coronavirus disease of 2019 pandemic. Surg Neurol Int. 2020;11:395. doi: 10.25259/SNI_675_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dash C, Venkataram T, Goyal N, Chaturvedi J, Raheja A, Singla R, et al. Neurosurgery training in India during the COVID-19 pandemic: Straight from the horse's mouth. Neurosurg Focus. 2020;49:E16. doi: 10.3171/2020.9.FOCUS20537. [DOI] [PubMed] [Google Scholar]
- 51.Goyal N, Chaturvedi J, Arora RK. Letter to the editor regarding “neurosurgical referral patterns during the COVID-19 pandemic: A United Kingdom experience”. World Neurosurg. 2021;145:555–6. doi: 10.1016/j.wneu.2020.09.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nepogodiev D, Bhangu A, Glasbey JC, Li E, Omar OM, Simoes JF, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Delhi Corona News: Delhi's Sero-Prevalence Study Finds 23.48 Per Cent People Affected by Covid-19 | Delhi News – Times of India. [Last accessed on 2020 Aug 10]. Available from: https://timesofindia.indiatimes.com/city/delhi/delhis-sero-prevalence-study-finds-23-48-per-cent-peopleaffected-by-covid-19/articleshow/77085162.cms .