Abstract
Background
Much of the literature about the costs of metastatic pancreatic cancer is focused on the Medicare population, but the cost in the commercially insured population is not well-documented. Differences in treatment patterns between commercially insured and Medicare patients with metastatic pancreatic cancer can provide insights into healthcare utilization and the total cost of care.
Objective
To compare the total cost of care for commercially insured versus Medicare patients with metastatic pancreatic cancer who are receiving National Comprehensive Cancer Network (NCCN)-recommended treatment regimens.
Methods
We identified 3904 patients (mean age at diagnosis, 56 years) with metastatic pancreatic cancer using International Classification of Diseases, Ninth/Tenth Revision diagnosis codes in claims data in the 2014–2018 MarketScan commercial database and 28,063 patients (mean age at diagnosis, 73 years) with metastatic pancreatic cancer in the 2014–2017 Medicare Parts A, B, and D 100% research identifiable data files. We calculated the total cost of care and resource utilization by NCCN-recommended (category 1) treatment regimen, including 5-fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFIRINOX); gemcitabine plus nab-paclitaxel; gemcitabine monotherapy; and liposomal irinotecan. All patients had ≥2 claims with a pancreatic cancer diagnosis more than 30 days apart and ≥1 subsequent claims with a secondary malignancy diagnosis for metastatic disease.
Results
The mean total cost of care was 186% higher in the commercially insured cohort than in the Medicare cohort. Excluding gemcitabine monotherapy, the total cost of care for patients with metastatic pancreatic cancer was similar between the regimens used in each cohort, ranging from $95,426 to $116,325 in the commercial insurance group and from $39,777 to $40,390 in the Medicare group. The components of hospital-based inpatient and outpatient costs varied between similar regimens in both cohorts. The inpatient admission patterns of patients' regimens were consistent across the 2 cohorts, with patients receiving gemcitabine monotherapy or liposomal irinotecan having the lowest overall number of admissions in each cohort.
Conclusions
The treatment patterns varied across the regimens but were largely consistent between the commercially insured and the Medicare patients who received the same regimen for metastatic pancreatic cancer; the ratio of total cost of care was 3:1 (commercially insured to Medicare). The total costs of care were similar across the regimens in each cohort, but the components of the total cost varied. These results can inform clinical guidelines and pathways for pancreatic cancer therapy as new evidence and treatment options emerge, and in the context of increasing value-based care models.
Keywords: commercial insurance, cost of care, healthcare resource utilization, Medicare, metastatic pancreatic cancer, NCCN-recommended regimens, pancreatic cancer pathways
KEY POINTS
-
▸
There is limited research comparing costs and resource utilization for patients with metastatic pancreatic cancer in Medicare versus patients with commercial insurance.
-
▸
This observational study compared the total cost of care and NCCN-recommended therapies for commercially insured and Medicare patients with metastatic pancreatic cancer.
-
▸
Patients received FOLFIRINOX, gemcitabine plus nab-paclitaxel, gemcitabine monotherapy, or liposomal irinotecan.
-
▸
The mean inpatient costs of patients with commercial insurance ($12,745–$20,247) were more than double those of patients with Medicare coverage ($5330–$9123) for all regimens.
-
▸
Commercially insured patients had 186% higher healthcare costs and lower mean hospital admission rates than Medicare patients.
-
▸
Excluding gemcitabine monotherapy, the total cost of care ranged from $95,426 to $116,325 for commercially insured patients versus $39,777 to $40,390 for Medicare patients.
-
▸
Patients who received gemcitabine monotherapy had the highest CCI scores and the oldest age at diagnosis of metastatic disease in both groups.
-
▸
These results can inform clinical guidelines and treatment pathways for pancreatic cancer as new therapies emerge and as value-based care models become more prevalent.
In 2020, the National Cancer Institute estimated that 57,600 adults in the United States would be diagnosed with pancreatic cancer.1 Pancreatic cancer currently accounts for 3.2% of US cancer diagnoses and results in 7.8% of cancer deaths.1 For 52% of patients with pancreatic cancer, the cancer has metastasized at the time of diagnosis.2 A previous study comparing the total cost of care among frequently used treatment regimens for metastatic pancreatic cancer indicated that there are differences in the inpatient and outpatient cost components.
An analysis of Medicare fee-for-service patients with metastatic pancreatic cancer showed that the mean total cost of care for first-line gemcitabine monotherapy was $20,462, which was lower than the $40,392 for first-line treatment with gemcitabine plus nab-paclitaxel or the $40,325 for first-line treatment with the combination of 5-fluorouracil (5-FU), leucovorin, oxaliplatin, and irinotecan (FOLFIRINOX).3
Patients who received second-line liposomal irinotecan had a higher mean total cost of care than patients who received third-line liposomal irinotecan ($41,600 vs $36,810, respectively), although the mean total cost of care was similar for first-line gemcitabine plus nab-paclitaxel and FOLFIRINOX.3 Existing research has not assessed the differences in costs of care between commercially insured and Medicare patient populations with metastatic prostate cancer.
This current observational study compared the mean total cost of care for commercially insured patients and for Medicare patients with metastatic pancreatic cancer who received US Food and Drug Administration (FDA)-approved, category 1 National Comprehensive Cancer Network (NCCN)-recommended chemotherapy regimens. The NCCN Clinical Practice Guidelines in Oncology are recognized as a standard of care for 97% of cancers, including pancreatic cancer.4,5 The FDA-approved category 1 NCCN-recommended treatment options for metastatic pancreatic adenocarcinoma include first-line FOLFIRINOX, first-line gemcitabine plus nab-paclitaxel, first-line gemcitabine monotherapy, and second-line 5-FU plus leucovorin and liposomal irinotecan.5 These recommendations are consistent with real-world treatment patterns seen in claims analyses of patients with metastatic pancreatic cancer.
Studies suggest a link between aggressive cancer treatments and overall survival.6–9 A meta-analysis of randomized clinical trials of gemcitabine-based therapies indicates that gemcitabine monotherapy is associated with lower overall survival and less toxicity than combination therapies in patients with metastatic pancreatic cancer.6 A study of patients with metastatic pancreatic cancer who received liposomal irinotecan after treatment with fluorouracil and a gemcitabine-based regimen showed a 2.2-month increase in survival if patients received liposomal irinotecan as a second-line therapy compared with the third-line setting or later.7 In another study of patients with metastatic pancreatic cancer who received first-line category 1 NCCN-recommended treatment regimens, the median overall survival from diagnosis was 9.4 months in patients who received first-line FOLFIRINOX; 6.6 months in patients who received first-line gemcitabine plus nab-paclitaxel; and 3.7 months in patients who received first-line gemcitabine monotherapy.8 In a similar study of patients with metastatic pancreatic cancer, those who received second- or third-line liposomal irinotecan had a median overall survival of 5.4 months and 4 months, respectively.9
In addition to cost and survival, outcome measures of healthcare utilization, including hospitalizations, readmissions, and emergency department visits, may influence the prescribing patterns of providers assuming risk in a value-based payment model, such as the Center for Medicare & Medicaid Innovation's Oncology Care Model (OCM) and its successor, the Oncology Care First (OCF) model. To curb the expenses associated with evolving cancer treatments, the Centers for Medicare & Medicaid Services (CMS) has developed episode-based models to incorporate high-value, high-quality oncology care.10
The OCF model was anticipated to begin in January 2021; however, because of the COVID-19 pandemic, the start date has been delayed indefinitely, while the OCM model continues into 2022.11,12 Like its predecessor the OCM, the OCF proposes a similar episode-based methodology to balance the total cost of care with appropriate quality metrics, such as rates of hospital admissions, readmissions, and emergency department visits.11
The 2 payment structures proposed by the OCF model include a monthly population payment based on a prospective lump-sum payment, and a performance-based payment, which measures the total cost of care for 6-month episodes of care. These payment structures will provide further incentives for the adoption of therapies that can demonstrate high value in addition to better outcomes.11
The primary objective of our analysis was to characterize the mean total cost of care for commercially insured and Medicare-covered patients with metastatic pancreatic cancer who received FDA-approved, NCCN category 1–recommended regimens (first-line gemcitabine plus nab-paclitaxel, first-line FOLFIRINOX, first-line gemcitabine monotherapy, or second-line 5-FU plus leucovorin and liposomal irinotecan). A secondary objective was to compare the treatment patterns and components of the total cost of care across the treatment regimens and patient cohorts.
Methods
We used administrative claims to evaluate payers' costs for commercially insured patients and for those with Medicare fee-for-service coverage. We used International Classification of Diseases, Ninth/Tenth Revision diagnosis codes (Appendix A, available at www.AHDBonline.com) in claims data in the 2014–2018 MarketScan commercial database and the CMS 2014–2017 Medicare 100% research identifiable data files.
MarketScan is an annual database comprised of geographically diverse, private-sector health data from approximately 100 payers, and includes more than 28 million commercially insured lives. The data include person-specific clinical healthcare utilization, expenditures, and enrollment across inpatient, outpatient, and prescription drug services from a selection of large employers, health plans, and governmental and public organizations.
The Medicare 100% research identifiable data files contain paid fee-for-service claims generated for all Medicare beneficiaries in the United States for Parts A, B, and D services. Information in the Medicare 100% research identifiable data files include diagnosis codes, procedure codes, site of service, and patient information, including age, eligibility status, and health maintenance organization enrollment. Appendix B (see www.AHDBonline.com) lists the study exclusions for Medicare and MarketScan data.
All study patients had at least 2 claims more than 30 days apart with a pancreatic cancer diagnosis and at least 1 claim with a secondary malignancy (ie, metastatic) diagnosis on or after the first pancreatic cancer diagnosis date. We defined the index date as the earliest metastatic pancreatic cancer diagnosis date and excluded patients with preindex malignancies that are not pancreatic cancer.
We excluded commercially insured patients who were not enrolled within the 3-month preindex or 1-month postindex period, and Medicare beneficiaries without enrollment in the 6-month preindex or 3-month (or until death, if earlier) postindex period. Because of variation in the monthly MarketScan enrollment, we have reduced the preindex period from 6 months to 3 months to preserve credible sample sizes for the commercially insured population.
The end date of a therapeutic regimen was defined as the day before a new chemotherapy began, 28 days after the last chemotherapy (if no new chemotherapy was recorded), or at death for the Medicare cohort (no reliable information was available for the commercial population). Appendix C (see www.AHDBonline.com) lists the chemotherapies and other related drugs included in this study.
The period from the start of the therapeutic regimen through the end date represents a line of therapy. Lines of therapy were assigned based on the order of therapies used: the first line of therapy was defined as the first occurrence of an eligible therapy initiated after or within the 14 days preceding the patient's index date, with the next line of therapy beginning on the day a patient switched to a new regimen. The end of the most recent line of therapy was defined as the earlier of 28 days after the most recent administration, visit date, or fill date for oral therapy (after the first date of chemotherapy), or the date of death. Liposomal irinotecan was most frequently used as a second-line or third-line therapy.
We calculated a Charlson Comorbidity Index (CCI) score for each regimen within every cohort. The CCI is a scale from 1 to 6, which weights patients' comorbidities to estimate the 10-year mortality risk.13 The mean admissions per line of therapy were defined as the mean number of admissions per patient receiving 1 line of therapy. The mean length of stay was calculated as the mean number of days for each admission. The readmission rates, surgery rates, and intensive care unit (ICU) utilization rates were calculated as the proportion of admissions with a readmission, surgery, or ICU utilization, respectively. Each measurement was calculated per regimen and per line of therapy.
Cost Measures
The mean total cost of care was calculated as the sum of a payer's inpatient, outpatient, or pharmacy costs incurred during a line of therapy, divided by the number of patients within that line of therapy. Each measurement was calculated separately for all patients in the cohort who received the same regimen and the same line of therapy. The costs reflect the paid amounts (ie, payer liabilities, not including patient cost-sharing) by line of therapy and do not consider drug manufacturers' rebates.
Statistical Testing
All statistical tests were performed using SAS version 9.2 (SAS Institute, Inc; Cary, NC). Confidence intervals (CIs) were calculated for each outcome measure by treatment regimen and by line of therapy. The results with outcome measures where at least one 95% CI did not overlap with those from the other 3 regimens or lines of therapy were selected for additional statistical testing. A GENMOD procedure with negative binomial distribution for count outcomes and a MIXED procedure for cost outcomes were used to determine if an outcome for one regimen was significantly different from the other regimens. These procedures were selected to account for repeated measurements for patients who may have received more than 1 regimen during different lines of therapy.
The regimen and line of therapy combinations within the cohorts often resulted in small cell sizes that produced wide CIs, which limited the testing significance of pair-wise comparisons. The results were considered significant if P ≤.05. The P values were reported for outcomes that were significantly different from other combinations of regimens or line of therapy.
Results
We identified 3904 patients with metastatic pancreatic cancer in the commercially insured population, with a mean age of 56 years at diagnosis, and 28,063 patients with metastatic pancreatic cancer in the Medicare population, with a mean age of 73 years at diagnosis. All patients received FOLFIRINOX, gemcitabine plus nab-paclitaxel, or gemcitabine monotherapy primarily as first-line regimens; liposomal irinotecan was the most often prescribed drug as a second- and third-line treatment for both patient populations.
Patients received multiple regimens more often in the commercially insured group than in the Medicare group, and patients in the commercially insured cohort were more likely to switch therapies earlier in their treatment process.
As expected, the patients in the commercially insured cohort were younger than those in the Medicare cohort; however, their CCI scores were higher, possibly indicating a higher risk profile. For the population with commercial insurance, the mean ages at diagnosis of metastatic pancreatic cancer were 55.4 years, 56.1 years, 56.6 years, and 55.3 years, and the CCI scores were 4, 4.1, 4.4, and 4.3 for patients who received first-line FOLFIRINOX, first-line gemcitabine plus nab-paclitaxel, first-line gemcitabine monotherapy, and second- or third-line therapy liposomal irinotecan, respectively.
For the Medicare population, the mean ages at the diagnosis of metastatic pancreatic cancer were 69.8 years, 72.5 years, 75 years, and 72.2 years, and the CCI scores were 3, 3.3, 3.6, and 3.3 for patients receiving first-line FOLFIRINOX, first-line gemcitabine plus nab-paclitaxel, first-line gemcitabine monotherapy, and second- or third-line liposomal irinotecan, respectively.
With any treatment regimen, patients with commercial insurance were diagnosed with pancreatic cancer at a mean 19.7-year younger age than patients with Medicare coverage (55.3 years vs 75 years, respectively).
The mean lengths of therapy by regimen in the commercially insured cohort were 165 days, 138 days, 133 days, and 97 days for patients receiving first-line FOLFIRINOX, first-line gemcitabine plus nab-paclitaxel, first-line gemcitabine monotherapy, and second- or third-line liposomal irinotecan, respectively. The mean lengths of therapy by regimen in the Medicare cohort were 156 days, 142 days, 128 days, and 104 days for first-line FOLFIRINOX, first-line gemcitabine plus nab-paclitaxel, first-line gemcitabine monotherapy, and second- or third-line liposomal irinotecan patients, respectively.
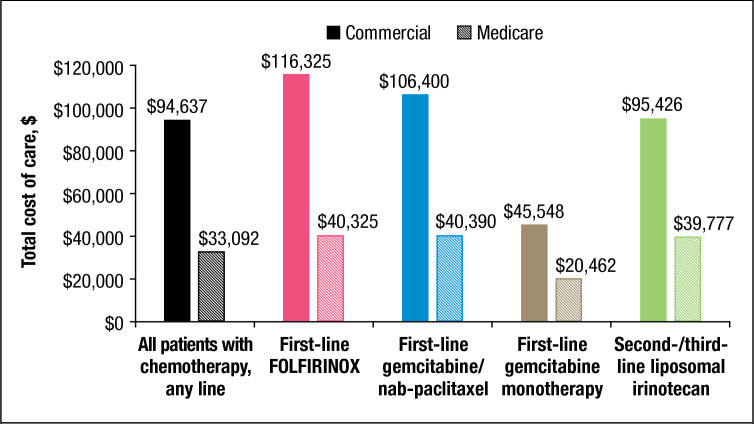
The mean total cost of care per line of therapy was 186% higher in the commercially insured cohort ($94,637) than in the Medicare cohort ($33,092; P <.05) for all chemotherapy regimens using any line of therapy, which resulted, in part, from the higher provider reimbursement rates of commercial payers (Figure 1).14
Figure 1. Mean Total Cost of Carea per Line of Therapy, by Regimen and Payer Cohort.
aMean total cost of care includes the service cost categories of inpatient facility, professional, chemotherapy (Part B and Part D claims for Medicare), chemotherapy-related procedures, antiemetic drugs, hematopoietic agents, other supportive drugs, outpatient facility, professional, skilled nursing facility/hospice/home health, surgery, and emergency department/observation costs.
FOLFIRINOX indicates 5-fluorouracil, leucovorin, oxaliplatin, and irinotecan.
Source: Pelech D. Congressional Budget Office. An analysis of private-sector prices for physician services. Presented at the Academy Health Annual Research Meeting. June 26, 2017.
The mean total cost of care for first-line gemcitabine monotherapy was lower than for any other therapy: $45,548 for commercially insured patients and $20,462 for Medicare patients (P <.001). The differences in the mean total cost of care for all other regimens in the commercially insured and Medicare populations were not statistically significant.
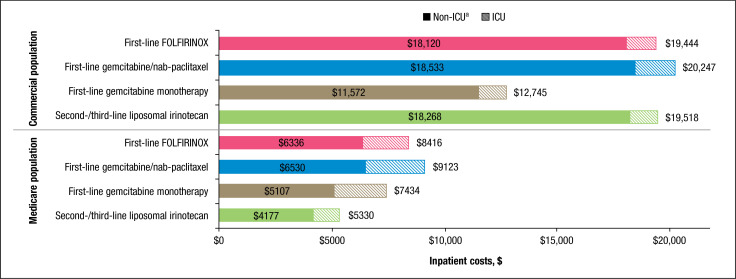
The mean inpatient costs per line of therapy in the commercially insured cohort ($12,745–$20,247) were more than twice the Medicare cohort's costs ($5330–$9123) for all regimens (P <.05; Figure 2). In the commercially insured cohort, the mean inpatient costs per line of therapy for first-line gemcitabine plus nab-paclitaxel, first-line FOLFIRINOX, and second- or third-line liposomal irinotecan were not significantly different (P >.05). Patients who received first-line gemcitabine monotherapy had lower mean inpatient costs ($12,745) than those who received first-line gemcitabine plus nab-paclitaxel ($20,247; P <.05) or first-line FOLFIRINOX ($19,444; P <.05), but the mean inpatient costs were not statistically significant compared with the patients who received second- or third-line liposomal irinotecan (P >.10).
Figure 2. Mean Inpatient Costs per Line of Therapy, by Regimen and Payer Cohort.
aNon-ICU includes inpatient facility, professional, and skilled nursing facility/hospice/home health costs.
FOLFIRINOX indicates 5-fluorouracil, leucovorin, oxaliplatin, and irinotecan; ICU, intensive care unit.
In the Medicare cohort, patients who received second- or third-line liposomal irinotecan had lower inpatient costs than patients who received all other regimens ($5330; P <.001). Patients who received second- or third-line liposomal irinotecan also had the lowest mean ICU costs in the Medicare cohort ($1153; P <.05).
Overall, the mean inpatient costs for commercially insured patients were from 71% to 266% higher than the costs for patients with Medicare coverage. Among the patients who received the same regimen, the mean hospital admissions per line of therapy were lower in the commercially insured patients than in the Medicare population (P <.05), with the exception of patients who received second- or third-line liposomal irinotecan (Table 1).
Table 1.
Mean Hospital Readmissions, Admissions with ICU, and Length of Stay
| Chemotherapy regimen | Mean admissions per line of therapy, N | Mean length of stay, days | Mean percent of total admissions | ||
|---|---|---|---|---|---|
| With readmissions, % | With ICU use, % | With surgery, % | |||
| Commercial analysis (MarketScan 2014–2018), N = 3904 | |||||
| First-line FOLFIRINOX | 0.70 | 5.96 | 23 | 21 | 16 |
| First-line gemcitabine/nab-paclitaxel | 0.78 | 6.01 | 24 | 22 | 13 |
| First-line gemcitabine monotherapy | 0.54 | 6.88 | 22 | 25 | 14 |
| Second-/third-line liposomal irinotecan | 0.60 | 6.90 | 17 | 21 | 5 |
| Medicare analysis (Medicare 100% research identifiable data 2014–2017), N = 16,065 | |||||
| First-line FOLFIRINOX | 0.85 | 6.79 | 16 | 23 | 17 |
| First-line gemcitabine/nab-paclitaxel | 0.95 | 6.62 | 21 | 25 | 11 |
| First-line gemcitabine monotherapy | 0.75 | 7.00 | 20 | 26 | 12 |
| Second-/third-line liposomal irinotecan | 0.61 | 6.79 | 17 | 21 | 8 |
FOLFIRINOX indicates 5-fluorouracil, leucovorin, oxaliplatin, and irinotecan; ICU, intensive care unit.
In the Medicare cohort, the patients who received first-line gemcitabine plus nab-paclitaxel had a higher mean number of admissions than patients who received any other regimen (0.95; P <.001). Patients receiving first-line gemcitabine monotherapy had the lowest mean number of admissions among the commercially insured cohort (0.54; P <.001).
Patients who received second- or third-line liposomal irinotecan had the lowest mean number of admissions among the Medicare beneficiaries (0.61; P <.001).
Patients who received first-line FOLFIRINOX or first-line gemcitabine plus nab-paclitaxel had a shorter length of hospital stay than patients who received first-line gemcitabine monotherapy (5.96, 6.01, and 6.88 days, respectively; P <.05) in the commercially insured cohort. Patients who received first-line gemcitabine plus nab-paclitaxel had a shorter length of hospital stay than the patients who received first-line gemcitabine monotherapy (6.62 vs 7 days, respectively; P <.001) in the Medicare cohort.
Medicare beneficiaries receiving first-line FOLFIRINOX had similar rates of readmissions to those who received second- or third-line liposomal irinotecan, and a lower mean number of readmissions than patients receiving gemcitabine-based regimens (P <.05). In the Medicare cohort, patients receiving first-line FOLFIRINOX had the highest mean rate of surgical admissions (17%; P <.001), and patients receiving second- or third-line liposomal irinotecan had the lowest rate of surgical admissions (8%; P <.05).
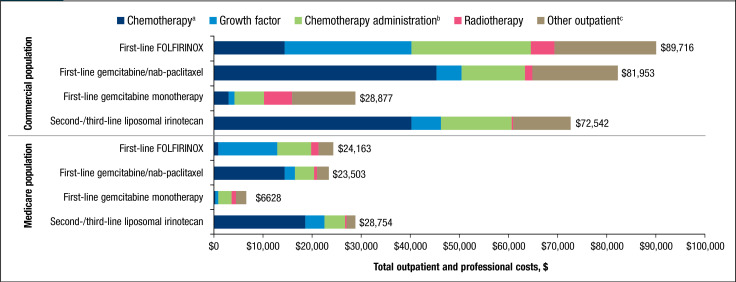
The mean outpatient costs per line of therapy were 152% to 336% higher in the commercially insured cohort ($28,877–$89,716) than in the Medicare cohort ($6628–$28,754; P <.05; Figure 3). For first-line gemcitabine monotherapy in both cohorts, the mean outpatient costs were lowest (commercially insured: $28,877, P <.001; Medicare: $6628, P <.001). The mean outpatient costs per line of therapy were highest for second- or third-line liposomal irinotecan ($28,754; P <.001) in the Medicare cohort. The differences in mean outpatient costs per line of therapy for all other regimens in the commercially insured and Medicare populations were not statistically significant.
Figure 3. Mean Outpatient and Professional Costs.
aChemotherapy costs for Medicare include Part B and Part D claims.
bContains chemotherapy-related procedures, antiemetic drugs, hematopoietic agents, and other supportive drugs.
cIncludes outpatient facility, professional, and skilled-nursing facility/hospice/home health, surgery, and emergency department/observation costs.
FOLFIRINOX indicates 5-fluorouracil, leucovorin, oxaliplatin, and irinotecan.
The mean outpatient cost ratios between the commercially insured and Medicare populations were approximately 15:1 for chemotherapy, 3:1 for growth factor, 4:1 for chemotherapy administration and associated drugs, and 6:1 for radiotherapy (Table 2).
Table 2.
Components of Mean Outpatient Costs
| Chemotherapy regimen | Chemotherapy,a $ | Growth factor, $ | Chemotherapy administration and supportive drugs,b $ | Radiotherapy, $ | Other outpatient costs,c $ |
|---|---|---|---|---|---|
| Commercial analysis (MarketScan 2014–2018), N = 3904 | |||||
| First-line FOLFIRINOX | 14,331 | 25,772 | 24,322 | 4888 | 20,404 |
| First-line gemcitabine/nab-paclitaxel | 45,256 | 5042 | 12,818 | 1597 | 17,238 |
| First-line gemcitabine monotherapy | 3043 | 1274 | 5906 | 5620 | 13,034 |
| Second-/third-line liposomal irinotecan | 40,180 | 5887 | 14,327 | 438 | 11,710 |
| Medicare analysis (Medicare 100% research identifiable data 2014–2017), N = 16,065 | |||||
| First-line FOLFIRINOX | 1022 | 11,964 | 6845 | 1502 | 2830 |
| First-line gemcitabine/nab-paclitaxel | 14,510 | 1971 | 3852 | 477 | 2693 |
| First-line gemcitabine monotherapy | 197 | 805 | 2481 | 916 | 2229 |
| Second-/third-line liposomal irinotecan | 18,635 | 3842 | 4227 | 308 | 1742 |
Chemotherapy costs for Medicare include Part B and Part D claims.
Contains chemotherapy-related procedures, antiemetic drugs, hematopoietic agents, and other supportive drugs.
Includes outpatient facility, professional, and skilled-nursing facility/hospice/home health, surgery, emergency department/observation costs.
FOLFIRINOX indicates 5-fluorouracil, leucovorin, oxaliplatin, and irinotecan.
Patients receiving first-line gemcitabine plus nab-paclitaxel or second- or third-line liposomal irinotecan had the highest mean chemotherapy costs in both cohorts: $45,256 and $40,180, respectively, for commercially insured patients; $14,510 and $18,635, respectively, for Medicare patients (P <.001).
Patients receiving first-line gemcitabine monotherapy had the lowest mean chemotherapy costs in both populations ($3043 for commercially insured patients, P ≤.001; $197 for Medicare patients, P <.05), and the lowest mean chemotherapy administration and supportive drug costs in the commercial insurance ($5906; P <.001) and Medicare ($2481; P <.001) cohorts.
Patients receiving first-line FOLFIRINOX had the highest mean growth factor costs in both study populations ($25,772 in commercially insured patients, P <.001; $11,964 in Medicare patients, P <.001) and also had higher mean chemotherapy administration and supporting drug costs in both populations ($24,322 in commercially insured patients, P <.001; $6845 in Medicare patients, P <.001).
Patients receiving first-line gemcitabine monotherapy had the lowest mean growth factor costs in both populations ($1274 in commercially insured patients, P <.05; $805 in Medicare patients, P <.001). For the commercial insurance cohort, second- or third-line liposomal irinotecan and first-line gemcitabine monotherapy had lower “other” outpatient (eg, outpatient facility, surgery, emergency department) costs than treatment with first-line gemcitabine plus nab-paclitaxel or with first-line FOLFIRINOX (P <.05). In the Medicare population, second- or third-line liposomal irinotecan had lower “other” outpatient costs than all of the other regimens (P <.05).
Discussion
These findings highlight the similarities in treatment patterns for frequently prescribed FDA-approved and NCCN category 1–recommended regimens within commercially insured and Medicare fee-for-service populations with metastatic pancreatic cancer, as well as stark differences in the mean costs between the 2 groups. In this analysis, the patients who received first-line gemcitabine monotherapy had the highest CCI score (commercially insured patients, 4.4; Medicare patients, 3.6) and the oldest age at metastatic diagnosis (commercially insured patients, 56.6 years; Medicare patients, 75 years) in both populations.
For patients receiving gemcitabine monotherapy, older age and comorbidities are demographic trends supported by other research.8,9 In a study of data from 2015 to 2019, patients with metastatic pancreatic cancer who were receiving first-line gemcitabine monotherapy were older at diagnosis and had higher Eastern Cooperative Oncology Group (ECOG) scores,8 which is a similar diagnosis tool to the CCI.15
In the same study, patients who received first-line gemcitabine monotherapy had a shorter treatment duration and a lower median overall survival than patients who received first-line FOLFIRINOX or first-line gemcitabine plus nab-paclitaxel.8
Although more common in the commercial insurance cohort, some patients in each cohort in this study received multiple regimens; further analysis is needed to determine if patients who received gemcitabine monotherapy had transitioned from other therapies.
In recent studies of patients with metastatic pancreatic cancer, the patients who received regimens with a higher mean total cost of care (ie, first-line FOLFIRINOX, first-line gemcitabine plus nab-paclitaxel, and second- or third-line liposomal irinotecan) had longer overall survival, whereas patients receiving first-line gemcitabine monotherapy, which accounted for approximately 50% of the mean total cost of care of the other regimens, had a 39% to 56% lower overall survival rate.8,9 Cost and survival, along with adverse events, are key components of value-based payment models that are gaining influence beyond Medicare's OCM.
Hospital resource utilization is an important component of value-based care models. In our analysis, commercially insured patients had generally lower mean admission rates (Table 1) than Medicare beneficiaries. In the Medicare cohort, first-line gemcitabine plus nab-paclitaxel had the highest mean admissions (0.95; P <.001), and patients receiving second- or third-line liposomal irinotecan had the lowest mean admissions (0.61; P <.05) of all regimens in the study. In addition, in the Medicare cohort, first-line FOLFIRINOX had the highest rate of surgical admissions (17%; P <.001), and patients receiving second- or third-line liposomal irinotecan had the lowest rate of surgical admissions (8%; P <.05).
In the Medicare cohort, patients who received first-line gemcitabine plus nab-paclitaxel had a shorter length of stay (6.62 days) than patients who received first-line gemcitabine monotherapy (7 days; P <.001).
In a similar study of commercially insured and Medicare patients with metastatic pancreatic cancer receiving category 1 NCCN-recommended regimens (ie, FOLFIRINOX, gemcitabine plus nab-paclitaxel, gemcitabine monotherapy, or liposomal irinotecan–based therapy), patients who received liposomal irinotecan in any line of therapy had the lowest mean admissions in the Medicare population (0.62) and was among the regimens with the lowest admission rate in the commercially insured population, along with gemcitabine monotherapy (0.56 and 0.54, respectively).16 In the same study, commercially insured and Medicare patients who received liposomal irinotecan in any line of therapy had the lowest rates of readmissions (commercially insured, 14%; Medicare, 16%) and the lowest rate of surgical admissions (commercially insured, 6%; Medicare, 7%) versus patients who received other regimens.16
There were stark differences in the mean treatment costs between patients with commercial insurance and those with Medicare coverage, which are likely a result of higher provider reimbursement rates in the commercial insurance market; the mean commercial insurance costs were 2 to 3 times higher than with Medicare coverage. In a review of 19 recent cost analyses, the Kaiser Family Foundation observed that commercial insurers paid an average of 199% of Medicare rates for all services; for outpatient services, the difference between commercial insurance and Medicare rates was even larger, at an average of 264%.17
This ratio is consistent with the findings of the Congressional Budget Office's analysis of overall physician reimbursement differences among commercial insurance and Medicare markets.14 However, our findings also indicated marked similarities in mean resource utilization for patients with metastatic pancreatic cancer who received the same chemotherapy regimen within the commercially insured and Medicare cohorts.
Limitations
This observational analysis was based on administrative claims data. The study has several limitations, because of the inherent restrictions of claims data. Patients in our study were not randomly assigned to each regimen. In addition, we were unable to adjust for individual dosing periods for regimens and did not include therapies administered before the metastatic pancreatic cancer diagnosis date.
Furthermore, because of the limited qualitative data in claims, we were not able to include quality-of-life measures. Because we were unable to track a patient's date of death in the MarketScan commercial claims files, we did not analyze survival in either cohort. Because the differences in emergency department utilization and emergency department costs were consistent, we decided to use emergency department costs in lieu of emergency department utilization.
The results have not been adjusted for differences in age, sex, CCI scores, or patient acuity. In addition, ECOG scores were not included in the data; thus, CCI scoring was used but was understood to not be as useful in describing the severity of illness in oncology.
Furthermore, this analysis does not consider other factors that may influence regimen performance, such as toxicity, tolerability, and side effects.
Because this analysis did not use health records data, we could not control for clinical covariates, nor were we able to determine cancer stage, although the studied regimens are indicated for metastatic pancreatic cancer. Patient characteristics and regimen performance may influence which regimens patients receive.
We also did not examine whether patients who received liposomal irinotecan also received concomitant 5-FU or previous gemcitabine-based therapy.
Also, later lines of therapy can be at a disadvantage when comparing the use of services and costs with earlier lines of therapy, particularly as a result of disease progression in patients with metastatic pancreatic cancer.
Commercial insurance claims data do not include reliable mortality information, and the Medicare and commercial insurance claims data do not include quality-of-life indicators. Although these data can be approximated with complex algorithms, this was not within the scope of our study.
Conclusions
Within each patient cohort, the mean treatment costs were similar among the therapeutic regimens, with the exception of first-line gemcitabine monotherapy. Previous studies show that patients who received first-line gemcitabine monotherapy had lower overall survival than patients who received FOLFIRINOX, gemcitabine plus nab-paclitaxel, or liposomal irinotecan–based therapy. The mean total cost of care was similar for patients who received second- or third-line liposomal irinotecan, and for those who received first-line gemcitabine plus nab-paclitaxel or first-line FOLFIRINOX, despite patients being more heavily pretreated and receiving treatment in a later line of therapy than patients who received treatment earlier in their disease.
The components of the mean treatment costs differed widely across the treatment regimens, with a difference observed between the commercially insured and Medicare cohorts. Healthcare resource utilization will have a greater impact on value-based care as public and private health plans increase their participation in alternative payment models. Considering these demographic and resource utilization differences can help inform clinical guidelines and pathways as they continue to evolve with new treatment options and emerging evidence, balancing costs, quality metrics, and overall survival.
Acknowledgments
The authors thank Jared Hirsch and Sujith Peta from Milliman for their research assistance.
Appendix
Funding Source
This study was funded by Ipsen Biopharmaceuticals.
Author Disclosure Statement
Ms Tomicki, Ms Latimer, and Ms Dieguez are employees of Milliman, which provided consulting services to Ipsen Biopharmaceuticals. Dr Cockrum is an employee of and owns stock in Ipsen. Dr Kim is a consultant to and serves on the Speaker's Bureau of Ipsen.
Contributor Information
Samantha Tomicki, Healthcare Analytics Consultant, Milliman, New York, NY.
Gabriela Dieguez, Principal & Consulting Actuary, Milliman, New York, NY.
Helen Latimer, Senior Healthcare Data Analyst, Milliman, New York, NY.
Paul Cockrum, Director, Oncology, Ipsen Medical–HEOR, Ipsen Biopharmaceuticals, Cambridge, MA.
George Kim, Chief, GI Cancer Section, Associate Professor, Medical Faculty Associates, George Washington University, Washington, DC.
References
- 1. National Cancer Institute SEER Program. Cancer stat facts: pancreatic cancer. https://seer.cancer.gov/statfacts/html/pancreas.html. Accessed March 11, 2020.
- 2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. [DOI] [PubMed] [Google Scholar]
- 3. Pelizzari P, Hirsch J, Cockrum P. Treatment patterns, survival rate, and total costs by line of therapy for FDA-approved/NCCN Category 1 treatments for Medicare patients with metastatic pancreatic cancer. J Manag Care Spec Pharm. 2019;25(10-a suppl):S26–S27. [Google Scholar]
- 4. National Comprehensive Cancer Network. About the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). www.nccn.org/professionals/#:~:text=The%20NCCN%20Guidelines%C2%AE%20are,patients%20in%20the%20United%20States. Accessed March 12, 2020.
- 5. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Pancreatic Adenocarcinoma Version 1.2020. October 23, 2020. www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf. Accessed March 12, 2020.
- 6. Ciliberto D, Botta C, Correale P, et al. Role of gemcitabine-based combination therapy in the management of advanced pancreatic cancer: a meta-analysis of randomised trials. Eur J Cancer. 2013;49:593–603. [DOI] [PubMed] [Google Scholar]
- 7. Kim GP, Surinach A, Corvino FA, Cockrum P. Impact of treatment sequence on overall survival in metastatic pancreatic cancer patients treated with liposomal irinotecan in the real-world setting. Value Health. 2019;22(suppl 2):S58. [Google Scholar]
- 8. Kim G, Cockrum P, Arndorfer S, Surinach A. Clinical pathway implications and real-world characteristics and outcomes for patients with metastatic pancreatic ductal adenocarcinoma (mPDAC) treated with first line category 1 National Comprehensive Cancer Network (NCCN) regimens. Ann Oncol. 2020;31(suppl 4):S881–S897. Abstract 1564P. [Google Scholar]
- 9. Kim GP, Cockrum P, Surinach A, Koeller JM. Real-world use of liposomal irinotecan-based regimens among patients (pts) with metastatic pancreatic adenocarcinoma (mPDAC) in the United States (U.S.). J Clin Oncol. 2020;38(15_suppl): Abstract e16740. [Google Scholar]
- 10. Kline RM, Muldoon LD, Schumacher HK, et al. Design challenges of an episode-based payment model in oncology: the Centers for Medicare & Medicaid Services Oncology Care Model. J Oncol Pract. 2017;13:e632–e645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Medicare & Medicaid Services. Oncology Care First Model: informal request for information. https://innovation.cms.gov/Files/x/ocf-informalrfi.pdf. Accessed March 12, 2020.
- 12. Centers for Medicare & Medicaid Services. CMS Innovation Center models COVID-19 related adjustments. June 3, 2020. www.cms.gov/files/document/covid-innovation-model-flexibilities.pdf. Accessed April 21, 2021.
- 13. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 14. Pelech D. Congressional Budget Office. An analysis of private-sector prices for physician services. Presented at the 115th Academy Health Annual Research Congress. New Orleans, LA; June 26, 2017. www.cbo.gov/system/files/115th-congress-2017-2018/presentation/52818-dp-presentation.pdf. Accessed May 15, 2020.
- 15. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655. [PubMed] [Google Scholar]
- 16. Tomicki S, Latimer H, Dieguez G, et al. Utilization of hospital inpatient services among patients with metastatic pancreatic cancer with commercial and Medicare insurance treated with FDA-Approved/NCCN Category 1 regimens. Poster presented at AMCP Nexus; October 19–23, 2020.
- 17. Lopez E, Neuman T, Jacobson G, Levitt L. How much more than Medicare do private insurers pay? A review of the literature. Issue brief. Kaiser Family Foundation; April 15, 2020. www.kff.org/medicare/issue-brief/how-much-more-than-medicare-do-private-insurers-pay-a-review-of-the-literature/. Accessed May 15, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.