Abstract
AIM
This study aimed to determine the effect of poststroke swallowing training and follow-up on swallowing function, nutritional status, and the development of problems associated with dysphagia.
METHOD
This study was designed as a single-group, pretest-posttest, quasi-experimental study and was conducted with 32 patients, who met the inclusion criteria for the study and were hospitalized with a diagnosis of acute stroke in the neurology clinic of a training and research hospital between June 2010 and September 2011. The patients were provided with swallowing training, followed up during meals, and given a training brochure. The Structured Information Form, the Standardized Mini Mental Test, the Barthel Index, and the Bedside Water Drinking Assessment Test were used to collect the data. Data were analyzed by the SPSS 16.0 program using descriptive and comparative statistical methods. TREND statement was followed for reporting.
RESULTS
It was determined that there was a statistically highly significant difference (p < .01) between the mean total score of the bedside water drinking assessment test after training compared with before the swallowing training, the duration of eating shortened (p < .01), and the amount of food consumed increased (p < .01) in the first follow-up. It was determined that the patients stayed in the hospital for an average of 9.75 ± 3.44 days; and aspiration occurred in 9.4% of them during this period. It was observed that patients who developed aspiration had prior lung problems.
CONCLUSION
It was observed that swallowing training decreased the duration of eating and increased the amount of food consumed in patients with stroke and resulting dysphagia. It was considered that the implementation of the training and the follow-up of swallowing function could be useful in preventing the development of problems.
Keywords: Dysphagia, stroke, swallowing training, swallowing follow-up
Introduction
Dysphagia is one of the common problems after a stroke (Bonilha et al., 2014; Boyraz, 2015; Çiyiltepe, 2004; Karaca Umay et al., 2010; Özdemir & Çekin 2011; Palli et al., 2017). Although the duration of the disease varies depending on factors such as the location and size of the lesion and the evaluation method used, the incidence of dysphagia after a stroke varies between 29%–81% (Huang et al., 2014; Smithard et al., 2007; Türkmen, 2005; Westergren, 2006). Paciaroni et al. (2004) evaluated 406 patients who were diagnosed with a stroke within the first 24 hours, and they observed that 34.7% of them developed dysphagia. Smithard et al. (2007) conducted a long-term follow-up in a sample of 1288 people who had a stroke for the first time, and they detected dysphagia in 567 (44%) patients in the initial evaluation.
Poststroke dysphagia is associated with decreased oral, pharyngeal, and esophageal functions, leads to social isolation in addition to serious problems resulting in airway obstruction, aspiration, aspiration pneumonia, dehydration, malnutrition, sepsis and death, affects the quality of life, and may cause a delay in rehabilitation and an increase in health spending (Huang et al., 2014; Karaca Umay et al., 2010; McFarlane et al., 2014; Mourao et al., 2016; Özdemir & Çekin, 2011; Türkmen, 2005; Westergren, 2006). For the treatment and rehabilitation of dysphagia, it is universally recommended to diagnose and continuously monitor the swallowing function in all the patients with a diagnosis of acute stroke within the first 24 hours by using validated, reliable, and sensitive bedside assessment tools (American Heart Association/American Stroke Association, 2013, Class; Level of evidence B) (Boyraz, 2015; Jauch et al., 2013; Kang et al., 2012), and it is emphasized that the nurse has an important role in swallowing training (Palli et al., 2017).
Different methods, direct and indirect methods, are used in the rehabilitation and training program of dysphagia. The aim of direct methods is to improve voluntary motor activities. It includes sensory stimulation of motor activity and speed with electrical, chemical, and thermal applications. The aim of indirect methods is to increase swallowing safety and prevent aspiration into the respiratory tract without correcting the underlying neuromuscular insufficiency by providing compensation with individualized interventions. Indirect methods that are also applied by nurses include postural arrangements (chin-to-chest, chin tuck posture, tilting the head backward, turning the head to the strong/weak side), diet modification (viscous liquids, homogenized semi-solid foods), and compensatory maneuvers (supraglottic swallowing technique, super-supraglottic swallowing technique, Mendelsohn maneuver, and hard swallowing) (Arsava et al., 2018; McCullough et al., 2012; Perry, 2001; Vural et al., 2004).
Ensuring and maintaining safe nutrition will help prevent the development of problems owing to swallowing difficulties as well as reducing the duration of the patient’s hospital stay and contributing to an increase in life expectancy and quality of life (Perry, 2001; Selçuk, 2006). In their study, Elfetoh and Karaly (2018) concluded that the swallowing training program given to stroke patients with dysphagia was effective in improving swallowing. A study by Lin et al. (2003) determined that swallowing training in stroke patients with dysphagia increased the amount of food consumed and that there was a significant increase in arm circumference and body weight of these patients. However, in our country, no study has been found in which the swallowing function was evaluated in patients with stroke and swallowing training given to the patient and the person who would care for the patient and the results were evaluated. Therefore, this study aimed to determine the effect of poststroke swallowing training and follow-up on swallowing function, nutritional status, and the development of problems associated with dysphagia.
The following hypotheses (H) were tested in the study:
H1: Swallowing training and follow-up in stroke patients with dysphagia strengthens the patient’s swallowing function.
H2: Swallowing training and follow-up in stroke patients with dysphagia shorten the duration of eating.
H3: Swallowing training and follow-up in stroke patients with dysphagia increase the amount of food consumed.
H4: Swallowing training and follow-up in stroke patients with dysphagia prevents the development of problems associated with dysphagia.
Method
Study Design
This study was conducted as a single-group, pretest-posttest, quasi-experimental study.
Sample
A total of 180 patients diagnosed with acute stroke and hospitalized in the neurology clinic of a training and research hospital between June 2010 and September 2011 constituted the population of the study. Among these patients, 37 patients who developed dysphagia within the first 24–48 hours and met the inclusion criteria for the study constituted the sample of the study. However, 5 patients were excluded from the study because of changes in the patients’ clinical and cognitive condition after 48 hours. Thus, the study was conducted with a total of 32 patients. TREND statement was followed for reporting. Figure 1 illustrates the inclusion process in a flow chart.
Figure 1.
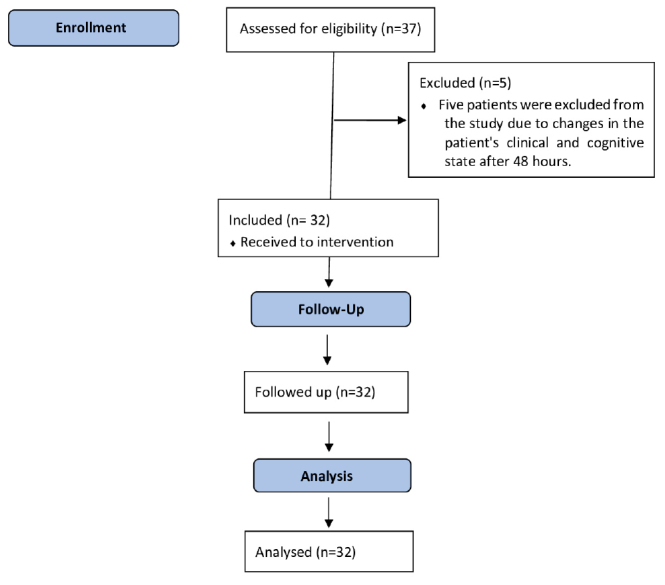
Flow Diagram of the Study (TREND Statement)
Inclusion criteria
Patients with a standardized mini mental test (SMMT) score ≥24, having the first assessment of swallowing function within 24–48 hours, having voluntary coughing, being able to swallow secretions, having symmetrical facial movements, having a bedside water drinking assessment test score ≥3, and who were willing and volunteered to participate in the study were included.
Data Collection Tools
The data of the study were collected using SMMT, structured information form, Barthel Index, and bedside water drinking assessment test. A training brochure was given to the patient/family/caregiver. The scores of the SMMT and bedside water drinking assessment test, which were among the data collection tools, were also used as inclusion criteria for the study.
Standardized Mini Mental Test
The SMMT, which was developed by Folstein et al. in 1975, is a short, useful, and standardized method that can be used to evaluate the cognitive level globally. It includes 11 items and 5 sub-dimensions, namely orientation (10 points), record memory (3 points), attention and calculation (5 points), recall (3 points), and language (9 points), and is evaluated over a total of 30 points. The scores between 24 and 30 indicate normal cognitive level, 21–23 indicate mild cognitive impairment, and ≤20 indicate moderate and severe cognitive impairment (Folstein et al., 1975; Güngen et al., 2002). Although the SMMT was adapted to the Turkish society for literate individuals by Güngen et al. in 2002, its adaptation to the Turkish society for illiterate individuals was performed by Ertan et al. in 1999. Patients with a score of ≥24 from the SMMT were included in the study.
Structured Information Form
This form was developed after reviewing the literature and included 3 parts. The first part of the form included individual (age, sex, and educational status) and disease-related characteristics of the patient (diagnosis and total length of stay in the hospital), the second part included the variables affecting nutrition and swallowing function (the Barthel Index and bedside water drinking assessment test to determine nutrition and swallowing function and the variables affecting them), and the third part included observational data during swallowing training and nutrition (the amount of food consumed and duration of eating, the development of problems associated with dysphagia, and so on) and the data obtained by measurements (body mass index, body temperature follow-up, sodium in blood, blood urea nitrogen [BUN] and albumin values). The third part of the information form allowed recording of repeated measurement data for each patient.
Dehydration and malnutrition are among the common poststroke complications owing to dysphagia. On the basis of literature review, this study evaluated sodium and BUN values in the blood as an indicator of hydration status of the patients (Crary et al., 2013), and the BMI and serum albumin levels as an indicator of nutritional status (Boyraz, 2015; Horasan, 2012).
Barthel Index
The sensitivity of the 10-item index, which was developed by Mahoney and Barthel in 1965 to measure the level of disability experienced during life activities, was modified and increased by Shah et al. in 1989. This index, adapted for the Turkish society by Küçükdeveci et al. in 2000, was demonstrated to be valid and reliable for groups of patients with stroke and spinal cord injury. The index includes 10 subheadings; eating, bathing, self-care, dressing, bladder and bowel control, toilet use, chair/bed transfer, mobility, and staircase use. The total score ranges from 0 to 100, where 0 indicates full dependence and 100 indicates full independence. The Cronbach’s alpha internal consistency coefficient for stroke patients was found to be 0.93 (Küçükdeveci et al., 2000; Shah et al., 1989). In this study, the Cronbach’s alpha internal consistency coefficient of the scale was found to be 0.83 in the first follow-up and 0.89 in the second and third follow-ups. In this study, the Barthel Index was used to evaluate the physical dependence of patients in their life activities during follow-up.
Bedside Water Drinking Assessment Test
It is a commonly used method to evaluate the swallowing function by giving patients small amounts of water (Arsava et al., 2018; Osawa et al., 2013). Patients with a score of 0–2 are believed to have normal swallowing function, whereas those with a score of 3–6 have dysphagia (Türkmen, 2005). In other studies, it was observed that the evaluation of this test together with oxygen saturation led to more precise results (Smith et al., 2000; Tippett, 2011; Türkmen, 2005). Therefore, in our study, the bedside water drinking assessment test was performed along with pulse oximetry. The patient was seated in an upright position and asked to drink 10 mL of water from a plastic glass without using a pipette and without pausing (those who coughed or seemed to choke and those whose voice quality changed after drinking were considered unsuccessful in the water swallowing test). During this time and for the next 10 minutes, arterial O2 saturation was evaluated from the unaffected arm and the second (index) finger with a battery-operated console type pulse oximeter. Pulse oximetry is an easy and fast non-invasive method, which is reliable in determining aspiration (Tippett, 2011). In this study, the bedside water drinking assessment test was performed along with pulse oximetry to evaluate the swallowing function of the patients during follow-up.
Training brochure
The training brochure was prepared using evidence-based practice guidelines (American Heart Association/American Stroke Association, 2013, Class I; Evidence Level B) (Jauch et al., 2013), meta-analysis studies (Hines et al., 2010; Westergren, 2006), and reviewing literature (Akın & Durna 2016; Çiyiltepe, 2004; Gulanick & Myers, 2007; Horasan, 2012; Özdemir & Çekin, 2011; Potter & Perry, 2008; Vural et al., 2004). This brochure included information on the issues related to swallowing and nutrition that should be considered before, during, and after nutrition to ensure and maintain safe nutrition. In this study used the training brochure to ensure and maintain safe nutrition of patients with stroke whose swallowing function was affected.
Data Collection
The study was conducted in 3 follow-ups. The first follow-up was performed at patient admission, the second at discharge, and the third at the first clinical control in the hospital 30–45 days after discharge. The applications in the first and second follow-ups were maintained until the patients were discharged.
The first part of SMMT, the structured information form, the bedside water drinking assessment test, the second part of the form, and Barthel Index were applied at patient admission (within the first 24–48 hours after stroke diagnosis) to obtain basic data from the patients who met the inclusion criteria for the study. Body temperature and anthropometric measurements (BMI) were performed, information in the patient file (sodium, BUN, and albumin value in blood and chest radiography report) such as laboratory and radiology test results performed upon the physician’s request were recorded in the third part of the information form (n = 37) (first follow-up). The measurements and evaluations, except for the first part of the SMMT and the structured information form, including individual characteristics and disease characteristics, were repeated during the patient’s discharge and at the first check-up in the hospital approximately 30–45 days after discharge (second and third follow-ups).
Swallowing training and follow-up were performed in accordance with the information included in the training brochure. When deciding on the method to be used in the swallowing training, a physiotherapist was used when necessary; and chin-to-chest, supraglottic swallowing, and Mendelsohn maneuvers were used.
Chin-to-chest is the process of swallowing with the head tilted forward and the patient’s chin resting on the chest. Aspiration is less likely to occur when the head is slightly tilted forward. Supraglottic swallowing refers to taking food inside the mouth and chewing it, taking a deep breath before swallowing and holding it, passing the bite to the pharynx as a whole by pushing the head back slightly at the same time, and swallowing the bite while keeping the breath. The patient coughs immediately after swallowing and before breathing again. Thus, the bite passes through the pharynx without any problem. Voluntarily extending the time to keep the airway closed before and during swallowing is a technique to protect the airway and prevent aspiration. Mendelsohn maneuver is a swallowing technique used to improve the cricopharyngeal opening width and opening time during swallowing. The patient is asked to swallow and hold the larynx for 2–3 seconds after swallowing and then swallow again (Boyraz, 2015; Çiyiltepe, 2004; Vural et al., 2004).
In patients who were functionally dependent in maintaining their life activities, families/caregivers were included in the training. The swallowing training, which continued until the patient was discharged, was performed and repeated by the researcher in cases where the family members/caregivers involved in the care changed. In the first 2 meals, the act of swallowing was guided by the researcher and observed by the patient and family/caregiver. During the next meals, the patient and family/caregiver managed swallowing and nutrition, and the researcher participated as an observer. The researcher intervened when necessary, repeated the swallowing training at required stages, and supported the maintenance of safe nutrition.
Swallowing Training
Patients who used glasses, hearing aids, and dentures were fitted with them before nutrition.
Clothes tightening the neck, torso, and abdomen were loosened if any.
The patients were provided with oral care to prevent aspiration pneumonia and to stimulate the flow of saliva and the sense of taste before nutrition.
In accordance with the physician’s recommendation, a diet consisting of viscous liquids and homogenized semi-solid food was prepared for bolus control by collaborating with the dietician and the patient’s family/caregiver.
A suitable body and head position was provided for safe swallowing. The head of the patients fed in the sitting position was raised to 90 degrees, and the head of the patients fed in the lying position was raised to 60 degrees. The weak parts of the body, the hips, and back were supported by pillows.
The chin-to-chest, supraglottic swallowing, and Mendelsohn maneuver were used to ensure safe swallowing.
During nutrition, the patient was warned not to speak when eating. The spoon used was held above mouth level, and touching the teeth or placing the food far behind the mouth was avoided. Only 1 teaspoon of homogenized semi-solid food or 10–15 mL of viscous liquid food was given at a time. The amount was increased once the patients managed to swallow this amount successfully. Before each spoon, the patient was encouraged to swallow through verbal guidance (Take the food in your mouth. Keep the food in your mouth. Close your lips. Lift your tongue to your palate. Think about your swallowing. Close your mouth and swallow. Swallow again. Cough to clear the airway). The patient was observed in terms of delayed cough, change in voice quality, and change in lung sounds during nutrition. If any of them were present, the physician was informed, and the nutrition was interrupted or stopped.
Sufficient time was allocated for nutrition. A patient-specific nutrition plan was prepared with small meals, 6 meals a day.
The increased amount of food was measured with a 50 cc glass tip feeding injector. The amount of food given to the patients at 1 meal included 300 mL of viscous liquid food. The amount of food was increased when swallowing function started to improve at the end of a week.
Patient responses during feeding, the amount of food consumed, and the duration of eating were recorded.
After nutrition, whether there was any food left in the patient’s mouth was checked, oral care was provided, and the patient was seated in an upright position for approximately 30–45 minutes.
Daily excretion efficiency and dryness of the skin were monitored, and BMI was calculated by weight monitoring. The body weight of the patients was followed up every day at the same time, with the same clothes, using a scale with a sensitivity of 100 g and the maximum measuring capacity of 150 kg. Body temperature was measured with a tympanic thermometer twice a day until discharge. The patients with a body temperature above 37.5°C were evaluated for lung infection. Chest radiography was evaluated in terms of lung infection once in patients with normal body temperature and twice in patients with a body temperature above 37.5°C. The results of the chest radiography and laboratory tests (sodium, BUN, albumin) from files were evaluated by the patient’s physician and recorded in the third part of the structured information form.
Statistical Analysis
The data were analyzed using descriptive (arithmetic mean, median, minimum-maximum, percentage values) and comparative (repeated measures test, Bonferroni test, Friedman test, Wilcoxon signed ranks test, and Yates’ continuity correction test) statistical methods with the Statistical Package for Social Sciences version 16.0 program (SPSS Inc.; Chicago, IL, USA).
Ethical Considerations
The ethical compliance of the study was approved by the İstanbul University-Cerrahpaşa Medical Faculty Clinical Research Ethics Committee (date and number: 10.11.2009/B-015). Written institutional permission (date and number: 26.01.2010/4344743-326) was obtained. The written informed consents were obtained from the patients voluntarily after explaining the aim and duration of the study to them.
Results
The age of the patients included in the study varied between 46 and 80 years, the mean age was 66.28 ± 9.73 years, 56.3% of them were women, 62.5% of them were literate or primary school graduates, 59.4% of them were married, and 78.1% of them were living with their spouses and children. It was determined that SMMT scores of the patients varied between 24 and 28 and that the mean score was 25.19 ± 1.35 (Table 1).
Table 1.
Distribution of Patients’ Individual and Disease Characteristics (n = 32)
| Variables | Min–Max | Mean ± SD | |
|---|---|---|---|
| Age (y) | 46–80 | 66.28 ± 9.73 | |
| n | % | ||
|
| |||
| Sex | Female | 18 | 56.3 |
| Male | 14 | 43.7 | |
| Educational status | Literate and primary school | 20 | 62.5 |
| Secondary and high school | 12 | 37.5 | |
| People living with | Alone | 7 | 21.9 |
| Spouse and children | 25 | 78.1 | |
| Diagnosis | Acute ischemic stroke | 30 | 93.7 |
| Hemorrhagic stroke | 2 | 6.3 | |
|
| |||
| Min–Max Mean ± SD Median | |||
|
| |||
| Standardized Mini Mental Test score | 24–28 | 25.19 ± 1.35 25 | |
| Total length of stay in the hospital (d) | 5–21 | 9.75 ± 3.44 | |
Note. Min = minimum; Max = maximum; SD= standard deviation.
When the distribution of disease characteristics of the patients was examined, it was observed that 93.7% of them were diagnosed with acute ischemic stroke, and 21.9% of them had previous lung problems. It was determined that the patients’ length of stay in the hospital varied between 5 and 21 days and that the patients were hospitalized for an average of 9.75 ± 3.44 days (Table 1).
When the mean total score of the Barthel Index, which was applied to determine the physical dependence of patients, was examined; it was determined that the level of physical dependence, which was mostly observed in the first follow-up, decreased in the second follow-up (p < .01) and further decreased in the third follow-up (p < .01), and that their independence increased. This difference was found to be statistically highly significant (p < .01, Table 2). When the dependence related to the nutrition dimension of the Barthel Index was examined, it was found that 43.8% of the patients in the first and second follow-ups and 31.3% of them in the third follow-up were functionally dependent, which was also found to be statistically significant (p < .05, Table 2).
Table 2.
Physical Dependence and Dependence on Nutritional Activity of the Patients during Follow-ups (n = 32)
| Barthel Index Total Score Mean ± SD (median) | ap | bPost-Hoc | |
|---|---|---|---|
| First follow-up | 42.50 ± 18.27 (50.0) | .001** | p = .001**,1–2 |
| p = .001**,1–3 | |||
| p = .001**,2–3 | |||
| Second follow-up | 48.44 ± 18.94 (52.5) | ||
| Third follow-up | 56.25 ± 18.58 (60.0) | ||
|
| |||
| Barthel Index Nutrition Dimension | Functionally Dependent, n (%) | Independent, n (%) | p |
|
| |||
| First follow-up | 14 (43.8) | 18 (56.3) | .018* |
| Second follow-up | 14 (43.8) | 18 (56.3) | |
| Third follow-up | 10 (31.3) | 22 (68.8) | |
Note.
Friedman test;
Wilcoxon signed ranks test.
p = indicates statistical significance.
p < .01 Cochran test
p < .05.
SD = Standard deviation.
When the mean score of the bedside water drinking assessment test, which was performed to evaluate the swallowing function of the patients, was examined; it was observed that dysphagia, which was high in the first follow-up, decreased but continued in the second follow-up, and that the swallowing function almost returned to normal in the third follow-up, and this difference was found to be statistically highly significant (p < 0.01) (Table 3).
Table 3.
Swallowing Function of Patients during Follow-ups
| Bedside Water Drinking Assessment Test | ap | bPost-Hoc | ||
|---|---|---|---|---|
|
| ||||
| Mean ± SD | Median | |||
| First follow-up | 3.59 ± 0.71 | 3.00 | .001** | p = .001**,1–2 |
| Second follow-up | 2.50 ± 0.92 | 2.00 | p = .001**,1–3 | |
| Third follow-up | 1.12 ± 0.66 | 1.00 | p = .001**,2–3 | |
Note.
Friedman test,
Wilcoxon signed ranks test.
p = indicates statistical significance.
p < .01.
SD = Standard deviation.
It was determined that each of the patients included in the study received swallowing training at an average of 19.50 ± 6.89 meals according to the needs of the patient/family/caregiver until discharge, in addition to the swallowing training given for the first 2 meals. It was ensured that the family/caregiver participated in all the trainings along with the patient (Table 4).
Table 4.
Distribution of Patients’ Characteristics Related to Swallowing Training and Nutrition Status
| Variables | n | % | |
|---|---|---|---|
| Provided with Training | Patient | — | — |
| Patient and family/caregiver | 32 | 100 | |
|
| |||
| Min–Max | Mean ± SD | ||
|
| |||
| Number of Swallowing Trainings | 10–42 | 19.50 ± 6.89 | |
|
| |||
| Duration of Eating (Min) | |||
|
|
|||
| Min–Max | Mean ± SD | p | |
|
| |||
| First follow-up | 10–28 | 16.43 ± 4.88 | .001** |
| Second follow-up | 8–20 | 11.65 ± 3.99 | |
|
| |||
| Amount of Food Consumed (mL) | |||
|
|
|||
| Min–Max | Mean ± SD | ||
|
| |||
| First follow-up | 140–280 | 229.06 ± 40.43 | .001** |
| Second follow-up | 160–350 | 285.93 ± 56.16 | |
Note. p = indicates statistical significance.
p < .01, paired samples test.
Min = Minimum; Max = Maximum; SD = Standard deviation.
When the results of swallowing training and nutrition observed during the meals during the hospitalization of the patients were examined, it was observed that the mean duration of eating decreased by 4.78 minutes in the second follow-up compared with the first follow-up, and that the mean amount of food consumed increased by 56.87 mL in the second follow-up compared with the first follow-up. This difference was found to be statistically significant (p < .01) (Table 4).
When sodium, BUN, albumin, and BMI values analyzed to monitor dehydration and malnutrition in patients were examined, it was determined that after the first follow-up, sodium and BUN values gradually increased; however, albumin and BMI values decreased. These differences in repeated measurement results were also found to be statistically significant (p < .05, Table 5).
Table 5.
Distribution of Patients’ Anthropometric Measurements and Laboratory Values (n = 32)
| Sodium Value in Blood | ap | bPost-Hoc | |
|---|---|---|---|
|
| |||
| Mean ± SD | |||
| First follow-up1 | 138.50 ± 1.70 | .001** | p = .507,1–2 |
| Second follow-up2 | 138.81 ± 1.75 | p = .001**,1–3 | |
| Third follow-up3 | 139.69 ± 1.89 | p = .001**,2–3 | |
| BUN Value in Blood | |||
| Mean ± SD | ap | bPost-Hoc | |
| First follow-up1 | 12.60 ± 2.97 | .017* | p = .023*,1–2 |
| Second follow-up2 | 12.99 ± 3.02 | p = .046*,1–3 | |
| Third follow-up3 | 13.03 ± 2.87 | p = 1.000,2–3 | |
| Albumin Value in Blood | |||
| Mean ± SD | ap | bPost-Hoc | |
| First follow-up1 | 4.34 ± .44 | .001** | p = .001**,1–2 |
| Second follow-up2 | 4.13 ± .36 | p = .004**,1–3 | |
| Third follow-up3 | 4.10 ± .32 | p = 1.000,2–3 | |
| BMI | |||
| Mean ± SD | ap | bPost-Hoc | |
| First follow-up1 | 25.36 ± .64 | p = .001**,1–2 | |
| Second follow-up2 | 25.12 ± .65 | .001** | p = .001**,1–3 |
| Third follow-up3 | 24.88 ± .71 | p = .007**,2–3 |
Note.
Repeated measures test (analysis of variance in repeated measures),
Bonferroni test.
p = indicates statistical significance.
p < .01,
p < .05.
BUN = blood urea nitrogen; BMI = Body mass index; SD = Standard deviation.
During the hospitalization period of the patients, it was determined that mean body temperature values did not differ significantly between morning and evening measurements (p < .01), body temperatures were within normal limits, and aspiration developed in 9.4% of the patients. When the patients who developed aspiration were examined, it was observed that these patients had previous lung problems. In the third follow-up examination during the post-discharge control, it was observed that none of the patients experienced signs and symptoms of aspiration during the meals (Table 6).
Table 6.
Patients’ Body Temperature Measurements and Problem Development Related to Dysphagia
| Variables | Body Temperature (°C) | p | ||
|---|---|---|---|---|
|
| ||||
| Min–Max | Mean ± SD | |||
| Body temperature | Morning | 36.4–37.2 | 36.57 ± 0.04 | .001** |
| Evening | 36.7–37.7 | 37.03 ± 0.07 | ||
| n | % | |||
|
| ||||
| Problems | Aspiration | 3 | 9.4 | |
| No problem occurred | 29 | 90.6 | ||
Note. p = indicates statistical significance.
p < .01, paired samples test.
Min = Minimum; Max = Maximum; SD = Standard deviation.
Discussion
In patients with stroke, it is universally recommended to evaluate and monitor the swallowing function within the first 24 hours after admission (McFarlane et al., 2014; Perry, 2001). For swallowing problems that do not resolve spontaneously in the first few weeks after stroke, planning and implementation of individualized care including early measures with a multidisciplinary approach can prevent/minimize the development of problems (McFarlane et al., 2014; Perry, 2001; Selçuk, 2006). Palli et al. (2017) have found that the monitoring of swallowing in patients with stroke reduced the rate of pneumonia associated with aspiration and the length of stay in the hospital.
Accordingly, within the scope of the study conducted to determine the effect of poststroke swallowing training and follow-up on swallowing function, nutritional status, and the development of problems associated with dysphagia, when the individual characteristics of the patients were examined, it was observed that they were in parallel with the studies conducted on patients with stroke and the literature data (Benbir & İnce, 2013; Boyraz, 2015; Crary et al., 2014; Smithard et al., 2007; Türkmen, 2005).
The mean SMMT score of the patients included in the study was 25.19 ± 1.35 (Table 1). This result, which was included among the inclusion criteria for the study, revealed that the cognitive level of the patients was adequate in terms of perception and implementation of the swallowing training to be provided.
The diagnosis was acute ischemic stroke in 90.6% of the patients (Table 1). This result was found to be consistent with the literature data and study results emphasizing that ischemic strokes constitute 89% of all strokes and that hemorrhagic strokes are observed less frequently (Boyraz, 2015; Mourao et al., 2016). The patients’ length of stay in the hospital varied between 5 and 20 days, and they were hospitalized for an average of 9.75 ± 3.44 days (Table 1). In the study conducted by Demirci Şahin et al. (2015), it was determined that the median hospital stay of the patients with stroke varied between from 8 and 11 days. This result supported the result of the above study.
The patients’ levels of physical dependence decreased in repeated measurements, and the difference between the measurements was significant (p < .01) (Table 2). The deficiencies in motor, sensory, and cognitive functions in the poststroke period cause dependence in patients and prevent them from performing life activities. Although the improvement in physical functions depends on the intensity of the motor deficit that develops at the beginning of the stroke, it progresses most rapidly within the first 3 months, the recovery rate slows down within 6 months, and the patient’s condition may continue (Öztürk et al., 2014). Considering the period between the patients’ total length of stay in the hospital (5–21 days) and the first clinical control (approximately 30–45 days after discharge), it was observed that the results of the study were consistent with the literature data.
In this study, found that the swallowing functions of the patients gradually improved in repeated measurements and that the difference between the measurements was significant (p < .01) (Table 3). In the literature, it was reported that dysphagia was observed in approximately 29%–81% of patients with stroke (Huang et al., 2014), 70% of them were able to recover at the end of the first week; however, dysphagia continued for a long time (>6 months) in 11%–19% of them (Boyraz, 2015). Considering that the mean total hospital stay of the patients participating in the study was 9.75 ± 3.44 days, the fact that the incidence of dysphagia in the second follow-up was 37.5%, and this rate decreased in the third follow-up was found to be consistent with the literature data. As members of the healthcare team, nurses play a key role in diagnosing, evaluating, and managing dysphagia and preventing the development of problems associated with it. A study by Tülek et al. (2018) on the current practices in the nursing care of patients with stroke in 11 European countries (Sweden, Belgium, Denmark, England, Norway, Turkey, Malta, the Netherlands, Switzerland, Iceland, and Serbia) in which a total of 92 nurses participated, indicated that 75 nurses performed bedside swallowing assessment alone or together with other healthcare team members within the first 24 hours.
Each patient included in the study was accompanied at meals from the time of admission until discharge, and they received an average of 19.50 ± 6.89 swallowing and nutrition training according to need. The patient and family/caregiver participated in all trainings (Table 4). There is limited scientific evidence demonstrating the positive effects of improving the nutritional status and providing appropriate energy intake on clinical improvement in patients with stroke and resulting dysphagia (Arsava, 2018; Nii et al., 2016). Nevertheless, considering the negative effects of malnutrition on prognosis in patients with stroke, it becomes necessary to reach protein and calorie targets as early as possible (Arsava et al., 2018). In the literature review, although the importance of guiding the swallowing action of the patient with verbal warnings is emphasized to ensure safe swallowing and nutrition during the meals in patients with dysphagia (Werner, 2005), there was no study evaluating this practice.
It was observed that the mean duration of eating decreased by 4.78 minutes, and the mean amount of food consumed increased by 56.87 mL in the second follow-up compared with the first follow-up. This difference was found to be statistically significant (p < .01) (Table 4). During the 3 follow-ups, although a gradual improvement was observed in swallowing function, the fact that the functional dependence of the patients during their hospital stay did not change (Table 2); and therefore, the affected extremity functions remained the same according to the nutrition dimension of the Barthel Index suggested that the swallowing training provided to the patient had an effect on shortening the duration of eating and the increasing the amount of food consumed during meals. Krajczy et al. (2019) have applied comprehensive swallowing therapy including training to the patient and family about safe food and fluid intake in the early period in patients with stroke and with dysphagia, and they found that there was a significant decrease in swallowing time after therapy in the experimental group. In the same study, it was emphasized that a comprehensive therapy could reduce the complications that may develop owing to dysphagia.
It was determined that sodium and BUN values increased in patients after the first follow-up, albumin and BMI decreased, and these differences in the measurement results were statistically significant (p < .05) (Table 5). Because of the lack of an accepted standard for the determination of dehydration, the number of studies revealing the relationship between dysphagia and hydration is less than the number of studies revealing the relationship between dysphagia and nutritional status. Dehydration is a complication associated with poststroke dysphagia and is associated with the 3-month mortality after a stroke. BUN value is considered to be one of the best indicators in the evaluation of dehydration. There is evidence indicating that the BUN/creatinine (Cr) levels may increase in patients with stroke and with dysphagia, which may lead to further dehydration. In general, a BUN value of 6–20 mg/dL is a common reference for hydration status (Crary et al., 2013). In the studies, a BMI value of below 18.5% and a serum albumin level of below 3.5 g/dL were considered as malnutrition (Boyraz, 2015; Horasan, 2012). In their study, Crary et al. (2013) have evaluated the nutrition (prealbumin) and hydration status (BUN/Cr) of patients with stroke and with dysphagia during admission to the hospital and 7 days after admission (at discharge), and they found that patients with stroke and dysphagia had higher BUN/Cr levels at admission and at discharge compared with patients with but without dysphagia. However, they could not find a significant relationship between dysphagia and malnutrition within the first 7 days after admission. Finestone et al. (1995) have evaluated albumin and transferrin levels, total lymphocyte count, BMI, skin thickness, and arm muscle circumference in patients with stroke and dysphagia, and they considered low values in at least 2 of the 6 parameters as malnutrition and reported the malnutrition rate as 65%. Davalos et al. (1996) have evaluated the albumin level, skin, and arm circumference in patients with stroke and with dysphagia and found malnutrition in 51% of them. According to the results of the studies, it can be said that patients with stroke and with dysphagia are at risk for dehydration and malnutrition during their hospital stay, and it is recommended that they be followed up in terms of adequate nutrition and hydration. Moreover, it is necessary to conduct relevant studies to determine other patient and/or healthcare factors that contribute to poor nutrition and hydration status in patients with stroke.
During the hospitalization period of the patients, it was seen that mean body temperature values did not differ significantly between morning and evening measurements (p < .01), and that body temperatures were within normal limits except for 1 patient (Table 6). It was determined that the body temperature of this patient reached 37.7°C only once in the evening measurement performed immediately after the visit time. Indeed, when the chest radiography of this patient was evaluated by his physician, it was observed that there was no evidence of infection. This result on the mean body temperature values of the patients was similar to the results of the study of Karabacak et al. (2012) in which they have evaluated the vital signs of the patients before, during, and after the visit and found a statistically significant difference in body temperature.
As a complication of the dysphagia, 9.4% of the patients developed aspiration during their stay in the hospital (Table 6). When the patients who developed aspiration were examined, it was observed that these patients had a previous lung problem. In the literature, it was reported that aspiration mostly occurred in patients with dysphagia and low level of consciousness (Palli et al., 2017; Westergren, 2006) and that the risk of developing pneumonia in patients with stroke and aspiration was 7.6 times higher than in patients without aspiration (Smith & Connolly, 2003). It is also indicated in the literature that approximately 35% of deaths observed after an acute stroke were related to pneumonia developing after aspiration owing to dysphagia (Turner-Lawrence et al., 2009). Early detection of dysphagia in patients with stroke is, therefore, important for the prevention of complications, especially pneumonia. It was determined that the incidence of pneumonia was higher in patients with stroke who were not screened for swallowing than in patients who were screened (Arsava et al., 2018). In particular, the determination that none of the patients experienced the signs and symptoms of aspiration in their third follow-up suggested that the patients continued to swallow and feed safely at home as a result of the swallowing training and follow-up applied with the evaluation of swallowing functions in the first 24–48 hours; and thus, the training applied may be effective in preventing the development of problems associated with dysphagia.
When the results obtained from the study were evaluated, it was observed that swallowing function could be strengthened in patients whose swallowing function was evaluated and were provided with swallowing training, that the completion time of portion at meals was reduced, that the amount of food consumed during meals increased, and that the development of complications owing to dysphagia could be prevented. The results of the study supported all hypotheses.
Study Limitations
This study had a few limitations, including the fact that the study was conducted in a single institution and with a single group because of the low clinical bed capacity (15 beds). Another limitation was the failure to create a control group, and the sample size was not determined by power analysis. The results of the study can only be generalized to patients who meet the sample selection criteria, and the use of structured forms prepared according to the literature owing to a lack of a valid and reliable scale evaluating dysphagia in Turkey.
Conclusion and Recommendations
It was determined that swallowing training decreased the duration of eating and increased the amount of food consumed in patients with and resulting dysphagia. The evaluation of swallowing function and the implementation of training supported by an effective material (brochure, and the like) on the patient or caregiver could be effective in preventing the development of problems and supporting the strengthening of swallowing function.
This study recommended that measurement tools be developed that provide more concrete results in the evaluation and follow-up of swallowing function and to perform reliability and validity studies, to include swallowing training guides to ensure safe swallowing and nutrition in the planning of care of patients with and with dysphagia, and to repeat the study as a randomized controlled experimental study.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the İstanbul University-Cerrahpaşa medical faculty clinical research ethics committee (date and number: 10.11.2009/B-015).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – C.S., R.A.; Design – C.S., R.A.; Supervision – C.S., R.A.; Resources – C.S., R.A.; Materials – C.S., R.A.; Data Collection and/or Processing – C.S.; Analysis and/or Interpretation - C.S., R.A.; Literature Search – C.S., R.A.; Writing Manuscript – C.S., R.A.; Critical Review – C.S., R.A.; Other – C.S., R.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- Akın S, Durna Z. Stroke and care. Turkiye Klinikleri Journal of Internal Medicine Nursing-Special Topics. 2016;2(2):10–25. [Google Scholar]
- Arsava EM, Aydoğdu İ, Güngör L, Işıkay CT, Yaka E. Nutritional approach and treatment in patients with stroke, an expert opinion for Turkey. Turkish Journal of Neurology. 2018;24(3):226–242. doi: 10.4274/tnd.92603. [DOI] [Google Scholar]
- Benbir G, İnce B. Stroke and woman. Turkish Journal of Cerebrovascular Diseases. 2013;19(3):84–87. doi: 10.5505/tbdhd.2013.03522. [DOI] [Google Scholar]
- Bonilha HS, Simpson AN, Ellis C, Mauldin P, Harris BM, Simpson K. The one-year attributable cost of post-stroke dysphagia. Dysphagia. 2014;29(5):545–552. doi: 10.1007/s00455-014-9543-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyraz S. İnmeli bireylerde yutma ve beslenme. [Swallow and nutrition in stroke individuals]. Türkiye Klinikleri Journal of Internal Medicine Nursing-Special Topics. 2015;1(1):1–6. [Google Scholar]
- Crary MA, Humphrey JL, Carnaby-Mann G, Sambandam R, Miller L, Silliman S. Dysphagia, nutrition, andhydration in ischemic stroke patients at admission and discharge from acute care. Dysphagia. 2013;28(1):69–76. doi: 10.1007/s00455-012-9414-0. [DOI] [PubMed] [Google Scholar]
- Crary MA, Carnaby GD, Sia I. Spontaneous swallow frequency compared with clinical screening in the identification of dysphagia in acute stroke. Journal of Strokeand Cerebrovascular Diseases. 2014;23(8):2042–2053. doi: 10.1016/j.jstrokecerebrovasdis.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çiyiltepe M. Yutma bozukluklarının rehabilitasyonu. [Rehabilitation of swallowing disorders]. Türkiye Klinikleri. 2004;4(3):195–201. [Google Scholar]
- Davalos A, Ricart W, Gonzalez Huix F, Soler S, Marrugat J, Molins A, Suner R, Genis D. Effect of malnutrition after acute stroke on clinical outcome. Stroke. 1996;27(6):1028–1032. doi: 10.1161/01.STR.27.6.1028. [DOI] [PubMed] [Google Scholar]
- Demirci Şahin A, Üstü Y, Işık D, Öztaş D, Karataş Eray İ, Uğurlu M. Demographic characteristics of patients who had cerebrovascular disease and management of risk factors which can be prevented in primary health centers. Ankara Medical Journal. 2015;15(4):196–208. doi: 10.17098/amj.79435. [DOI] [Google Scholar]
- Elfetoh EEEA, Karaly SFM. Effect of swallowing training program on dysphagia following cerebrovascular stroke. Egyptian Nursing Journal. 2018;15(2):125–134. [Google Scholar]
- Ertan T, Eker E, Güngen C. The standardised mini mental state examination for illiterate Turkish elderly poupulation: SMMSE-E. 2nd International Symposium on Neurophysiological and Neuropsychological Assessment of Mental and Behavioral Disorders; Bursa, Turkey. 1999. [Google Scholar]
- Finestone HM, Greene Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: Prevalence and predictors. Archives of Physical Medicine Rehabilitation. 1995;76:310–316. doi: 10.1016/S0003-9993(95)80655-5. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician”. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gulanick M, Myers JL. Nursing care plans: Nursing diagnosis and intervention. 6th ed. St Louis: Elsevier; 2007. [Google Scholar]
- Güngen C, Ertan T, Eker E, Yaşar R, Engin F. Reliability and validity of the standardized mini mental state examination in the diagnosis of mild dementia in Turkish population. Türk Psikiyatri Dergisi. 2002;13:273–281. [PubMed] [Google Scholar]
- Hines S, Wallace K, Crowe L, Finlayson K, Chang A, Pattie M. Identification and nursing management of dysphagia in individuals with acute neurological impairment (update) JBI Evidence Synthesis. 2010;8(6):255–301. doi: 10.11124/jbisrir-2010-113. [DOI] [PubMed] [Google Scholar]
- Horasan NE. In: Hemşirelik esasları: Hemşirelik bilimi ve sanatı. Atabek Aştı Beslenme T, Karadağ A., editors. [Nutrition Fundamentas of nursing: science and art of Nursing]. İstanbul: Akademi Basın ve Yayıncılık.; 2012. [Google Scholar]
- Huang KL, Liu TY, Huang YC, Leong CP, Lin WC, Pong YP. Functional outcome in acute stroke patients with oropharyngeal dysphagia after swallowing therapy. Journal of Stroke and Cerebrovascular Diseases. 2014;23(10):2547–2553. doi: 10.1016/j.jstrokecerebrovasdis.2014.05.031. [DOI] [PubMed] [Google Scholar]
- Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, Scott PA. American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- Kang JH, Park RY, Lee SJ, Kim JY, Yoon SR, Jung KI. The effect of bedside exercise program on stroke patients with dysphagia. Annals of Rehabilitation Medicine. 2012;36(4):512–520. doi: 10.5535/arm.2012.36.4.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karabacak Ü, Şenturan L, Özdilek S, Şimşek A, Karateke Y, Eti Aslan F, Ertekin C. The impact of visits on vital signs of the patients in surgical intensive care unit: A pilot study. Ulusal Travma ve Acil Cerrahi Dergisi. 2012;18(1):18–22. doi: 10.5505/tjtes.2012.58908. [DOI] [PubMed] [Google Scholar]
- Karaca Umay E, Gürçay E, Ünlü E, Ekşioğlu E, Çakcı A. Functional and nutritional effects of dysphagia in early stroke patients. Türkiye Klinikleri. 2010;30(3):925–931. doi: 10.5336/medsci.2008-9549. [DOI] [Google Scholar]
- Krajczy E, Krajczy M, Luniewski J, Bogacz K, Szczegielniak J. Assessment of the effects of dysphagia therapy in patients in the early post-stroke period: A randomised controlled trial. Neurologia i Neurochirurgia Polska. 2019;53(6):428–434. doi: 10.5603/PJNNS.a2019.0053. [DOI] [PubMed] [Google Scholar]
- Küçükdeveci AA, Yavuzer G, Tennant BA, Süldür N, Sonel B, Arasıl T. Adaptation of the modified Barthel index for use in physical medicine and rehabilitation in Turkey. Scandinavian Journal of Rehabilitation Medicine. 2000;32(2):87–92. doi: 10.1080/003655000750045604. [DOI] [PubMed] [Google Scholar]
- Lin LC, Wang SC, Chen SH, Wang TG, Chen MY, Wu SC. Efficacy of swallowing training for residents following stroke. Journal of Advanced Nursing. 2003;44(5):469–478. doi: 10.1046/j.0309-2402.2003.02830.x. [DOI] [PubMed] [Google Scholar]
- Mahoney FI, Barthel D. Functional evaluation: The Barthel Index. Maryland State Medical Journal. 1965;14:56–61. doi: 10.1037/t02366-000. [DOI] [PubMed] [Google Scholar]
- McCullough GH, Kamarunas E, Mann GC, Schmidley JW, Robbins JA, Crary MA. Effects of Mendelsohn maneuver on measures of swallowing duration post stroke. Topics in Stroke Rehabilitation. 2012;19(3):234–243. doi: 10.1310/tsr1903-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane M, Miles A, Atwal P, Parmar P. Interdisciplinary management of dysphagia following stroke. British Journal of Neuroscience Nursing, Supplement. 2014;10(1):13–20. doi: 10.12968/bjnn.2014.10.1.13. [DOI] [Google Scholar]
- Mourao AM, Almeida EO, Lemos SMA, Vicente LCC, Teixeira AL. Evolution of swallowing in post-acute stroke: A descriptive study. Revista CEFAC. 2016;18(2):417–425. doi: 10.1590/1982-0216201618212315. [DOI] [Google Scholar]
- Nii M, Maeda K, Wakabayashi H, Nishioka S, Tanaka A. Nutritional improvement and energy intake are associated with functional recovery in patients after cerebrovascular disorders. Journal of Stroke Cerebrovascular Disease. 2016;25(1):57–62. doi: 10.1016/j.jstrokecerebrovasdis.2015.08.033. [DOI] [PubMed] [Google Scholar]
- Osawa A, Maeshima S, Tanahashi N. Water-swallowing test: Screening for aspiration in stroke patients. Cerebrovascular Diseases. 2013;35(3):276–281. doi: 10.1159/000348683. [DOI] [PubMed] [Google Scholar]
- Özdemir A, Çekin AH. Disfajiye genel yaklaşım. [General approach to dysphagia]. Güncel Gastroenteroloji. 2011;15(4):227–234. [Google Scholar]
- Öztürk A, Tartar A, Ersöz Hüseyinsinioğlu B. İnme sonrası üst ekstremite motor fonksiyonunun kinematik analizi. Tıp Teknolojileri Ulusal Kongresi; Kapadokya: 2014. [Google Scholar]
- Paciaroni M, Mazzotta G, Corea F, Caso V, Venti M, Milia P, Gallai V. Dysphagia following stroke. European Neurology. 2004;51(3):162–167. doi: 10.1159/000077663. [DOI] [PubMed] [Google Scholar]
- Palli C, Fandler S, Doppelhofer K, Niederkorn K, Enzinger C, Vetta C, Gattringer T. Early dysphagia screening by trained nurses reduces pneumonia rate in stroke patients. STROKE. 2017;48(9):2583–2585. doi: 10.1161/STROKEAHA.117.018157. [DOI] [PubMed] [Google Scholar]
- Perry L. Screening swallowing function of patients with acute stroke. Part two: Detailed evaluation of the tool used by nurses. Journal of Clinical Nursing. 2001;10(4):474–481. doi: 10.1046/j.1365-2702.2001.00502.x. [DOI] [PubMed] [Google Scholar]
- Potter PA, Perry AG. Fundamentals of nursing. 7th ed. Elsevier; 2008. pp. 1087–1127. [Google Scholar]
- Selçuk B. Dysphagia in stroke. Türk Fiziksel Tıp ve Rehabilitasyon Dergisi. 2006;52(Özel Ek B):38–44. [Google Scholar]
- Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for the stroke rehabilitation. Journal of Clinical Epidemiology. 1989;42(8):703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- Smith HA, Lee SH, O’Neill P, Connolly MJ. The combination of bedside swallowing assesment and oxygen saturation monitoring of swallowing in acute stroke: A safe and humane screening tool. Age and Agening. 2000;29(6):495–499. doi: 10.1093/ageing/29.6.495. [DOI] [PubMed] [Google Scholar]
- Smith HA, Connolly MJ. Evaluation and treatment of dysphagia following stroke. Topics in Geriatric Rehabilitation. 2003;19(1):43–59. doi: 10.1097/00013614-200301000-00004. [DOI] [Google Scholar]
- Smithard D, Smeeton NC, Wolfe CDA. Long-term outcome after stroke: Does dysphagia matter. Age and Ageing. 2007;36(1):90–94. doi: 10.1093/ageing/afl149. [DOI] [PubMed] [Google Scholar]
- Tippett DC. Clinical challenges in the evaluation and treatment of individuals with post stroke dysphagia. Topics in Stroke Rehabilitation. 2011;18(2):120–133. doi: 10.1310/tsr1802-120. [DOI] [PubMed] [Google Scholar]
- Turner-Lawrence DE, Peebles M, Price MF, Singh SJ, Asimos AW. A feasibility study of the sensitivity of emergency physician dysphagia screening in acute stroke patients. Annals of Emergency Medicine. 2009;54(3):344–348. doi: 10.1016/j.annemergmed.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Tülek Z, Poulsen I, Gillis K, Jonsson AC. Nursing care for stroke patients: A survey of current practice in 11 European countries. Journal of Clinical Nursing. 2018;27(3–4):684–693. doi: 10.1111/jocn.14017. [DOI] [PubMed] [Google Scholar]
- Türkmen Ç. Akut iskemik inmede yutma değerlendirmesi. [Evaluation of swallowing in acute ischemic stroke]. (Nöroloji Uzmanlık Tezi) Şişli Etfal Eğitim ve Araştırma Hastanes person-group-type="editor"i; İstanbul: 2005. [Google Scholar]
- Vural H, Çiyiltepe M, Aslan F. Disfajili hastanın beslenmesi ve hemşirelik bakımı. [Nutrition and nursing care of the patient with dysphagia]. Türkiye Klinikleri. 2004;4(3):202–210. [Google Scholar]
- Werner H. The benefits of the dysphagia clinical nurse specialist role. Journal of Neuroscience Nursing. 2005;37(4):212–215. doi: 10.1097/01376517-200508000-00008. [DOI] [PubMed] [Google Scholar]
- Westergren A. Detection of eating difficulties after stroke: A systematic review. International Nursing Rreview. 2006;53(2):143–149. doi: 10.1111/j.1466-7657.2006.00460.x. [DOI] [PubMed] [Google Scholar]


