Abstract
AIM
This study aimed to compare the measurement results of arterial blood pressure obtained through intra-arterial, auscultatory, and oscillometric methods.
METHOD
This prospective and descriptive study was conducted with 180 patients hospitalized in the intensive care units of cardiovascular surgery and anesthesia. Arterial blood pressures of the patients in the study were measured with 3 methods, and the mean arterial pressure values obtained by each method were analyzed to find out whether they were different or consistent.
RESULTS
The average systolic blood pressure value using the intra-arterial method was found to be 125.47 ± 21.39 mm Hg, and the average of diastolic blood pressure measurement obtained using the oscillometric method was the highest (73.91 ± 10.62 mm Hg). The highest correlation was seen between the arterial BP measurements of the intra-arterial and auscultatory methods (systolic [0.96] and diastolic [0.90]). According to the British and Irish Hypertension Society protocol, a very good agreement between the diastolic blood pressure values and a good agreement between the systolic blood pressure values were obtained.
CONCLUSION
The measurement results obtained through the auscultatory method more consistent with the results obtained through the intra-arterial method compared with those obtained using the oscillometric method.
Keywords: Auscultatory, blood pressure, intra-arterial, oscillometric
Introduction
Arterial blood pressure (BP) is a key measurement of hemodynamic status and is a marker of adequate organ perfusion and tissue flow (Thomas & Rees, 2018). Arterial BP is measured routinely in clinical settings (McMahon et al., 2012) and is a parameter used for making several diagnostic and treatment decisions (Ribezzo et al., 2014). Inaccurate measurement of BP might lead to misdiagnoses, inadequate control of BP, and inappropriate treatments (Barnason et al., 2012). It is therefore important to determine BP values accurately (McMahon et al., 2012).
Measuring BP directly from the artery using intra-arterial catheters is the gold standard (Kayrak et al., 2008; Romagnoli et al., 2014). However, it is an expensive and invasive procedure and carries an increased risk of complications (Meidert & Saugel, 2018; Spelde & Monahan, 2016). Therefore, the insertion of an intra-arterial cannula is not desirable in all patients. Instead, noninvasive methods are preferred to measure BP (Büyüköztürk, 2000; Meidert et al., 2018).
Until recently, the auscultatory BP (ABP) measurement method on the basis of the hearing of the Korotkoff sounds was widely used; however, in recent years, it has been replaced by the oscillometric measurement method. Today, in all areas of healthcare and in homes, automated BP devices that measure BP on the upper arms or wrists are being widely used (Micozkadıoğlu, 2011). Oscillometric sphygmomanometers allow multiple measurements of BP in a short time and are simple to use (Akpolat, 2010).
A significant increase in devices designed for the measurement BP has raised concerns about whether the measurement of arterial BP performed with these different instruments and methods is accurate and reliable as BP itself can be extremely variable (Akpolat, 2010; Kaczorowski et al., 2012). The differences between the BP results obtained by the direct intra-arterial (invasive) method and the indirect (noninvasive) method may adversely affect treatment decisions (Araghi et al., 2006).
In the literature related to BP measurement methods, there are several studies on the different devices and methods used to measure BP. A study by Jones et al. (2001) conducted to compare the oscillometric and auscultatory methods, which are noninvasive BP measurement methods, determined that the results obtained with the oscillometric method were higher. A study by Watson et al. (1998), compared BP measurements obtained using the intra-arterial method with those obtained with an oscillometric wrist device and mercury sphygmomanometer and found that both diastolic and systolic BP values obtained with the mercury sphygmomanometer were higher than those obtained using the other 2 methods.
A study by Vera-Cala et al. (2011) conducted to compare the BP values of 1,084 randomly selected people aged between 15 and 64 years, revealed that systolic BP (SBP) values obtained with the oscillometric method were 1.8 mm Hg higher than those obtained with the auscultation method; however, diastolic BP (DBP) values determined using the former were 1.6 mm Hg lower than those determined with the latter method. In a study by Holt et al. (2011), the direct arterial method was compared with indirect BP measurement methods. They found that there was no clinically significant difference between the methods in normotensive children. A study by Ribezzo et al. (2014) found that the SBP values obtained intra-arterially and DBP values obtained with the auscultatory method were higher.
This study aimed to investigate whether BP values obtained from ABP and oscillometric BP (OBP) measurements, which are commonly used in healthcare centers and in homes, were consistent with each other and with the values obtained with the intra-arterial method.
Research Questions
In arterial BP measurements,
Are BP values obtained with the auscultatory method consistent with those obtained with the intra-arterial method?
Are BP values obtained with the oscillometric method consistent with those obtained with the intra-arterial method?
Are BP values obtained with the auscultatory and oscillometric methods consistent with each other?
Methods
Study Design
This was a prospective and descriptive study.
Sample
This study was conducted in the intensive care units of the cardiovascular surgery and anesthesia clinics of a university hospital in the province of Izmir in January and August 2014. The study sample included 180 patients who met the inclusion criteria, agreed to participate in the study, and were hospitalized and treated in the intensive care units where the study was conducted. To determine the sample size (the power of the research was set to be at least 80%), power analysis was used.
Inclusion Criteria
The sample included patients over 18 years of age who:
Agreed to participate in the study.
Had an intra-arterial catheter inserted in the radial artery.
Had an upper arm circumference of 16–30 cm.
Had different stable vital signs and normal range during arterial blood pressure measurements.
Did not have cardiac rhythm disorders, fractures, peripheral vascular diseases, edema, skin lesions, or burns and/or fistula in the upper arm.
Did not have any disorder preventing the patient from lying in a supine position.
Did not have heart rate changes greater than 10 beats per minute, pain or any other stimulant during BP measurements.
Did not have high-dose fluid treatment likely to affect BP or the discontinuation of this treatment in the last 6 hours.
Did not have a BP deviation of 20 mm Hg or more in the last 6–8 hours.
Did not have drugs used in the treatment of hypertension or hypotension in the last 6–8 hours.
Data Collection
For the collection of the study data, the case report form, aneroid sphygmomanometer (F. Bosch Aneroid Sphygmomanometer), automatic upper arm BP monitor (Microlife BP 3AC1-PC oscillometric), and intra-arterial BP (IABP) monitor (Nihon Kohden) were used. The case report form included items inquiring which intensive care unit the patient was hospitalized in; the patient’s sex, age, body mass index; and the diagnosis and drugs the patient was on.
All BP measurements were made with the patient in the supine position, with the arm kept straight at the heart level and supported from the bottom and the palm facing upward. For all the measurement methods, BP values were measured twice and their averages calculated. First, the patients’ IABP values were obtained twice from the monitor at an interval of 15 seconds; then the auscultatory and the oscillometric methods were used on the upper arm with radial artery catheterization at 5-minute intervals.
In the study, indirect BP measurements were made by a single researcher. To avoid bias in indirect measurements, arterial BP measurements were made by a blinded observer, who did not participate in the indirect measurements, by reading the values on the intra-arterial monitor.
BP Measurement Protocol
Auscultation method
The brachial artery was located, and the cuff was placed on the arm with the lower edge 2–3 cm above the antecubital fold. After placing a stethoscope on the artery, the cuff was inflated. Then the air in the cuff was deflated at a rate of 2–3 mm Hg/sec. When the first Korotkoff sound was heard through the stethoscope, the reading on the manometer was determined as the SBP value. The reading on the manometer was determined as the DBP value when the sound ceased.
Oscillometric method
The measurement was made by locating the cuff with its center on the brachial artery of the arm with radial artery catheterization. Connective tubes were placed at the front of the forearm, and BP values measured were recorded.
IABP measurement
BP values on the monitor were recorded twice at 15-second intervals.
Statistical Analysis
The data were evaluated using the Statistical Package for Social Sciences version 16.0 (SPSS Inc.; Chicago, Il, USA). Descriptive statistics were calculated for quantitative items. The paired sample t test, independent sample t test, one-way analysis of variance, Tukey test, correlation analysis, and the Bland-Altman analysis were used to analyze the data. Statistical significance was set at p ≤ .05.
All the mean values of the BP measurements were verified to be within acceptable limits according to the British and Irish Hypertension Society (BIHS) protocol (O’Brien et al., 1993).
(*The British Hypertension Society changed its name to the British and Irish Hypertension Society in 2016).
Ethical Considerations
The study was approved date 25.09.2013 number is 2013-13 by the Ethical Commitee of Ege University Nursing Faculty was obtained before the study from the board of scientific ethics (#2013-41) and the institution where the study was to be conducted. The recruited patients were informed about the study and their verbal and written consents obtained. Informed consents were obtained from the legal guardians for the patients who were unconscious or unable to make decisions. The patient-identifying information was not used during or after the study.
Results
Of the patients, 69.4% were men, 55% were in the 41–65 age group (mean 7.07 ± 14.85 years), 47.0% had a diagnosis of cardiovascular system disease. BP measurement of 61.7% of the patients was made on the left arm. Table 1 shows the descriptive characteristics of the participating patients.
Table 1.
Descriptive Characteristics of the Participating Patients
| n | % | ||
|---|---|---|---|
| Sex | Women | 55 | 30.6 |
| Men | 125 | 69.4 | |
| Age (years) | 18–40 | 20 | 11.1 |
| 41–65 | 99 | 55.0 | |
| 66 and above | 61 | 33.9 | |
| Intensive care unit | Cardiovascular surgery | 109 | 60.6 |
| Anesthesia | 71 | 39.4 | |
| Measurement arm | Right | 69 | 38.3 |
| Left | 111 | 61.7 | |
| Diagnosis (n = 259)* | Cardiovascular system diseases | 122 | 47.0 |
| Cerebrovascular system diseases | 32 | 12.4 | |
| Respiratory system diseases | 52 | 20.1 | |
| Gastrointestinal system diseases | 20 | 7.7 | |
| Endocrine system diseases | 12 | 4.6 | |
| Urinary system diseases | 8 | 3.1 | |
| Other diseases | 13 | 5.1 |
Note.
The number of some patients is shown to be higher because many had multiple diseases.
Comparison of mean BP values determined through the intra-arterial and auscultatory methods are shown in Table 2. Although the mean SBP values determined using the intra-arterial method (t = 11.59, p = .000) were higher than those determined with the auscultatory method, the mean DBP values determined using the auscultatory method (t = −4.20, p = .000) were higher than those determined with the intra-arterial method. The results of the Bland-Altman analysis are shown in Figures 1 and 2. Bland-Altman analysis showed that the limits of the agreement for auscultatory SBP (ASBP) and intra-arterial SBP (IASBP) values ranged from −6.1 to 15.7 mm Hg; and for auscultatory DBP (ADBP) and intra-arterial DBP (IADBP) values, the limits ranged between −10.7 and 7.8 mm Hg (Figures 1 and 2). According to the BIHS protocol, a very good agreement between the DBP values and a good agreement between the SBP values were obtained, Table 3.
Table 2.
Differences between Systolic and Diastolic BP Measured Using Intra-Arterial, Auscultatory, and Oscillometric Methods
| Systolic Mean ± SD | Diastolic Mean ± SD | |
|---|---|---|
| Intra-arterial method | 125.47 ± 21.39 | 64.59 ± 11.18 |
| Auscultatory method | 120.68 ± 19.57 | 66.07 ± 10.26 |
| Difference | 4.79 ± 5.54 | −1.47 ± 4.71 |
| p value* | t = 11.59 p = .000 | t = −4.20. p = .000 |
| Intra-arterial method | 125.47 ± 21.39 | 64.59 ± 11.18 |
| Oscillometric method | 121.13 ± 19.04 | 73.91 ± 10.62 |
| Difference | 4.33 ± 12.11 | −9.31 ± 7.98 |
| p value* | t = 4.80. p = .000 | t = −15.66. p = .000 |
| Auscultatory | 120.68 ± 19.57 | 66.07 ± 10.26 |
| Oscillometric | 121.13 ± 19.04 | 73.91 ± 10.62 |
| Difference | −1.55 ± 9.52 | −7.84 ± 7.38 |
| p value* | t = −.64. p = .552 | t = −14.24. p = .000 |
Note.
Paired samples t test.
Figure 1.
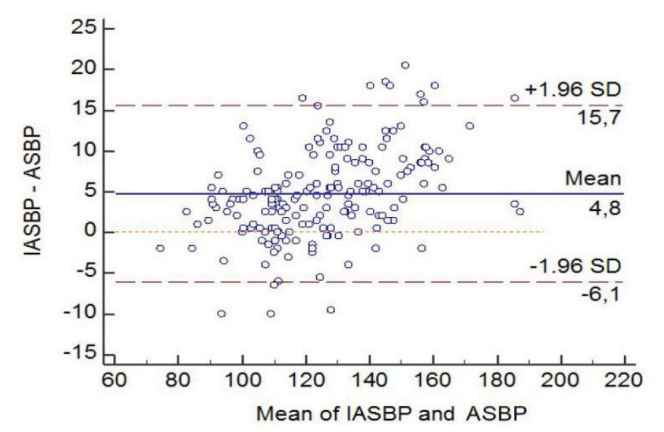
Bland-Altman Analysis of the Agreement between Mean Systolic BP Values Using Intra-Arterial and Auscultatory Methods
Note: IASBP = Intra-arterial systolic BP; ASBP = Auscultatory systolic BP
Figure 2.
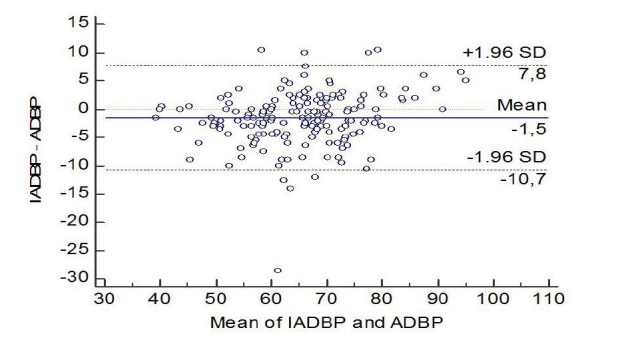
Bland-Altman Analysis of the Agreement between Mean Diastolic BP Values Using Intra-Arterial and Auscultatory Methods
Note: IADBP = Intra-arterial diastolic BP; ADBP = Auscultatory diastolic BP
Table 3.
BIHS Grade of Agreement between Methods: Cumulative Percentage of Absolute Difference (mm Hg) between IABP, ABP, and OBP
| ≤5 mm Hg | ≤10 mm Hg | ≤15 mm Hg | ≤20 mm Hg | BIHS grade* | |
|---|---|---|---|---|---|
| IABP versus ABP (%) | |||||
| Systolic | 54.4 | 82.8 | 94.4 | 99.4 | B (good) |
| Diastolic | 79.4 | 96.1 | 99.4 | 99.4 | A (very good) |
| IABP versus OBP (%) | |||||
| Systolic | 33.9 | 57.8 | 73.3 | 85.6 | D (very poor) |
| Diastolic | 19.4 | 54.4 | 81.1 | 93.3 | D (very poor) |
| ABP versus OBP (%) | |||||
| Systolic | 40.6 | 71.1 | 87.2 | 95.6 | C (poor) |
| Diastolic | 29.4 | 63.9 | 85.6 | 94.4 | D (very poor) |
Note: IABP = Intra-arterial BP; ABP = Auscultatory BP; OBP = Oscillometric BP; BIHS = British and Irish Hypertension Society.
Grades are derived from percentages of readings within 5, 10, and 15 mm Hg. To achieve a grade, all 3 percentages must be equal to or greater than the tabulated values. For example, to achieve the “A” grade, 60% of the measured BP values with intra-arterial BP and auscultatory BP must be within 5 mm Hg, 85% within 10 mm Hg, and 95% within 15 mm Hg. The limit of ≤20 mm Hg does not belong to the BIHS criteria and has been inserted to highlight, in particular, the poor agreement for systolic or diastolic arterial pressure.
Comparison of mean the BP values determined through the intra-arterial and oscillometric methods is shown in Table 2. The mean SBP values determined with the intra-arterial method (t = 4.80, p = .000) were higher than those determined with the oscillometric method, and the mean DBP values determined with the oscillometric method (t = −15.66, p = .000) were higher than those determined using the intra-arterial method. The results of the Bland-Altman analysis are shown in Figure 3. Bland-Altman analysis showed that the limits of the agreement for the oscillometric SBP (OSBP) and IASBP values ranged from −19.4 to 28.1 mm Hg; and for the oscillometric DBP (ODBP) and IADBP values, they ranged between −25.0 and 6.3 mm Hg, Figure 4. According to the BIHS protocol, a very poor agreement was obtained both for the SBP values and for the DBP values, Table 3.
Figure 3.
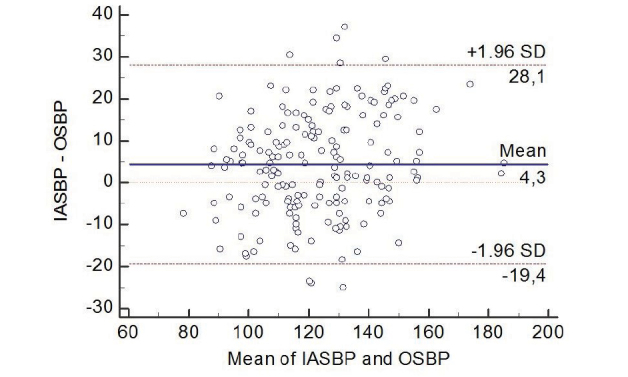
Bland-Altman Analysis of the Agreement between Mean Systolic BP Values Using Intra-Arterial and Oscillometric Methods
Note: IASBP = Intra-arterial systolic BP; OSBP = Oscillometric systolic BP
Figure 4.
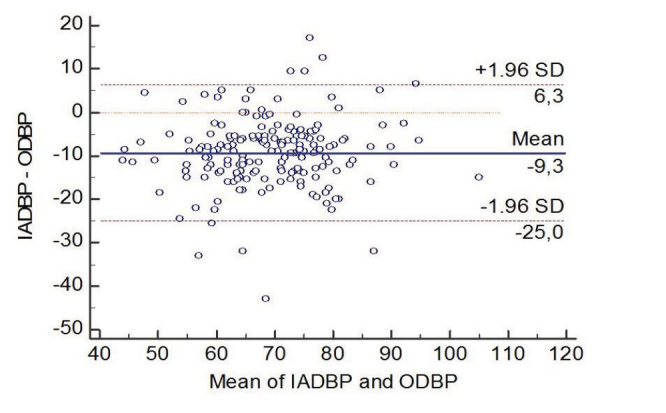
Bland-Altman Analysis of the Agreement between Mean Diastolic BP Values Using Intra-Arterial and Oscillometric Methods
Note: IADBP = Intra-arterial diastolic BP; ODBP = Oscillometric diastolic BP
Comparison of the mean BP values determined through the auscultatory and oscillometric methods is shown in Table 2. No differences were determined between the mean ASBP and OSBP values (t = −.64, p = .552). The mean ODBP values were higher than the mean ADBP values (t = −14.24, p = .000). The results of the Bland-Altman analysis are shown in Figures 5 and 6. Bland-Altman analysis showed that the limits of the agreement for the OSBP and ASBP values ranged from −19.1 to 18.2 mm Hg, and for the ODBP and ADBP values, they ranged between −22.3 and 6.6 mm Hg. According to the BIHS protocol, a poor agreement was obtained for the SBP values and a very poor agreement for the DBP values as shown in Table 3.
Figure 5.
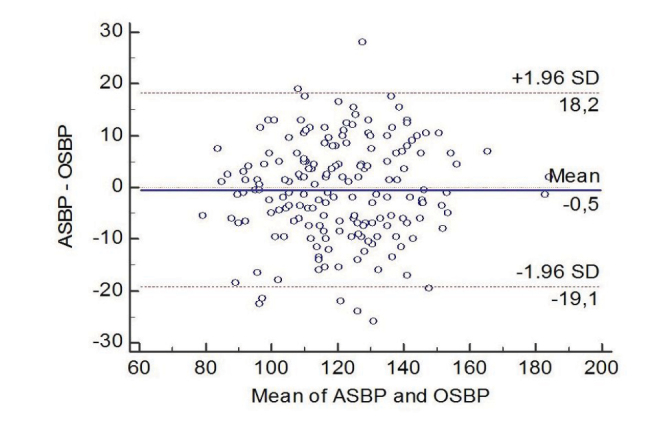
Bland-Altman Analysis of the Agreement between Mean Systolic BP Values Using Auscultatory and Oscillometric Methods
Note: ASBP = Auscultatory systolic BP; OSBP = Oscillometric systolic BP
Figure 6.
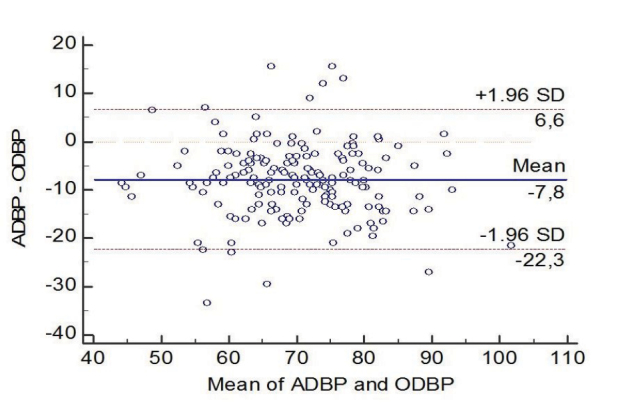
Bland-Altman Analysis of the Agreement between Mean Diastolic BP Values Using Auscultatory and Oscillometric Methods
Note: ADBP = Auscultatory diastolic BP; ODBP = Oscillometric diastolic BP
Discussion
This study results revealed that the mean SBP values obtained with the intra-arterial method were higher than those obtained with the auscultatory and oscillometric methods (p < .001) and that the mean DBP values obtained with the auscultatory and oscillometric methods were higher than those obtained with the intra-arterial method (p < .001).
The comparison of noninvasive arterial BP measurements with IABP measurements carried out in studies with different patient groups revealed that the former were inaccurate (Araghi et al., 2006; Bur et al., 2003; Manios et al., 2007; Mireles et al., 2009; Muecke et al., 2009). The study by Wax et al. (2011) found a difference between noninvasive BP and IABP values.
In a study by Neslioğlu (2004), a difference was found between the mean SBP values and between the mean DBP values measured with intra-arterial and oscillometric methods. As in other studies, in this study too, the BP results obtained with the auscultatory and oscillometric methods were different from those obtained with the intra-arterial method considered as the gold standard, which suggests that the results obtained with the auscultatory and oscillometric methods which are routinely used in clinics, and sometimes in intensive care units, might be misleading and thus could lead to misdiagnoses and wrong treatments.
Although there are no precise data in the literature, Gibbs et al. (1991) have reported that in patients under anesthesia, differences higher than 10 mm Hg should be regarded as clinically significant and that differences higher than 20 mm Hg should be considered unacceptable. In this study, the highest difference was between the ODBP and IADBP values −9.31 ± 7.98 mm Hg), and the lowest difference was between the IADBP and ADBP values (−1.47 ± 4.71 mm Hg). According to the BIHS criteria, although the agreement between ASBP and IASBP measurements was very good, it was good between IADBP and ADBP measurements. The agreement between the SBP measurements and that between the DBP measurements obtained with the IABP and OBP methods were very poor. In a study by Ribezzo et al. (2014), according to the BIHS protocol, there was a very good agreement between IADBP and ODBP values.
In this study, among the differences higher than 10 mm Hg, the lowest ones were between the IABP and ABP methods (systolic: 17.2%; diastolic: 3.9%), and highest ones were between the IABP and OBP methods (systolic 42.2%; diastolic 45.6%) (Table 3 shows the differences lower than 10 mm Hg). These results indicate that the BP results obtained with the auscultatory method were closer to the BP results obtained with the intra-arterial method. Therefore, the results obtained with the oscillometric measurement method are believed to be more misleading, particularly in determining the treatment protocol of critically ill patients.
Bland-Altman analysis revealed a poor agreement between IADBP and ODBP values. On the basis of these results, we can hypothesize that none of the measurement values, except for the ADBP values, were consistent with the values determined with the intra-arterial method considered as the gold standard. Meng et al. (2013) found a moderate correlation between the SBP values and a very limited correlation between the DBP values obtained with the intra-arterial and oscillometric methods. They also found that the agreement between the 2 methods was poor per the Bland-Altman analysis. Amadasun and Isa compared the auscultatory method with the oscillometric method and determined the correlations between SBP and between DBP values obtained with the 2 methods as r = .81 and r = .95, respectively (Amadasun & Isa, 2005). Therefore, it can be said that the results obtained with the auscultatory method were closer to the results obtained with the intra-arterial method. In their systematic study investigating the variability and reliability of manual and automated BP measurements, Skirton et al. (2011) reviewed 16 papers published between January 1997 and May 2009 and stated that BP measurement results obtained with the auscultatory method were more reliable than those obtained with the oscillometric method. The results of this study support this conclusion.
In this study, we determined that the mean ODBP results were higher (mean difference = −7.8, p = .000), and that the agreement between the 2 methods was poor for the SBP values and very poor for the DBP values according to the BIHS protocol. In a study by Landgraf et al. (2010), the auscultatory and oscillometric methods were compared, and the mean BP values obtained with the auscultatory method were reported to be higher. Similarly, in their study Amadasun and Isa found that both ASBP (mean difference = 7.3) and DBP values (mean difference = 3.7) were higher; however, these differences were not clinically significant (Amadasun et al., 2005). These results indicate that DBP measurements, in particular, obtained using the 2 methods were different from each other.
Conclusion and Recommendations
This study found that the differences between the mean SBP values were lesser, and for mean DBP values, the highest difference was between the intra-arterial and oscillometric methods, and the minimum difference was between the intra-arterial and auscultatory methods. On the basis of the BIHS protocol, the agreement between the IADBP and ADBP values and between the ASBP and IASBP values was very good and good, respectively.
Therefore, in clinics or other healthcare centers, results obtained with the auscultatory method should be preferred when diagnosing hypertension or hypotension.
Especially for critically ill patients, if the intra-arterial method cannot be used, the results obtained with the auscultatory method should be preferred.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Ege University Faculty of Nursing (Date: September 25, 2013; Decision numbered: 2013-41).
Informed Consent: Verbal and written consent was obtained from the patient and relatives.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – K.B., A.Z.; Design – K.B., A.Z.; Supervision – A.Z.; Resources – K.B., A.Z.; Materials – K.B.; Data Collection and/or Processing – K.B., A.Z.; Analysis and/or Interpretation – K.B., A.Z.; Literature Search – K.B.; Writing Manuscript – K.B.; Critical Review – A.Z.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- Akpolat T. Kan basıncı ölçüm cihazları ve problemler. Kan basıncı ölçüm aleti. Journal of Anatolia Kidney Foundation, Renaliz. 2010;11(37):6–7. [Google Scholar]
- Amadasun FE, Isa JI. A comparison of sphygmomanometric and oscillometric methods of blood pressure measurements in adult in-patients. Nigerian Journal of Clinical Practice. 2005;8(2):86–9. [PubMed] [Google Scholar]
- Araghi A, Bander JJ, Guzman JA. Arterial blood pressure monitoring in overweight critically ill patients: invasive or noninvasive? Critical Care. 2006;10:1–85. doi: 10.1186/cc4896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnason S, Williams J, Patrick VC, Storer A, Brim C, Halpern J, Leviner S, Lindauer C, Proehl AC, Bradford JY. Clinical Practice Guideline: Non-Invasive Blood Pressure Measurement with Automated Devices. Emergency Nurses Association; 2012. https://www.ena.org/docs/default-source/resource-library/practice-resources/CPG/nibpmcpg. [Google Scholar]
- Bur A, Herkner H, Vlcek M, Woisetschläger C, Derhaschnig U, Delle Karth G, Laggner AN, Hirschl MM. Factors influencing the accuracy of oscillometric blood pressure measurement in critically ill patients. Critical Care Medicine. 2003;31:793–799. doi: 10.1097/01.CCM.0000053650.12025.1A. [DOI] [PubMed] [Google Scholar]
- Büyüköztürk K. Kan Basıncının Ölçümü ve Klinik Değerlendirme. Türk Kardiyoloji Derneği Ulusal Hipertansiyon Tedavi ve Takip Kılavuzu (Turkish Society of Cardiology national Hypertension Treatment and Follow-Up Guide) 2000. https://tkd.org.tr/kilavuz/k03.htm.
- Gibbs NM, Larach DR, Derr JA. The accuracy of Finapres (TM) noninvasive mean arterial pressure measurements in anesthetized patients. Anesthesiology. 1991;74:647–652. doi: 10.1097/00000542-199104000-00004. [DOI] [PubMed] [Google Scholar]
- Holt TR, Withington DE, Mitchell E. Which pressure to believe? A comparison of direct arterial with indirect blood pressure measurement techniques in the pediatric intensive care unit. Pediatric Critical Care Medicine. 2011;12:391–394. doi: 10.1097/PCC.0b013e3182230f43. [DOI] [PubMed] [Google Scholar]
- Jones CR, Taylor K, Poston L, Shennan AH. Validation of the Welch Allyn ‘Vital Signs’ oscillometric blood pressure monitör. Journal of Human Hypertension. 2001;15:191–195. doi: 10.1038/sj.jhh.1001141. [DOI] [PubMed] [Google Scholar]
- Kaczorowski J, Dawes M, Gelfer M. Measurement of blood pressure: New developments and challenges. British Columbia Medical Journal. 2012;54:399–403. [Google Scholar]
- Kayrak M, Ülgen MS, Yazıcı M, Demir K, Doğan Y, Koç F, Zengin K, Arı H. Comparison between brachial blood pressures obtained by aneroid sphygmomanometer and central aortic pressures: factors affecting the measurements. Archives of the Turkish Society of Cardiology. 2008;36(4):239–246. [PubMed] [Google Scholar]
- Landgraf J, Wishner SH, Kloner RA. Comparison of automated oscillometric versus auscultatory. Blood pressure measurement. The American Journal of Cardiology. 2010;106(3):386–388. doi: 10.1016/j.amjcard.2010.03.040. [DOI] [PubMed] [Google Scholar]
- Manios E, Vemmos K, Tsivgoulis G, Barlas G, Koroboki E, Spengos K, Zakopoulos N. Comparison of noninvasive oscillometric and intra-arterial blood pressure measurements in hyperacute stroke. Blood Pressure Monitoring. 2007;12(3):149–156. doi: 10.1097/MBP.0b013e3280b083e2. [DOI] [PubMed] [Google Scholar]
- McMahon N, Hogg LA, Corfield AR, Exton AD. Comparison of non-invasive and invasive blood pressure in aeromedical care. Anaesthesia. 2012;67(12):1343–1347. doi: 10.1111/j.1365-2044.2012.07302.x. [DOI] [PubMed] [Google Scholar]
- Meidert AS, Saugel B. Techniques for non-invasive monitoring of arterial blood pressure. Frontiers in Medicine. 2018;4:231. doi: 10.3389/fmed.2017.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng X, Zang G, Fan L, Zheng L, Dai J, Wang X, Xia W, Liu J, Zhang C. Non-Invasive monitoring of blood pressure using the philips intellivue Mp50 monitor cannot replace invasive blood pressure techniques in surgery patients under general anesthesia. Experimental and Therapeutic Medicine. 2013;6(1):9–14. doi: 10.3892/etm.2013.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micozkadıoğlu H. Blood pressure monitorisation in hypertension management: Home? Office? Ambulatory? Turkish Nephrology, Dialysis and Transplantation Journal. 2011;20:214–219. doi: 10.5262/tndt.2011.1003.02. [DOI] [Google Scholar]
- Mireles SA, Richard A, Jaffe RA, David R, Drover DR, Brock-Utne JG. A poor correlation exists between oscillometric and radial arterial blood pressure as measured by the philips Mp90 monitor. Journal of Clinical Monitoring and Computing. 2009;23(3):169–174. doi: 10.1007/s10877-009-9178-8. [DOI] [PubMed] [Google Scholar]
- Muecke S, Bersten A, Plummer J. The mean machine; accurate non invasive blood pressure measurement in the critically ill patient. Journal of Clinical Monitoring and Computing. 2009;23(5):283–297. doi: 10.1007/s10877-009-9195-7. [DOI] [PubMed] [Google Scholar]
- Neslioğlu SE. Doctoral Thesis. Ondokuz Mayıs University; Samsun: 2004. The comparison of blood pressure values obtained with the mercury sphygmomanometer and oscillometric measurement methods with those obtained with the intra-arterial method. http://acikerisim.omu.edu.tr/xmlui/handle/20.500.12712/32235. [Google Scholar]
- O’Brien E, Petrie J, Little W, de Swiet M, Padfield PL, Altman DG, Bland M, Coats A, Atkins N. The British Hypertension Society protocol for the evaluation of blood pressure measuring devices. Journal of Hypertension. 1993;11:677–679. doi: 10.1097/00004872-199306000-00013. [DOI] [PubMed] [Google Scholar]
- Ribezzo S, Spina E, Di Bartolomeo S, Sanson G. Noninvasive techniques for blood pressure measurement are not a reliable alternative to direct measurement: A Randomized Crossover Trial in ICU. The Scientific World Journal. 20142014:353628. doi: 10.1155/2014/353628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romagnoli S, Ricci Z, Quattrone D, Tofani L, Tujjar O, Villa G, Romano SM, De Gaudio AR. Accuracy of invasive arterial pressure monitoring in cardiovascular patients: an observational study. Critical Care. 2014;18(6):644. doi: 10.1186/s13054-014-0644-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirton H, Chamberlain W, Lawson C, Ryan H, Young E. A systematic review of variability and reliability of manual and automated blood pressure readings. Journal of Clinical Nursing. 2011;20(5–6):602–614. doi: 10.1111/j.1365-2702.2010.03528.x. [DOI] [PubMed] [Google Scholar]
- Spelde A, Monahan C. In: Anesthesiology Core Review: Part 2, Advanced Exam Chapter 1: Invasive Arterial Blood Pressure Monitoring. Brian S, Freeman, Berger Jeffrey S, editors. McGraw-Hill Education; Cenveo®: 2016. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=1750§ionid=117318120. [Google Scholar]
- Thomas G, Rees D. Monitoring arterial blood pressure. Anaesthesia and Intensive Care Medicine. 2018;19(4):194–197. doi: 10.1016/j.mpaic.2018.02.003. [DOI] [Google Scholar]
- Vera-Cala LM, Orostegui M, Valencia-Angel L, López N, Bautista LE. Accuracy of the omron HEM-705 CP for blood pressure measurement in large epidemiologic studies. Arquivos Brasileiros De Cardiologia. 2011;96(5):393–398. doi: 10.1590/S0066-782X2011005000038. [DOI] [PubMed] [Google Scholar]
- Watson S, Wenzel RR, di Matteo C, Meier M, Lüscher TF. Accuracy of new wrist cuff ossilometric blood pressure devices. American Journal of Hypertension. 1998;11(12):1469–1474. doi: 10.1016/S0895-7061(98)00188-5. [DOI] [PubMed] [Google Scholar]
- Wax DB, Hung-Mo Lin, HM, Leibowitz AB. Invasive and concomitant noninvasive intraoperative blood pressure monitoring observed differences in measurements and associated therapeutic interventions. Anesthesiology. 2011;115(5):973–978. doi: 10.1097/ALN.0b013e3182330286. [DOI] [PubMed] [Google Scholar]


